Abstract
Purpose:
Little is known about adolescent relationship abuse (ARA) and related sexual and reproductive health among females who either identify as lesbian or bisexual or engage in sexual behavior with female partners (i.e., sexual minority girls [SMGs]).
Methods:
Baseline data were collected from 564 sexually active girls ages 14–19 years seeking care at eight California school-based health centers participating in a randomized controlled trial. Associations between ARA, sexual minority status and study outcomes (vaginal, oral, and anal sex, number and age of sex partners, contraceptive nonuse, reproductive coercion, sexually transmitted infection [STI] and pregnancy testing) were assessed via logistic regression models for clustered survey data.
Results:
SMGs comprised 23% (n = 130) of the sample. Controlling for exposure to ARA, SMGs were less likely to report recent vaginal sex (adjusted odds ratio [AOR],.51; 95% confidence interval [Cl],.35–.75) and more likely to report recent oral sex (AOR, 2.01; 95% CI, 1.38–2.92) and anal sex (AOR, 1.76; 95% CI, 1.26–2.46) compared with heterosexual girls. Heterosexual girls with ARA exposure (AOR, 2.85; 95% CI, 1.07–7.59) and SMGs without ARA exposure (AOR, 3.01; 95% CI, 2.01–4.50) were more likely than nonabused heterosexual girls be seeking care for STI testing or treatment than heterosexual girls without recent victimization.
Conclusions:
Findings suggest the need for attention to STI risk among all girls, but SMGs in particular. Clinicians should be trained to assess youth for sexual contacts and sexual identity and counsel all youth on healthy relationships, consensual sex, and safer sex practices relevant to their sexual experiences.
Keywords: Adolescent relationship abuse, Sexual minority youth, Sexually transmitted infections
Adolescent relationship abuse (ARA)—physical, sexual, and psychological abuse or harassment in romantic or intimate relationships—is experienced by as many as one in three youth [1,2]. Female adolescents who experience ARA are more likely to report sexual risk behaviors including early sexual initiation, multiple sexual partners, and inconsistent condom use [3,4] and sexual and reproductive health outcomes, including unintended pregnancy and sexually transmitted infections (STIs) [5–8]. These associations are likely related to the fear of and limited agency to negotiate whether, when, and how young women engage in sexual behavior with their abusive partners [3,7]. Recent studies have also documented reproductive coercion as another mechanism linking ARA and unintended pregnancy [5,9]. Collectively, these studies underscore the substantial burden of ARA on young women’s reproductive and sexual health.
Until recently, research on ARA has focused almost exclusively on violence in heterosexual relationships, generating little understanding of the experiences of girls who either identify as lesbian or bisexual or have sex with female partners (subsequently referred to as sexual minority girls [SMGs]). One recent nationally representative study found the prevalence of lifetime physical intimate partner violence to be higher among bisexual (61%) and lesbian women (44%) compared with their heterosexual counterparts (35%), and intimate partner rape was highest among bisexual women (22%) compared with heterosexual women (9%) [10]. A recent study confirmed these findings, with lesbian adolescents (ages 15–20 years) six times more likely and bisexual adolescent females three times more likely than heterosexual adolescents to have been forced by a man to have sexual intercourse [11]. Although these studies confirm that ARA is a concern for SMGs, they do not include girls who may not identify as lesbian or bisexual but have same-sex sexual contacts, thus missing a unique population at risk for ARA [12].
Similar to studies on ARA, only a handful of recent studies have considered the sexual and reproductive health of SMGs. One study documented that sex under the influence of alcohol or drugs, having multiple sex partners, and having unprotected vaginal sex with male partners were common among sexual minority adolescent and young adult women and associated with pregnancy and STIs. This study also found that sexual coercion was associated with greater sexual risk behavior [13]. However, experiences of sexual minority women were not compared with those of heterosexual women. One nationally representative study found that bisexual girls were more likely than heterosexual girls to have ever used emergency contraception and to have had a pregnancy termination [11]. Another study found that bisexual girls reported more pregnancy compared with their exclusively heterosexual counterparts, despite a greater likelihood of hormonal contraceptive use [14]. Although clinical settings serving adolescents are key sites for ARA prevention and intervention [15], little is known about the care-seeking patterns, risk profiles, and ARA experiences among SMGs who attend such clinics.
Despite the increasing attention in the literature to the health of SMGs, no studies of the sexual and reproductive health of these adolescents consider the role ARA may play in their sexual and reproductive risk and reason for seeking clinical care. Furthermore, studies comparing heterosexual and sexual minority youth are rarely comprehensive in their measurement of sexual minority status (i.e., including both sexual identity and sexual contacts). Finally, there are no studies of ARA among SMGs using school-based health centers (SBHCs), an important clinical setting given SBHCs, typically located in lower-income com munities of color, reach adolescents with numerous barriers to accessing confidential clinical care [16]. The purpose of the present study was to assess experiences of ARA and associations with sexual and reproductive health among a sexually active sample of adolescent females at SBHCs, to examine sexual behavior and sexual risk among SMGs, controlling for ARA, and to determine whether associations between ARA and outcomes differ by sexual minority status.
Methods
Data
Data were collected as part of a cluster randomized trial, “School Health Center Healthy Adolescent Relationships Program,” that evaluated a brief psychoeducational intervention in SBHCs to promote healthy relationships and reduce ARA. Eight SBHCs in Northern California were randomly assigned to the program or a wait-list control condition. Youth ages 14–19 years seeking services at one of the SBHCs were invited to participate (n = 1,012, 95% participation rate). Primary reasons for nonparticipation were lack of time and plans to move away from the area in the near future (because of the study’s longitudinal design).
Before program implementation, youth completed a 15-minute computer-based survey about ARA, sexual behavior, pregnancy risk, and care seeking for sexual and reproductive health. Students received a $10 gift card to thank them for their time. Study procedures were approved by Institutional Review Boards at the Public Health Institute, University of Pittsburgh, and participating school districts.
Measures
Primary predictors for the current analysis included sexual minority status and ARA. Sexual minority status was measured via two items assessing sexual identity and sexual behavior. Sexual identity was measured with the item, “Do you consider yourself: heterosexual/straight, bisexual, homosexual/gay/lesbian, or not sure?” Participants were also asked if they had ever had vaginal, oral, or anal sex, and if so, whether their partners since they started having sex were “women only,” “mostly women,” “equally men and women,” “mostly men,” and “men only.” A participant was classified as a sexual minority if they either identified as lesbian, bisexual, or questioning (i.e., not sure) OR reported having had same-sex sexual contacts. The reference category for this predictor included girls who identified as heterosexual AND had male sex partners only (i.e., “completely heterosexual”). Physical and sexual ARA was measured via three items modified from the Revised Conflict Tactics Scale [17] and the Sexual Experiences Survey [18] including, “In the past 3 months, has someone you going out with or hooking up with” (1) “ever hit, pushed, slapped, choked or otherwise physically hurt you? (including such things as being hit, slammed into something, or injured with an object or weapon),” and (2) “used force or threats to make you have sex (vaginal, oral, or anal sex) when you didn’t want to.” The third item read: “In the past 3 months, have you had sex with someone you were going out with or hooking up with when you did not want to, because you felt like you did not have a choice, even though they did not use physical force or threats?” Participants who endorsed at least one item were coded as having experienced ARA. Data on the perpetrators were not available.
Outcomes included sexual behavior, sexual risk, pregnancy risk, and care seeking for sexual and reproductive health. Three items assessed whether participants engaged in vaginal, oral, or anal sex in the past 3 months. Participants were also asked the number of sex (vaginal, oral, or anal sex) partners they had in the past 3 months (0 or 1 vs. 2 or more) and whether they recently had sex with a male partner ≥5 years older. Female participants were asked one item assessing recent contraceptive use; respondents who chose “I do not use anything to prevent pregnancy” were coded as contraceptive nonusers. Reproductive coercion was measured via a 10-item scale created by the investigative team and tested in previous clinic-based samples [5,9]. Finally, care seeking was determined by assessing participants’ reason for visit, including “STI testing or treatment” and “pregnancy test.” We collected demographic information on age, race and/or ethnicity, grade, and whether a participant was U.S. born. Publicly available data on the percent of students who received free lunch at each participating school were used as a proxy for socioeconomic status.
Analysis
The effective sample (n = 564) was restricted to girls who ever had vaginal, oral, or anal sex and had complete data on ARA (n = 4 missing), and sexual minority status (n = 1 missing). Our sample size precluded us from assessing differences among participants identifying as male (n = 240; 23 identified as sexual minority) or transgender (n = 1, one identified as sexual minority). Wald log-linear chi-square tests and linear regression models for clustered data were used to assess differences in sexual behavior, sexual risk, pregnancy risk, and care seeking for sexual and reproductive health by recent ARA and sexual minority status. Adjusted logistic regression models specified to account for clinic clustering were built to assess the relationships between ARA, sexual minority status, and outcomes. Models included sexual minority status, ARA, and covariates age, race and/or ethnicity, grade, whether participants were U.S. born, and percent free school lunch. For each outcome, an information- theoretic complexity-penalized model goodness-of-fit criterion for clustered survey data [19] was used to select between two models, one specified with main effects for the binary ARA and sexual minority status indicators, the other model specified to permit interaction among these two explanatory factors. Post hoc analyses were conducted to assess whether noted associations differed by sexual identity or sexual contacts (data not shown). Statistical analyses were conducted in SAS v9.3.
Results
Demographic characteristics
Demographic characteristics are presented in Table 1. Two- thirds of the sample (63.5%) were ages 16 and 17 years, whereas 25.9% were ages 14 and 15 years. Thirty-nine percent were in grade 12, whereas 11.2%, 19.7%, and 28.4% of participants were in grades 9,10, and 11, respectively. Most adolescent females identified as either Hispanic or Latina (36.9%) or African-American (29.1%) and 86.9% were born in the United States.
Table 1.
Demographic characteristics of the total sample and by sexual minority status (n = 564)
| Demographic | Total sample | Sexual minority | Completely |
|---|---|---|---|
| (n = 564), | adolescents | heterosexual | |
| n (%)a | (n = 130), | adolescents | |
| n (%)b | (n = 434), n(%)b | ||
| Age, years | |||
| 14–15 | 146 (25.9) | 51 (39.2) | 95 (21.9) |
| 16–17 | 358 (63.5) | 63 (48.5) | 295 (68.0) |
| 18–19 | 60 (10.6) | 16 (12.3) | 44 (10.1) |
| p value* | .0004 | ||
| Grade | |||
| 9th | 63 (11.2) | 31 (23.9) | 32 (7.4) |
| 10th | 111 (19.7) | 27 (20.8) | 84 (19.4) |
| 11th | 160 (28.4) | 29 (22.3) | 131 (30.2) |
| 12th | 219 (38.8) | 41 (31.5) | 178 (41.0) |
| p value* | .001 | ||
| Race/Ethnicity | |||
| Black or African- | 164 (29.1) | 40 (30.8) | 124 (28.6) |
| American | |||
| Hispanic or Latina | 208 (36.9) | 43 (33.1) | 165 (38.0) |
| Asian or other | 88 (15.6) | 14 (10.8) | 74 (17.1) |
| Multiracial | 50 (8.9) | 14 (10.8) | 36 (8.3) |
| American-Indian or | 26 (4.6) | 6 (4.6) | 20 (4.6) |
| Pacific Islander | |||
| White | 28 (5.0) | 13 (10.0) | 15 (3.5) |
| p value* | .10 | ||
| Born in the United | 490 (86.9) | 117 (90.0) | 376 (85.9) |
| States | |||
| p value* | .20 | ||
| Mean percent of | .15 (.54) | .14 (.53) | .15 (.54) |
| students eligible for | |||
| free lunch at school | |||
| [mean (standard | |||
| deviation)] | |||
| p value** | .32 |
Column percents.
Row percents.
p Values for categorical variables derived from Wald log-linear chi-square tests for clustered data. Significance set at p <.05.
p Values for continuous variables derived from linear regression models for clustered data. Significance set at p <.05.
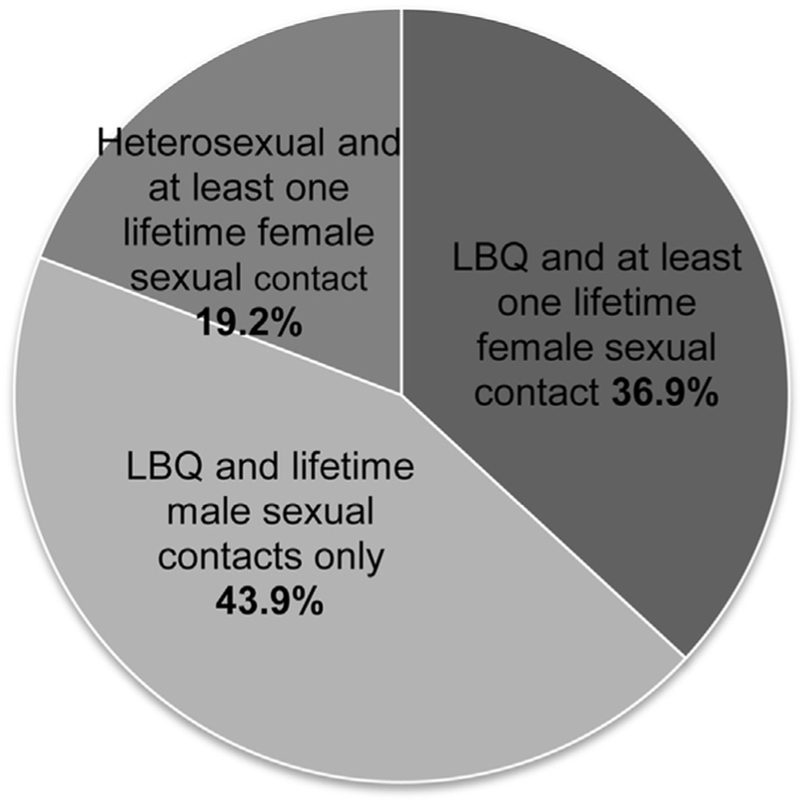
Twenty-three percent of the sample (n = 130) was coded as sexual minority (either identifying as lesbian, bisexual, or questioning or reporting female sex partners). Nineteen percent (n = 105) identified as lesbian, bisexual, or questioning (of which 77% identified as bisexual), whereas 13% (n = 73) reported any same-sex sexual contacts. Among SMGs, 37% identified as lesbian, bisexual, or questioning and had female sex partners, 44% identified as lesbian, bisexual, or questioning but had male sex partners only, and 19% identified as heterosexual but had female sex partners (Figure 1). Seventy-seven percent (n = 434) of the entire sample was “completely heterosexual” (i.e., they identified as heterosexual and had male sex partners only).
Figure 1.
Overlap of sexual identity and sexual contacts among sexual minority adolescent females (n = 130). LBQ represents adolescent girls who were identified as lesbian, bisexual, or questioning.
Differences in demographic characteristics by sexual minority status were found for age and grade with younger participants more likely than their older peers to either identify as lesbian, bisexual, or questioning or have had same-sex sexual contacts (Table 1).
Adolescent relationship abuse exposure, sexual minority status, and associations with sexual behavior, sexual and reproductive risk, and care seeking
In our sample of sexually active females, 17.7% reported experiencing recent ARA, with 21.5% and 16.6% of SMGs and completely heterosexual girls reporting this exposure, respectively. In bivariate analyses, girls reporting recent ARA were more likely to report recent oral sex (p =.002), two or more recent sex partners (p =.003), having a male sex partner ≥5 years older (p =.02), contraceptive nonuse (p =.05), and recent reproductive coercion (p =.001). SMGs were less likely to have had recent vaginal sex and were more likely to have had recent oral (p =.01) and anal sex (p =.02) and were more likely to be coming into the clinic for STI testing or treatment (Table 2).
Table 2.
Prevalence estimates of ARA and study outcomes (sexual behavior, sexual risk, pregnancy risk, and care seeking) among the total sample and by ARA and sexual minority status (n = 564)
| Total (n = 564), n (%) | Recent ARA | Sexual minority status | |||
|---|---|---|---|---|---|
| Recent ARA yes | Recent ARA no | Sexual minority females | Non–sexual minority females | ||
| (n = 100), n (%) | (n = 464), n (%) | (n = 130), n (%) | (n = 434), n (%) | ||
| Recent ARA | 100 (17.7) | — | — | 28 (21.5) | 72 (16.6) |
| Recent sexual behavior | |||||
| Vaginal sex | 483 (85.6) | 93 (93.0) | 390 (84.1) | 104 (80.0) | 379 (87.3)** |
| Oral sex | 314 (56.0) | 70 (70.0) | 244 (52.6)** | 88 (67.7) | 226 (52.1)* |
| Anal sex | 64 (11.4) | 16 (16.0) | 48 (10.3) | 21 (16.2) | 43 (9.9)* |
| Sexual risk | |||||
| Two + sex partners | 99 (17.6) | 26 (26.0) | 73 (15.7)***: | 27 (20.8) | 72(16.6) |
| Male sex partner ≥ 5 older | 41 (7.3) | 16 (16.0) | 25 (5.4)* | 11 (8.5) | 30 (6.9) |
| Pregnancy risk | |||||
| Contraceptive nonuse | 29 (5.1) | 9 (9.0) | 20 (4.3)* | 11 (8.5) | 18 (4.2) |
| Reproductive coercion | 70 (12.4) | 24 (24.0) | 46 (9.9)*** | 16 (12.3) | 54 (12.4) |
| Care seeking | |||||
| STI testing and/or treatment | 80 (14.2) | 20 (20.0) | 60 (12.9) | 27 (20.8) | 53 (12.2)** |
| Pregnancy test | 102 (18.1) | 23 (23.0) | 79 (17.0) | 22 (16.9) | 81 (18.4) |
p Values are derived from Wald log-linear chi-square tests.
ARA = adolescent relationship abuse; STI = sexually transmitted infection.
p <.05.
p <.01.
p <.001.
In models adjusting for demographics and sexual minority status, girls who experienced recent ARA were two times more likely to have recently engaged in oral sex (adjusted odds ratio [AOR], 2.22; 95% confidence interval [Cl], 1.61–3.05) and 1.8 times more likely than girls without exposure to ARA to have recently had anal sex (95% CI, 1.19–2.77). Girls who experienced recent ARA were also more than two times more likely to have multiple sex partners (AOR, 2.02; 95% CI, 1.56–2.61) and almost four times more likely to have recently had a male sex partner that was ≥5 years older (AOR, 3.62; 95% CI, 1.65–7.97). Finally, recent ARA was also associated with more than a two-fold increase and three-fold increase in the odds of contraceptive nonuse and reproductive coercion, respectively (contraceptive nonuse: AOR, 2.30; 95% CI, 1.07–4.95 and reproductive coercion: AOR, 3.32; 95% CI, 1.87–5.92).
Controlling for ARA and demographics, sexual minority status was associated with decreased odds of recent vaginal sex (AOR,.51; 95% CI,.35–.75) and increased odds of oral (AOR, 2.01; 95% Cl, 1.38–2.92) and anal sex (AOR, 1.76; 95% Cl, 1.26–2.46). The best-fit models for care-seeking outcomes included the interaction of ARA and sexual minority status. Heterosexual girls with recent ARA exposure (AOR, 2.85; 95% CI, 1.07–7.59) and SMGs without recent ARA exposure (AOR, 3.01; 95% CI, 2.01–4.50) were more likely than nonabused heterosexual girls to be seeking care for STI testing or treatment (Table 3).
Table 3.
Adjusted effects of ARA and SM status on study outcomes, from multiple logistic regression models for clustered survey data
| ARA, AOR (95% CI)a | SM status, AOR (95% CI)b | |||
| Sexual behavior | ||||
| Vaginal sex | 2.49 (.85–7.28) | .51 (.35–.75)*** | ||
| Oral sex | 2.22 (1.61–3.05)*** | 2.01 (1.38–2.92)*** | ||
| Anal sex | 1.81 (1.19–2.77)*** | 1.76 (1.26–2.46)** | ||
| Sexual risk | ||||
| Two + sex partners | 2.02 (1.56–2.61)*** | 1.43 (.89–2.29) | ||
| Male sex partner ≥ 5 older | 3.62 (1.65–7.97)** | 1.15 (.48–2.78) | ||
| Pregnancy risk | ||||
| Contraceptive nonuse | 2.30 (1.07–4.95)* | 1.82 (.97–3.43) | ||
| Reproductive coercion | 3.32 (1.87–5.92)*** | 1.18 (.62–2.25) | ||
| Heterosexual girls with exposure | Heterosexual girls without | SM girls with exposure to | SM girls without ARA | |
| to ARA, AOR (95% CI) | exposure to ARA, AOR (95% CI) | ARA, AOR (95% CI) | exposure, AOR (95% CI) | |
| Care seeking | ||||
| STI testing or treatment | 2.85 (1.07–7.59)* | ref | 1.25 (.48–3.24) | 3.01 (2.01–4.50)* |
| Pregnancy testing | 1.28 (.65–2.52) | ref | 1.48 (.65–3.35) | .76 (.27–2.16) |
AOR from logistic regression models with statistical adjustment for age, race, grade, whether participants were U.S. born, and percent free school lunch as a proxy of socioeconomic status. For each outcome, an information-theoretic complexity-penalized model goodness-of-fit criterion for clustered survey data was used to select between two models, one specified with only main effects for the binary ARA and sexual minority status indicators (results in top half of table), the other model specified to permit effect modification (interaction) among these two explanatory factors (results in bottom half of table). For the “interaction” models, AOR for combinations of ARA and sexual minority status are reported with respect to the reference category of heterosexual girls without exposure to ARA.
AOR = adjusted odds ratio; ARA = adolescent relationship abuse; CI = confidence interval; SM, sexual minority; STI, sexually transmitted infection.
Additionally adjusted for sexual minority status.
Additionally adjusted for ARA.
p <.05.
p <.01.
p <.001.
Differences in associations of sexual minority status and study outcomes by sexual identity and sexual contacts
Post hoc analyses indicated that when sexual identity and sexual contacts were examined separately, girls who had same-sex sexual contacts were significantly more likely than those with exclusively male sexual contacts to report recent ARA (26% vs. 17%, p =.04). Meanwhile, girls who identified as lesbian, bisexual, or questioning were significantly more likely to not be using a method of contraception (including condom use) (AOR, 2.61; 95% CI, 1.31–5.19) compared with girls who identified as heterosexual.
Discussion
These findings indicate that recent ARA is common among sexually active girls seeking care at SBHCs. More than 21% (21.5%) of SMGs experienced recent ARA, compared with 16.6% of completely heterosexual girls. Post hoc analyses revealed that the prevalence of ARA was higher among SMGs whether we compared youth by sexual identity OR sexual contacts. However, statistically significant differences were only noted between girls with same-sex sexual contacts compared with girls with male sexual contacts only (26% vs. 17%, p =.04). Although these findings suggest that girls with both male and female sexual contacts may be at elevated risk for relationship abuse, we do not know the contexts in which these adolescents are experiencing abuse (including perpetrator characteristics). Moreover, further research is needed to understand whether unique risk factors and coercive tactics (e.g., gay-related victimization, threats of “outing”) influence SMG’s risk for ARA and whether this operates differently for girls who identify as lesbian or bisexual versus those who have relationships with the same-sex partners.
Importantly, girls who experienced recent ARA were more likely to report multiple and older sex partners, recent reproductive coercion, and were less likely to be using a method of contraception. Although previous studies have found girls with a history of ARA to engage in riskier sexual behavior than those without histories of abuse [20,21], this study points to the concurrence of ARA and sexual and/or pregnancy risk among sexually active adolescent girls. Clinicians working in SBHCs are in a unique position to talk to adolescent girls about healthy relationships and the links between ARA and the reason they are coming into the clinic. Moreover, SBHCs offer a unique and vital setting for this work as adolescents can access confidential sexual and reproductive health care with clinical appointments featuring a strong emphasis on targeted health education [2 2].
In addition to documenting the prevalence of recent ARA, we sought to understand the experiences of SMGs, including their own histories of abuse and related sexual and reproductive health, in this SBHC sample. Almost one quarter of sexually active girls reported either identifying as lesbian, bisexual, or questioning or having ever had a female sex partner, which is notably higher than the proportion of sexual minority youth in other surveys conducted in school settings [23,24]. Given evidence that SBHCs provide confidential health care, girls may have felt more comfortable disclosing their sexual minority status than they would in another clinic-based or classroom setting. We also know that women and girls who experience relationship abuse disproportionately access sexual and reproductive health services [7,25], and this care-seeking pattern may extend to girls in the SBHC setting. Confirming findings from previous work, sexual identity and sexual behavior did not overlap perfectly in this sample [12]. A number of girls identifying as heterosexual in the sample reported having female sexual partners, and lesbian or bisexually identified girls reported various combinations of male and female sexual partners. These findings suggest that clinicians should ask both about sexual identity and sexual contacts as identity and behavior may not coincide.
Until recently, research has not focused on the sexual and reproductive health of sexual minority women and girls, which has resulted in the perception clinically that SMGs are at lower risk for STIs and unintended pregnancy [26]. However, in one recent study, adolescent girls who identified as lesbian or bisexual reported a greater number of male sexual partners in their lifetime compared with heterosexual girls, indicating that they are, indeed, at risk for these outcomes [11]. Particularly notable in the present study was the greater likelihood of anal sex among SMGs compared with heterosexual girls. While recent work has found that adolescent and young adult women who have experienced partner violence are more likely to engage in unprotected anal sex [7], our findings from models controlling for ARA suggest there may be unique factors in the social contexts of sexual minority girls beyond coercive behavior characteristics of ARA that increase the likelihood for anal sex. Drawing on the minority stress framework, one potential hypothesis is that SMGs may feel pressure to conform to heteronormative behavior and thus engage in riskier sexual behavior, such as unprotected anal sex, with male partners. Alternatively, SMGs may feel more com for table exploring their sexuality, contributing to these findings. In this sample, heterosexual girls with recent abuse exposure and SMGs without exposure to abuse were more likely to be seeking care for STI testing or treatment, underscoring the need for comprehensive clinical services for adolescent girls, regardless of their sexual identity or the sex category of their current sexual partner, and careful assessment for ARA during these clinical visits. Contrary to what we hypothesized, SMGs with recent ARA were not more likely to be seeking care for STI testing or treatment compared with heterosexual girls without recent abuse exposure, and further research on the contexts in which SMGs experience abuse and how this impacts their care-seeking behavior is needed.
In post hoc analyses, which used sexual identity and sexual contacts as separate predictors, we found that girls identifying as lesbian, bisexual, or questioning were less likely than those identifying as heterosexual to use any form of contraception. In light of the substantial number of girls in our sample who identify as lesbian or bisexual but engage in heterosexual intercourse, contraceptive counseling should remain an option for all girls seeking care at SBHCs, guided by conversations with youth about sexual identity, attraction, and behavior.
These findings should be interpreted in light of several limitations. First, these analyses are cross sectional thus associations are not causal and the temporality of exposures and outcomes of interest cannot be confirmed. However, the measures used in this study capture sexual behavior and exposure to ARA within the past 3 months, which strengthens the temporal proximity of ARA exposure and sexual risk behavior. Another limitation was our inability to understand how these associations would appear among male or transgender populations, given the small sample of boys and transgender youth in our sample. We also combined girls identifying as lesbian, bisexual, and questioning in response to our sample size, which precludes us from understanding how ARA and the sexual and reproductive health differ for these unique groups of adolescent girls. Similar to the limited work on ARA among sexual minority youth, data are not available regarding the perpetrators and the context in which sexual minority youth experience ARA or the sex category of partners with which girls are having oral or anal sex. Future work includes qualitative research with SMGs to further elucidate these critically important missing pieces. Finally, findings from this nonrepresentative sample from eight SBHCs in one Northern California region cannot be generalized to all high school students, to adolescents who receive care in other clinical settings, or vulnerable youth who may not access care. However, this study has several important strengths including limited missing data and the racial and/or ethnic diversity (95% of respondents were non-white), which is important given most studies on sexual minority women are conducted in primarily white samples. Adolescent girls of color are at increased risk for ARA regardless of their sexuality [27], and SMGs of color are at elevated risk of poor sexual and reproductive health driven by their disadvantaged social position in relation to sexuality, race and/or ethnicity, and socioeconomic status [28]. Therefore, this study may inform intervention strategies to reduce ARA and poor sexual and reproductive health for this vulnerable population.
Our findings suggest the need for attention to STI risk and contraceptive nonuse among SMGs and education for clinicians about sexual behavior and STIs among lesbian and bisexual girls or girls who identify as heterosexual but engage in sex with female partners. Youth seeking STI care should be carefully assessed for sexual attraction and contacts in addition to sexual identity. Given the clear link between ARA and poor sexual and reproductive health behaviors, counseling should also include discussion of healthy relationships, consensual sex, and risks associated with high risk sexual behavior, unprotected anal sex, in particular.
IMPLICATIONS AND CONTRIBUTION.
This study assesses sexual minority and heterosexual adolescent girls’ experiences of relationship abuse and poor sexual and reproductive health. Findings highlight the need for clinicians to ask about both sexual identity and behavior among youth and provide comprehensive testing and treatment for sexually transmitted infections framed within a discussion of healthy relationships.
Acknowledgments
The study sponsors had no influence on study design, data collection, analysis, interpretation, article preparation, or decision to submit for publication. This study was presented orally at the 2014 Society for Adolescent Health and Medicine annual meeting in Austin, TX.
Funding Sources
The parent study was funded by the National Institute of Justice (grant number: 2011-MU-MU-0023). Findings presented here were supported by a Health Resources and Services Administration National Research Service Award for Primary Care to University of Pittsburgh (T32HP22240).
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to report.
References
- [1].Exner-Cortens D, Eckenrode J, Rothman E Longitudinal associations between teen dating violence victimization and adverse health outcomes. Pediatrics 2013;131:71–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Haynie DL, Farhat T, Brooks-Russell A, et al. Dating violence perpetration and victimization among U.S. adolescents: Prevalence, patterns, and associations with health complaints and substance use. J Adolesc Health 2013; 53:194–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Silverman JG, McCauley HL, Decker MR, et al. Coercive forms of sexual risk and associated violence perpetrated by male partners of female adolescents. Perspect Sex Reprod Health 2011;43:60–5. [DOI] [PubMed] [Google Scholar]
- [4].Silverman JG, Raj A, Mucci LA, et al. Dating violence against adolescent girls and associated substance use, unhealthy weight control, sexual risk behavior, pregnancy, and suicidality. JAMA 2001;286:572–9. [DOI] [PubMed] [Google Scholar]
- [5].Miller E, Decker MR, McCauley HL, et al. Pregnancy coercion, intimate partner violence and unintended pregnancy. Contraception 2010;81:316–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Miller E, Levenson RR, Herrera L, et al. Exposure to partner, family, and community violence: Gang-affiliated Latina women and risk of unintended pregnancy. J Urban Health 2012;89:74–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Decker MR, Miller E, McCauley HL, et al. Recent partner violence and sexual and drug-related STI/HIV risk among adolescent and young adult women attending family planning clinics. Sex Transm Infect 2013;90:145–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Hess KL, Javanbakht M, Brown JM, et al. Intimate partner violence and sexually transmitted infections among young adult women. Sex Transm Dis 2012;39:366–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Miller E, McCauley HL, Tancredi DJ, et al. Recent reproductive coercion and unintended pregnancy among female family planning clients. Contraception 2014;89:122–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Walters ML, Chen J, Breiding MJ The national intimate partner and sexual violence survey (NISVS): 2010 findings on victimization by sexual orientation. Atlanta, GA: National Center for Injury Prevention and Control, Centers for Disease Control and Prevention; 2013. [Google Scholar]
- [11].Tornello SL, Riskind RG, Patterson CJ Sexual orientation and sexual and reproductive health among adolescent young women in the United States. J Adolesc Health 2014;54:160–8. [DOI] [PubMed] [Google Scholar]
- [12].Saewyc E, Bauer GR, Skay CL, et al. Measuring sexual orientation in adolescent health surveys: Evaluation of eight school-based surveys. J Adolesc Health 2004;35:345. [DOI] [PubMed] [Google Scholar]
- [13].Herrick A, Kuhns L, Kinsky S, et al. Demographic, psychosocial, and contextual factors associated with sexual risk behaviors among young sexual minority women. J Am Psychiatr Nurses Assoc 2013;19:345–55. [DOI] [PubMed] [Google Scholar]
- [14].Charlton BM, Corliss HL, Missmer SA, et al. Sexual orientation differences in teen pregnancy and hormonal contraceptive use: An examination across 2 generations. Am J Obstet Gynecol 2013;209:204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Miller E, Levenson RR Hanging out or hooking up: Clinical guidelines on responding to adolescent relationship abuse. San Francisco, CA: Futures Without Violence; 2013. [Google Scholar]
- [16].Allison MA, Crane LA, Beaty BL, et al. School-based health centers: Improving access and quality of care for low-income adolescents. Pediatrics 2007;120:e887–94. [DOI] [PubMed] [Google Scholar]
- [17].Straus MA, Hamby SL, Boney-McCoy S, et al. The revised conflict tactics scale: Development and preliminary psychometric data. J Family Issues 1996;171:283–316. [Google Scholar]
- [18].Koss MP, Gidycz CA Sexual experiences survey: Reliability and validity. J Consult Clin Psychol 1985;531:422–3. [DOI] [PubMed] [Google Scholar]
- [19].Pan W Akaike’s information criterion in generalized estimating equations. Biometrics 2001;57:120–5. [DOI] [PubMed] [Google Scholar]
- [20].Silverman JG, Raj A, Clements K Datingviolence and associated sexual risk and pregnancy among adolescent girls in the United States. Pediatrics 2004;114:e220–5. [DOI] [PubMed] [Google Scholar]
- [21].Wingood GM, DiClemente RJ, McCree DH, et al. Dating violence and the sexual health of black adolescent females. Pediatrics 2001;107:e72. [DOI] [PubMed] [Google Scholar]
- [22].Fothergill K, Feijoo A Family planning services at school-based health centers: Findings from a national survey.J Adolesc Health 2000;27:166–9. [DOI] [PubMed] [Google Scholar]
- [23].Martin-Storey A Prevalence ofdatingviolence among sexual minorityyouth: Variation across gender, sexual minority identity and gender of sexual partners [published online ahead of printJanuary 10,2014].JYouth Adolesc [Google Scholar]
- [24].Mustanski B, Van Wagenen A, Birkett M, et al. Identifying sexual orientation health disparities in adolescents: Analysis of pooled data from the youth risk behavior survey, 2005 and 2007. Am J Public Health 2014;104: 211–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Miller E, Decker MR, Raj A, et al. Intimate partner violence and health care-seeking patterns among female users of urban adolescent clinics. Matern Child Health J 2010;14:910–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Levine DA Committee on adolescence. Office-Based care for lesbian, gay, bisexual, transgender, andquestioningyouth.Pediatrics 2013;132:e297–313. [DOI] [PubMed] [Google Scholar]
- [27].Rothman EF, Xuan Z Trends in physical dating violence victimization among U.S. high school students, 1999–2011.JSch Violence 2013;13:277–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Ferguson AD, Carr G, Snitman A Intersections of race-ethnicity, gender and sexual minority communities In: Miville ML, Ferguson AD, eds. Handbook of race-ethnicity and gender in psychology. New York, NY: Springer; 2014. [Google Scholar]