Abstract
Objective:
Chronic positive energy balance leads to obesity and the “excess” weight is usually described as consisting solely of adipose tissue (AT) or its two components, fat and fat-free mass (non-fat cell mass, extracellular fluid). This study aimed to clarify the nature of “obesity” tissue.
Methods:
333 adults had AT, skin, skeletal muscle, bone, heart, liver, kidneys, spleen, brain, and residual mass measured/derived using MRI-DXA. First, associations between these components and AT were examined by developing multiple regression models. Next, obesity tissue composition was developed by deriving mean component mass differences between participant groups who were normal-weight (BMI, <25 kg/m2) and those who were obese (>29.9 kg/m2); respective resting energy expenditures (REE) and metabolizable energy/protein contents were calculated.
Results:
AT significantly predicted organ-tissue mass in 17 of 18 multiple regression models. In addition to AT and skeletal muscle, skin, liver, and bone were main contributors to obesity tissue composition; liver, kidneys, and heart to REE; and skin, liver, and bone to metabolizable energy/protein contents. A pronounced sexual dimorphism was present in all three models.
Conclusions:
Obesity is characterized not only by excess AT, but by increases in the masses of other “companion” organs and tissues and their related metabolic properties.
Keywords: Body Fat, Excess Body Weight, Metabolism, Energy Expenditure, Obesity
INTRODUCTION
Obesity develops as the result of long term positive energy balance with accumulation of excess adipose tissue and its stored fat, mainly triglycerides (1–3). The increase in body mass is variously referred to as “excess body weight” (4), “adiposity tissue” (5) and “obesity tissue” (6, 7). Even though this compartment is a sizable portion of adult body mass at a global level, lack of clarity surrounds its detailed composition, energy expenditure, and metabolizable energy content. This information is important when studying the pathophysiology of obesity (1, 2) and when developing body composition-energy expenditure models (8–10).
Keys and Brozek in 1953 (7) and later Brozek et al. in 1963 (6) were among the first to develop detailed “obesity tissue” models by quantifying the difference in measured body density (Db) between an average “normal young man” and that of a group of men with higher levels of adiposity and with weight gains and losses. Using the two-component Db body composition model that partitions body mass into fat and fat-free mass (FFM), the authors and their colleagues in 1963 estimated that obesity tissue is 64% fat, 32% “cell residue”, and 4% extracellular water, the latter two components comprising FFM (6). Brozek et al. (6) considered obesity tissue similar to but not identical to adipose tissue, a view held widely at the time. Forbes and Welle in 1983 (11) largely replicated Keys and Brozek’s observation that obesity tissue, as we will refer to it, consists of both fat and “lean body mass (LBM)” components. Using the two-component total body potassium body composition model, Forbes and Welle reported that adolescents and adults who were overweight or obese had an excess body weight consisting of 71% fat and 29% LBM (11). Lean body mass, as defined by the authors, is a compartment devoid of stored triglyceride or “fat” and is analogous to FFM.
The adipose tissue-centric model of excess body weight began to change with the study of Webster et al. in 1984 (12) who used three separate two-component models based on measured Db, total body potassium, and total body water to estimate the mean composition of “excess” body weight as 78% fat and 22% FFM in a sample of women ranging widely in adiposity. Webster et al., in a careful analysis, compared the composition of “excess weight” to that of adipose tissue and concluded that “other types of lean tissue must also be involved” (12). Support for their speculation comes from a little discussed comment by Pitts in a 1962 paper (13, 14) devoted to the development of body composition models in hamsters. Pitts hypothesized that a “dynamic mechanism” operates to maintain the proportions of major organs and tissues stable in relation to changes in fat mass as an “independent variable” (14). Alterations in fat (or adipose tissue) mass, according to Pitts, places metabolic and mechanical demands on non-fat organs that then respond with adjustments in their functional outputs and anatomic body sizes. In support of Pitts’s theory, the resting energy expenditure (REE) of excess body weight is much larger than can be explained solely by adipose tissue, a low metabolic rate component (~4 kcal/kg/d) (15). Reference Man (age 25 yrs, height 1.7 m), for example, gaining weight from 70 kg to 100 kg is predicted to increase his REE by about 400 kcal/d (16), far more (by ~280 kcal) than if the extra 30 kg in body weight consisted only of adipose tissue. The higher than expected REE based solely on an increase in adipose tissue mass may stem from enlargement of high metabolic rate organs such as the heart and kidney (i.e., ~440 kcal/kg/d) (15).
A critical analysis of obesity tissue composition, beyond that provided by the one (i.e., adipose tissue) and two-component (i.e., fat mass and FFM) models, is needed to reconcile disparate or incomplete views of what constitutes “excess body weight”. The aim of the current study was to fill this gap by examining in detail the cross-sectional organ and tissue composition of obesity tissue and relating its contents to REE and metabolically available energy stores.
METHODS
Study Aims and Design
Three specific related questions were evaluated in the current study: What is the organ-tissue composition of obesity tissue? What is the REE of this compartment? How much metabolizable energy and protein are available from this compartment? These three questions were examined by evaluating the organ and tissue composition of a healthy Caucasian adult (≥18 yrs) sample varying widely in body mass index (BMI). As an initial exploratory step, sex-specific multiple regression models were developed to test the hypothesis that adipose tissue mass is significantly positively associated with the masses of the other major organ-tissue components after controlling for height and age, two potential model covariates.
Following this proof-of-concept phase, the next series of analyses specifically examined the posed questions by dividing the evaluated sample into three BMI groups, normal weight (<25 kg/m2), overweight (25 kg/m2 to 29.9 kg/m2), and obese (>29.9 kg/m2). We then defined obesity tissue, as did Brozek et al. (6), as the mean difference in organ-tissue mass present between the groups who were obese and normal weight. Lastly, we derived the REE and metabolizable energy and protein content of obesity tissue from the organ-tissue composition of this body compartment.
Obesity Tissue Estimates
Composition.
The volumes of total body adipose tissue, skeletal muscle, heart, liver, kidney, spleen, and brain were measured with magnetic resonance imaging (MRI) (17). The mass of each organ and tissue was derived from the respective volumes and densities using previously reported component densities (Table S1) (15). Skin mass was calculated using a model based on body surface area and skin thickness as established in earlier cadaver and ultrasound studies (Table S1) (18). Bone mineral content was quantified with dual-energy X-ray absorptiometry (DXA) and converted to bone mass as previously reported (Table S1) (18). Residual mass was derived as the difference between body mass and the sum of the other nine organ-tissue component masses.
Resting Energy Expenditure.
The second question, the REE of obesity tissue, was evaluated by taking the product of each organ-tissue component mass and its estimated mass-specific REE as previously reported (Table S1) (18). The total REE for obesity tissue mass was then calculated as the sum of the ten organ-tissue heat production rates and is expressed in kcal/d and kcal/g.
Metabolizable Energy Content.
The third question was examined by estimating the fat, protein, and carbohydrate content of each organ and tissue and then deriving the respective component’s metabolizable energy and protein content. Organ and tissue fat, protein, and carbohydrate (i.e., glycogen) values were from those reported for Reference Man (19). The metabolizable energy values for each of the ten organs and tissues was then summed and expressed as total kcal and kcal/kg for the obesity tissue.
Study Participants
Participants were healthy volunteers in previously reported studies at the Institute of Human Nutrition and Food Science at the University of Kiel, Germany (20, 21). The study was approved by the university’s Institutional Review Board and all participants signed an informed consent prior to participation.
Body Composition
Participant height was measured without shoes to the nearest 0.5 cm using a Seca stadiometer (Hamburg, Germany). Body weight was measured to the nearest 0.01 kg using a Tanita (Tokyo, Japan) digital scale. The volumes of total adipose tissue, skeletal muscle, heart, liver, kidneys, spleen, and brain were measured using a 1.5 T Magnetom Vision or Avanto Siemens magnetic resonance imaging scanner (Siemens Medical Systems, Erlangen, Germany) as previously reported (17, 20, 22). The cross-sectional images were segmented using SliceOmatic software (version 4.3, Tomovision, Montreal, Canada) by a trained staff member. The measurement technical errors for the same scan on two separate days were (mean±SD) 0.7± 0.1% and 1.1±1.2% for skeletal muscle and adipose tissue, respectively. The magnetic resonance imaging protocol is presented in detail in Supplementary Information. Some subjects did not have measurements of spleen mass. Regression models predicting spleen and residual mass were therefore developed on the smaller sample with complete data.
Bone mineral content was measured using a Hologic (Marlborough, Massachusetts) QDR 4500A DXA system with software version V8.26a:3. Bone mineral content was converted to bone mass (Table S1). The short-term precision of DXA bone mineral, lean soft tissue (i.e., FFM – bone mineral), and fat mass estimates are 1.2%, 0.7%, and 1.9%, respectively (23). During the study analysis phase it became clear that a larger sample was needed to clarify our initial bone mineral content observations. The sample evaluated was from the National Health and Nutrition Survey (NHANES) that included 4406 and 4235 non-Hispanic white men and women, respectively (24). The details of these analyses are presented in Results and in Table S2.
Statistical Methods
All statistical evaluations were conducted in JMP (SAS Institute Inc., Cary, NC) with demographic and other baseline results presented as the mean±standard deviation. Between-sex differences in body composition were tested for significance using unpaired t-tests with p<0.05 considered statistically significant.
Multiple regression models were developed to test the hypothesis that significant positive associations are present between adipose tissue mass and the other organ-tissue mass components, after controlling for height and age. All of the regression model variables were normally distributed and model interaction terms were non-significant.
Differences in mass between the groups who were obese and normal weight were calculated for the ten organ and tissue components separately for men and women, thus defining the sex-specific composition of obesity tissue. The normal weight groups had mean BMIs in the range of 22-23 kg/m2, approximately that of the classical Reference Man and Woman (19). The groups with obesity had mean weights of about 100-105 kg and BMIs of 33-35 kg/m2, those typically found in clinical trials of participants who are obese. Men and women in the groups with obesity had non-significantly different average heights and ages compared to their counterparts whose weights were in the normal range. The results of these analyses are presented in a table as the group mean values at each BMI level and as the differences between the groups who were obese and normal weight; the corresponding means and standard errors are presented in a figure along with between-group statistical comparisons using the Tukey method (25). The organ and tissue composition of obesity tissue was then used to derive values for REE and metabolizable energy and protein content.
RESULTS
Participants
The study sample characteristics are summarized in Table 1. There were 163 men and 170 women with an overall mean age of about 43 years (range, 19-80 yrs) and a BMI of about 27 kg/m2 (16.8-45.0 kg/m2). Women had a significantly higher BMI (p<0.05) and more adipose tissue and less skeletal muscle, bone, heart, liver, kidneys, spleen, brain, and residual mass compared to the men (all p<0.001). The subset of participants with spleen mass included 108 men and 147 women. The groups who were normal-weight, overweight, and obese included, respectively 32, 50, and 26 men and 61, 36, and 50 women.
Table 1.
Subject Characteristics.
| All Participants | BMI < 25 | BMI 25-29.9 | BMI > 29.9 | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Men | Women | Total | Men | Women | Men | Women | Men | Women | |
| N | 163 | 170 | 333 | 32 | 61 | 50 | 36 | 26 | 50 |
| Age (yrs) | 43.4 ± 17.2 | 41.9 ± 15.9 | 42.6 ± 16.5 | 43.1 ± 16.2 | 38.6 ± 15.1 | 46.8 ± 14.8 | 45.0 ± 13.7 | 44.8 ± 11.7 | 34.9 ± 8.7 |
| Height (cm) ‡ | 179.4 ± 6.4 | 167.4 ± 7.0 | 173.1± 8.9 | 176.5 ± 5.8 | 167.9 ± 6.4 | 179.6 ± 6.4 | 168.1 ± 5.7 | 178.3 ± 6.2 | 168.5 ± 7.5 |
| BMI (kg/m2)* | 26.3 ± 4.0 | 28.1 ± 6.4 | 27.2 ± 5.5 | 22.9 ± 1.4 | 22.4 ± 2.05 | 27.4 ± 1.7 | 27.3 ± 1.63 | 32.9 ± 2.4 | 35.5 ± 3.6 |
| Body Composition (kg) | |||||||||
| AT‡ | 19.3 ± 7.5 | 29.6 ± 13.5 | 24.6 ± 12.1 | 14.5 ± 3.1 | 19.1 ± 5.09 | 22.2 ± 4.8 | 27.8 ± 4.0 | 30.6 ± 4.8 | 44.7 ± 8.9 |
| Skin‡ | 4.20 ± 0.34 | 3.89 ± 0.49 | 4.04 ± 0.45 | 3.88 ± 0.20 | 3.55 ± 0.24 | 4.31 ± 0.24 | 3.89 ± 0.24 | 4.62 ± 0.26 | 4.38 ± 0.42 |
| SM‡ | 30.6 ± 5.2 | 21.3 ± 4.3 | 25.8 ± 6.6 | 27.4 ± 3.5 | 19.4 ± 2.83 | 31.6 ± 3.4 | 21.7 ± 3.3 | 36.9 ± 5.8 | 24.7 ± 3.9 |
| Bone‡ | 4.95 ± 0.44 | 4.00 ± 0.53 | 4.46 ± 0.68 | 4.72 ± 0.37 | 3.91 ± 0.40 | 5.01 ± 0.45 | 3.97 ± 0.40 | 5.10 ± 0.40 | 4.35 ± 0.47 |
| Heart‡ | 0.33 ± 0.09 | 0.28 ± 0.07 | 0.31 ± 0.08 | 0.33 ± 0.07 | 0.25 ± 0.05 | 0.37 ± 0.07 | 0.29 ± 0.07 | 0.33 ± 0.08 | 0.32 ± 0.07 |
| Liver‡ | 1.68 ± 0.33 | 1.50 ± 0.33 | 1.59 ± 0.34 | 1.46 ± 0.22 | 1.34 ± 0.21 | 1.82 ± 0.25 | 1.50 ± 0.18 | 2.05 ± 0.32 | 1.77 ± 0.31 |
| Kidneys‡ | 0.30 ± 0.07 | 0.27 ± 0.07 | 0.28 ± 0.07 | 0.28 ± 0.05 | 0.24 ± 0.05 | 0.35 ± 0.05 | 0.26 ± 0.05 | 0.35 ± 0.05 | 0.34 ± 0.07 |
| Spleen‡ | 0.30 ± 0.13 | 0.22 ± 0.10 | 0.25 ± 0.12 | 0.23 ± 0.08 | 0.18 ± 0.06 | 0.33 ± 0.12 | 0.21 ± 0.07 | 0.37 ± 0.12 | 0.29 ± 0.11 |
| Brain‡ | 1.60 ± 0.12 | 1.43 ± 0.11 | 1.51 ± 0.14 | 1.57 ± 0.10 | 1.44 ± 0.11 | 1.60 ± 0.10 | 1.43 ± 0.10 | 1.69 ± 0.12 | 1.46 ± 0.09 |
| Residual‡ | 21.2 ± 4.2 | 16.8 ± 4.2 | 19.0 ± 4.8 | 17.0 ± 3.2 | 13.8 ± 2.83 | 20.7 ± 3.7 | 16.2 ± 2.78 | 22.8 ± 3.9 | 19.0 ± 4.7 |
<0.05;
<0.001 for men vs. women. AT, adipose tissue; BMI, body mass index, kg/m2. are presented as X±SD.
Associations between Adipose Tissue and Other Organs and Tissues
The developed organ-tissue multiple regression models are presented in Table 2 separately for men and women. Each component model includes adipose tissue mass, age, and height as potential covariates. The regression models for bone mass developed on the Kiel sample were significant in men (p<0.01) and non-significant in women. To clarify the relationships between adipose tissue and bone mass, we developed corresponding multiple regression models using the NHANES database values for DXA-derived fat mass and bone mineral content (Table S2). These values were adjusted to adipose tissue and bone mass as outlined in Table S2. Adipose tissue mass was a significant predictor of bone mass, after controlling for age and height, in both men and women NHANES participants.
Table 2.
Organ-Tissue Composition Multiple Regression Models.
| Component | Adipose Tissue | Age | Height | Intercept | R2 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Men | β | 95% CI | SE | β | 95% CI | SE | β | 95% CI | SE | β | 95% CI | SE | |
| Skin | 0.03‡ | 0.03, 0.04 | 0.001 | −0.0002 | −0.001, 0.001 | 0.0007 | 0.03‡ | 0.02, 0.03 | 0.002 | −1.51‡ | −2.14, −0.88 | 0.32 | 0.85‡ |
| SM | 0.37‡ | 0.29, 0.45 | 0.04 | −0.11‡ | −0.15, −0.07 | 0.02 | 0.22‡ | 0.13, 0.32 | 0.05 | −11.6 | −29.4, 6.28 | 9.04 | 0.48‡ |
| Bone1 | 0.02‡ | 0.02, 0.02 | 0.0007 | −0.006‡ | −0.007, −0.005 | 0.0005 | 0.06‡ | 0.06, 0.06 | 0.001 | −5.59‡ | −6.06, −5.12 | 0.24 | 0.45‡ |
| Heart | 0.003* | 0.001, 0.004 | 0.0009 | 0.002‡ | 0.001, 0.003 | 0.0004 | 0.001 | −0.001, 0.003 | 0.001 | 0.03 | −0.35, 0.41 | 0.19 | 0.19‡ |
| Liver | 0.03‡ | 0.02, 0.03 | 0.003 | −0.003* | −0.005, −0.0001 | 0.001 | 0.007* | 0.0002, 0.01 | 0.003 | 0.03 | −1.17, 1.23 | 0.61 | 0.43‡ |
| Kidneys | 0.005‡ | 0.004, 0.006 | 0.0006 | 0.0003 | −0.0002, 0.001 | 0.0003 | −0.0001 | −0.002, 0.001 | 0.001 | 0.21 | −0.05, 0.47 | 0.13 | 0.34‡ |
| Spleen | 0.006† | 0.003, 0.01 | 0.002 | −0.002 | −0.003, 1.66E-5 | 0.0008 | −0.003 | −0.007, 0.001 | 0.002 | 0.73‡ | 0.04, 1.42 | 0.35 | 0.12‡ |
| Brain | 0.005† | 0.002, 0.007 | 0.001 | −0.0003 | −0.001, 0.001 | 0.0006 | 0.004* | 0.001, 0.007 | 0.001 | 0.78* | 0.24, 1.33 | 0.28 | 0.12‡ |
| Residual | 0.13* | 0.02, 0.23 | 0.05 | 0.06* | 0.01, 0.11 | 0.03 | 0.22† | 0.10, 0.35 | 0.06 | −25.2* | −47.6, −2.67 | 11.3 | 0.19‡ |
| Women | |||||||||||||
| Skin | 0.03‡ | 0.03, 0.03 | 0.0006 | 0.0007 | −0.0004, 0.002 | 0.0005 | 0.03‡ | 0.02, 0.03 | 0.001 | −1.49‡ | −1.90, −1.08 | 0.21 | 0.96‡ |
| SM | 0.16‡ | 0.13, 0.19 | 0.01 | −0.05‡ | −0.08, −0.03 | 0.01 | 0.25‡ | 0.19, 0.30 | 0.03 | −22.8‡ | −32.4, −13.1 | 4.89 | 0.71‡ |
| Bone1 | 0.01‡ | 0.01, 0.02 | 0.0005 | −0.01‡ | −0.01, −0.01 | 0.0004 | 0.05‡ | 0.04, 0.05 | 0.001 | −3.57‡ | −3.94, −3.20 | 0.19 | 0.55‡ |
| Heart | 0.001† | 0.001, 0.002 | 0.0004 | 0.0003 | −0.0004, 0.001 | 0.0004 | 0.002* | 0.001, 0.004 | 0.001 | −0.14 | −0.42, 0.14 | 0.14 | 0.12‡ |
| Liver | 0.03‡ | 0.01, 0.02 | 0.001 | −0.002 | −0.004, 0.0005 | 0.001 | 0.01‡ | 0.010, 0.02 | 0.003 | −1.32* | −2.21, −0.44 | 0.45 | 0.58‡ |
| Kidneys | 0.003‡ | 0.002, 0.003 | 0.0003 | −0.0006 | −0.001, 6.16E-5 | 0.0003 | 0.002* | 0.0002, 0.003 | 0.001 | −0.07 | −0.31, 0.17 | 0.12 | 0.39‡ |
| Spleen | 0.004‡ | 0.003, 0.005 | 0.0005 | −0.0006 | −0.002, 0.0003 | 0.0005 | 0.003* | 0.001, 0.005 | 0.001 | −0.38* | −0.72, −0.05 | 0.17 | 0.38‡ |
| Brain | 0.0003 | −0.001, 0.002 | 0.0006 | −0.001* | −0.003, −0.0004 | 0.0005 | 0.003* | 0.001, 0.005 | 0.001 | 0.98‡ | 0.56, 1.41 | 0.21 | 0.12‡ |
| Residual | 0.17‡ | 0.13, 0.21 | 0.02 | 0.05* | 0.01, 0.09 | 0.02 | 0.23‡ | 0.14, 0.31 | 0.04 | −28.9† | −43.4, −14.4 | 7.34 | 0.44‡ |
<0.05;
<0.001;
<0.0001.
Bone model derived from NHANES data. Model units: components are in kg, age in years, and height in cm. SM, skeletal muscle; SE, standard error.
Adipose tissue mass was a significant predictor of organ-tissue composition in 17 of the 18 multiple regression models; the only non-significant association was present between adipose tissue and brain mass in women.
Obesity Tissue Composition
Composite Analysis
The mean mass of each of the ten components and their differences between the groups who were normal-weight and obese are summarized in Table 3. All of these between-group mass differences were statistically significant except for heart mass in men (Figure 1) and brain mass in women (Figure 2). The percentage organ-tissue composition of obesity tissue is shown in Table 3 and in Figure 3.
Table 3.
Composite Organ-Tissue Composition and Resting Energy Expenditure (REE) of Obesity Tissue.
| Composition† | REE§ | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| BMI (kg/m2) | Δ | %Δ | BMI (kg/m2) | Δ | %Δ | |||||
| <25 | 25-29.9 | >29.9 | <25 | 25-29.9 | >29.9 | |||||
| Men | ||||||||||
| AT | 14.5 | 22.2 | 30.6 | 16.0 | 48.0 | 65.3 | 99.8 | 138 | 72.2 | 15.7 |
| Skin | 3.88 | 4.31 | 4.62 | 0.75 | 2.23 | 27.9 | 31.0 | 33.3 | 5.37 | 1.17 |
| SM | 27.4 | 31.6 | 36.9 | 9.53 | 28.5 | 356 | 411 | 480 | 124 | 27.0 |
| Bone | 4.72 | 5.01 | 5.10 | 0.38 | 1.14 | 10.8 | 11.5 | 11.7 | 0.88 | 0.19 |
| Heart | 0.33 | 0.37 | 0.33 | 0.002 | 0.01 | 144 | 162 | 145 | 0.89 | 0.19 |
| Liver | 1.46 | 1.82 | 2.05 | 0.59 | 1.77 | 293 | 365 | 411 | 118 | 25.7 |
| Kidneys | 0.28 | 0.35 | 0.35 | 0.06 | 0.19 | 125 | 152 | 153 | 27.4 | 5.97 |
| Spleen | 0.23 | 0.33 | 0.37 | 0.14 | 0.41 | 23.1 | 33.4 | 36.7 | 13.5 | 2.95 |
| Brain | 1.57 | 1.60 | 1.69 | 0.11 | 0.34 | 378 | 385 | 405 | 27.5 | 5.98 |
| Residual | 17.0 | 20.7 | 22.8 | 5.81 | 17.4 | 204 | 248 | 274 | 69.8 | 15.2 |
| Total | 71.4 | 88.3 | 105 | 33.4 | 1,627 | 1,898 | 2,086 | 459 | ||
| Women | ||||||||||
| AT | 19.1 | 27.7 | 44.7 | 25.5 | 66.9 | 86.0 | 125 | 201 | 115 | 26.9 |
| Skin | 3.55 | 3.89 | 4.38 | 0.83 | 2.18 | 25.6 | 28.0 | 31.6 | 5.98 | 1.40 |
| SM | 19.4 | 21.7 | 24.7 | 5.38 | 14.1 | 252 | 282 | 322 | 69.9 | 16.4 |
| Bone | 3.91 | 3.97 | 4.35 | 0.45 | 1.18 | 8.98 | 9.13 | 10.0 | 1.03 | 0.24 |
| Heart | 0.25 | 0.29 | 0.32 | 0.06 | 0.17 | 112 | 126 | 140 | 27.9 | 6.53 |
| Liver | 1.34 | 1.50 | 1.77 | 0.43 | 1.12 | 269 | 300 | 354 | 85.7 | 20.1 |
| Kidneys | 0.24 | 0.26 | 0.34 | 0.10 | 0.26 | 104 | 114 | 148 | 43.7 | 10.2 |
| Spleen | 0.18 | 0.21 | 0.29 | 0.10 | 0.27 | 18.3 | 21.5 | 28.6 | 10.3 | 2.41 |
| Brain | 1.44 | 1.43 | 1.46 | 0.02 | 0.05 | 345 | 343 | 349 | 4.88 | 1.14 |
| Residual | 13.8 | 16.2 | 19.0 | 5.24 | 13.7 | 165 | 195 | 228 | 62.9 | 14.7 |
| Total | 63.2 | 77.2 | 101 | 38.1 | 1,385 | 1,543 | 1,812 | 427 | ||
Results are expressed as group mean values; corresponding mean values ±SE are shown in Figure 1 along with between-group statistical comparisons.
Component composition units are in kg.
Component units in kcal/d. Δs are the differences between the groups who were obese and normal weight that constitute obesity tissue; %Δ is the percentage of total mass or REE difference. AT, adipose tissue; BMI, body mass index; SM, skeletal muscle
Figure 1.
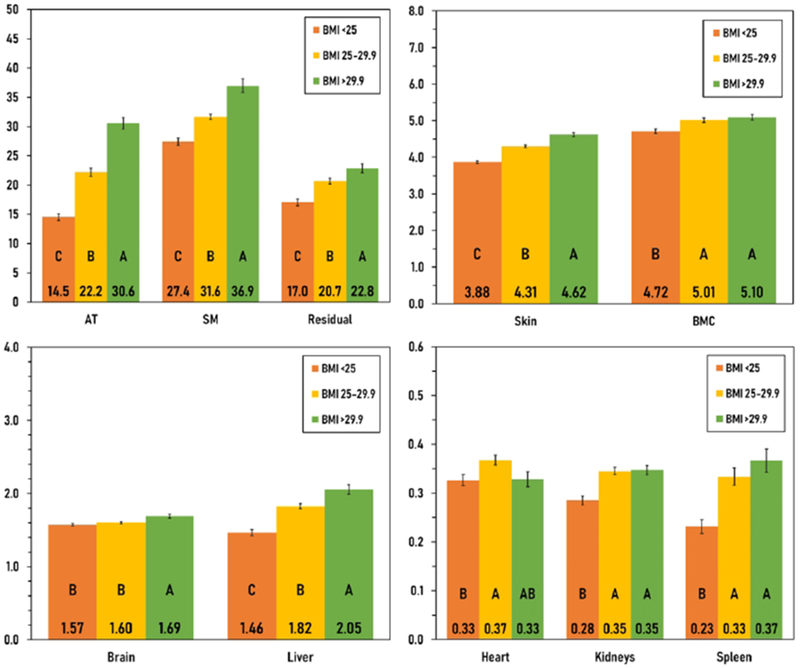
Organ and tissue mass, expressed in kg, of the three body mass index (BMI, kg/m2) groups for men. The group mean mass (±SE) of each component is shown in the vertical bars along with the Tukey letters corresponding to each group (between-group significant differences are denoted by different letters). Heart did not differ significantly between the groups of men who were normal weight and obese. Additional numerical details are presented in Table 3. AT, adipose tissue; BMC, bone mineral content; SM, skeletal muscle.
Figure 2.
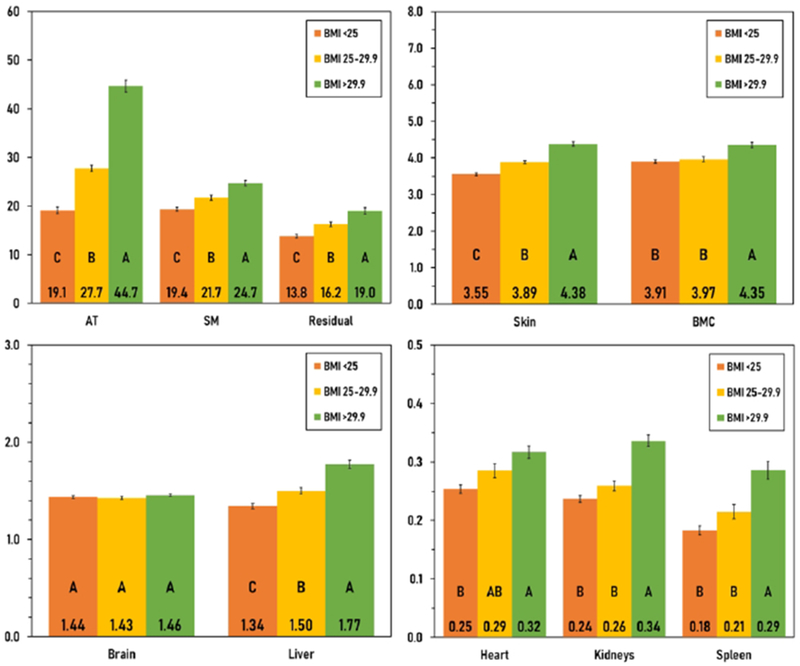
Organ and tissue mass, expressed in kg, of the three body mass index (BMI, kg/m2) groups for women. The group mean mass (±SE) of each component is shown in the vertical bars along with the Tukey letters corresponding to each group (between-group significant differences are denoted by different letters). Brain mass did not differ significantly between the groups of women who were normal weight and obese. Additional numerical details are presented in Table 3. AT, adipose tissue; BMC, bone mineral content; SM, skeletal muscle.
Figure 3.
Composition of obesity tissue, in percent, observed in the men (upper left) and women (lower left). Percentage contributions to resting energy expenditure (REE) for the men (upper right) and women (lower right). Additional numerical details are presented in Table 3.
Several key between-sex differences are present in obesity tissue. First, 48% of obesity tissue in men is adipose tissue, lower than the 67% present in women. By contrast, the obesity tissue is 29% skeletal muscle in men, more than double the 14% observed in women. Adipose tissue and skeletal muscle together constitute 77% and 81% of obesity tissue in men and women, respectively. The remaining components comprise a relatively small percentage of obesity tissue, as for example in men, about 0.01% for heart up to 2.2% for skin. Rankings in organ percentages were approximately the same in the men and women.
The relatively large difference in percentage adipose tissue between the men and women (i.e., 48.0% vs. 66.9%; Δ 18.9%) led us to seek secondary confirmation using the NHANES database as a source of DXA-measured fat mass (Table S2). As outlined by Webster et al. (12), we regressed BMI against fat mass index (fat mass/height2) as shown in the scatter plot presented in Figure S1. The inverse of the regression model slopes, adjusted for age and expressed in percent, were 60.8% and 68.2% (Δ 7.4%) for men and women, respectively. The comparable analysis for adipose tissue mass from the current data set was 65.5% and 71.3% (Δ 5.8%) for men and women, respectively (Figure S1). Similarly, we used the sex and race-specific regression model based on NHANES developed by Thomas et al. (24) to estimate the proportion of obesity tissue as fat mass. The respective results for men and women were 61.0% and 68.4% (Δ, 7.4%).
The sex difference (Δ, 14.4%) in the obesity tissue-relative content of skeletal muscle mass was also large, with 28.5% versus 14.1% in the men and women, respectively. As a secondary confirmation, we regressed BMI against appendicular lean soft tissue mass (appendicular LST)/height2 from DXA data acquired from the NHANES database. The appendicular LST component is a surrogate measure of a large proportion of total body skeletal muscle mass (25). Using the Webster et al. approach (12), the respective regression line inverse slopes, adjusted for age, were 26.6% and 19.9% (Δ 6.7%) for the men and women (Figure S2).
Resting Energy Expenditure
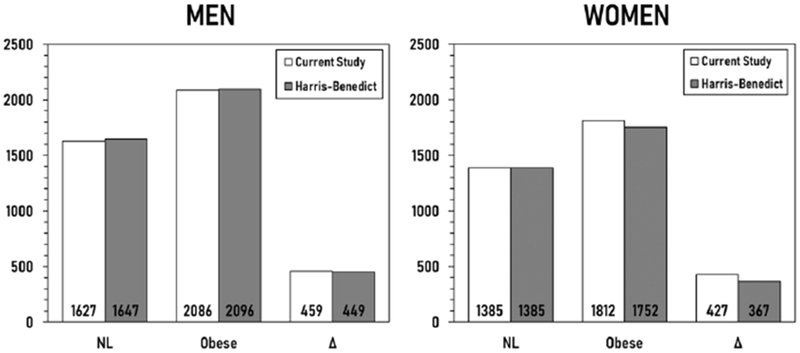
The calculated REE of obesity tissue for men and women are 459 kcal/d (kcal/d) and 427 kcal/d, respectively (Table 3). Of the total, 16% and 27% of obesity tissue REE is accounted for by adipose tissue in the men and women, respectively. About 36% to 53% of the remainder is accounted for by the combined mass of skeletal muscle and liver. Another 6% to 17% is attributable to heart and kidneys (Figure 3).
The obesity tissue REE estimates were compared to corresponding estimates made by the commonly used Harris-Benedict REE prediction equations based on body weight, height, and age (16). As shown in Figure S3, the three organ-estimated REE values (i.e., for the groups who were normal weight and obese and the between-group difference) for men and women show close associations (mean Δs −10 to +60 kcal/d)) between those estimated by the Harris-Benedict equations (16). The mass-specific REE of obesity tissue was larger in the men compared to the women for both the organ-tissue derivations of current study (~14 vs. 11 kcal/kg/d) and for the Harris Benedict equations (~13 vs. 10 kcal/kg/d).
Metabolizable Energy Content
The fat, protein, and carbohydrate contents of obesity tissue are presented in Table S3 for the men and women. The metabolizable energy content of obesity tissue is about 142,075 kcal or 4,562 kcal/kg in men and 210,908 kcal or 5,525 kcal/kg in the women (Table 4). Adipose tissue, a large proportion of which is fat, and skeletal muscle are the main contributors to the metabolizable energy content of obesity tissue in both the men and women. Obesity tissue also contains an estimated 3.6 kg and 3.3 kg of protein in men and women, respectively (Table S3), a potential source of essential and non-essential amino acids during periods of negative energy and nitrogen balance. This substantial protein pool contrasts to the amount present in normal-weight adults of about 9-10 kg.
Table 4.
Metabolizable Energy Content of Obesity Tissue.
| BMI (kg/m2) | ΔE | Δ | ||||||
|---|---|---|---|---|---|---|---|---|
| <25 | 25-29.9 | >29.9 | kcal | % | ||||
| Energy | % | Energy | % | Energy | % | |||
| Men | ||||||||
| AT | 112,574 | 63.8 | 172,034 | 70.2 | 236,921 | 74.4 | 124,347 | 87.5 |
| Skin | 8,898 | 5.04 | 9,887 | 4.03 | 10,611 | 3.33 | 1,713 | 1.21 |
| SM | 29,826 | 16.9 | 34,457 | 14.1 | 40,204 | 12.6 | 10,378 | 7.30 |
| Bone | 8,959 | 5.08 | 9,527 | 3.90 | 9,684 | 3.04 | 724 | 0.51 |
| Liver | 2,482 | 1.41 | 3,094 | 1.26 | 3,483 | 1.09 | 1,001 | 0.70 |
| Heart | 563 | 0.32 | 633 | 0.26 | 566 | 0.18 | 3.47 | 0.002 |
| Kidneys | 367 | 0.21 | 445 | 0.18 | 447 | 0.14 | 80.4 | 0.06 |
| Spleen | 246 | 0.14 | 355 | 0.14 | 391 | 0.12 | 144 | 0.10 |
| Brain | 2,165 | 1.23 | 2,206 | 0.90 | 2,323 | 0.73 | 158 | 0.11 |
| Residual | 10,324 | 5.85 | 12,541 | 5.12 | 13,850 | 4.35 | 3,526 | 2.48 |
| Total | 176,404 | 245,178 | 318,479 | 142,075 | ||||
| Women | ||||||||
| AT | 148,285 | 74.7 | 215,187 | 79.5 | 346,298 | 84.6 | 198,013 | 93.9 |
| Skin | 8,155 | 4.11 | 8,924 | 3.30 | 10,061 | 2.46 | 1,906 | 0.90 |
| SM | 21,077 | 10.6 | 23,650 | 8.74 | 26,936 | 6.58 | 5,858 | 2.78 |
| Bone | 7,420 | 3.74 | 7,540 | 2.79 | 8,272 | 2.02 | 852 | 0.40 |
| Liver | 2,277 | 1.15 | 2,546 | 0.94 | 3,004 | 0.73 | 727 | 0.34 |
| Heart | 437 | 0.22 | 491 | 0.18 | 546 | 0.13 | 109 | 0.05 |
| Kidneys | 305 | 0.15 | 334 | 0.12 | 433 | 0.11 | 128 | 0.06 |
| Spleen | 195 | 0.10 | 229 | 0.08 | 305 | 0.07 | 110 | 0.05 |
| Brain | 1,976 | 1.00 | 1,965 | 0.73 | 2,004 | 0.49 | 28.0 | 0.01 |
| Residual | 8,353 | 4.21 | 9,847 | 3.64 | 11,530 | 2.82 | 3,177 | 1.51 |
| Total | 198,480 | 27,0713 | 409,388 | 210,908 | ||||
Results are expressed as group mean values tor metabolizable energy in kcal tor each component and the total kcal for that BMI group; a second column presents each component’s percentage of total kcal. ΔE is the metabolizable energy content of obesity tissue (i.e., the difference between the groups who were normal-weight and obese) and Δ (%) is each component’s percentage of the total ΔE. AT, adipose tissue; BMI, body mass index; SM, skeletal muscle. Additional composition data is presented in Table S3.
DISCUSSION
The current study confirms that Pitts’s 1962 speculation on the composition of obesity tissue was largely correct (14). That is, obesity tissue is composed not only of adipose tissue and its two associated non-lipid components (i.e., non-fat cell mass and extracellular fluid), but all other major non-adipose organs and tissues that enlarge as a means of accommodating steady-state mechanical and metabolic functional demands (2). These findings indicate that “obesity” is not solely characterized by excess adipose tissue, but by increases in these other “companion” organs and tissues (26). The composite obesity tissue compartment that includes high metabolic rate organs largely accounts for the greater heat production rates observed in people who are obese relative to those who are normal weight (15, 17).
Systemic Response to Excess Adipose Tissue
The current study extends the single component (adipose tissue) and two-component (i.e., fat mass and FFM) portrayals of obesity tissue to include all major organs and tissues that are reliably measurable in vivo. Our findings are consistent with multiple earlier studies reporting relative increases in the mass of selected organs and tissues present in persons who are obese (e.g., left ventricular hypertrophy (27); glomerular hypertrophy (28); and hepatomegaly (29)). Notably, our analyses reveal that with excess adipose tissue mass there are accompanying increases in the mass of skin (integumentary system), skeletal muscle (muscular system), bone (skeletal system), heart (circulatory system), liver (digestive system), kidneys (urinary system), spleen (lymphatic system), and brain (nervous system), the latter in men only. The mechanisms underlying these increases in organ and tissue mass reflect their molecular and anatomic plasticity (2). These system-level features of obesity tissue add to the now well-established hormonal and metabolic mileu accompaning an enlarged adipose tissue compartment (1, 2).
Energy Expenditure
The observed organ-tissue profile of obesity tissue translated directly into the heat production rates of this compartment with our estimates similar to those calculated using the commonly referenced Harris-Benedict prediction equations based on body weight, height, and age. The four main contributors (~80%) to the estimated REEs included skeletal muscle, adipose tissue, liver, and kidneys (Figure 3). Excess adipose tissue alone cannot thus account for the greater rate of heat production seen in people who are obese, a finding consistent with the long held observation that both fat mass and FFM are independent predictors of REE (30). The FFM component includes not only the non-adipose organ and tissue mass associated with obesity tissue, but the small heat-producing fat-free cell mass and extracellular portions of adipose tissue (31).
Longitudinal Considerations
The current study focused on the cross sectional features of obesity tissue as might be encountered on an initial patient evaluation. An important question that arises is if with negative energy balance, losses in organ and tissue mass follow. An earlier study from our group examined this question in a sample of 45 women with obesity (BMI 35.9 kg/m2) who lost weight (9.5 kg) during a 12-week low-calorie diet period (32). Significant reductions were observed in skeletal muscle (−3.1%), heart (−5.2%), liver (−4.4%), and kidney (−6.1%) mass; a small significant increase was present in bone mass (+1.3%) and there was no change in brain mass (+0.4%). More recently Gallagher et al. (33) evaluated changes in organ and tissue mass over one-(n=36) and two-year periods in 26 patients who were overweight and obese (BMI −31 kg/m2) with type 2 diabetes treated with an intensive lifestyle program that included a low calorie diet and exercise. Body weight loss was 6.6 kg and 5.2 kg at the two respective time points with reductions of variable statistical significance in skeletal muscle, heart, liver, kidney, and spleen mass. These observations strengthen and extend the companionship rule advanced by Pitts (1962) (14) and later Forbes (1993) (26) by providing evidence that during periods of negative energy balance there are not only dynamic changes in fat and adipose tissue mass, but of mechanistically-linked organs and other non-adipose tissues (8, 9). The potential exists to conduct detailed studies with larger and more diverse samples as a means of developing dynamic body composition-energy expenditure models.
Sexual Dimorphism
While the general patterns of body composition effects were similar across the men and women with the exception of brain mass, the relative contributions to obesity tissue showed pronounced sexual dimorphism. The proportion of obesity tissue as skeletal muscle mass was larger (Δ, 14.4%) in the men than in the women, a finding supported by DXA-measured appendicular LST in the NHANES sample (Δ, 6.7%). By contrast, the proportion of obesity tissue as adipose tissue mass was substantially larger (Δ, 18.9%) in the women than in the men (Figure 3). The net effect of these differences is that women had a larger metabolizable energy store than the men (~48%), a greater energy density of obesity tissue (~5,534 kcal/kg vs. 4,253 kcal/kg), and a lower compartment total and mass-specific REE (~427 kcal/d vs. 459 kcal/d; and ~11 kcal/kg/d vs. 14 kcal/kg/d). These differences in obesity tissue partitioning, all of which potentially impact weight gain and weight loss dynamics, likely arise from hormonal mechanisms (34). These observations indicate that the well-known sexual dimorphism in skeletal muscle mass and adiposity as reflected in the classical Reference Man and Woman (19) extends to the composition and metabolic properties of obesity tissue.
Study Limitations
As noted throughout our report we distinguished between “fat” and “adipose tissue”. As observed in our previous study, triglyceride or “fat”, averages about 80-85% of adipose tissue mass, although the range observed both in vitro and in vivo is very wide (i.e., 0.62-0.94) (20). Converting from fat to adipose tissue mass or vice versa using assumed proportionalities may thus not be very accurate (20). Moreover, with weight loss the expectation is that relative reductions in body fat will exceed those of adipose tissue since the latter includes non-triglyceride cell mass, extracellular fluid, connective tissues, and vascular structures forming a pannus that in extreme cases may need surgical excision as often follows with the massive weight loss accompanying bariatric surgery. These legacy tissues, including skin, will be included in adipose tissue-free mass and FFM (31). Additionally, with weight loss there may be non-linear changes in organ and tissue mass that would not be accurately captured by our linear models. The predicted changes in organ mass with weight loss are relatively small and future studies should thus be adequately powered in order to accurately capture the magnitudes of these effects. Another limitation of the current study is that not all fat is in adipose tissue and we were unable to adjust our organ mass estimates for non-adipose intracellular triglyceride content (35). Similarly, we did not build brown fat, a potential source of thermogenesis, into our models (36). Lastly, we contrasted obesity tissue features in men those observed in our sample of women. Women tended to be younger and have a higher BMI than the men, both of which can influence our findings to a small extent, emphasizing the population-specific nature of the current study observations.
CONCLUSIONS
The current study extends reports characterizing the nature of what descriptively is referred to as excess body weight, adiposity tissue, or obesity tissue (4, 6, 12). Three main features of this compartment are presented, including in depth composition, resting heat production rates, and metabolically available energy and protein content. An important task that remains is development of mechanism-based static and dynamic physiological models that integrate excess adipose tissue mass with the previously not-fully appreciated companion non-adipose organs and tissues.
Supplementary Material
What is already known about this subject?
Chronic positive energy balance leads to adipose tissue accumulation and obesity over time.
The “excess” body mass accompanying obesity is variably referred to as “adiposity” or “obesity” tissue.
The current paradigm establishes obesity tissue as consisting either solely of adipose tissue mass or a combination of fat (intracellular triglycerides) and fat-free components (non-fat cell mass and extracellular fluid).
What does this study add?
Obesity tissue, the “extra” body mass present between people who are normal weight and people who are obese, includes skin, skeletal muscle, bone, heart, liver, kidney, spleen, brain, and residual mass in addition to adipose tissue mass.
The increase in resting energy expenditure observed in persons with obesity can be accounted for by these ten components with only a small proportion contributed by adipose tissue.
A pronounced sexual dimorphism is present in the composition and resting energy expenditure of obesity tissue, a major component of body mass that defines the obese phenotype.
Acknowledgments
FUNDING:
This work was partially supported by National Institutes of Health NORC Center Grants P30DK072476, Pennington/Louisiana; and P30DK040561, Harvard; and R01DK109008, Shape UP! Adults.
Footnotes
DISCLOSURE:
The authors declared no conflict of interest.
REFERENCES
- 1.Bray GA, Kim KK, Wilding JPH, World Obesity F. Obesity: a chronic relapsing progressive disease process. A position statement of the World Obesity Federation. Obes Rev 2017;18(7):715–23. [DOI] [PubMed] [Google Scholar]
- 2.Gadde KM, Martin CK, Berthoud HR, Heymsfield SB. Obesity: Pathophysiology and Management. J Am Coll Cardiol 2018;71(1):69–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jastreboff AM, Kotz CM, Kahan S, Kelly AS, Heymsfield SB. Obesity as a Disease: The Obesity Society 2018 Position Statement. Obesity (Silver Spring) 2019;27(1):7–9. [DOI] [PubMed] [Google Scholar]
- 4.Sharples AJ, Mahawar K, Cheruvu CVN. Systematic review and retrospective validation of prediction models for weight loss after bariatric surgery. Surg Obes Relat Dis 2017;13(11):1914–20. [DOI] [PubMed] [Google Scholar]
- 5.Mechanick JI, Hurley DL, Garvey WT. Adiposity-Based Chronic Disease as a New Diagnostic Term: The American Association of Clinical Endocrinologists and American College of Endocrinology Position Statement. Endocr Pract 2017;23(3):372–8. [DOI] [PubMed] [Google Scholar]
- 6.Brozek J, Grande F, Anderson JT, Keys A. Densitometric Analysis of Body Composition: Revision of Some Quantitative Assumptions. Ann N Y Acad Sci 1963;110:113–40. [DOI] [PubMed] [Google Scholar]
- 7.Keys A, Brozek J. Body fat in adult man. Physiol Rev 1953;33(3):245–325. [DOI] [PubMed] [Google Scholar]
- 8.Heymsfield SB. Energy expenditure-body size associations: molecular coordination. Eur J Clin Nutr 2018;72(9):1314–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Heymsfield SB, Thomas DM, Bosy-Westphal A, Muller MJ. The anatomy of resting energy expenditure: body composition mechanisms. Eur J Clin Nutr 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Thomas DM. Modeling in clinical nutrition: does it add to patient care? Eur J Clin Nutr 2013;67(5):555–7. [DOI] [PubMed] [Google Scholar]
- 11.Forbes GB, Welle SL. Lean body mass in obesity. Int J Obes 1983;7(2):99–107. [PubMed] [Google Scholar]
- 12.Webster JD, Hesp R, Garrow JS. The composition of excess weight in obese women estimated by body density, total body water and total body potassium. Hum Nutr Clin Nutr 1984;38(4):299–306. [PubMed] [Google Scholar]
- 13.Forbes GB. Lean body mass-body fat interrelationships in humans. Nutr Rev 1987;45(8):225–31. [DOI] [PubMed] [Google Scholar]
- 14.Pitts GC. Density and composition of the lean body compartment and its relationship to fatness. Am J Physiol 1962;202:445–52. [DOI] [PubMed] [Google Scholar]
- 15.Gallagher D, Belmonte D, Deurenberg P et al. Organ-tissue mass measurement allows modeling of REE and metabolically active tissue mass. Am J Physiol 1998;275(2 Pt 1):E249–58. [DOI] [PubMed] [Google Scholar]
- 16.Harris JA, Benedict FG. A Biometric Study of Human Basal Metabolism. Proc Natl Acad Sci U S A 1918;4(12):370–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bosy-Westphal A, Reinecke U, Schlorke T et al. Effect of organ and tissue masses on resting energy expenditure in underweight, normal weight and obese adults. Int J Obes Relat Metab Disord 2004;28(1):72–9. [DOI] [PubMed] [Google Scholar]
- 18.Heymsfield SB, Peterson CM, Bourgeois B et al. Human energy expenditure: advances in organ-tissue prediction models. Obes Rev 2018;19(9):1177–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Snyder WS, Cook MJ, Nasset ES, Karhausen LR, Howells GP, Tipton IH. Report of the Task Group on Reference Man. New York: Pergamon Press; 1975. 480 p. [Google Scholar]
- 20.Hubers M, Geisler C, Bosy-Westphal A et al. Association between fat mass, adipose tissue, fat fraction per adipose tissue, and metabolic risks: a cross-sectional study in normal, overweight, and obese adults. Eur J Clin Nutr 2019;73(1):62–71. [DOI] [PubMed] [Google Scholar]
- 21.Later W, Bosy-Westphal A, Kossel E, Gluer CC, Heller M, Muller MJ. Is the 1975 Reference Man still a suitable reference? Eur J Clin Nutr 2010;64(10):1035–42. [DOI] [PubMed] [Google Scholar]
- 22.Later W, Bosy-Westphal A, Hitze B et al. No evidence of mass dependency of specific organ metabolic rate in healthy humans. Am J Clin Nutr 2008;88(4):1004–9. [DOI] [PubMed] [Google Scholar]
- 23.Leonard CM, Roza MA, Barr RD, Webber CE. Reproducibility of DXA measurements of bone mineral density and body composition in children. Pediatr Radiol 2009;39(2):148–54. [DOI] [PubMed] [Google Scholar]
- 24.Heymsfield SB, Peterson CM, Thomas DM et al. Scaling of adult body weight to height across sex and race/ethnic groups: relevance to BMI. Am J Clin Nutr 2014;100(6):1455–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tukey JW. Comparing individual means in the analysis of variance. Biometrics 1949;5(2):99–114. [PubMed] [Google Scholar]
- 26.Forbes GB. The companionship of lean and fat. Basic Life Sci 1993;60:1–14. [DOI] [PubMed] [Google Scholar]
- 27.Lauer MS, Anderson KM, Kannel WB, Levy D. The impact of obesity on left ventricular mass and geometry. The Framingham Heart Study. JAMA 1991;266(2):231–6. [PubMed] [Google Scholar]
- 28.Tsuboi N, Okabayashi Y, Shimizu A, Yokoo T. The Renal Pathology of Obesity. Kidney Int Rep 2017;2(2):251–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kratzer W, Fritz V, Mason RA, Haenle MM, Kaechele V, Roemerstein Study G. Factors affecting liver size: a sonographic survey of 2080 subjects. J Ultrasound Med 2003;22(11):1155–61. [DOI] [PubMed] [Google Scholar]
- 30.Heymsfield SB, Thomas D, Bosy-Westphal A, Shen W, Peterson CM, Muller MJ. Evolving concepts on adjusting human resting energy expenditure measurements for body size. Obes Rev 2012; 13(11):1001–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Abe T, Dankel SJ, Loenneke JP. Body Fat Loss Automatically Reduces Lean Mass by Changing the Fat-Free Component of Adipose Tissue. Obesity (Silver Spring) 2019. [DOI] [PubMed] [Google Scholar]
- 32.Bosy-Westphal A, Kossel E, Goele K et al. Contribution of individual organ mass loss to weight loss-associated decline in resting energy expenditure. Am J Clin Nutr 2009;90(4):993–1001. [DOI] [PubMed] [Google Scholar]
- 33.Gallagher D, Kelley DE, Thornton J et al. Changes in skeletal muscle and organ size after a weight-loss intervention in overweight and obese type 2 diabetic patients. Am J Clin Nutr 2017;105(1):78–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bredella MA. Sex Differences in Body Composition. Adv Exp Med Biol 2017;1043:9–27. [DOI] [PubMed] [Google Scholar]
- 35.Bosy-Westphal A, Braun W, Albrecht V, Muller MJ. Determinants of ectopic liver fat in metabolic disease. Eur J Clin Nutr 2018. [DOI] [PubMed] [Google Scholar]
- 36.Leitner BP, Huang S, Brychta RJ et al. Mapping of human brown adipose tissue in lean and obese young men. Proc Natl Acad Sci U S A 2017;114(32):8649–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


