Abstract
Sexual assault (SA) is a common experience in the lives of women and men and is associated with numerous deleterious outcomes. Understanding the relative prevalence of psychiatric diagnoses in people who have been sexually assaulted versus people who have not been assaulted could help to prioritize assessment and intervention efforts, but there has been no quantitative review of this topic. A search of PsychINFO, ProQuest Digital Dissertations & Theses, and Academic Search Premier for articles dated between 1970 and 2014 was conducted, and unpublished data was obtained. Eligible studies used diagnostic interviews to assess DSM diagnoses in both individuals experiencing adolescent/adult and/or lifetime sexual assault and unassaulted individuals. The search yielded 171 eligible effects from 39 studies representing 88,539 participants. Meta-analysis was used to aggregate the prevalence of psychiatric diagnoses in sexually assaulted and unassaulted samples, as well as calculate odds ratios reflecting the difference between these prevalence estimates. Results indicated that most disorders were more prevalent in survivors of SA, and depressive disorders and PTSD were especially prevalent. Disorder-specific differences in odds ratios were observed as a function of sample type, type of comparison group, and time frame of SA. Service providers should be prepared to address depressive disorders and PTSD in survivors of SA, and interventions that prevent the development of these disorders are especially needed.
Keywords: sexual violence, psychopathology, meta-regression, depression, victimization, rape
Sexual assault (SA) is a widespread and deleterious problem. In the United States, 17–25% of women and 1–3% of men will be sexually assaulted in their lifetime (Black et al., 2011; Fisher, Cullen, & Turner, 2000; Koss, Gidycz, & Wisniewski, 1987; Tjaden & Thoennes, 2000, 2006). The high prevalence of SA is particularly concerning in light of its multiple consequences for survivors, including psychological disorders (Campbell, Dworkin, & Cabral, 2009; Dworkin, Menon, Bystrynski, & Allen, 2017), educational difficulties (Baker et al., 2016), physical health problems (Golding, 1994; Stein & Barrett-Connor, 2000), and problems with sexual and relationship functioning (Van Berlo & Ensink, 2000). These consequences have tangible and intangible costs to both survivors and society more broadly (McCollister, French, & Fang, 2011; Post, Mezey, Maxwell, & Wibert, 2002), which highlights the importance of preventing and effectively responding to SA as a public health issue.
Prevalence of Mental Disorders in Survivors of Sexual Assault
It is clear that SA victimization is associated with a variety of forms of psychopathology (Campbell et al., 2009; Dworkin et al., 2017). A recent meta-analysis found that people exposed to SA were significantly more symptomatic than unassaulted comparisons across a range of forms of psychopathology, including anxiety (g = 0.53), depression (g = 0.60), bipolar conditions (g = 0.66), disordered eating (g = 0.39), obsessive-compulsive conditions (g = 0.71), trauma and stressor-related conditions including posttraumatic stress disorder (PTSD) (g = 0.71), and substance abuse and dependence (g = 0.37) (Dworkin et al., 2017). An earlier qualitative review found that 73–82% of sexually assaulted adults developed fear/anxiety, 12–40% reported generalized anxiety, 17–65% evidenced PTSD, 13–49% developed alcohol dependence, and 28%−61% used drugs (Campbell et al., 2009). Although these reviews evidence the diversity in conditions associated with SA, both reviews conceptualized psychopathology as broad, dimensional constructs and included forms of distress that do not meet criteria for mental disorders as defined by the Diagnostic and Statistical Manual of Mental Disorders (DSM) (American Psychiatric Association, 2013). Both reviews also combined estimates of lifetime and current psychopathology. As a result, the relative prevalence of various DSM-defined mental disorders in survivors of SA, as well as the degree to which SA is associated with increased risk for each disorder, remain unclear.
It is important to have accurate normative data regarding the expected prevalence of various disorders among people who have been sexually assaulted relative to people who have not been assaulted for several reasons. First, systems serving survivors of SA (e.g., rape crisis centers) should be prepared to address the disorders most likely to be seen in survivors. Second, the design of preventative interventions for the development of various disorders after SA should consider the disorders most likely to develop. Third, such information would be useful as part of efforts to educate survivors, the public, grantmakers, and clinicians about the impact of SA, especially if it was available in a manner that is readily meaningful to individuals without statistical training (i.e., as prevalence estimates rather than Hedges’ g or odds ratios). However, there has been no quantitative summary of the prevalence of mental disorders associated with SA. The ranges in prevalence of each form of psychopathology reported in the previous qualitative review were wide (Campbell et al., 2009), which makes it difficult to determine the expected prevalence of each disorder and thereby prioritize efforts to intervene.
Potential Factors Accounting for Differences in Prevalence Estimates
The conditions under which people who have been sexually assaulted are more likely to evidence specific mental disorders also remain unclear. In general, most studies of psychopathology associated with SA attempt to identify correlates of a single form of psychopathology. Relatively less research has attempted to understand differential moderators of effect sizes for specific disorders, and when this research is conducted, it is difficult to determine the degree to which observed effects are driven by characteristics of the sample or study methods. Meta-analysis is an ideal method for disentangling these effects, as it can compare across multiple studies investigating with different methods and samples to understand the conditions under which smaller or larger effect sizes are observed for multiple types of mental disorders. Beyond characteristics of disorders themselves (e.g., type of disorder, past year versus lifetime diagnosis), several characteristics of studies may alter the relative prevalence of various disorders in people with a history of SA as compared to those without such a history.
Sample type.
SA and associated psychopathology have been studied in a wide variety of samples (e.g., veterans, college students, individuals seeking rape kits), and there may be differences in risk for specific mental disorders across these samples. Group differences in psychopathology between survivors of SA and people who have not been assaulted tend to be smaller in populations selected for specific trait (e.g., college students, people seeking healthcare) relative to the general population (Dworkin et al., 2017). This could occur for two reasons. First, survivors of SA in some populations may be less likely to exhibit certain forms of psychopathology than survivors in other populations. This could occur if having a given disorder interferes with being a member of that population. For example, some research indicates that substance use disorders and bipolar disorder, but not depressive disorders, anxiety disorders, or posttraumatic stress disorder, are associated with failure to enter college and increased likelihood of college dropout (Breslau, Lane, Sampson, & Kessler, 2008). If survivors of SA are more likely to develop these disorders, survivors in college populations may, as a whole, evidence lower average levels of psychopathology than survivors in the general population. In addition, characteristics of the types of assaults experienced or the degree to which psychotherapy resources are accessible to survivors in these populations could affect the degree to which survivors evidence psychopathology. Survivors recruited from college campuses, for example, may be less likely to experience assaults involving weapon use—a risk factor for psychopathology (Dworkin et al., 2017)—than survivors presenting at emergency departments seeking a rape kit. However, it is unclear whether this differs across disorders. Second, in some populations, people who have not been sexually assaulted may have different base rates of certain disorders. When base rates are higher in a given population, this would reduce group differences between people who have not been assaulted and people who have been assaulted. For example, PTSD rates are relatively higher among veterans (12–14%) (Kang, Natelson, Mahan, Lee, & Murphy, 2003; Tanielian & Jaycox, 2008) and people seeking healthcare (9%) (Gillock, Zayfert, Hegel, & Ferguson, 2005) than in the general population (4%) (Kessler, Chiu, Demler, & Walters, 2005). In college populations, risk of alcohol use disorder is higher than in non-college populations (Blanco et al., 2008). Thus, in these populations, people who have not experienced SA may have similar odds of meeting criteria for these disorders as compared to people who have experienced SA.
Comparison group type.
The group to whom survivors of SA are compared differs across studies. Some studies use comparison groups that have not experienced SA, others use comparison groups exposed to a non-SA form of trauma (e.g., physical assault), and still others use comparison groups unexposed to any interpersonal violence. The degree to which effect sizes from these types of studies differ from each other could clarify the degree to which SA is a stronger risk factor for various disorders than other forms of trauma. Several studies have found higher rates of PTSD in people exposed to SA relative to people exposed to other forms of trauma (Kelley et al., 2009; Kessler et al., 1995), but it is unclear whether this is true for other mental disorders, or how the magnitude of these differences compares to studies using other types of comparison groups. In an epidemiological study of adolescents, different forms of trauma exposure were differentially associated with specific diagnoses (Kilpatrick et al., 2003). For example, physical assault, but not SA, was associated with higher risk of non-comorbid major depressive episode and non-comorbid substance use disorder, but neither was a significant risk factor for non-comorbid posttraumatic stress disorder. In contrast, in a study of female veterans, SA was associated with higher risk than other traumas for mood disorders, anxiety disorders, and PTSD, but not substance use disorders (Zinzow, Grubaugh, Frueh, & Magruder, 2008). Testing whether the odds of various mental disorders differ as a function of comparison group type could resolve these conflicting findings and clarify whether SA is associated with higher risk of a range of mental disorders than other forms of trauma.
Timing of sexual assault.
Unlike the broader literature on traumatic stress, which typically examines lifetime exposure to traumatic events, some studies of SA limit their focus to assaults that occurred in adolescence and/or adulthood, or in the past year. Studies of lifetime SA include individuals who experienced SA in either childhood or adolescence/adulthood. As a result, if the risk for a given mental disorder associated with SA is time-limited, studies of lifetime SA should evidence smaller effect sizes than studies of adolescent/adult SA, which should in turn evidence smaller effect sizes than studies of past-year SA. Indeed, age at trauma exposure has been associated with PTSD risk in past meta-analyses (Brewin, Andrews, & Valentine, 2000; Ozer, Best, Lipsey, & Weiss, 2003). However, no past review has attempted to compare risk for various mental disorders between studies of past-year SA, adolescent/adult SA, and lifetime SA.
The Current Study
In sum, although past reviews have summarized the degree to which SA is associated with various forms of broadly-defined psychological distress—using both diagnostic and non-diagnostic measures and collapsing across timeframes in which this distress could have occurred (e.g., lifetime, past year) (Campbell et al., 2009; Dworkin et al., 2017)—no review has summarized the prevalence of various specific mental disorders in sexually assaulted versus unassaulted samples, or examined disorder-specific moderators of associations between psychopathology and SA. The primary goal of this study was thus to provide normative data regarding (1) the prevalence of various DSM-defined disorders in people who have been sexually assaulted and people who have not been assaulted and (2) the odds of experiencing each disorder as a function of SA history. A secondary goal was to examine disorder-specific heterogeneity in these effects and understand what factors might account for heterogeneity, given that moderators of the association between SA and psychopathology might differ depending on the specific disorder under investigation.
Method
Data were collected as part of a larger meta-analysis assessing associations between SA and multiple forms of broadly-defined psychological distress (AUTHOR CITATION). Articles included in the current manuscript reflect the subset of articles from the prior meta-analysis that reported on the prevalence of DSM diagnosis, from which disorder-specific prevalence estimates and odds ratios (ORs) could be obtained and disorder-specific moderators could be tested. Detailed information regarding study methodology is available in the original manuscript and its supplemental materials.
Literature Search and Study Retrieval
Literature searches were conducted in PsycINFO, ProQuest Digital Dissertations & Theses, and Academic Search Premier for publications issued between January 1, 1970 and December 31, 2014, which yielded 125,780 search results that received title review. Of these, 2813 received full-text review. A database of articles collected by the author for a previous qualitative review on this topic (Campbell et al., 2009) was examined. In addition, 2010–2014 issues of seven journals most-frequently represented on a tentative list of eligible articles were reviewed. Finally, researchers were contacted personally to obtain unpublished data.
Eligibility Criteria
Figure 1 summarizes the study selection process. Both observational and experimental studies were eligible, although only baseline data from experimental studies (i.e., before exposure to an experimental condition) was extracted. Eligibility criteria for the broader analysis were as follows. First, the study must have been quantitative with N >10. Second, data must have been available for a group comprised of survivors of either adolescent/adult or lifetime SA, defined as unwanted/nonconsensual sexual contact (i.e., the SA group). To avoid duplicating past reviews (Chen et al., 2010; Smolak & Murnen, 2002), the SA group must not have been exclusively comprised of survivors of child sexual abuse. Third, data for a comparison (i.e., no-SA) group comprised of people who had not experienced SA must have been available. Studies that compared people who had experienced a specific form of SA to all others (i.e., people who had experienced other forms of SA as well as people who had not been assaulted) were excluded, as people who had experienced SA were included in the no-SA groups in these studies. Fourth, to avoid clinical selection bias (du Fort et al., 1993) in a manner consistent with similar meta-analyses (Brewin, Andrews, & Valentine, 2000; Tolin & Foa, 2006), the study must not have exclusively or primarily sampled people seeking psychological treatment or with mental disorders. Fifth, adequate data must have been available in English to calculate effect sizes. Sixth, the study must have assessed one of the disorders of interest. Studies that assessed SA risk prospectively after onset of a mental disorder were excluded; only baseline data was included for longitudinal studies. A final eligibility criterion was added to create a subset of studies relevant to the goals of the current meta-analysis: studies must have used a structured or semi-structured interview (including computerized interview methods) to assess whether participants met DSM diagnostic criteria for the disorders of interest. This led to the exclusion of 326 effect sizes and 156 studies.
Figure 1.
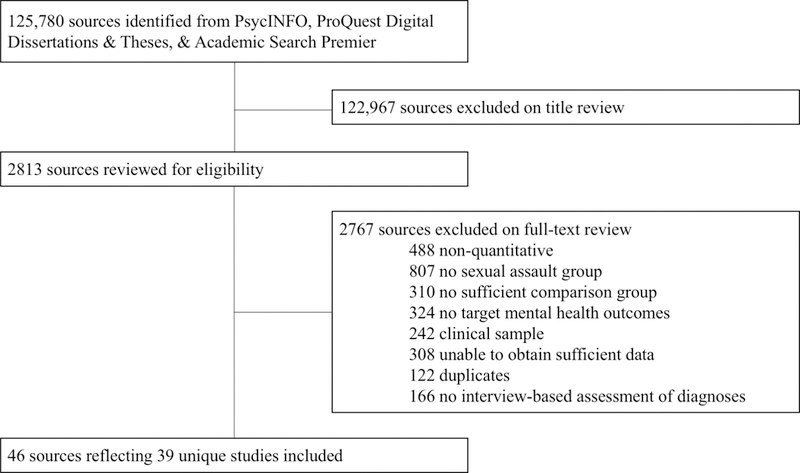
Study exclusion table.
Data Extraction
The coding team was comprised of the study author and 12 extensively-trained research assistants. Effects were coded by at least two coders. All discrepancies received review by the author and/or at least one other coder; discrepancies were resolved by discussion. Coding accuracy was tracked for variables judged to be difficult to code; substantial to near-perfect agreement for independent coders was obtained.
The following information was extracted. First, for each effect, a 2×2 contingency table representing the number of participants in the SA and no-SA group with and without each diagnosis was recorded. Second, in addition to moderators characterizing a specific diagnosis (i.e., type of mental disorder, whether the diagnosis reflected a lifetime or past-year disorder) the following moderators were coded: type of comparison group (i.e., no SA exposure, no interpersonal violence exposure, other-trauma exposure)1, type of sample (e.g., general community, college students, veterans), and time frame of SA victimization (i.e., in participants’ lifetime, in adolescence/adulthood, in the past year). Finally, for the purposes of describing each study, the source of data (i.e., journal article, book chapter, dissertation/thesis, unpublished dataset), the country of data collection, the percent of women in the sample, the sample mean age, and the majority (>60%) racial group represented in US samples were recorded.
Analytic Plan
Analyses were conducted using metafor (Viechtbauer, 2010) in R 3.3.1 (R Development Core Team, 2014). Proportions and associated variances for the SA and no-SA group, and log ORs and associated variances, were calculated.
To minimize the influence of outliers, sensitivity analyses were conducted within each lifetime and past-year diagnostic category if at least 5 effects were available within that category. Outliers were truncated to the upper limit of the 95% CI for an unconditional model computed using data without outliers. Sensitivity analyses were conducted on the prevalence of each diagnostic category in the SA and no-SA group for the purposes of aggregating these values (i.e., truncated proportions were not used to calculate ORs). Sensitivity analyses were separately conducted for ORs and these values were aggregated for descriptive purposes and used in meta-regression models.
The need for fixed versus random effects models was considered. Because sampling error was likely not the only source of variation in study effects, and random variation likely existed because the effect sizes meta-analyzed represented a sample of a larger population of effect sizes with an unknown distribution, a random-effects meta-analysis was appropriate (Borenstein, Hedges, Higgins, & Rothstein, 2010). Given the nested data structure (i.e., samples could contribute multiple effect sizes), likelihood ratio tests were computed for unconditional models to assess whether it was necessary to include multilevel random effects (i.e., to explicitly model between- and within-study variation); additional random effects were deemed unnecessary. To pool effects, separate unconditional models were conducted for lifetime and past-year disorders for (1) the prevalence in the SA group, (2) the prevalence in the no-SA group, and (3) the log odds.
To understand disorder-specific heterogeneity, mixed effects models using inverse variance weights were tested within each diagnostic category. Heterogeneity was examined in unconditional models. When significant heterogeneity was observed for a given disorder, a multivariate analysis including all moderators was tested to understand whether the moderators significantly accounted for heterogeneity, and whether ORs differed significantly as a function of moderators.
Results
In all, M = 39 independent samples and K = 171 effects were included, reflecting N = 88,539 participants. Full data and study characteristics are available online (AUTHOR CITATION); study characteristics are listed by study in Table 1.
Table 1:
Study characteristics
| Study | Outcomes | # effects | Sample size* | Comparison group* | Country | Sample type* | % women* | SA time frame* |
|---|---|---|---|---|---|---|---|---|
| Acierno et al. (2007), Boudreaux et al. (1998), Dansky et al. (1997) Kilpatrick et al. (1992), & Resnick et al. (1993) | ANX, DEP, ED, OCD, PTSD, SUD | 15 | 389–4008 | No SA, other trauma (any non-SA trauma) | US | Community | 100.00 | Lifetime |
| Arata (1999) | ANX, BIP, DEP, ED, OCD, PTSD, SUD | 31 | 77–94 | No SA, other trauma (any non-SA trauma) | US | College | 100.00 | Adult/adolescent |
| Badour (2011) | PTSD | 1 | 52 | Other trauma (physical assault) | US | Mixed | 100.00 | Lifetime |
| Betts et al. (2013) | PTSD | 1 | 1318 | Other trauma (any non-SA trauma) | Australia | Community | 51.39 | Lifetime |
| Blanchard et al. (1996) | PTSD | 1 | 40 | Other trauma (motor vehicle accident) | US | Mixed | 92.50 | Missing |
| Breslau et al. (1991) | PTSD | 1 | 394 | Other trauma (any non-SA trauma) | US | Community | 61.67 | Lifetime |
| Burnam et al. (1998) | ANX, BIP, DEP, OCD, SUD | 7 | 864 | No SA | US | Community | 81.94 | Lifetime |
| Cheasty et al. (2002) | DEP | 1 | 237 | No SA | Ireland | Medical | 100.00 | Adult/adolescent |
| Clark et al. (2012) | SUD | 4 | 19415 | No SA | US | Prison inmates | 23.39 | Lifetime |
| Creamer et al. (2001) | PTSD | 1 | 6104 | Other trauma (any non-SA trauma) | Australia | Community | 49.54 | Lifetime |
| Davidson et al. (1996) & Winfield et al. (1990) | ANX, DEP, OCD, SUD | 6 | 1157–2918 | No SA | US | Community | 54.34 & 100.00 | Lifetime |
| Eap (2008) | DEP | 1 | 283 | No SA | US | Community | 52.30 | Lifetime |
| Evans-Campbell et al. (2006) | DEP | 2 | 91 | No interpersonal violence | US | Community | 100.00 | Lifetime |
| Faravelli et al. (2004) | ANX, DEP, ED, PTSD | 4 | 72 | Other trauma (any non-SA trauma) | Italy | Mixed | 100.00 | Past year |
| Frank & Anderson (1987) | ANX, DEP, SUD | 3 | 91–92 | No SA | US | Trauma help-seeking | 100.00 | Past year |
| Freedy, Magruder, Mainous et al. (2010) & Zinzow et al. (2008) | DEP, PTSD, SUD | 5 | 737–865 | Other trauma (any non-SA trauma) | US | Veteran | 21.27 & 21.30 | Lifetime |
| Freedy, Magruder, Zoller et al. (2010) | PTSD | 1 | 40 | No SA | US | Community | 82.38 | Lifetime |
| Gutner et al. (2006) & Resick (1991) | DEP, PTSD, SUD | 5 | 122–190 | Other trauma (physical assault) | US | Trauma help-seeking | 100.00 | Past year |
| Halligan et al. (2003) - study 1 | PTSD | 2 | 81 | Other trauma (physical assault) | UK | Trauma help-seeking | 40.74 | Lifetime |
| Halligan et al. (2003) - study 2 | PTSD | 2 | 73 | Other trauma (physical assault) | UK | Trauma help-seeking | 42.47 | Past year |
| Hapke et al. (2006) | PTSD | 1 | 806 | Other trauma (any non-SA trauma) | Germany | Community | 49.10 | Lifetime |
| Johnson et al. (2010) | PTSD | 1 | 972 | No SA | Congo | Community | 59.42 | Lifetime |
| Kaltman et al. (2005) | DEP, PTSD, SUD | 3 | 125 | No SA | US | College | 100.00 | Adult/adolescent |
| Kaminer et al. (2008) | PTSD | 1 | 2174 | Other trauma (interpersonal violence or abuse) | South Africa | Community | 58.60 | Lifetime |
| Kaysen et al. (2011) | DEP, SUD, PTSD | 5 | 59–63 | Other trauma (physical assault) | US | Community | 100.00 | Past year |
| Kessler et al. (1999) | PTSD | 1 | 3277 | Other trauma (any non-SA trauma) | US | Community | 52.15 | Lifetime |
| Kilpatrick et al. (2007) & Zinzow et al. (2012) | DEP, PTSD, SUD | 11 | 1000–3001 | No SA | US | College & community members | 100.00 | Lifetime & adolescent/adult |
| Lown & Vega (2001) | SUD | 1 | 1501 | No SA | US | Community | 100.00 | Lifetime |
| Martinson (2013) | ANX, DEP, ED, OCD | 6 | 51 | No SA | US | College | 100.00 | Lifetime |
| Masho & Ahmed (2007) | PTSD | 1 | 1769 | No SA | US | Community | 100.00 | Lifetime |
| McCutcheon et al. (2010) | PTSD | 1 | 1638 | Other trauma (any non-SA trauma) | US | Other | 100.00 | Adult/adolescent |
| Norris (1992) | PTSD | 1 | 947 | Other trauma (any non-SA trauma) | US | Community | 50.00 | Lifetime |
| Read et al. (2012) | PTSD | 1 | 576 | No SA | US | College | 64.99 | Lifetime |
| Sadler et al. (2012) | SUD | 2 | 959–1012 | No SA | US | Veteran | 100.00 | Lifetime |
| Testa et al. (2007) | DEP, SUD | 3 | 1014 | No SA | US | Community | 100.00 | Past year |
| Thompson et al. (2003) & Wonderlich & Crosby (2001) | ANX, ED, SUD | 6 | 97 | No SA | US | Mixed | 100.00 | Adult/adolescent |
| Walker et al. (1995) | ANX, DEP, OCD, SUD | 10 | 89 | No SA | US | Medical | 100.00 | Lifetime |
| Xu et al. (2013) | ANX, BIP, DEP, PTSD, SUD | 20 | 31,835–31,875 | No SA | US | Community | 50.01 | Adult/adolescent |
| Zlotnick et al. (2006) | PTSD | 2 | 1032–2390 | No SA, other trauma (any non-SA trauma) | Chile | Community | 43.70 | Lifetime |
Study characteristics varied by effect and/or source in which study results were reported.
ANX = anxiety disorders, BIP = bipolar disorder, DEP = depressive disorders, ED = eating disorders, OCD = obsessive compulsive disorder, PTSD = trauma and stressor-related disorders, SUD = substance use disorders
Publication Bias
Untruncated ORs from published studies (85.4% of ORs) were used to create a funnel plot (Figure 2). No statistically-significant asymmetry was observed, z = −1.74, p = .08.
Figure 2:
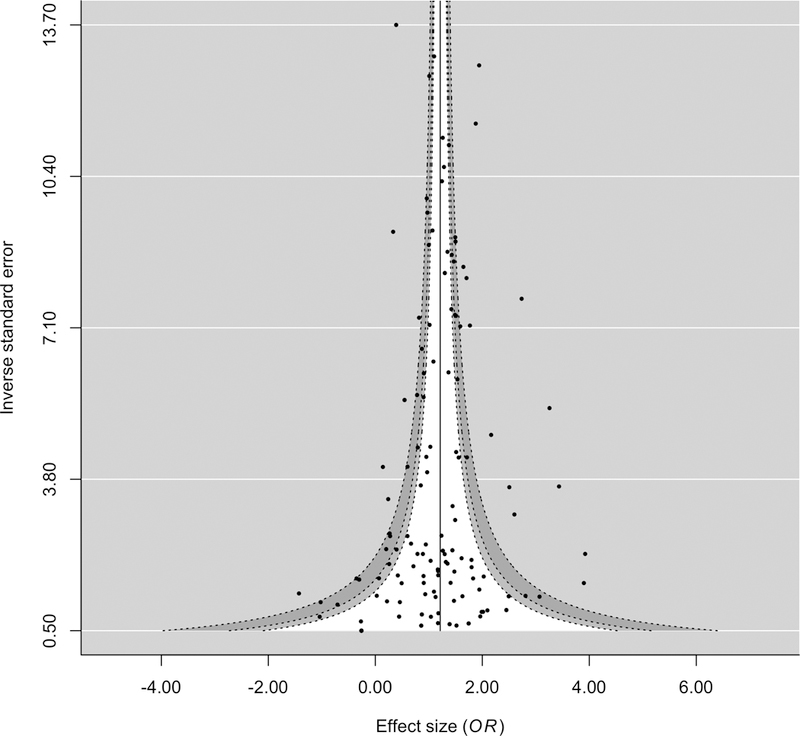
Funnel Plot
Prevalence Estimates and Odds Ratios by Diagnostic Category
Forest plots are presented for each diagnostic category in Supplemental Figures 1–7. Summary prevalence estimates and odds ratios by diagnosis are presented in Table 2. Prevalence estimates and ORs were calculated in two ways for each lifetime and past-year diagnosis. First, overall models that included all effect sizes, regardless of comparison group type (i.e., no SA exposure, non-SA trauma exposure, no interpersonal violence exposure), were run to generate an overall OR, overall percentage of the SA groups with the diagnosis, and overall percentage of the no-SA groups with the diagnosis. Second, separate models were run for studies using each comparison group type, which yielded comparison-group-specific ORs and percentages of the no-SA groups with each diagnosis; results from these models are presented in Table 2.
Table 2.
Aggregated Prevalence and Odds Ratios
| Lifetime Diagnoses (k = 103) | m | k | I2 | Overall OR | % with disorder in SA group | % with disorder in comparison groups and group-specific odds ratios |
||
|---|---|---|---|---|---|---|---|---|
| No SA exposure | Other (non-SA) trauma exposure | No interpersonal violence exposure | ||||||
| Anxiety disorders | 9 | 21 | 63.64 | 2.59** | 20.0% | 9.4% (k = 20; OR = 2.54**) | N/A | N/A |
| Generalized anxiety disorder | 5 | 5 | 52.24 | 2.85** | 32.2% | 19.3% (k = 5; OR = 2.85**) | N/A | N/A |
| Specific phobia | 3 | 3 | 89.03 | 2.10 | 14.9% | 8.5% (k = 3; OR = 2.10) | N/A | N/A |
| Panic disorder | 5 | 6 | 49.45 | 2.23* | 7.4% | 3.6% (k = 6; OR = 2.23*) | N/A | N/A |
| Social anxiety disorder | 3 | 3 | 22.04 | 2.21** | 12.7% | 6.0% (k = 3; OR = 2.21**) | N/A | N/A |
| Agoraphobia | 2 | 2 | 0.00 | 1.44 | 20.7% | 16.2% (k = 2; OR = 1.44) | N/A | N/A |
| Bipolar conditions | 3 | 3 | 0.00 | 3.51** | 8.7% | 2.5% (k = 3; OR = 3.51**) | N/A | N/A |
| Depressive disorders | 16 | 23 | 63.23 | 3.44** | 38.8% | 13.2% (k = 18; OR = 3.53**) | 40.2% (k = 3; OR = 2.16) | 27.0% (k = 2; OR = 6.62**) |
| Dysthymia | 4 | 4 | 57.35 | 2.67* | 14.2% | 3.2% (k = 3; OR = 2.00) | N/A | N/A |
| Major depressive episode | 4 | 6 | 55.38 | 4.41** | 31.9% | 9.0% (k = 6; OR = 4.41**) | N/A | N/A |
| Major depressive disorder | 12 | 12 | 0.00 | 2.99** | 49.6% | 19.6% (k = 8; OR = 1.22**) | 40.2% (k = 3; OR = 2.16) | N/A |
| Eating disorders | 5 | 9 | 0.73 | 1.92** | 8.2% | 1.7% (k = 8; OR = 1.83**) | N/A | N/A |
| Bulimia nervosa | 3 | 3 | 0.00 | 2.40** | 8.2% | 2.1% (k = 3; OR = 2.40**) | N/A | N/A |
| Binge eating disorder | 2 | 2 | 0.00 | 1.01 | 10.4% | 1.0% (k = 2; OR = 1.01) | N/A | N/A |
| Anorexia nervosa | 2 | 2 | 0.00 | 4.44 | 6.1% | 1.5% (k = 2; OR = 4.44) | N/A | N/A |
| Obsessive-compulsive disorder | 5 | 5 | 0.00 | 4.54** | 5.5% | 1.7% (k = 5; OR = 4.54**) | N/A | N/A |
| Posttraumatic stress disorder | 17 | 21 | 96.80 | 7.57** | 36.2% | 7.0% (k = 12; OR = 10.73**) | 12.1% (k = 9; OR = 4.40**) | N/A |
| Substance use disorders | 13 | 21 | 64.38 | 2.14** | 19.4% | 9.1% (k = 18; OR = 2.30**) | 11.7% (k = 3; OR = 0.86) | N/A |
| Drug use disorder | 6 | 6 | 0.00 | 3.43** | 15.1% | 4.5% (k = 6; OR = 3.43**) | N/A | N/A |
| Alcohol use disorder | 10 | 12 | 35.30 | 1.75** | 18.0% | 9.1% (k = 9; OR = 1.87**) | 11.7% (k = 3; OR = 0.86) | N/A |
| Past-Year Diagnoses (k = 68) | m | k | I2 | Overall OR | % with disorder in SA group | % with disorder in comparison groups and group-specific odds ratios |
||
| No SA exposure | Other (non-SA) trauma exposure | No interpersonal violence exposure | ||||||
| Anxiety disorders | 5 | 16 | 64.63 | 2.79** | 7.3% | 2.6% (k = 15; OR = 2.86**) | N/A | N/A |
| Generalized anxiety disorder | 2 | 2 | 0.00 | 3.66** | 9.4% | 3.1% (k = 2; OR = 3.66**) | N/A | N/A |
| Specific phobia | 3 | 3 | 78.29 | 1.53 | 12.8% | 6.5% (k = 3; OR = 1.53) | N/A | N/A |
| Panic disorder | 4 | 5 | 20.06 | 3.48** | 4.6% | 1.9% (k = 5; OR = 3.48**) | N/A | N/A |
| Social anxiety disorder | 3 | 3 | 0.00 | 3.10** | 6.9% | 2.1% (k = 3; OR = 3.10**) | N/A | N/A |
| Agoraphobia | 2 | 2 | 6.13 | 5.17* | 3.3% | 1.0% (k = 2; OR = 5.17*) | N/A | N/A |
| Bipolar conditions | 2 | 2 | 0.00 | 4.33** | 8.6% | 2.9% (k = 2; OR = 4.33**) | N/A | N/A |
| Depressive disorders | 9 | 12 | 64.98 | 3.10** | 23.8% | 8.7% (k = 10; OR = 3.33**) | 25.6% (k = 2; OR = 3.21) | N/A |
| Dysthymia | 2 | 2 | 0.00 | 2.74** | 1.7% | 0.6% (k = 2; OR = 2.74**) | N/A | N/A |
| Major depressive episode | 2 | 3 | 0.00 | 4.35** | 23.6% | 6.7% (k = 3; OR = 4.35**) | N/A | N/A |
| Major depressive disorder | 7 | 7 | 27.25 | 2.43** | 30.7% | 13.5% (k = 5; OR = 2.73**) | 25.6% (k = 2; OR = 3.21) | N/A |
| Eating disorders | 1 | 2 | 0.00 | 1.51 | 1.4% | 1.2% (k = 2; OR = 1.51) | N/A | N/A |
| Bulimia nervosa | 1 | 1 | N/A | N/A | N/A | N/A | N/A | N/A |
| Binge eating disorder | 0 | 0 | N/A | N/A | N/A | N/A | N/A | N/A |
| Anorexia nervosa | 1 | 1 | N/A | N/A | N/A | N/A | N/A | N/A |
| Obsessive-compulsive disorder | 2 | 2 | 0.00 | 5.80** | 7.7% | 1.9% (k = 2; OR = 5.80**) | N/A | N/A |
| Posttraumatic stress disorder | 16 | 19 | 85.58 | 3.01** | 25.9% | 10.2% (k = 11; OR = 4.11**) | 25.1% (k = 8; OR = 2.06**) | N/A |
| Substance use disorders | 8 | 15 | 92.55 | 1.75** | 12.7% | 7.6% (k = 13; OR = 1.76**) | 6.8% (k = 2; OR = 1.73) | N/A |
| Drug use disorder | 6 | 7 | 96.69 | 2.04** | 14.2% | 9.2% (k = 7; OR = 2.04**) | N/A | N/A |
| Alcohol use disorder | 6 | 6 | 0.00 | 1.51** | 13.3% | 5.4% (k = 5; OR = 1.50**) | N/A | N/A |
Note. p < .05,
p < .01.
OR = odds ratio. Each percentage and OR was calculated by aggregating relevant studies where k ≥ 2 in a separate unconditional model. I2 = total amount of variance attributable to heterogeneity rather than sampling error in the null model summarizing ORs; I2 values were calculated from overall OR models (i.e., across comparison group types). Outliers were identified and truncated separately for each overall model where k ≥ 5. k = number of unique effects; m = number of samples.
Anxiety disorders.
The pooled prevalence of lifetime anxiety disorders was 20% (95% CI: 12%−28%) for SA groups versus 10% (95% CI: 6%−13%) across all types of no-SA groups; OR = 2.59, p < .001. The pooled prevalence of past-year anxiety disorders was 7% (95% CI: 5%−10%) for SA groups versus 3% (95% CI: 2%−4%) across no-SA groups; OR = 2.79, p < .001. Statistically-significant overall ORs were observed for lifetime and past-year generalized anxiety disorder, social anxiety disorder, and panic disorder. The overall OR for past-year, but not lifetime agoraphobia was statistically significant, and neither overall OR for specific phobia was significant.
Bipolar disorder.
The pooled prevalence of lifetime bipolar disorders was 9% (95% CI: 0%−18%) for SA groups versus 2% (95% CI: 0%−6%) across no-SA groups; OR = 3.51, p < .001. Similarly, the pooled prevalence of past-year bipolar disorders was 9% (95% CI: 2%−15%) for SA groups versus 3% (95% CI: 3%−3%) across no-SA groups; OR = 4.33, p < .001.
Depressive disorders.
The pooled prevalence of lifetime depressive disorders was 39% (95% CI: 29%−48%) for SA groups versus 17% (95% CI: 12%−23%) across no-SA groups; OR = 3.44, p < .001. The pooled prevalence of past-year depressive disorders was 24% (95% CI: 13%−35%) for SA groups versus 11% (95% CI: 5%−16%) across no-SA groups; OR = 3.10, p < .001. Statistically-significant overall ORs were observed for lifetime and past-year dysthymia, major depressive episodes, and major depressive disorder.
Eating disorders.
The pooled prevalence of lifetime eating disorders was 8% (95% CI: 3%−13%) for SA groups versus 2% (95% CI: 1%−3%) across no-SA groups; OR = 1.92, p < .001. The pooled prevalence of past-year eating disorders was 1% (95% CI: 0%−4%) for SA groups versus 1% (95% CI: 0%−4%) across no-SA groups; OR = 1.51, p = .75. ORs for specific eating disorder diagnoses were only summarized for lifetime diagnoses due to low frequency of effect sizes for past-year diagnoses. Of these, a statistically-significant overall OR was observed only for lifetime bulimia nervosa.
Obsessive-compulsive disorder.
The pooled prevalence of lifetime obsessive-compulsive disorder was 6% (95% CI: 3%−8%) for SA groups versus 2% (95% CI: 1%−3%) across no-SA groups; OR = 4.54, p < .001. The pooled prevalence of past-year obsessive-compulsive disorder was 8% (95% CI: 2%−14%) for SA groups versus 2% (95% CI: 0%−3%) across no-SA groups; OR = 5.80, p < .001.
PTSD.
The pooled prevalence of lifetime PTSD was 36% (95% CI: 31%−41%) for SA groups versus 9% (95% CI: 6%−11%) across no-SA groups; OR = 7.57, p < .001. The prevalence of past-year PTSD was 26% (95% CI: 20%−32%) for SA groups versus 18% (95% CI: 11%−26%) across no-SA groups; OR = 3.01, p < .001.
Substance use disorders.
The prevalence of lifetime substance use disorders was 19% (95% CI: 15%−24%) for SA groups versus 9% (95% CI: 6%−12%) across no-SA groups; OR = 2.14, p < .001. The prevalence of past-year substance use disorders was 13% (95% CI: 7%−19%) for SA groups versus 7% (95% CI: 4%−11%) across no-SA groups; OR = 1.75, p < .001. Significant overall ORs were observed for lifetime and past-year drug and alcohol use disorders.
Moderator Analyses
Summary ORs for moderators characterizing diagnoses within groups (i.e., diagnosis type, past year versus lifetime diagnosis, comparison group) are included in Table 2; summary ORs within other moderators (i.e., sample type, time frame of SA victimization) are presented in Table 3. In meta-regressions of log ORs, statistically-significant heterogeneity was observed in the null model for anxiety disorders, Q(36) = 75.00, p < .001, depressive disorders, Q(34) = 82.19, p < .0001, PTSD, Q(39) = 471.91, p < .001, and substance use disorders, Q(35) = 333.12, p < .001, but not bipolar disorders, Q(4) = 2.69, p = .61, disordered eating, Q(10) = 7.01, p = .72., or OCD, Q(6) = 0.70, p = .99. Moderators were tested for disorder types with significant heterogeneity; analyses are presented in Table 4.
Table 3.
Summarized Odds Ratios by Study Characteristics
| Anxiety | Bipolar | Depressive | Eating | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| k | OR | % SA | % no SA | k | OR | % SA | % no SA | k | OR | % SA | % no SA | k | OR | % SA | % no SA | |
| Sample type | ||||||||||||||||
| Community | 15 | 3.12** | 12.7% | 4.5% | 3 | 3.87** | 10.2% | 3.0% | 18 | 3.71** | 30.3% | 12.8% | 2 | 1.45 | 2.6% | 1.5% |
| College | 14 | 1.12 | 3.0% | 2.7% | 2 | 4.81 | 5.5% | 1.2% | 8 | 4.21** | 23.8% | 8.5% | 5 | 1.42 | 1.7% | 1.6% |
| Medical | 4 | 1.92** | 32.5% | 19.1% | 0 | N/A | N/A | N/A | 4 | 2.34** | 55.4% | 24.0% | 0 | N/A | N/A | N/A |
| Veteran | 1 | 2.21** | 10.5% | 3.9% | 0 | N/A | N/A | N/A | 1 | 2.62** | 34.3% | 16.6% | 0 | N/A | N/A | N/A |
| Trauma help-seeking | 1 | 3.18* | 29.4%2 | 32.3% | 0 | N/A | N/A | N/A | 3 | 1.51 | 38.1% | 27.4% | 0 | N/A | N/A | N/A |
| Other | 2 | 2.44** | 51.5% | 15.6% | 0 | N/A | N/A | N/A | 1 | 3.86** | 75.0% | 43.8% | 4 | 2.12* | 16.3% | 3.8% |
| Time frame of SA victimization | ||||||||||||||||
| Lifetime SA | 15 | 2.26** | 16.5% | 7.4% | 1 | 8.13* | 1.9% | 0.2% | 16 | 3.87** | 34.8% | 11.2% | 3 | 1.40 | 3.4% | 1.6% |
| Adolescent/adult SA | 20 | 3.05** | 11.1% | 4.7% | 4 | 3.85** | 10.6% | 3.2% | 12 | 3.25** | 22.1% | 9.0% | 7 | 1.98* | 7.6% | 1.8% |
| Past-year SA | 2 | 3.20** | 31.8% | 23.1% | 0 | N/A | N/A | N/A | 7 | 2.53** | 51.2% | 33.7% | 1 | 2.82 | 13.0% | 6.3% |
| OCD | PTSD | SUD | ||||||||||||||
| k | OR | % SA | % no SA | k | OR | % SA | % no SA | k | OR | % SA | % no SA | |||||
| Sample type | ||||||||||||||||
| Community | 3 | 4.58** | 6.5% | 1.6% | 21 | 7.06** | 31.4% | 8.8% | 17 | 2.12** | 14.0% | 6.1% | ||||
| College | 3 | 4.60 | 6.4% | 1.5% | 7 | 3.68** | 30.0% | 10.7% | 5 | 1.85 | 7.4% | 4.0% | ||||
| Medical | 1 | 6.22** | 8.3% | 8.7% | 1 | 4.53** | 51.5% | 18.9% | 2 | 3.78** | 22.6% | 6.7% | ||||
| Veteran | 0 | N/A | N/A | N/A | 2 | 1.58* | 21.3% | 14.9% | 3 | 1.45 | 17.9% | 11.9% | ||||
| Trauma help-seeking | 0 | N/A | N/A | N/A | 5 | 2.21* | 42.0% | 27.9% | 3 | 2.01 | 16.3% | 8.9% | ||||
| Other | 0 | N/A | N/A | N/A | 4 | 2.25 | 29.1% | 27.4% | 6 | 1.82** | 27.6% | 17.5% | ||||
| Time frame of SA victimization | ||||||||||||||||
| Lifetime SA | 5 | 4.85** | 7.3% | 1.7% | 24 | 5.36** | 32.1% | 10.9% | 16 | 1.87** | 17.7% | 9.2% | ||||
| Adolescent/adult SA | 2 | 4.81 | 5.5% | 1.2% | 10 | 5.59** | 29.1% | 7.1% | 13 | 2.16** | 12.1% | 6.5% | ||||
| Past-year SA | 0 | N/A | N/A | N/A | 5 | 3.32* | 36.7% | 28.7% | 7 | 1.74* | 21.7% | 9.8% | ||||
Note. p < .05,
p < .01.
k = number of unique effects, OR = odds ratio obtained from unconditional model, OCD = obsessive compulsive disorder, PTSD = trauma and stressor-related disorders, SUD = substance use disorders
Table 4.
Moderator Analyses
| Anxiety disorders (m = 37) | OR | SE(OR) | 95% CI | p |
|---|---|---|---|---|
| Intercept | 3.25** | 1.25 | 2.12, 5.00 | 0.00 |
| College student sample (versus community sample) | 0.36** | 1.36 | 0.20, 0.65 | 0.00 |
| Medical sample (versus community sample) | 0.59 | 1.39 | 0.31, 1.13 | 0.11 |
| Veteran sample (versus community sample) | 0.37 | 2.29 | 0.07, 1.90 | 0.24 |
| Trauma help-seeking sample (versus community sample) | 0.98 | 1.79 | 0.31, 3.06 | 0.97 |
| Other type sample (versus community sample) | 0.57 | 1.61 | 0.22, 1.44 | 0.23 |
| Other trauma comparison group (versus no sexual assault) | 1.76 | 2.19 | 0.38, 8.21 | 0.47 |
| Adult/adolescent SA (versus past year) | 1.14 | 1.21 | 0.79, 1.67 | 0.48 |
| Past year diagnoses (versus lifetime) | 1.03 | 1.14 | 0.80, 1.34 | 0.81 |
| Agoraphobia (versus generalized anxiety disorder) | 0.99 | 1.56 | 0.42, 2.37 | 0.99 |
| Panic disorder (versus generalized anxiety disorder) | 1.01 | 1.20 | 0.70, 1.45 | 0.97 |
| Specific phobia (versus generalized anxiety disorder) | 0.68* | 1.20 | 0.48, 0.96 | 0.03 |
| Social anxiety (versus generalized anxiety disorder) | 0.80 | 1.22 | 0.55, 1.17 | 0.25 |
| Depressive disorders (m = 35) | OR | SE(OR) | 95% CI | p |
| Intercept | 3.24** | 1.15 | 2.47, 4.24 | 0.00 |
| College student sample (versus community sample) | 1.06 | 1.13 | 0.83, 1.35 | 0.63 |
| Medical sample (versus community sample) | 0.75 | 1.33 | 0.43, 1.31 | 0.31 |
| Veteran sample (versus community sample) | 1.08 | 1.31 | 0.64, 1.82 | 0.77 |
| Trauma help-seeking sample (versus community sample) | 0.39* | 1.53 | 0.17, 0.90 | 0.03 |
| Other type sample (versus community sample) | 1.04 | 1.95 | 0.28, 3.83 | 0.96 |
| No-interpersonal-violence comparison group (versus no sexual assault) | 2.70* | 1.49 | 1.25, 5.87 | 0.01 |
| Other trauma comparison group (versus no sexual assault) | 1.15 | 1.54 | 0.49, 2.68 | 0.75 |
| Adult/adolescent SA (versus past year) | 0.93 | 1.16 | 0.69, 1.25 | 0.64 |
| Lifetime SA (versus past year) | 0.79 | 1.19 | 0.56, 1.12 | 0.18 |
| Past year diagnoses (versus lifetime) | 0.95 | 1.08 | 0.81, 1.10 | 0.48 |
| Dysthymia (versus major depressive disorder) | 0.90 | 1.14 | 0.69, 1.17 | 0.42 |
| Nonspecific depressive disorder effects (versus major depressive disorder) | 1.91 | 1.72 | 0.66, 5.49 | 0.23 |
| Major depressive episode (versus major depressive disorder) | 1.69** | 1.11 | 1.39, 2.07 | 0.00 |
| PTSD (m = 39) | OR | SE(OR) | 95% CI | p |
| Intercept | 16.52** | 1.95 | 4.47, 61.08 | 0.00 |
| College student sample (versus community sample) | 0.70 | 1.51 | 0.31, 1.57 | 0.39 |
| Medical sample (versus community sample) | 0.86 | 2.26 | 0.17, 4.25 | 0.85 |
| Veteran sample (versus community sample) | 0.33 | 1.87 | 0.10, 1.13 | 0.08 |
| Trauma help-seeking sample (versus community sample) | 0.39 | 1.94 | 0.11, 1.44 | 0.16 |
| Other type sample (versus community sample) | 0.87 | 1.85 | 0.26, 2.89 | 0.81 |
| Other trauma comparison group (versus no sexual assault) | 0.59 | 1.41 | 0.30, 1.15 | 0.12 |
| Adult/adolescent SA (versus past year) | 0.56 | 1.98 | 0.15, 2.14 | 0.40 |
| Lifetime SA (versus past year) | 0.68 | 1.87 | 0.20, 2.33 | 0.54 |
| Past year diagnoses (versus lifetime) | 0.47* | 1.33 | 0.27, 0.82 | 0.01 |
| Substance use disorders (m = 36) | OR | SE(OR) | 95% CI | p |
| Intercept | 2.20** | 1.31 | 1.30, 3.73 | 0.00 |
| College student sample (versus community sample) | 0.92 | 1.59 | 0.37, 2.28 | 0.85 |
| Medical sample (versus community sample) | 1.72 | 1.84 | 0.52, 5.67 | 0.37 |
| Veteran sample (versus community sample) | 0.28 | 2.37 | 0.05, 1.54 | 0.14 |
| Trauma help-seeking sample (versus community sample) | 0.93 | 1.77 | 0.30, 2.83 | 0.90 |
| Other type sample (versus community sample) | 0.57 | 1.47 | 0.27, 1.20 | 0.14 |
| Other trauma comparison group (versus no sexual assault) | 0.56 | 1.55 | 0.23, 1.32 | 0.18 |
| Adult/adolescent SA (versus past year) | 0.79 | 1.44 | 0.39, 1.60 | 0.51 |
| Lifetime SA (versus past year) | 0.92 | 1.41 | 0.47, 1.82 | 0.82 |
| Past year diagnoses (versus lifetime) | 0.98 | 1.30 | 0.59, 1.62 | 0.93 |
| Drug use disorder (versus alcohol use disorder) | 1.59* | 1.23 | 1.05, 2.40 | 0.03 |
Note. OR = odds ratio, SE(OR) = standard error of odds ratio, CI = confidence interval.
p < .05,
p < .01
Anxiety disorders.
Heterogeneity in ORs for anxiety disorders was sufficiently accounted for by moderators, QE(24) = 29.05, p = .22. Type of sample was a significant moderator of effects, such that college samples exhibited significantly lower ORs than community samples. Disorder type was also a significant moderator, such that ORs were significantly lower for specific phobia as compared to generalized anxiety disorder.
Depressive disorders.
In a multivariate moderator analysis of ORs reflecting depressive disorders, heterogeneity was sufficiently accounted for by moderators, QE(21) = 16.04, p = .77. Sample type was a significant moderator: trauma help-seeking samples had significantly smaller ORs than community samples. Comparison group type was a significant moderator, such that ORs were significantly larger in studies comparing people who had experienced SA to people who had not experienced any interpersonal violence, relative to those comparing people who had experienced SA to people who had not experienced SA. Disorder type was also a significant moderator, such that ORs were significantly larger for major depressive episodes than major depressive disorder.
PTSD.
In the moderation analysis for PTSD, residual heterogeneity remained significant, QE(29) = 314.55, p < .001. Only diagnosis time frame was a significant moderator, such that ORs for past-year diagnoses were significantly smaller than ORs for lifetime diagnoses.
Substance use disorders.
Heterogeneity remained significant in the model with moderators, QE(24) = 260.30, p < .001. Disorder type was a significant moderator, such that ORs for drug use disorders were significantly larger than those for alcohol use disorder.
Discussion
In the first quantitative review of the prevalence of specific DSM-defined mental disorders in survivors of SA, findings indicate that SA is associated with increased risk for most disorders tested. The primary goal of this meta-analysis was to summarize the prevalence of a variety of lifetime and past-year mental disorders in people exposed to SA and people without a history of SA, which was accomplished using 171 estimates obtained from diagnostic interviews with 88,539 participants. Nearly every study included found a higher prevalence for mental disorders among people who had been sexually assaulted than in people who had not been assaulted. Significantly higher risk associated with SA was identified for all anxiety disorders (except for specific phobia and lifetime agoraphobia), all depressive disorders, lifetime bulimia nervosa, obsessive-compulsive disorder, PTSD, and all substance use disorders.
Among people who have been sexually assaulted, depressive disorders and PTSD appear to be particularly common. About one third of people exposed to SA evidenced lifetime (36%) or past-year (26%) PTSD, more than one third evidenced lifetime depressive disorders (39%), and almost a quarter evidenced past-year depressive disorders (24%). This is consistent with epidemiological studies: estimates for PTSD have ranged from 31% to 52% in survivors’ lifetime (Kessler et al., 1999; Kilpatrick, Edmunds, & Seymour, 1992; Xu et al., 2013; Zinzow et al., 2012) and 11% to 36% in the past year (Creamer, Burgess, & McFarlane, 2001; Xu et al., 2013; Zinzow et al., 2012), and estimates for major depressive episodes/disorder have ranged from 30% to 43% in SA survivors’ lifetime (Kilpatrick et al., 1992; Xu et al., 2013; Zinzow et al., 2012) and 13% to 36% in the past year (Xu et al., 2013; Zinzow et al., 2012). Service providers should screen for these conditions in patients exposed to SA and be prepared with high-quality referral options. Each of these conditions are highly treatable using short-term cognitive behavioral therapies. Evidence-based treatments for PTSD include cognitive processing therapy (Resick, Monson, & Chard, 2014) and prolonged exposure (Rothbaum, Foa, & Hembree, 2007); evidence-based treatments for depression include cognitive therapy (Beck, Rush, Shaw, & Emery, 1979) and behavioral activation (Lejuez, Hopko, & Hopko, 2001). These treatments are associated with substantial reductions in symptoms within 12–16 sessions (Bradley, Greene, Russ, Dutra, & Westen, 2005; Cuijpers, van Straten, Andersson, & van Oppen, 2008; Hofmann, Asnaani, Vonk, Sawyer, & Fang, 2012; Mazzucchelli, Kane, & Rees, 2009; Mendes, Mello, Ventura, de Medeiros Passarela, & de Jesus Mari, 2008; Powers, Halpern, Ferenschak, Gillihan, & Foa, 2010) and thus represent efficient and cost-effective strategies to address these conditions. There also is some promising evidence that PTSD can be prevented after SA (Dworkin & Schumacher, 2016) and other forms of trauma (Kornør et al., 2008; Litz, Gray, Bryant, & Adler, 2002) through early intervention, but this has not been investigated for depression. Service providers responding in the immediate aftermath of SA exposure (e.g., rape crisis advocates) provide a front line for disseminating such interventions.
Although it is not possible to conclude from observational data that SA causes mental disorders, this review provides further evidence of their association across specific mental disorders. There are multiple possible explanations for the observed relationships (Dworkin et al., 2017). First, it is possible that SA increases vulnerability to the development of mental disorders. SA might cause the onset of mental disorders in otherwise healthy individuals, trigger the expression of a genetic liability, or worsen subthreshold forms of psychopathology to diagnostic level. Second, mental disorders could increase risk for SA victimization (Orcutt, Erickson, & Wolfe, 2002; Pineles, Shipherd, Welch, & Yovel, 2007), potentially because people with mental disorders are targeted by perpetrators. It also is important to note that both lifetime and past-year mental disorders are reflected in this analysis; in the case of lifetime disorders especially, it is possible that SA exposure occurred after the onset of a mental disorder. The significantly increased risk for past-year mental disorders provides stronger evidence of the causal association between SA and mental disorders. However, prospective studies and meta-analyses of these studies are needed to clarify the causal direction of observed relationships.
Moderators of Disorder-Specific Risk Associated with Sexual Assault
A secondary goal of this review was to identify moderators that could alter the degree to which risk for various mental disorders are higher in survivors of SA. Moderators were tested in four diagnostic categories: anxiety disorders, depressive disorders, PTSD, and substance use disorders. It was notable that group differences in most diagnostic categories were relatively robust to differences in characteristics of studies (i.e., comparison group type, sample type, time frame of SA) and effects (i.e., time frame of diagnosis, specific type of disorder). However, several significant moderators were observed that could guide future disorder-specific research on the effects of SA.
Sample type.
Several sample types evidenced different risk for diagnosis of specific disorders associated with SA when other moderators were controlled for. First, relative to community samples, effect sizes were smaller for anxiety disorders in college students. This may indicate that students most severely affected by anxiety disorders associated with SA may be less likely to enter college or more likely to leave college than those without anxiety disorders. This was somewhat surprising, as prior studies failed to find associations between anxiety disorders and failure to enter college or college dropout (Breslau et al., 2008). It is possible that anxiety disorders that develop subsequent to experiences of campus SA involve avoidance of college-specific stimuli (e.g., attending class) that could increase likelihood of dropout, whereas anxiety disorders not associated with SA or associated with non-campus SA may interfere less. Second, relative to community samples, trauma-help-seeking samples evidenced lower effect sizes for depressive disorders. This smaller group difference appeared to be driven by higher rates of depressive disorders in the comparison groups (which were comprised of survivors of physical assault in two of the three effects representing trauma-help-seeking samples), rather than lower rates of depression in the SA group. However, because these samples included individuals seeking help for SA and other forms of trauma within a year of trauma exposure, it also is possible that group differences in depressive disorders might emerge later in time. The latency of post-SA depression should be investigated in future prospective research.
Comparison group type.
Results from this analysis indicate that SA is associated with relatively higher risk for PTSD than other forms of trauma. Significant odds ratios were observed for studies comparing survivors of SA to people who had experienced other forms of trauma (in most cases, comparison groups were comprised of survivors of any non-SA trauma or survivors of physical assault). According to multivariate analyses controlling for other moderators, these odds ratios were similar in magnitude to odds ratios from studies using comparison groups comprised of people who had not experienced sexual assault. This is consistent with past research suggesting that SA may be significantly more harmful than other forms of trauma in terms of PTSD outcomes (Kelley et al., 2009; Kessler et al., 1995). However, for other types of disorders, no significant effects were observed when comparing survivors of SA to survivors of other forms of trauma. Because these calculations were based on very small numbers of studies, more research is needed in this area to conclude whether SA is relatively more deleterious in terms of non-PTSD sequelae.
Time frame of sexual assault.
In multivariate models controlling for other moderators, similar risk for specific mental disorders was observed regardless of whether studies assessed SA that had occurred in the past year, in adolescence/adulthood, or at any point in the lifespan. Importantly, this analysis did not directly compare survivors of past-year SA with survivors of assaults that had occurred more than a year prior, as survivors of past-year SA could be included in studies of lifetime or adolescent/adult SA. As a result, the degree to which increased risk for these disorders necessarily endures over time cannot be concluded from this study. Instead, this finding indicates that widening the range of how far in the past SA could have occurred does not reduce survivors’ relatively increased risk for anxiety disorders, depressive disorders, PTSD, or substance use disorders. Past research has indicated that risk for PTSD is highest in the months following SA and reduces over the first year post-assault (Frazier, Conlon, & Glaser, 2001), and studies of other traumas indicate that PTSD remission likelihood decreases after the one-year mark (Breslau, 2009). However, most research has not followed survivors for longer than a year, and as a result, it remains unclear how time since SA affects risk for various mental disorders. Future research should follow survivors prospectively to assess the degree to which diagnostic criteria for various disorders are met over time.
Type of disorder.
Some differences in risk for specific disorders within diagnostic categories were observed when controlling for other moderators. First, for the anxiety disorders, ORs for specific phobia (lifetime OR = 2.10, past-year OR = 1.53) were significantly smaller than for generalized anxiety disorder (lifetime OR = 2.85, past-year OR = 3.66). This may indicate that, of the anxiety disorders, specific phobia is relatively less trauma-related. When survivors of SA develop fear and avoidance of specific trauma-related stimuli, this is considered to be a symptom of PTSD rather than specific phobia; anxiety disorders are only diagnosed when the associated symptoms are not associated with a specific traumatic event (American Psychiatric Association, 2013). Although SA survivors may experience general increases in anxious arousal that could manifest as other anxiety disorders, it is possible that it is relatively rare for this to manifest narrowly as fear towards a non-trauma-related stimulus, as necessary for a diagnosis of specific phobia. Second, for the depressive disorders, ORs for major depressive episode (lifetime OR = 4.41, past-year OR = 4.35) were significantly larger than those for major depressive disorder (lifetime OR = 2.99, past-year OR = 2.43). This is likely due to the lower bar needed to meet criteria for a major depressive episode than major depressive disorder, as a diagnosis of major depressive disorder requires at least one major depressive episode that is not better explained by another condition, without the presence of manic episodes that would indicate bipolar disorder (American Psychiatric Association, 2013). It is possible that some survivors who evidenced a major depressive episode would ultimately have been diagnosed with a disorder other than major depressive disorder if those criteria were applied. Finally, for the substance use disorders, ORs for drug use disorders (lifetime OR = 3.43, past-year OR = 2.04) were significantly larger than those for alcohol use disorder (lifetime OR = 1.75, past-year OR = 1.51). It is possible that drugs are more likely than alcohol to be used for self-medication—indeed, different patterns of use of alcohol and drugs for self-medication are observed across the anxiety disorders (Robinson, Sareen, Cox, & Bolton, 2009)—or that dependence is more likely to develop following habitual self-medication with drugs than alcohol. Alternatively, given prior research suggesting that drug use, but not alcohol use, prospectively increases risk of physical/sexual assault (Kilpatrick, Acierno, Resnick, Saunders, & Best, 1997), it is possible that the higher ORs seen for drug use disorders relative to alcohol use disorders indicate that drug use disorders are a stronger risk factor for SA.
Past year versus lifetime diagnoses.
Diagnosis time frame was a significant moderator of ORs for PTSD only, such that SA survivors’ relative odds of receiving a diagnosis of past-year PTSD (OR = 3.01) was lower than their risk of meeting criteria for PTSD in their lifetime (OR = 7.57) in multivariate models controlling for other moderators. Because studies differed in terms of when assaults could have occurred, findings could be, in part, driven by survivors of an assault that occurred more than a year prior who met criteria for PTSD in the months following assault but whose symptoms remitted. Indeed, 63% of survivors meet diagnostic criteria two months after SA (Frazier et al., 2001). Similar post-SA spikes in risk might not be evident for other conditions, or their symptoms may be better accounted for by a diagnosis of PTSD. This should be investigated in future research.
Strengths & Limitations
This meta-analysis had several strengths, including a comprehensive study identification strategy that resulted in the inclusion of a large number of studies and many unpublished effects. The selection of studies that used high-quality diagnostic interviews is also a strength, as studies that use lower-quality methods to assess psychopathology—such as unpublished self-report measures unvalidated against DSM diagnostic criteria—may result in over- or under-diagnosis (e.g., Foa, Cashman, Jaycox, & Perry, 1997; Griffin, Uhlmansiek, Resick, & Mechanic, 2004). However, this study had limitations. First, estimates for several diagnostic categories, including bipolar conditions, obsessive-compulsive disorder, and eating disorders, were based on a small number of effects, which precluded testing moderation for these conditions. Several specific disorders were also represented with low frequency (e.g., agoraphobia, eating disorders). More research is needed on the impact of SA on these conditions. Second, although moderators satisfactorily accounted for heterogeneity in ORs for anxiety and depressive disorders, significant heterogeneity remained when moderators were included for PTSD and substance use disorders. This suggests that there may be important unassessed moderators. There is evidence that factors including whether assaults were perpetrated by strangers, involved weapon use, and led to physical injury may affect effect sizes (Dworkin et al., 2017), but was not possible to test these moderators in this analysis due to low frequency of reporting across diagnostic categories. Other possible moderators, such as number of assaults experienced, other lifetime trauma exposure, and perceived life threat during the assault should be explored in future analyses. Third, studies without a comparison group were excluded, as a goal of this study was to understand the relative odds of experiencing each disorder in assaulted versus unassaulted groups. It is possible that different prevalence estimates for SA groups would be obtained if such studies were included. Fourth, studies were limited in their gender and regional diversity. Although most meta-analyses have not observed gender differences in associations between interpersonal violence and psychopathology (Dworkin et al., 2017; Paolucci, Genuis, & Violatto, 2001; Tolin & Foa, 2006; cf. Weaver & Clum, 1995), the degree to which gender differences exist psychopathology after SA specifically remains unclear and should be investigated further. Given that most studies in this sample were conducted in the US, these results are limited in their ability to speak to the impact of SA on survivors in different regional contexts. In non-US settings, differences in the prevalence, nature, and context of sexual violence may lead to different mental health outcomes (World Health Organization, 2013). More international research is needed to understand the global impact of SA. Fifth, this analysis did not examine comorbidity between PTSD and other conditions. As a result, it is unclear whether these conditions were independently caused by an experience of SA rather than by symptoms of PTSD stemming from SA (Breslau, 2009). Future meta-analyses should compare SA survivors with and without PTSD in terms of their psychological profiles.
Conclusion
It is clear from this study that SA has a robust association with various mental disorders. Although more research is needed to understand the diversity of conditions associated with SA, the dissemination of evidence-based interventions to people exposed to SA is strongly warranted.
Supplementary Material
Summary Tables.
Critical Findings
Nearly every study included found a higher prevalence for mental disorders among people who had been sexually assaulted than in people who had not been assaulted.
Among people who had been sexually assaulted, depressive disorders and PTSD were especially common.
The prevalence of PTSD was higher in survivors of sexual assault than in survivors of other forms of trauma.
This review cannot conclude that sexual assault causes mental disorders, but instead demonstrates that several mental disorders are much more common in people who have been sexually assaulted.
Implications for Practice, Policy, and Research
Service providers interfacing with survivors of sexual assault should be prepared to assess and make referrals to treatment for PTSD and depression. Referral options should include short-term cognitive behavioral therapies given their success in treating these conditions.
It is important to create early interventions to prevent the development of PTSD after sexual assault. Such interventions could be disseminated by service providers responding in the early aftermath of sexual assault.
Longitudinal research is needed to clarify the causal association between sexual assault victimization and psychopathology.
More research is needed to understand how the impact of sexual assault differs across diverse groups and in non-US settings.
Acknowledgments:
The author would like to thank Sarah Ullman, Jennifer Cadigan, and Nicole Allen, who provided feedback on drafts of this manuscript; Nicole Allen, Jonathan Bystrynski, and Suvarna Menon, who were involved in study design and data collection; the research assistants who aided with data collection; and the researchers who provided unpublished data.
Financial Support: Manuscript preparation for this article was supported by National Institute of Alcohol Abuse and Alcoholism (NIAAA) (grant number T32AA007455, PI: Larimer & K99AA026317, PI: Dworkin). The views expressed in this article are those of the author and do not necessarily reflect the positions or policies of the University of Washington or the NIAAA. The author has no conflicts of interest.
Footnotes
Conflict of Interest: None.
In studies of PTSD, it was sometimes possible to code effects for either a no-SA exposure or other-trauma exposure comparison group. Given that it is not possible for untraumatized individuals to receive a diagnosis of PTSD (APA, 2013), no-SA exposure groups include some individuals who are ineligible for a diagnosis in the comparison group. Odds ratios for this type of study reflect differences as a result of both trauma exposure and diagnosis. Thus, data were coded separately for both types of comparison groups when possible and prevalence estimates are reported separately for each comparison group type in Table 2.
This proportion is a truncated outlier; thus, it is smaller than the proportion in the no-SA group despite the significant odds ratio favoring the SA group.
References
- Acierno R, Lawyer SR, Rheingold AA, Kilpatrick DG, Resnick HS, & Saunders BE (2007). Current psychopathology in previously assaulted older adults. Journal of Interpersonal Violence, 22(2), 250–258. doi: 10.1177/0886260506295369 [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: Author. [Google Scholar]
- Baker MR, Frazier PA, Greer C, Paulsen JA, Howard K, Meredith LN, ... & Shallcross SL (2016). Sexual victimization history predicts academic performance in college women. Journal of Counseling Psychology, 63, 685–692. [DOI] [PubMed] [Google Scholar]
- Beck AT, Rush AK, Shaw BF, & Emery G (1979). Cognitive therapy of depression. New York: The Guilford Press. [Google Scholar]
- Black MC, Basile KC, Breiding MJ, Smith SG, Walters ML, Merrick MT, … Stevens MR (2011). National intimate partner and sexual violence survey (NISVS): 2010 summary report. Atlanta, GA: National Center for Injury Prevention and Control, Centers for Disease Control and Prevention. [Google Scholar]
- Blanco C, Okuda M, Wright C, Hasin DS, Grant BF, Liu SM, & Olfson M (2008). Mental health of college students and their non–college-attending peers: Results from the national epidemiologic study on alcohol and related conditions. Archives of General Psychiatry, 65, 1429–1437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borenstein M, Hedges LV, Higgins JPT, & Rothstein HR (2010). A basic introduction to fixed effect and random effects models for meta-analysis. Research Synthesis Methods, 1, 97–111. [DOI] [PubMed] [Google Scholar]
- Bradley R, Greene J, Russ E, Dutra L, & Westen D (2005). A multidimensional meta-analysis of psychotherapy for PTSD. American Journal of Psychiatry, 162, 214–227. [DOI] [PubMed] [Google Scholar]
- Breslau N (2009). The epidemiology of trauma, PTSD, and other posttrauma disorders. Trauma, Violence, & Abuse, 10, 198–210. [DOI] [PubMed] [Google Scholar]
- Breslau J, Lane M, Sampson N, & Kessler RC (2008). Mental disorders and subsequent educational attainment in a US national sample. Journal of Psychiatric Research, 42, 708–716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brewin CR, Andrews B, & Valentine JD (2000). Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. Journal of Consulting and Clinical Psychology, 68(5), 748–766. [DOI] [PubMed] [Google Scholar]
- Campbell R, Dworkin E, & Cabral G (2009). An ecological model of the impact of sexual assault on women’s mental health. Trauma, Violence, and Abuse, 10(3), 225–246. [DOI] [PubMed] [Google Scholar]
- Chen LP, Murad MH, Paras ML, Colbenson KM, Sattler AL, Goranson EN, … Zirakzadeh A (2010). Sexual abuse and lifetime diagnosis of psychiatric disorders: Systematic review and meta-analysis. Mayo Clinic Proceedings, 85(7), 618–629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Creamer M, Burgess P, & McFarlane AC (2001). Post-traumatic stress disorder: Findings from the Australian National Survey of Mental Health and Well-being. Psychological Medicine, 31(7), 1237–1247. [DOI] [PubMed] [Google Scholar]
- Cuijpers P, van Straten A, Andersson G, & van Oppen P (2008). Psychotherapy for depression in adults: A meta-analysis of comparative outcome studies. Journal of Consulting and Clinical Psychology, 76(6), 909–922. [DOI] [PubMed] [Google Scholar]
- du Fort G, Newman SC, Bland RC, Galbaud Du Fort G, Newman SC, & Bland RC (1993). Psychiatric comorbidity and treatment seeking: Sources of selection bias in the study of clinical populations. The Journal of Nervous and Mental Disease, 181, 467–474. [PubMed] [Google Scholar]
- Dworkin ER, Menon SV, Bystrynski J, & Allen NE (2017). Sexual assault victimization and psychopathology: A review and meta-analysis. Clinical Psychology Review, 56, 65–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dworkin ER, & Schumacher JA (2016). Preventing posttraumatic stress related to sexual assault through early intervention: A systematic review. Trauma, Violence & Abuse. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher BS, Cullen FT, & Turner MG (2000). The sexual victimization of college women. Washington, D. C.: National Institute of Justice. [Google Scholar]
- Foa EB, Cashman L, Jaycox L, & Perry K (1997). The validation of a self-report measure of posttraumatic stress disorder: The Posttraumatic Diagnostic Scale. Psychological Assessment, 9(4), 445–451. 10.1037/1040-3590.9.4.445 [DOI] [Google Scholar]
- Frazier P, Conlon A, & Glaser T (2001). Positive and negative life changes following sexual assault. Journal of Consulting and Clinical Psychology, 69, 1048–1055. [DOI] [PubMed] [Google Scholar]
- Gillock KL, Zayfert C, Hegel MT, & Ferguson RJ (2005). Posttraumatic stress disorder in primary care: prevalence and relationships with physical symptoms and medical utilization. General Hospital Psychiatry, 27, 392–399. [DOI] [PubMed] [Google Scholar]
- Golding JM (1994). Sexual assault history and physical health in randomly selected Los Angeles women. Health Psychology, 13(2), 130–138. [DOI] [PubMed] [Google Scholar]
- Griffin MG, Uhlmansiek MH, Resick PA, & Mechanic MB (2004). Comparison of the Posttraumatic Stress Disorder Scale versus the Clinician‐Administered Posttraumatic Stress Disorder Scale in domestic violence survivors. Journal of Traumatic Stress, 17, 497–503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofmann SG, Asnaani A, Vonk IJ, Sawyer AT, & Fang A (2012). The efficacy of cognitive behavioral therapy: A review of meta-analyses. Cognitive Therapy and Research, 36(5), 427–440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kang HK, Natelson BH, Mahan CM, Lee KY, & Murphy FM (2003). Post-traumatic stress disorder and chronic fatigue syndrome-like illness among Gulf War Veterans: A population-based survey of 30,000 Veterans. American Journal of Epidemiology, 157, 141–148. [DOI] [PubMed] [Google Scholar]
- Kelley LP, Weathers FW, McDevitt-Murphy ME, Eakin DE, & Flood AM (2009). A comparison of PTSD symptom patterns in three types of civilian trauma. Journal of Traumatic Stress, 22, 227–235. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Chiu WT, Demler O, & Walters EE (2005). Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry, 62, 617–627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB, & Breslau N (1999). Epidemiological risk factors for trauma and PTSD In Yehuda R(Ed.), Risk factors for posttraumatic stress disorder (pp. 23–59). Washington DC: American Psychiatric Association. [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB, Sonnega A, ... Nelson CB (1995). Posttraumatic stress disorder in the National Comorbity Survey. Archives of General Psychiatry, 52, 1048–1060. [DOI] [PubMed] [Google Scholar]
- Kilpatrick DG, Acierno R, Resnick HS, Saunders BE, & Best CL (1997). A 2-year longitudinal analysis of the relationships between violent assault and substance use in women. Journal of Consulting and Clinical Psychology, 65, 834–847. [DOI] [PubMed] [Google Scholar]
- Kilpatrick DG, Edmunds CN, & Seymour AK (1992). Rape in America: A report to the nation. Charleston, SC: Crime Victims Research and Treatment Center. [Google Scholar]
- Kilpatrick DG, Ruggiero KJ, Acierno R, Saunders BE, Resnick HS, & Best CL (2003). Violence and risk of PTSD, major depression, substance abuse/dependence, and comorbidity: Results from the National Survey of Adolescents. Journal of Consulting and Clinical Psychology, 71, 692–700. [DOI] [PubMed] [Google Scholar]
- Kornør H, Winje D, Ekeberg Ø, Weisæth L, Kirkehei I, Johansen K, & Steiro A (2008). Early trauma-focused cognitive-behavioural therapy to prevent chronic post-traumatic stress disorder and related symptoms: A systematic review and meta-analysis. BMC Psychiatry, 8, 1–8. 10.1186/1471-244X-8-81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koss MP, Gidycz CA, & Wisniewski N (1987). The scope of rape: Incidence and prevalence of sexual aggression and victimization in a national sample of higher education students. Journal of Consulting and Clinical Psychology, 55(2), 162–170. [DOI] [PubMed] [Google Scholar]
- Lejuez CW, Hopko DR, & Hopko SD (2001). A brief behavioral activation treatment for depression. Behavior Modification, 25, 255–286. [DOI] [PubMed] [Google Scholar]
- Litz BT, Gray MJ, Bryant R, & Adler A (2002). Early interventions for trauma: Current status and future directions. Clinical Psychology: Science and Practice, 9, 112–134. [Google Scholar]
- Mazzucchelli T, Kane R, & Rees C (2009). Behavioral activation treatments for depression in adults: A meta‐analysis and review. Clinical Psychology: Science and Practice, 383–411. [Google Scholar]
- McCollister KE, French MT, & Fang H (2011). The cost of crime to society: New crime-specific estimates for policy and program evaluation. Drug and Alcohol Dependence, 108, 98–109. 10.1016/j.drugalcdep.2009.12.002.The [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mendes DD, Mello MF, Ventura P, de Medeiros Passarela C, & de Jesus Mari J (2008). A systematic review on the effectiveness of cognitive behavioral therapy for posttraumatic stress disorder. The International Journal of Psychiatry in Medicine, 38, 241–259. [DOI] [PubMed] [Google Scholar]
- Orcutt HK, Erickson DJ, & Wolfe J (2002). A prospective analysis of trauma exposure: The mediating role of PTSD symptomatology. Journal of Traumatic Stress, 15, 259–266. [DOI] [PubMed] [Google Scholar]
- Ozer EJ, Best SR, Lipsey TL, & Weiss DS (2003). Predictors of posttraumatic stress disorder and symptoms in adults: A meta-analysis. Psychological Bulletin, 129, 52–73. [DOI] [PubMed] [Google Scholar]
- Paolucci EO, & Genuis ML (2001). A meta-analysis of the published research on the effects of child sexual abuse. The Journal of Psychology, 135, 17–36. [DOI] [PubMed] [Google Scholar]
- Pineles SL, Shipherd JC, Welch LP, & Yovel I (2007). The role of attentional biases in PTSD: Is it interference or facilitation? Behaviour Research and Therapy, 45, 1903–1913. [DOI] [PubMed] [Google Scholar]
- Post LA, Mezey NJ, Maxwell C, & Wibert WN (2002). The rape tax: Tangible and intangible costs of sexual violence. Journal of Interpersonal Violence, 17, 773–782. [Google Scholar]
- Powers MB, Halpern JM, Ferenschak MP, Gillihan SJ, & Foa EB (2010). A meta-analytic review of prolonged exposure for posttraumatic stress disorder. Clinical Psychology Review, 30, 635–641. 10.1016/j.cpr.2010.04.007 [DOI] [PubMed] [Google Scholar]
- R Development Core Team. (2014). R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; Retrieved from http://www.r-project.org [Google Scholar]
- Resick PA, Monson CM, & Chard KM (2014). Cognitive processing therapy: Veteran/military version: Therapist and patient materials manual. Washington, D C: Department of Veterans Affairs. [Google Scholar]
- Robinson J, Sareen J, Cox BJ, & Bolton J (2009). Self-medication of anxiety disorders with alcohol and drugs: Results from a nationally representative sample. Journal of Anxiety Disorders, 23, 38–45. [DOI] [PubMed] [Google Scholar]
- Rothbaum B, Foa E, & Hembree E (2007). Reclaiming your life from a traumatic experience: A prolonged exposure treatment program workbook. New York: Oxford University Press. [Google Scholar]
- Smolak L, & Murnen SK (2002). A meta-analytic examination of the relationship between child sexual abuse and eating disorders. International Journal of Eating Disorders, 31, 136–150. 10.1002/eat.10008 [DOI] [PubMed] [Google Scholar]
- Stein MB, & Barrett-Connor E (2000). Sexual assault and physical health: Findings from a population-based study of older adults. Psychosomatic Medicine, 62, 838–843. [DOI] [PubMed] [Google Scholar]
- Tanielian T., & Jaycox L. (Eds.). (2008). Invisible wounds of war: Psychological and cognitive injuries, their consequences, and services to assist recovery. Santa Monica, CA: RAND Corporation. [Google Scholar]
- Tjaden P, & Thoennes N (2000). Prevalence and consequences of male-to-female and female-to-male intimate partner violence as measured by the National Violence Against Women Survey. Violence Against Women, 6(2), 142–161. [Google Scholar]
- Tjaden P, & Thoennes N (2006). Extent, nature, and consequences of rape victimization: Findings from the National Violence Against Women Survey. Washington, D. C. [Google Scholar]
- Tolin DF, & Foa EB (2006). Sex differences in trauma and posttraumatic stress disorder: A quantitative review of 25 years of research. Psychological Bulletin, 132(6), 959–992. [DOI] [PubMed] [Google Scholar]
- Van Berlo W, & Ensink B (2000). Problems with sexuality after sexual assault. Annual Review of Sex Research, 11(1), 235–257. [PubMed] [Google Scholar]
- Viechtbauer W (2010). Conducting meta-analyses in R with the metafor package. Journal of Statistical Software, 36(3), 1–48. [Google Scholar]
- Weaver TL, & Clum GA (1995). Psychological distress associated with interpersonal violence: A meta-analysis. Clinical Psychology Review, 15, 115–140. [Google Scholar]
- World Health Organization. (2013). Responding to intimate partner violence and sexual violence against women: WHO clinical and policy guidelines. World Health Organization. [PubMed] [Google Scholar]
- Xu Y, Olfson M, Villegas L, Okuda M, Wang S, Liu S, & Blanco C (2013). A characterization of adult victims of sexual violence: Results from the National Epidemiological Survey for Alcohol and Related Conditions. Psychiatry, 76, 223–240. [DOI] [PubMed] [Google Scholar]
- Zinzow HM, Grubaugh AL, Frueh BC, & Magruder KM (2008). Sexual assault, mental health, and service use among male and female veterans seen in Veterans Affairs primary care clinics: A multi-site study. Psychiatry Research, 159, 226–236. [DOI] [PubMed] [Google Scholar]
- Zinzow HM, Resnick HS, McCauley JL, Amstadter AB, Ruggiero KJ, & Kilpatrick DG (2012). Prevalence and risk of psychiatric disorders as a function of variant rape histories: Results from a National Survey of Women. Social Psychiatry and Psychiatric Epidemiology, 47(6), 893–902. doi: 10.1007/s00127-011-0397-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


