Abstract
To present our novel technique for subsequent port placement during video endoscopic inguinal lymphadenectomy (VEIL) surgery. VEIL has provided positive results in terms of reduction of pain, early recovery, and better cosmesis. Ten patients who underwent VEIL procedure during 2012–2015 were included in this study to assess feasibility, safety, and advantages of port placement by our new technique which include placement of subsequent ports with the help cannula of the first port. The size of incision, time taken for port placement, leakage of pneumo, any complication(s), and potential learning curve or special instrument requirements were noted in these patients. Median incision size was 10 mm and 5 mm for their respective sized ports with this new technique. Pneumo leakage was not seen in any patient. Median time taken for subsequent port placement was 2 min ± 15 s. No complication was noted to patients or the operating surgeon. The technique proved to be feasible and needed no special equipment or training. We report technical feasibility, safety, and advantages of a new technique for port placement during VEIL surgery emphasising its potential to become a standard technique in the near future.
Keywords: Port placement, VEIL surgery, Penile cancer
Introduction
Penile cancer is not uncommon in developing countries like India [1] and involvement of lymph nodes has prognostic implications. Radical inguinal lymphadenectomy is required for local control of disease. Though the procedure has a distinct survival advantage, the associated morbidity cannot be underestimated. With an aim to reduce the morbidity associated with its open counterpart, video endoscopic inguinal lymphadenectomy (VEIL) was developed as a minimally invasive approach and provided positive results in terms of reduction of pain, early recovery, and better cosmesis [1–11].
High-grade penile lesions (G3/G4), pT1 tumours with LVI (pT1b), and pT2 to pT4 tumours carry 20 to 30% risk of micrometastatic inguinal lymph node disease even in the presence of clinically normal groins, and VEIL is best suited for these subsets of patients although large prospective trials are still required for validation of endoscopic surgical approaches as comparable treatment option to standard open surgery with similar recurrence patterns and equivalent oncological outcomes [7, 11, 12]. With regard to the use of VEIL in positive groin, therapeutic role is not established as of now [7, 11]. Many techniques have been used for port placement during VEIL in the past but none have been described in detail in literature and still no procedure has been recommended as standard for port insertion. Since previously described techniques for placing ports during VEIL surgery have difficulties of large skin incision, high probability of injury to patient’s underlying vital structures or surgeon’s finger, longer time, and leakage of pneumo around trocars, we decided to evaluate a new technique for port placement. We present our initial experience with a new technique of port placement during VEIL surgery and assessment of its feasibility, safety, and any special equipment/training requirements in our patients.
Methods
After taking informed and written consent of the patients, a new technique has been used by our department from 2012 to 2015 in relation to a previously published study related to VEIL since 2012 [12]. Here, we have evaluated the feasibility of this new technique, need for any special instrument or training, safety of the patient in relation to risk of injury to underlying vital structures and safety of the surgeon with risk of injury to the guiding finger, incision size, time taken for port insertion, and leakage of pneumo from working space as evaluated by the need for any suturing around the trocar. Surgical technique after proper positioning the patient and surgical draping a 1-cm incision is made deep to superficial fascia, 2-cm caudal to the apex of the femoral triangle (Fig. 1). A plane is created by sharp dissection with scissors and bluntly by cannula, 5–6-cm supero-medially and supero-laterally to the incision at the level of the apex of femoral triangle to create adequate space for insertion of secondary ports. Skin is then lifted with cannula inserted through primary incision for making secondary incisions taking cannula as base (Fig. 1). We could see the lumen of primary cannula at secondary incisions. The 5-mm cannulas are inserted with guidance of primary cannula and negotiating it in the lumen of 10-mm cannula making the insertion safe and accurate (Fig. 2a, b). Rest of the procedure was continued as standard practice already described [12].
Fig. 1.
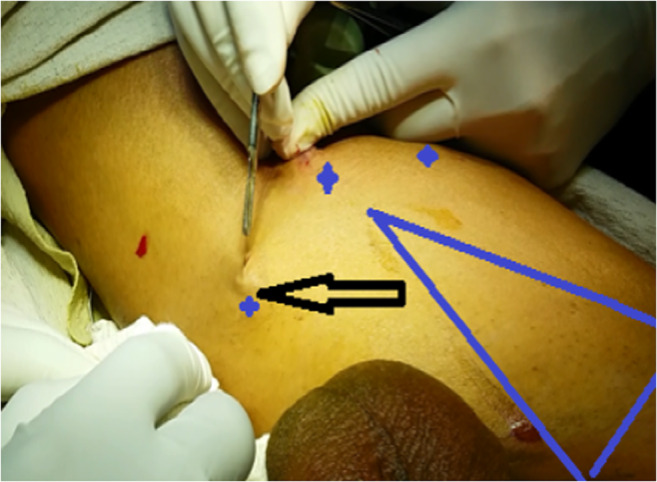
Cannula-assisted port site incision. Superficial marking of femoral triangle and port sites is shown (blue colour) and the incision for secondary port made by taking cannula of first port as the base and lifting the skin with it is shown (arrow)
Fig. 2.
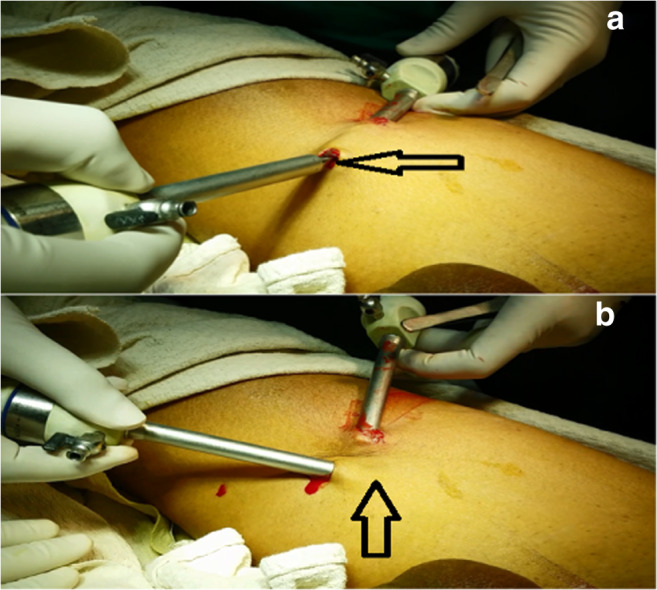
Cannula assisted port insertion. a Arrow showing secondary cannula being inserted by guidance and negotiating it into the lumen of first cannula. b After the seven secondary cannula is pushed in, both cannulas are rotated and placed into position (upward arrow)
Results
We report our results in 10 patients Carcinoma Penis in which VEIL was done with our technique of subsequent port insertion. In all of the 10 patients who underwent VEIL, the median size of incision needed was 1 cm for 10 mm port and 5 mm for 5 mm port (Table 1). The median time taken for port insertion was 2 min (Table 1). In all of our patients, the port placement was in the correct plane which was deep to scarpa’s fascia. Since incision in our technique is small and is trocar guided, the trocar fits in the incision leaving no space for leakage, and pneumo is well maintained during the surgery. There was no injury to the patients or operating surgeon in our study. No new instruments and further training of the operating surgeon were required in our study.
Table 1.
Port insertion
| Characteristics | New technique | Previous techniques |
|---|---|---|
| Incision size (10-mm port) | 1 cm | 1.5–2 cm |
| Time taken | 2 min ± 15 s | 3 min ± 15 s |
| Injury to patient | Not seen | Possible |
| Injury to surgeon | Not seen | Possible |
| Leakage of pneumo | Not significant | Significant |
Comments
Previous techniques were adapted from a technique described for port insertion during retroperitoneal port insertions but there is a substantial amount of subcutaneous tissue and muscle in that area which makes insertion feasible without complications. But here in the thigh, we do not have fat or muscle for support thus using the same technique is not justified and is dangerous.
Techniques of port insertion have not been described in detail in most of the studies related to VEIL. However, various techniques have been used to date for port insertion in VEIL surgery.
Finger-Assisted Port Insertion
A 1.5-cm incision was made 2 cm distally to the lower vertex of the femoral triangle. Scissors and digital manoeuvres were used to develop a plane of dissection deep into superficial fascia. A second 1.0-cm incision was made 6 cm medially to the apex of the triangle, after digital elevation of the skin through the first incision, to place a 10-mm trocar. The last 5-mm port was placed 6 cm laterally to the apex of the triangle in an analogous manner. A 10-mm Hasson trocar was inserted in the first incision. The first port accommodates 0° optics. The medial port accepts the harmonic scalpel or the clip applier and the lateral port may accept the grasper, scissors, or a dissection device [13, 14].
This technique is most commonly used nowadays but there are practical difficulties in following this technique in routine. First, it puts the surgeon to a risk of injury during the procedure because incision is being made with the surgeon’s finger beneath the skin. Moreover, the incision made to insert finger is 1.5–2 cm thus the pneumo leakage is a persistent problem with this technique. All of these potential complications are not seen with our new technique of port insertion.
Blind Open Technique
A 1.5-cm incision was made 2 cm distally to the lower vertex of the femoral triangle. A second incision was made 2 cm proximally and 6 cm medially. Two 10-mm Hasson trocars were inserted in these incisions and the working space was insufflated with CO2 at 5–15 mmHg. The final trocar was placed 2 cm proximally and 6 cm laterally from the first port, [14]. In this technique, the port is inserted blindly which makes the patient more prone to injuries. Furthermore, this technique is time-consuming.
As VEIL is focused on providing surgery with least morbidity and best cosmetic outcome, our technique is possibly better for the procedure. Since the time taken to place the port by finger-guided or any other technique is longer than the time taken with this technique, it saves the valuable time of surgeon.
Earlier, there were chances that the cannula might remain superficial or get deeper than required but as the cannula here is placed with the guidance of primary cannula, it is least possible that the cannula placed is in the wrong plane. The new technique is safer than previous techniques which used to put the patient to the danger of important structures below the incisions to get injured during the insertion of the port as there was no support from below. Surgeon’s finger was also at some risk of injury when incision was made over the finger. This new technique has shown to be safe for both the patient and surgeon because we have used cannula for support while making the incision thus structures beneath as well as the surgeon finger are not at risk of injury.
As this procedure does not need any new equipment, only simple cannula will do nor is any training needed so it is most feasible in the present setting. A surgeon who has training in laparoscopic surgeries can easily adapt to this technique without any lag and practice it in routine. Furthermore, we have observed that with this new technique greater area could be dissected as compared to finger dissection most likely as a result of the length of cannula used for dissection being more than surgeon’s finger.
Though this study presents our initial experience with a small number of patients, wider acceptance and practice of this novel technique with further studies especially randomised trials can pave way for the adoption of a potential standard practice of port placement in VEIL surgery in the near future.
Conclusion
We report a new technique of port insertion in VEIL surgery. It is unique in ensuring no leakage of pneumo, reducing time for port insertion, and ensuring safety of both the patient and the surgeon with no additional training or instrument requirement.
It is feasible, safer, and less associated potential drawbacks of port insertion by other techniques. It has a potential to become a standard practice in VEIL surgery.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Harvinder Singh Pahwa, Email: pahwa.kgmu@yahoo.co.in.
Ajay Kumar Pal, Email: akpal.jnmc@yahoo.com.
Awanish Kumar, Email: awanishkr79@gmail.com.
Sanjeev Misra, Email: misra@gmail.com.
Gunjeet Kaur, Email: gunjeet20@yahoo.com.
References
- 1.Tobias-Machado M, Starling ES, Oliveira ABP, Pompeo AC, Wroclawski ER. 5-Years experience with video endoscopic inguinal lymphadenectomy (VEIL): learning curve and technical variations of a new procedure. Journal of Andrological Sciences. 2009;16:25–32. [Google Scholar]
- 2.Ornellas AA, Correia Seixas AL, Marota A, Wisnescky A, Campos F, Moraes JR. Surgical treatment of invasive squamous cell carcinoma of the penis: retrospective analysis of 350 cases. J Urol. 1994;151:1244–1249. doi: 10.1016/S0022-5347(17)35222-9. [DOI] [PubMed] [Google Scholar]
- 3.Catalona WJ. Modified inguinal lymphadenectomy for carcinoma of the penis with preservation of saphenous veins: technique and preliminary results. J Urol. 1988;140:306–310. doi: 10.1016/S0022-5347(17)41589-8. [DOI] [PubMed] [Google Scholar]
- 4.Tobias-Machado M, Tavares A, Molina WR, Jr, Zambon JP, Medina JA, Forseto PH, Jr, Juliano RV, Wroclawski ER. Video endoscopic inguinal lymphadenectomy (VEIL): initial case report and comparison with open radical procedure. Arch Esp Urol. 2006;59(8):849–852. doi: 10.4321/S0004-06142006000800020. [DOI] [PubMed] [Google Scholar]
- 5.Tobias-Machado M, Tavares A, Molina WR, Jr, Forseto PH, Jr, Juliano RV, Wroclawski ER. Video endoscopic inguinal lymphadenectomy (VEIL): minimally invasive resection of inguinal lymph nodes. Int Braz J Urol. 2006;32(3):316–321. doi: 10.1590/S1677-55382006000300012. [DOI] [PubMed] [Google Scholar]
- 6.Tobias-Machado M, Tavares A, Ribeiro Silva MN, Molina WR, Jr, Forseto PH, Juliano RV, Wroclawski ER. Can video endoscopic inguinal lymphadenectomy achieve a lower morbidity than open lymph node dissection in penile cancer patients? J Endourol. 2008;22(8):1687–1692. doi: 10.1089/end.2007.0386. [DOI] [PubMed] [Google Scholar]
- 7.Tobias-Machado M, Tavares A, Ornellas AA, Molina WR, Jr, Juliano RV, Wroclawski ER. Video endoscopic inguinal lymphadenectomy: a new minimally invasive procedure for radical management of inguinal nodes in patients with penile squamous cell carcinoma. J Urol. 2007;177:953–958. doi: 10.1016/j.juro.2006.10.075. [DOI] [PubMed] [Google Scholar]
- 8.Favorito LA, Nardi AC, Ronalsa M, Zequi SC, Sampaio FJ, Glina S. Epidemiologic study on penile cancer in Brazil. Int Braz J Urol. 2008;34:587–591. doi: 10.1590/S1677-55382008000500007. [DOI] [PubMed] [Google Scholar]
- 9.Thyavihally Y, Tongaonkar H. Video endoscopic inguinal lymphadenectomy (VEIL): our initial experience. Urology. 2008;72:S106–S107. doi: 10.1016/j.urology.2008.08.310. [DOI] [Google Scholar]
- 10.Rawal S, Krishnappa RS, Khanna S, Sekon R, Koul R. Video endoscopic inguinal lymphadenectomy (VEIL): minimally invasive radical inguinal lymphadenectomy technique video abstract, VEIL technique Indian. J Surg Oncol. 2012;3(3):257–261. doi: 10.1007/s13193-012-0164-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sharma P, Zargar H, Spies PE. Surgical advances in inguinal lymph node dissection. Urol Clin N Am. 2016;43:457–468. doi: 10.1016/j.ucl.2016.06.007. [DOI] [PubMed] [Google Scholar]
- 12.Pahwa HS, Mishra S, Kumar A, Kumar V, Agarwal A, Shrivastava R. Video endoscopic inguinal lymphadenectomy (VEIL) - a prospective critical perioperative assessment of feasibility and morbidity with points of technique in penile carcinoma. World J Surg Oncol. 2013;11:42. doi: 10.1186/1477-7819-11-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Correa WF, Tobias-Machado M. Video-endoscopic inguinal lymphadenectomy. Eur Oncol. 2010;6(2):80–84. [Google Scholar]
- 14.Pompeo A, Tobias-Machado M, Molina WR, Lucio J, Sehrt D, et al. Extending boundaries in minimally invasive procedures with simultaneous bilateral video endoscopic inguinal lymphadenectomy (VEIL) for penile cancer: initial experience and surgical considerations. Int Braz J Urol. 2013;39:587–592. doi: 10.1590/S1677-5538.IBJU.2013.04.18. [DOI] [PubMed] [Google Scholar]


