Abstract
Traditional telepathology techniques like whole slide imaging and robotic microscopy are too expensive to be used in developing countries. With the advent of smartphones with high-resolution cameras and faster internet services, it is now possible to send good-quality images to pathologist for diagnosis. To study the utility of WhatsApp image transfer in the histopathological diagnosis of common oral malignant and benign lesions. A total of 100 cases of oral biopsy were included in the study. These comprised of 58 cases of squamous cell carcinoma, 33 cases of oral leukoplakia, 3 cases of oral lichen planus and 6 cases of moderate to severe dysplasia. The conventional microscopy diagnosis made by glass slide viewing was taken as the gold standard and the concordance of the WhatsApp diagnosis with the gold standard was calculated for each category of diagnosis and also for all the 100 cases. The concordance rate for squamous cell carcinoma was 96.6%(56/58). For leukoplakia, there was 100%(33/33) concordance between the WhatsApp diagnosis and conventional microscopy. The concordance rates for dysplasia (4/6) and oral lichen planus (2/3) were 66.7% each. Hence, for all the categories taken together, the overall concordance rate was 95%. A concordance rate of 95% is very encouraging; however, for routine diagnostic use in telepathology, there is still a long way to go. With the availability of better smartphone cameras and faster internet, it will be possible to send better quality images in the future. The pathologists will also learn where to draw the line and ask for glass slides for final diagnosis.
Keywords: Smartphone assisted telepathology, Oral biopsy, Tele-oncopathology
Introduction
Improvement in smartphone camera resolution and increasing use of social media tools like WhatsApp have resulted in new avenues for growth of telepathology. WhatsApp has already been used for better doctor patient interaction, teaching medical students, getting second opinions in histopathology. However, its use for primary diagnosis of histopathology slides has its own limitations [1, 2].
New smartphone accessories can adapt the smartphone to the microscope eyepieces and help in getting high-resolution images. With practice, it is also possible to get similar high quality images without using the adaptors. Vignetting is a common problem in smartphone microphotographs. It is defined as reduction of an image’s brightness or saturation toward the periphery compared with the image centre. This can be overcome by using optical zoom of the smartphone camera. It is generally presumed that better megapixel (MP) count of the camera translates to greater confidence in making a diagnosis on the image procured. This is a myth since other factors like optical quality of lens, camera sensor and the medium where the image is viewed are all equally important. A recent study found that an 8-MP smartphone camera is sufficient for telepathology consultations [3]. A grid template could be printed and placed under the slide to guide the reporting pathologist. If more images are required, then the reporting pathologist can simply guide the sender to take more pictures of the specific area of the grid [3].
In developing countries and in remote locations, cost of equipment can be an important factor in determining the mode of telepathology used. Hence, our study was designed to evaluate the accuracy of low-cost telepathology set-up in diagnosing common oral lesions. No smartphone camera adaptors were used. The grids were replaced by permanent marker pens used to outline the areas being photographed. The smartphones used to capture the images and evaluate the cases were also of low to medium budget range.
Aim
The aim of this work is to study the utility of WhatsApp image transfer in the histopathological diagnosis of common oral lesions.
Materials and Methods
A total of 100 cases of oral biopsy were included in the study. These comprised of 58 cases of squamous cell carcinoma, 33 cases of oral leukoplakia, 3 cases of oral lichen planus and 6 cases of moderate to severe dysplasia. The conventional microscopy diagnosis made by glass slide viewing was taken as the gold standard and the concordance of the WhatsApp diagnosis with the gold standard was calculated for each category of diagnosis and also for all the 100 cases. In order to avoid inter observer variability in the diagnosis, the WhatsApp images were sent to the same pathologist (N T) who had made the diagnosis on conventional microscopy.
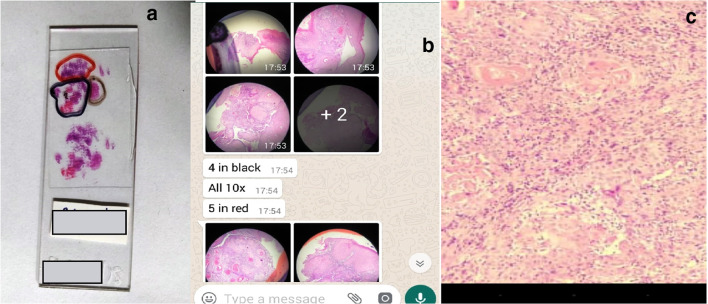
Instead of using the grid method for orienting the slides for the reporting pathologist, a novel method was devised by using permanent markers to outline the areas photographed (Fig. 1a, b). Then, each area photographed was captioned as red 1, red 2, red 3, black 1, black 2, black 3 and so on. The reporting pathologist was given the option of asking for more images by referring to the area colour code.
Fig. 1.
a A novel method of labelling the areas photographed on the glass slide with permanent markers of different colours. b A screenshot of the smartphone screen showing the images being sent with the corresponding colour code referring to the area of slide photographed. c A screenshot of the smartphone screen showing the problem of pixilation due to reduction of the size of image file on WhatsApp transfer
A pathologist (senior resident) captured the images of slides from the ocular of a binocular microscope (Dewinter classic microscope, Dewinter technologies, Milano, Italy) using a OnePlus A5000 smartphone (16 MP, made in Shenzen, Guangdong, China, by OnePlus). The images were transferred by WhatsApp to the reporting pathologist (NT) who viewed the images on his own smartphone screen (HTC Desire 623) and replied by sending the smartphone diagnosis of each case. The reporting pathologist was blinded to the conventional microscopy diagnosis of each case. The relevant clinical details of each case were also sent by WhatsApp. The diagnosis was entered on excel sheet and concordance rates for each category were calculated. The other metrics of the study like average time required per case for capturing the images and the time taken by the reporting pathologist to give the diagnosis by WhatsApp were also calculated.
Results
A total of 723 images were captured with a mean image capturing time per case of 5.33 min. Average time interval from image transfer to diagnosis per case via WhatsApp was 6.76 min (Table 1). For leukoplakia, there was 100% (33/33) concordance between the WhatsApp diagnosis and conventional microscopy (Fig. 2). The concordance rate for squamous cell carcinoma was 96.6% (56/58) (Fig. 3). The concordance rates for dysplasia (4/6) and oral lichen planus (2/3) were 66.7% each (Table 2). Image pixilation on digital zoom and problem of orientation of the different bits to one another were the main causes of discordance (Table 3).
Table 1.
Number of images, image capturing time, magnifications and number of cases which required additional images
| S. No. | Parameter | Value |
|---|---|---|
| 1. | Diagnoses of cases selected for the study | |
| a. Leukoplakia | 33 | |
| b. Squamous cell carcinoma | 58 | |
| c. Dysplasia | 06 | |
| d. Oral lichen planus | 03 | |
| Total | 100 | |
| 2. | Total number of images | 723 |
| 3. | Average number of image capture per case | 7.23 |
| 4. | Image number by × 4 magnification (N, ) | 90 |
| 5. | Image number by × 10 magnification (N, ) | 608 |
| 6. | Image number by × 20 magnification (N,) | 18 |
| 7. | Image number by × 40 magnification (N,) | 07 |
| 8. | Total image capturing time (min) | 533 |
| 9. | Average time of image capturing per case (min) | 5.33 |
| 10. | Total time from image transfer to diagnosis of the cases via WhatsApp (min) | 676 |
| 11. | Average time interval from image transfer to diagnosis per case via WhatsApp (min) | 6.76 |
| 12. | Number of cases that required digital zoom for making diagnosis via WhatsApp (N, %) | 100 (100%) |
| 13. | Number of cases that required additional images for diagnosis (N, %) | 4 (4%) |
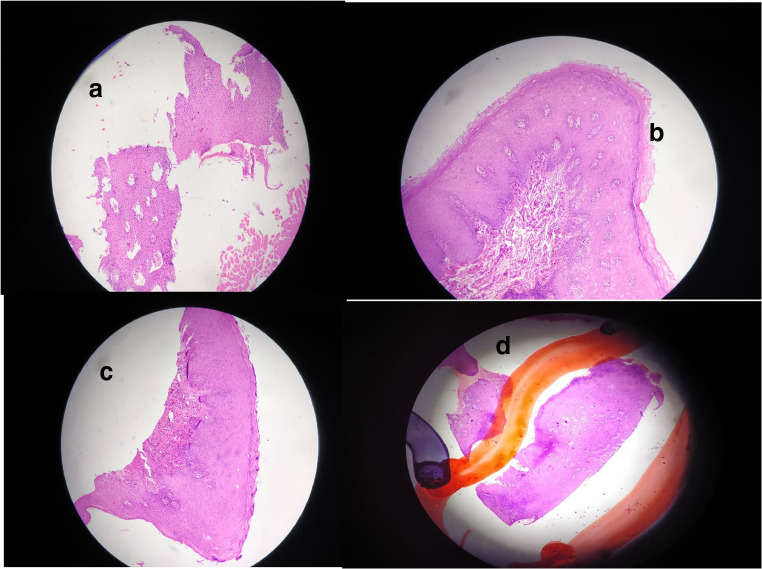
Fig. 2.
WhatsApp images of cases correctly diagnosed as leukoplakia on smartphone assisted tele-oralpathology (a to d, haematoxylin and eosin, × 10)
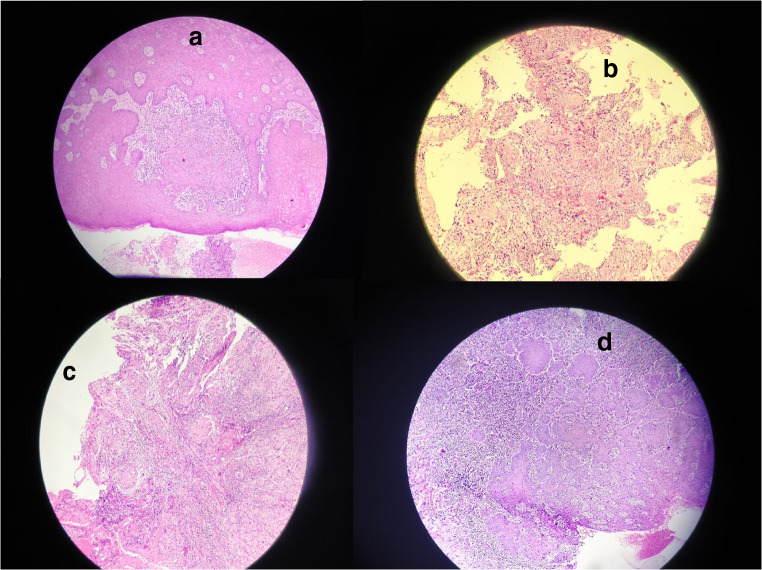
Fig. 3.
WhatsApp images of cases correctly diagnosed as squamous cell carcinoma on smartphone-assisted tele-oralpathology (a to d, haematoxylin and eosin, × 10)
Table 2.
Summary of concordance between WhatsApp diagnosis and conventional microscopy diagnosis for different categories of cases
| S. No | Conventional microscopy diagnosis | Number of cases | No. of cases correctly diagnosed on WhatsApp images | Concordance of diagnosis |
|---|---|---|---|---|
| 1 | Squamous cell carcinoma | 58 | 56 | 96.6% |
| 2 | Leukoplakia | 33 | 33 | 100% |
| 3 | Oral lichen planus | 03 | 02 | 66.7% |
| 4 | Moderate to severe dysplasia | 06 | 04 | 66.7% |
| Total | 100 | 95 | 95% |
Table 3.
Summary of discordant cases and possible reasons for discordance
| S. No. | Conventional microscopy diagnosis | WhatsApp diagnosis | Possible reason for discordance |
|---|---|---|---|
| 1 | Moderately differentiated squamous cell carcinoma | Severe dysplasia | Problem of orientation |
| 2 | Well-differentiated squamous cell carcinoma | Hyperplastic stratified squamous epithelium | Inability to switch between different fields on static images |
| 3 | Oral lichen planus | Hyperplastic stratified squamous epithelium | Pixelated image on digital zoom |
| 4 | Severe dysplasia | Moderately differentiated squamous cell carcinoma | Pixelated image on digital zoom |
| 5 | Moderate to severe dysplasia | Moderately differentiated squamous cell carcinoma | Problem of orientation and pixelated image on digital zoom |
Hence, for all the categories taken together, the overall concordance rate was 95%. The reporting pathologist asked for more images in only 4 out of the total 100 cases. All these cases were concordant with the conventional microscopy on final analysis.
Discussion
Mobile internet has completely changed the practice of medicine in the last few years. Doctors are increasingly becoming social media savvy and are more open to the use of internet technology in their professional spheres. WhatsApp (WhatsApp, Inc., Mountain View, CA, USA) is an instant messaging app developed for smartphones. It can be used to send messages, documents, images, audio and video files and internet links by using mobile numbers. It is one of the most popular instant messaging applications in the world.
With the advent of 4G networks even at remote locations, it is now possible to send images of histopathology slides to anyone having a smartphone and get his/her expert opinion. In many far-flung locations, it is difficult to get a histopathologist to interpret cases. The only way to get histopathology diagnostics at such places is to ship the slides/specimen to the centres where such facilities are available. Oral squamous cell carcinomas have a very high incidence rate in the Indian subcontinent mainly due to the practice of chewing gutkha and tobacco. The treatment is usually delayed because the facilities for cancer diagnostics are not available at remote locations. The use of WhatsApp has already been tried in facilitating remote oral medicine consultation [4]. It has also been used in getting second opinion in oral pathology [1].
In a recent study, Sarode SC et al. found that WhatsApp-based second opinion was correct in 98.22% of cases (4710 out of 4795). However, the accuracy was much lower in lesions like myoepithelial carcinoma, osteosarcoma and intravascular papillary hyperplasia. In our study since the lesions included only common conditions like squamous cell carcinoma, dysplasia, leukoplakia and oral lichen planus, the concordance rate was close to that of the study by Sarode SC et al. Hence, for common oral pathology lesions, WhatsApp-based telepathology set-up can give satisfactory results. For other subspecialities and biopsies from other anatomical sites, the list of differentials may be more complicated. The use of WhatsApp-based diagnosis at other anatomical sites may not yield such a high rate of concordance.
Smartphone-assisted telepathology has also been used in cytology and dermatopathology. A recent study by Sahin D et al. found a discordance rate of 20.44% for cervical cytology, 21.15% for thyroid cytology and 22.22% for urine cytology [5]. Teledermatopathology has also shown promising results. In another study on dermatopathology cases, a high concordance rate of 98.8% was achieved between glass slide conventional microscopy and video shot on a digital camera and transmitted via live streaming to iPad [6].
Smartphone adaptors can optimise the image acquisition process; however, good-quality images can be obtained by steady hand without using adaptors [7, 8]. All the images in our study were obtained by using the technique outlined by Morrison AS et al. [8]. The transfer of images by WhatsApp leads to a reduction in the file size and image quality. This is understandable since it facilitates the transfer of large number of images in a short span of time. However, this loss of image quality can be detrimental to the histopathological evaluation of the case. Although the rate of discordance in our study was low (5%), the causes of misinterpretation in these cases on smartphone screen were similar. The two main causes of diagnostic errors were image pixilation on digital zoom due to loss of image quality and the difficulty in orientation of the different images with respect to each other. The problem of pixilation (Fig. 1c) can be overcome by sending the images by Google Drive and evaluating the images on a bigger screen of a laptop or desktop. The problem of orientation is more difficult to solve. The inability of the operator to quickly shift between different areas of the slide is an inherent limitation of this technique of telepathology. In the future, new applications to stitch together the different images in a panorama may be developed to partially circumvent this problem.
Patient confidentiality has been a concern in the use of WhatsApp for sharing images. Few rules of thumb need to be followed while sharing images on WhatsApp. All patient identifying data like name of patient, unique features like tattoo marks, geographical area the patient belongs to and facial features should never be shared on WhatsApp [9]. If these basic rules are followed, then there should be no problem in the use of WhatsApp for diagnostic purpose. The other challenge is the lack of familiarity of the experienced faculty with the use of smartphone screen for evaluating cases. With regular use and training, this hurdle can also be crossed [10].
A concordance rate of 95% is very encouraging; however, for routine diagnostic use in telepathology, there is still a long way to go. With the availability of better smartphone cameras and faster internet, it will be possible to send better quality images in the future. The pathologists will also learn where to draw the line and ask for glass slides for final diagnosis.
An ideal set-up would be one where the pathologist trained to evaluate cases on smartphone screens is given the option of asking for the glass slides to be shipped to him in difficult cases. This would combine the advantages of both conventional microscopy and smartphone telepathology.
Compliance with Ethical Standards
Conflict of Interest
The authors declare that they have no conflict of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Neha Garg, Email: gargdoc118@gmail.com.
Nadeem Tanveer, Email: ntobh104@yahoo.co.in.
Jyotsana Harit Gaur, Email: jyotsanaharitgaur@gmail.com.
References
- 1.Sarode SC, Sarode GS, Anand R, Patil S, Unadkat H. WhatsApp is an effective tool for obtaining second opinion in oral pathology practice. J Oral Pathol Med. 2017;46(7):513–519. doi: 10.1111/jop.12515. [DOI] [PubMed] [Google Scholar]
- 2.Goyal A, Tanveer N, Sharma P. WhatsApp for teaching pathology postgraduates: a pilot study. J Pathol Inform. 2017;8:6. doi: 10.4103/2153-3539.201111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ekong D, Liu F, Brown GT, Ghosh A, Fontelo P. Evaluation of android smartphones for telepathology. J Pathol Inform. 2017;8:16. doi: 10.4103/jpi.jpi_93_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Petruzzi M, De Benedittis M. WhatsApp: a telemedicine platform for facilitating remote oral medicine consultation and improving clinical examinations. Oral Surg Oral Med Oral Pathol Oral Radiol. 2016;121(3):248–254. doi: 10.1016/j.oooo.2015.11.005. [DOI] [PubMed] [Google Scholar]
- 5.Sahin D, Hacisalihoglu UP, Kirimlioglu SH. Telecytology: is it possible with smartphone images? Diagn Cytopathol. 2018;46(1):40–46. doi: 10.1002/dc.23851. [DOI] [PubMed] [Google Scholar]
- 6.Speiser JJ, Hughes I, Mehta V, Wojcik EM, Hutchens KA. Mobile teledermatopathology: using a tablet PC as a novel and cost-efficient method to remotely diagnose dermatopathology cases. Am J Dermatopathol. 2014;36(1):54–57. doi: 10.1097/DAD.0b013e3182863186. [DOI] [PubMed] [Google Scholar]
- 7.Fontelo P, Liu F, Yagi Y. Evaluation of a smartphone for telepathology: lessons learned. J Pathol Inform. 2015;6:35. doi: 10.4103/2153-3539.158912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Morrison AS, Gardner JM. Smart phone microscopic photography: a novel tool for physicians and trainees. Arch Pathol Lab Med. 2014;138:1002. doi: 10.5858/arpa.2013-0425-ED. [DOI] [PubMed] [Google Scholar]
- 9.Crane GM, Gardner JM. Pathology image-sharing on social media: recommendations for protecting privacy while motivating education. AMA J Ethics. 2016;18:817–825. doi: 10.1001/journalofethics.2016.18.8.stas1-1608. [DOI] [PubMed] [Google Scholar]
- 10.Isom J, Walsh M, Gardner JM. Social media and pathology: where are we now and why does it matter? Adv Anat Pathol. 2017;24:294–303. doi: 10.1097/PAP.0000000000000159. [DOI] [PubMed] [Google Scholar]