Abstract
Purpose
Surplus cryopreserved affected/aneuploid blastocysts may be obtained after in vitro fertilization (IVF) treatments with preimplantation genetic testing (PGT). These embryos are considered not suitable for transfer and may be discarded. Currently, in Italy, an embryo disposition decision (EDD) is not allowed and the frozen/vitrified blastocysts (even if affected/aneuploid) should be kept cryopreserved indefinitely. In this peculiar clinical, social, and legislative scenario, we aimed at assessing the attitudes of the patients towards the fate of these embryos, in case the local regulation would be changed and allow an EDD regarding the surplus affected/aneuploid embryos obtained after PGT.
Methods
A questionnaire with multiple answers was submitted to 832 patients who obtained affected/aneuploid embryos during a PGT cycle at our private IVF center. They were asked to choose between three putative options with related reasons: everlasting cryopreservation (only option currently available); discard or donate them to research.
Results
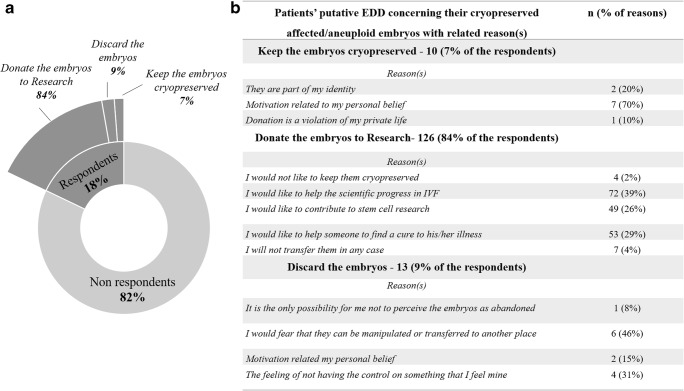
Overall, 149 patients (18%; 85 women and 64 men) answered the questionnaire. Among them, 84% (n = 126) would choose to donate their affected/aneuploid blastocysts to research, 9% (n = 13) would discard them and only 7% (n = 10) would keep them cryopreserved indefinitely.
Conclusions
Donation of the affected/aneuploid blastocysts is the option chosen from most of the respondents (84%; 15% of the eligible patients). These patients are motivated from the altruistic will of incentivating the progress in IVF and/or stem cell research and supporting future couples to limit/solve their infertility/health issues.
Electronic supplementary material
The online version of this article (10.1007/s10815-019-01465-2) contains supplementary material, which is available to authorized users.
Keywords: Surplus embryos, Donation, Preimplantation genetic testing, Embryo disposition decision, Affected embryos
Introduction
In in vitro fertilization (IVF) treatments, surplus embryos are commonly produced and cryopreserved. Indeed, the improvement of cryopreservation was essential to decrease the occurrence of ovarian hyperstimulation syndrome by the application of freeze-all strategy, to limit the use of multiple embryo transfer approach (and the related risk of multiple pregnancies), as well as to increase the cumulative chance of pregnancy in couples who fail to conceive after a fresh embryo transfer [1].
Patients with cryopreserved surplus embryos may be asked to make an embryo disposition decision (EDD) and state the fate of their embryos. These patients could choose to either warm or discard them, or to donate them to another couple or for research. Different scenarios involve an EDD: (i) one (or more) pregnancy obtained, (ii) divorce, (iii) death of a partner, or (iv) production of embryos affected from a monogenic disease and/or a chromosomal imbalance (i.e., aneuploid). Nonetheless, the possibility to decide of the fate of their embryos and to choose among the options previously listed varies between the IVF clinics around the world (https://www.iffs-reproduction.org/page/Surveillance). There are countries where an EDD is forbidden by the local Law and patients cannot decide upon the fate of their surplus embryos.
Interestingly, where allowed, several issues affect the EDD itself. It may be influenced by the personal representation of the embryo, which evolves during an IVF treatment and depends on its conceptualization, as well as by life circumstances, the evolution of parenthood, the information provided by the clinician/embryologist, the personal values, as well as demographic and psychosocial variables [2–13]. It has been reported that if the embryo is represented as a child, the patients may choose to discontinue its cryopreservation; instead, if the embryo is perceived as a project, they may choose to donate it for research; lastly, embryo donation to another couple is more likely chosen if it is perceived as a “potential person” [14].
In Italy, the current regulation (Constitutional Court Sentence n. 84 of the 22nd of March 2016) is very restrictive to this regard. Specifically, it forbids the use of cryopreserved embryos for purposes different from reproduction, and it obliges the IVF laboratories to provide a long-lasting (virtually everlasting) storage of cryopreserved embryos, also in the case of affected/aneuploid embryos. Indeed, we decided to examine which is the couple perspective in our private IVF center in Italy, where the Law does not allow an EDD.
We targeted this study to couples who underwent preimplantation genetic testing for monogenic diseases and/or aneuploidies (PGT-M and/or PGT-A), and who had at least one cryopreserved affected/aneuploid embryo. These embryos, if transferred, may result in an implantation failure, an early miscarriage, or the conception of a child affected from a monogenic or chromosomal disease [15–17]. Therefore, they will remain cryopreserved in almost all the cases with no purpose.
Materials and methods
This is an observational cohort study conducted between March and December 2017 in the psychological department of a private IVF center in Rome, Italy. We included all the patients that underwent IVF with PGT-M and/or PGT-A from to January 2015 to December 2016 and had surplus affected/aneuploid cryopreserved embryos. The patients (both male and female partners, n = 832) were invited by email to fill in a questionnaire on a supposed EED, in case the Italian Law would have allowed them to make a choice. The email, in case they would accept to participate, redirected them to a specific webpage. The questionnaire was developed by the team of psychologists of the IVF center, based on similar previously published studies focused on this subject [7, 18], and was composed on four items with multiple choices dealing with cryopreserved affected and/or aneuploid embryos (questionnaire shown in Supplementary Table 1). Each patient could choose among different options: (i) keep the embryos cryopreserved, (ii) donate the embryos for research, or (iii) discard the embryos. In case of no response, the same email was re-sent 3 months later, and again a last time 6 months later. The data were anonymized and analyzed from an independent operator. The main socio-demographic variables included in the analysis as putative effectors were gender, indication to PGT, age, and outcome of the IVF treatment (i.e., pregnancy achieved, implantation failure, no transferable embryo produced, or no embryo transfer yet performed for other reasons). The institutional review board (IRB) of Clinica Valle Giulia approved the study. Signed informed consent to participate to the study was obtained from all recruited patients.
Statistical analysis
Chi-squared test was used to determine significant differences among the distribution of the interviewed patients according to the different putative choices. The software G*Power was adopted to define the statistical power of the analysis. A logistic regression was conducted to assess the putative factors influencing each patient choice. The dependent variable was dichotomous: keep the affected/aneuploid embryos cryopreserved (only possibility allowed at present by the Italian Law) or donate/discard them (alternative choice). The independent variables investigated were age, gender (male or female), indication to PGT, and outcome of their own IVF cycle (pregnancy achieved or not).
Results
Out of 832 patients invited, 149 completed the questionnaire (17.9%) (Fig. 1). Among them, 85 were women and 64 were men. Among them, 4 men and 4 women belong to the same couple. The socio-demographic characteristics of the respondents are shown in Table 1. Most patients would choose to donate their cryopreserved affected/aneuploid embryos to research (84%).
Fig. 1.
Summary of the responses of the patients invited to fill the questionnaire dealing with a putative embryo disposition decision (EDD) concerning their affected/aneuploid cryopreserved embryos in case the Italian Law would allow it (a), with related reason(s) (b)
Table 1.
Socio-demographic data regarding the patients who responded to the questionnaire
| Patients, tot, n | 149 |
| Women, n (%) | 85 (57.0%) |
| Mean female age ± SD (year) | 39.7 ± 3.9 |
| Men, n (%) | 64 (43.0%) |
| Mean male age ± SD (year) | 43.8 ± 6.6 |
| Reason for PGT | |
| PGT-A, n (%) | 133 (89.3%) |
| PGT-M, n (%) | 9 (6.0%) |
| PGT-M and PGT-A, n (%) | 7 (4.7%) |
| Outcome IVF treatment | |
| Positive pregnancy test, n (%) | 98 (65.8%) |
| Negative pregnancy test, n (%) | 19 (12.7%) |
| No transferable embryos produced, n (%) | 28 (18.8%) |
| No embryo transfer for other reason, n (%) | 4 (2.7%) |
PGT preimplantation genetic testing, PGT-A PGT for aneuploidies, PGT-M PGT for monogenic diseases
Only 7% of the patients would choose to keep their affected and/or aneuploid embryos stored even if the Law would be changed. To discard affected/aneuploid embryos would be the choice of just 9% of the interviewed patients who responded to the questionnaire. To summarize, 93% of the respondents (which represent 16.6% of the total population to whom we submitted the questionnaire), would choose, if allowed by the Law, to either donate or discard their affected/aneuploid embryos. This rate is significantly higher compared to the 7% of patients who would keep them cryopreserved, the only option currently allowed by the Italian Law (p < 0.01; post hoc power 99.9%).
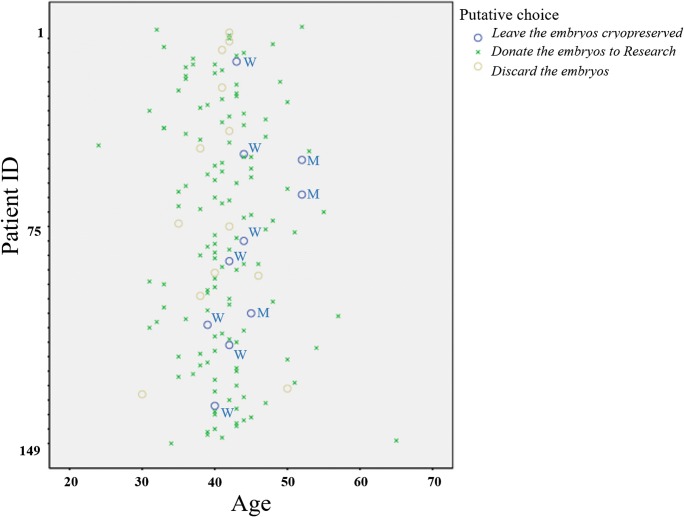
The logistic regression analyses conducted showed that the only variable which can influence the putative choice of each patient was his/her age corrected for the gender. Specifically, the odds ratio of making a choice different from the only option currently available was 0.85, 95% CI 0.74–0.98 (p = 0.03). None of the other variables from this dataset, besides the gender, showed an effect or can modulate this result. Figure 2 displays the putative choice of each patient dispersed according to their age. Clearly, all the patients that would choose to keep the embryos cryopreserved even if the Italian Law would allow an EDD are older than 40 years. Specifically, all the women (“W”) clustered in the range 40–45 years, and the 3 men (“M”) were all older than 46 years.
Fig. 2.
Distribution of the putative embryo disposition decisions (EDDs) of the respondents according to their age. The logistic regression analysis highlighted that only the age of the patients corrected for their gender was correlated with a putative choice to “leave the embryos cryopreserved” in case the Italian Law would allow a free EDD (OR 0.85; 95% CI 0.74–0.98; p value 0.03). Here, the blue dots represent that choice (W stands for “Woman,” and M stands for the “Man”) distributed according to the patients and their age
Discussion
The number of patients undergoing PGT is increasing worldwide; therefore, also the number of cryopreserved affected/aneuploid embryos is growing [19, 20]. In Italy, the Law does not allow an EDD yet, and currently these embryos can only be kept cryopreserved, despite of patients’ will.
In a previous study by Bruno and colleagues, the patients’ mental representation of the embryo was the main variable influencing their choice whether to donate or not the surplus embryos produced during an IVF cycle [14]. Specifically, after adjusting the data for age, gender, origin of the gametes, and number of previous conceptions, they reported that a choice to “stop cryopreservation” was more frequent if the embryo was represented as a child. Conversely, if the embryo was represented as a project, the patients were more prone to donation to research. Finally, if the embryo was represented as a potential individual, donation to another couple was the most frequent choice. In general, though, the authors underlined that once the embryos are cryopreserved, it is more difficult to choose to stop cryopreservation to discard them. Similarly, two other studies highlighted a higher inclination of the patients towards donating surplus embryos to research rather than discarding or donating them to other couples [7, 11].
This is the first study to our knowledge that evaluated a putative EDD by patients obtaining at least one affected/aneuploid embryo after PGT, whom they did not intend to transfer. Currently, the Italian Law does not allow a free choice, which then can only be hypothetical. In this scenario, the patients could express an opinion not biased from mental, legal, or psychological influences, as for instance the symbolic value represented from the embryo. Furthermore, we arranged a computerized questionnaire which was analyzed in an anonymous fashion to limit the putative influence of a phone interview upon patients’ opinion. The email inviting the patients to participate to this study was sent two more times (every 3 months) in case of no response. However, only ca.20% of the invited patients responded to the questionnaire. The population of respondents in this study should be therefore considered only a sub-population of the infertile patients that underwent IVF with PGT at a private Italian clinic. Possibly, a cluster of men and women are more sensible to the issue under investigation. The key result of this study, namely, the nearly unanimous (ca.85% of the respondents) inclination towards donating the affected/aneuploid cryopreserved embryos to research, must be then commented accordingly. Importantly, also this result is intriguing and in countertendency with the local regulation. In fact, currently in Italy, it is not possible to conduct Research with embryos produced in Italian centers, but stem cells can be imported from abroad and used to this end. This is another odd situation, which may have affected the patients’ opinion and choice.
Interestingly, the only patients who would keep their embryos cryopreserved, regardless of their affected/aneuploid genetic status, were older than 40 years and mostly women. The main reason for this putative choice would be their personal belief. This suggests a higher attachment from older patients to the embryos they maybe struggled to obtain, and therefore are less prone to donate. Probably, these embryos, even if affected/aneuploid represent a last hope to their biological limitation to conceive spontaneously. In this way these women could mentally “freeze” the problem indefinitely. Finally, 9% of patients would choose to discard their surplus embryos.
Our sample size did not allow the evaluation of a putative influence, among the patients that underwent PGT-M, of the specific condition they were carrier of, which is indeed an interesting future perspective. In fact, these embryos may result, if transferred, in a live birth of children affected from a monogenic disease (differently from aneuploid embryos that, except from vital trisomies and sex chromosome aneuploidies, mostly result into implantation failures and miscarriages), and therefore involve a different level of psychological and ethical evaluation. Moreover, future larger studies are desirable also to perform a more in-depth analysis that should address, among the patients that prefer taking a choice different from everlasting cryo-storage, what are the reasons for donating them to Research rather than discarding them.
This study is limited to patients that have spontaneously responded to the questionnaire, which does not allow a generalized overview and may possibly not represent the opinion of the whole population. Moreover, we could not analyze the level of concordance among patients belonging to the same couple, which was possible only for 8 of the respondents. Within these 8 patients, the choice that the couple would make was the same, i.e., donation to research. Future investigations are required to outline the concordance and discordance rate of the opinion within the couples, which is a critical information, since a final EDD is strictly dependent on a common view. Otherwise, a couple-oriented rather than patient-oriented design is suggested for future studies.
The Italian scenario dealing with surplus embryos is quite peculiar especially when compared with other countries worldwide. In the International Federation of Fertility Societies (IFFS) Surveillance of 2013 (https://www.iffs-reproduction.org/page/Surveillance), 54 delegates were specifically interrogated on their national policy regarding embryo experimentation. Twenty among these countries were European and only in Austria, Turkey, Ireland, and Italy, such options were reported as forbidden. Nevertheless, even where no experimentation is allowed, still surplus embryos might be discarded, like it happens in Austria after a 10-year period [21]. Italian couples therefore face a unique restriction of their decisional autonomy and the reasons for such uniqueness are ascribable to the legal, bioethical, and religious status of each embryo in our country: the embryo, even if affected and/or aneuploid, cannot be merely considered biological material and they are therefore conferred the same dignity of a human being. Since discarding or donating an embryo for research challenges such definition, no other fate is allowed other than indefinite long-term cryo-storage (Sentence 229/2015 of the Italian Constitutional Court). In this regard, more studies are warmly suggested in other countries with a different regulation, social, and religious background. This topic is clearly opened to multiple points of view which will inspire a fruitful international discussion with unpredictable implications.
To our knowledge, this design and the related data, especially in such a peculiar social and legislative scenario (i.e., Italy), are novel and may involve a proactive discussion in the scientific community. Indeed, the application of a freeze-all policy in an IVF/PGT cycle is common, if not mandatory, and the number of affected/aneuploid cryopreserved embryos is destined to keep increasing in the future.
Electronic supplementary material
(DOCX 21.6 kb)
Authors’ contribution
FF, MF, AC, and LR designed the study. FF, MF, and DC analyzed the data and drafted the manuscript. All authors contributed to the interpretation of the data and their discussion.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Rienzi L, Gracia C, Maggiulli R, LaBarbera AR, Kaser DJ, Ubaldi FM, et al. Oocyte, embryo and blastocyst cryopreservation in ART: systematic review and meta-analysis comparing slow-freezing versus vitrification to produce evidence for the development of global guidance. Hum Reprod Update. 2017;23(2):139–155. doi: 10.1093/humupd/dmw038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.de Lacey S. Parent identity and ‘virtual’ children: why patients discard rather than donate unused embryos. Hum Reprod. 2005;20(6):1661–1669. doi: 10.1093/humrep/deh831. [DOI] [PubMed] [Google Scholar]
- 3.Lyerly AD, Steinhauser K, Namey E, Tulsky JA, Cook-Deegan R, Sugarman J, et al. Factors that affect infertility patients’ decisions about disposition of frozen embryos. Fertil Steril. 2006;85(6):1623–1630. doi: 10.1016/j.fertnstert.2005.11.056. [DOI] [PubMed] [Google Scholar]
- 4.Lyerly AD, Steinhauser K, Voils C, Namey E, Alexander C, Bankowski B, Cook-Deegan R, Dodson WC, Gates E, Jungheim ES, McGovern P, Myers ER, Osborn B, Schlaff W, Sugarman J, Tulsky JA, Walmer D, Faden RR, Wallach E. Fertility patients' views about frozen embryo disposition: results of a multi-institutional U.S. survey. Fertil Steril. 2010;93(2):499–509. doi: 10.1016/j.fertnstert.2008.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Newton CR, Fisher J, Feyles V, Tekpetey F, Hughes L, Isacsson D. Changes in patient preferences in the disposal of cryopreserved embryos. Hum Reprod. 2007;22(12):3124–3128. doi: 10.1093/humrep/dem287. [DOI] [PubMed] [Google Scholar]
- 6.Hug K. Motivation to donate or not donate surplus embryos for stem-cell research: literature review. Fertil Steril. 2008;89(2):263–277. doi: 10.1016/j.fertnstert.2007.09.017. [DOI] [PubMed] [Google Scholar]
- 7.Mohler-Kuo M, Zellweger U, Duran A, Hohl MK, Gutzwiller F, Mutsch M. Attitudes of couples towards the destination of surplus embryos: results among couples with cryopreserved embryos in Switzerland. Hum Reprod. 2009;24(8):1930–1938. doi: 10.1093/humrep/dep103. [DOI] [PubMed] [Google Scholar]
- 8.Nachtigall RD, Mac Dougall K, Harrington J, Duff J, Lee M, Becker G. How couples who have undergone in vitro fertilization decide what to do with surplus frozen embryos. Fertil Steril. 2009;92(6):2094–2096. doi: 10.1016/j.fertnstert.2009.06.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Provoost V, Pennings G, De Sutter P, Dhont M. “Something of the two of us”. The emotionally loaded embryo disposition decision making of patients who view their embryo as a symbol of their relationship. J Psychosom Obstet Gynaecol. 2012;33(2):45–52. doi: 10.3109/0167482X.2012.676111. [DOI] [PubMed] [Google Scholar]
- 10.Provoost V, Pennings G, De Sutter P, Gerris J, Van de Velde A, De Lissnyder E, et al. Infertility patients’ beliefs about their embryos and their disposition preferences. Hum Reprod. 2009;24(4):896–905. doi: 10.1093/humrep/den486. [DOI] [PubMed] [Google Scholar]
- 11.Provoost V, Pennings G, De Sutter P, Van de Velde A, Dhont M. Trends in embryo disposition decisions: patients’ responses to a 15-year mailing program. Hum Reprod. 2012;27(2):506–514. doi: 10.1093/humrep/der419. [DOI] [PubMed] [Google Scholar]
- 12.Jin X, Wang G, Liu S, Liu M, Zhang J, Shi Y. Patients’ attitudes towards the surplus frozen embryos in China. Biomed Res Int. 2013;2013:934567. doi: 10.1155/2013/934567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Samorinha C, Pereira M, Machado H, Figueiredo B, Silva S. Factors associated with the donation and non-donation of embryos for research: a systematic review. Hum Reprod Update. 2014;20(5):641–655. doi: 10.1093/humupd/dmu026. [DOI] [PubMed] [Google Scholar]
- 14.Bruno C, Dudkiewicz-Sibony C, Berthaut I, Weil E, Brunet L, Fortier C, Pfeffer J, Ravel C, Fauque P, Mathieu E, Antoine JM, Kotti S, Mandelbaum J. Survey of 243 ART patients having made a final disposition decision about their surplus cryopreserved embryos: the crucial role of symbolic embryo representation. Hum Reprod. 2016;31(7):1508–1514. doi: 10.1093/humrep/dew104. [DOI] [PubMed] [Google Scholar]
- 15.Hassold T, Hunt P. To err (meiotically) is human: the genesis of human aneuploidy. Nat Rev Genet. 2001;2(4):280–291. doi: 10.1038/35066065. [DOI] [PubMed] [Google Scholar]
- 16.Heffner LJ. Advanced maternal age--how old is too old? N Engl J Med. 2004;351(19):1927–1929. doi: 10.1056/NEJMp048087. [DOI] [PubMed] [Google Scholar]
- 17.Nagaoka SI, Hassold TJ, Hunt PA. Human aneuploidy: mechanisms and new insights into an age-old problem. Nat Rev Genet. 2012;13(7):493–504. doi: 10.1038/nrg3245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bangsboll S, Pinborg A, Yding Andersen C, Nyboe Andersen A. Patients’ attitudes towards donation of surplus cryopreserved embryos for treatment or research. Hum Reprod. 2004;19(10):2415–2419. doi: 10.1093/humrep/deh441. [DOI] [PubMed] [Google Scholar]
- 19.De Rycke M, Goossens V, Kokkali G, Meijer-Hoogeveen M, Coonen E, Moutou C. ESHRE PGD Consortium data collection XIV-XV: cycles from January 2011 to December 2012 with pregnancy follow-up to October 2013. Hum Reprod. 2017;32(10):1974–1994. doi: 10.1093/humrep/dex265. [DOI] [PubMed] [Google Scholar]
- 20.Harper JC, Wilton L, Traeger-Synodinos J, Goossens V, Moutou C, SenGupta SB, et al. The ESHRE PGD Consortium: 10 years of data collection. Hum Reprod Update. 2012;18(3):234–247. doi: 10.1093/humupd/dmr052. [DOI] [PubMed] [Google Scholar]
- 21.Samorinha C, Silva S. A patient-centred approach to embryo donation for research. Isr J Health Policy Res. 2016;5:44. doi: 10.1186/s13584-016-0098-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 21.6 kb)