Abstract
Background:
Workplace violence (WPV) in the health care sector remains a prominent, under-reported global occupational hazard and public health issue.
Objective:
To determine the types and prevalence of WPV among doctors.
Methods:
Primary papers on WPV in medicine were identified through a literature search in 4 health databases (Ovid Medline, EMBASE, PsychoINFO and CINAHL). The study followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines for the mapping and identification of records. To assess the studies included in our review, we used the Critical Appraisal Skills Programme cohort review checklist and the Risk of Bias Assessment.
Results:
13 out of 2154 articles retrieved were reviewed. Factors outlining physician WPV included (1) working in remote health care areas, (2) understaffing, (3) mental/emotional stress of patients/visitors, (4) insufficient security, and (5) lacking preventative measures. The results of 6 studies were combined in a meta-analysis. The overall prevalence of WPV was 69% (95% CI 58% to 78%).
Conclusion:
The impact of WPV on health care institutions is profound and far-reaching; it is quite common among physicians. Therefore, steps must be taken to promote an organizational culture where there are measures to protect and promote the well-being of doctors.
Keywords: Physicians, Workplace violence, Systematic review [publication type], Meta-analysis [publication type], Occupational medicine
TAKE-HOME MESSAGE
In the health care sectors, workplace violence (WPV) is the most under-reported global occupational hazard.
This study was conducted to determine the types and prevalence of WPV among doctors.
WPV can appear in many ways (physical, verbal, sexual, etc) and lead to a multitude of negative consequences for physicians worldwide.
Several steps must be taken to promote an organizational culture where there are measures to protect and promote the well-being of health care workers.
Introduction
Workplace violence (WPV) in the health care sector remains a prominent, under-reported global occupational hazard. Currently, more than 50% of employees and approximately 25% of physicians from the emergency department reported encounters of physical assaults.1-5 The prevalence is likely even higher in some settings such as mental health units where physicians experience verbal and physical violence repeatedly due to the nature of their patients.4 Doctors worldwide typically endure verbal abuse, threats or actual physical violence from patients or their family members (type II violence), and even physicians and their co-workers (type III violence).6-8 An incident of an intoxicated patient striking a physician during the initial examination is an example of type II WPV.4,9 In type III WPV, the perpetrator is a current or former employee of the organization; a recently fired worker assaulting his or her former manager is an example of type III WPV.4,9
Research efforts have been made to identify antecedent factors of WPV to help create preventative interventions and understand the economic, health, as well as social consequences associated with WPV.15 However, a review of the literature has demonstrated that there are inconsistencies in results reported.3,4
The more developed areas in research look at perpetrators of WPV (eg, patients) and their victims (eg, physicians) as well as quantifications of violent encounters.4 Investigators have yet to identify experimental approaches that comprise an applicable model to mitigate WPV risk reduction and to identify the underlying mechanisms and antecedent factors.10 It is also improbable that a basic, “one-size-fits-all” model can be developed as a method for violence prevention.10,11 Even though violence prevention training is widely available for employees, this has been unsuccessful so far in reducing rates of occurrence for WPV.12 Furthermore, physicians tend to underreport many violent incidents due to the common health care principle which accepts violence as “part of the job”12. Thus, accentuating the gaps in WPV statistical knowledge since health care providers often do not hold their assailants responsible for their behavior.13 A large focus on customer service in the health care sector acts as a secondary deterrent to WPV reporting since the approach remains that the “customer is always right.”14 Nonetheless, we still see a significantly large incidence of WPV among physicians in the health care sector that remains to be addressed.
Research has shown that emergency physicians are at a higher risk of WPV due to the large intake of patients in various states (eg, intoxicated, delirious, etc) and report higher rates of mental distress.21 If physicians are experiencing poor mental health due to occupational stressors, a higher rate of medical mistakes and poorer patient outcomes are to be expected.15-17 In response, coping mechanisms are typically common; physicians use them to escape or avoid certain situations that they associate with their WPV experience, in addition to seeking social support.18
Given the high rates of WPV in the health care sector, and its impact on the mental health of physicians, financial losses to the institutions and poorer patient outcomes, it is essential to prioritize prevention of WPV. There are many diverse estimates of WPV prevalence, but the causes are still not clearly known in a specific setting. The objective of this systematic review was therefore to identify the antecedent factors of type II and type III WPV present in the work environment of doctors. Moreover, a meta-analysis was completed to estimate the prevalence of WPV among doctors in these settings.
Materials and Methods
This systematic review is registered with the PROSPERO (international prospective register of systematic reviews) under CRD42017070159. The following databases were utilized for the collection of relevant publications: Ovid Medline (1946 to November 17, 2018), EMBASE (1980 to November 17, 2018), PsychoINFO (2002 to November 17, 2018), and CINAHL (1982 to 2018) using a PICO framework to assist and refine the search process.
Search Strategy and Study Selection
The search criteria were finalized with the assistance of a health research librarian; all articles chosen were published in English. Our process complied with the requirements of each database used (Appendix). The selected articles were retrieved on September 16, 2016 and updated on November 17, 2018. The studies chosen for this review contained information regarding various types of WPV (eg, patient on worker violence, and worker on worker violence) that physicians are exposed to, as well as the antecedent factors and repercussions of these violent occurrences.
Inclusion and Exclusion Criteria
The studies chosen for this review contained information regarding type II or type III WPV. For example, they may include client on worker violence, and worker on worker violence that physicians are exposed to, as well as the antecedent factors and repercussions of these violent occurrences. The study followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines for the mapping and identification of records. A data extraction form was used based on the Systematic Review Data Repository (http://srdr.ahrq.gov) from the US Department of Health and Human Services. Three reviewers took part in accurately sorting and assembling the acquired data in an organized fashion. The information sought out from each article was the type of WPV, the type of injury assessed, the type of worker injured (eg, doctors), the antecedent factors to an occupational injury, sample size, author, and year and country of publication. Any discrepancies were thoroughly discussed and voted on by the rest of the research team.
Article Assessment
To assess the studies included in our review, we used the Critical Appraisal Skills Programme (CASP) cohort review checklist.19 This tool was used by three reviewers to evaluate the relevance, validity, and quality of each article. The first 12 questions were considered. A composite score was then generated from the questions and reported for each article.
The risk of bias was examined using the Cochrane Collaboration “risk of bias” assessment tool across six domains (selection bias, performance bias, detection bias, attrition bias, reporting bias, and other biases).20 An overall summary of the risk of bias for each study was reported. A study was considered “low risk” if attrition bias due to missing data was unlikely to be related to WPV (eg, for survival analysis data, censoring was unlikely to introduce bias). A study was designated “unclear” if there was insufficient information to determine its risk of bias. Eligible for inclusion in this meta-analysis were all prospective studies that addressed the prevalence of WPV among physicians, such as sociodemographic factors, health (behavior), mental health, psychosocial work factors, personal factors, and organizational factors, on sickness absence of physicians.
Definition of Workplace Violence
WPV can be defined as violence, such as assault or threat of assault, involving an individual performing their job duties.4 For this review, WPV can be characterized according to the type of relationship between the two involved parties.
Statistical Analysis
A meta-analysis of proportions was performed using the data obtained from selected articles. An arcsine transformation was applied to establish the variance of proportions (Freeman-Tukey variant of the arcsine square root of transformed proportions method). The pooled proportion was calculated as the back-transformation of the weighted mean of the transformed proportions, using inverse arcsine variance weights for the random effects model. We applied DerSimonian-Laird weights for the random effects model. The I2 statistic was also calculated as a measure of the overall variation in the proportion that was attributable to between-study heterogeneity. All analyses were performed with R 3.4.3 using “metafor” package for the meta-analysis of proportions.21,22 The standard meta-analytic procedures assumed that results were independent.
Results
Summary of Study Findings
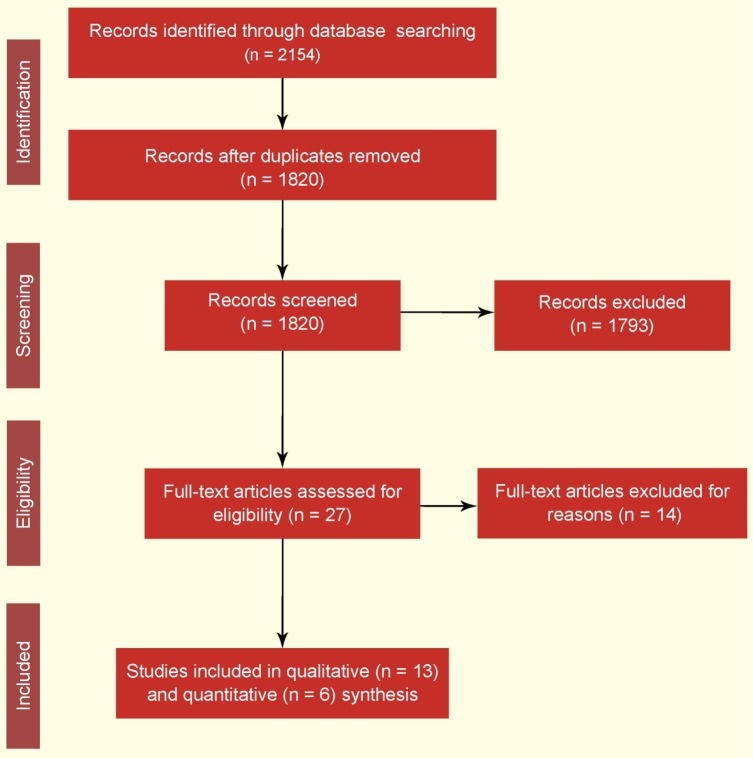
A total of 13 out of 2154 articles retrieved was reviewed (Fig 1).5,18,23-33 The mean CASP score was 8.54 (SD 1.05, range 7 to 10). The articles were categorized by the type of violence (patient on worker violence and client on worker violence and worker on worker violence). The majority of the articles reviewed report type II violence (92%); one study (8%) reports type III. Our systematic review outlined the following factors for physician WPV: (1) working in remote health care areas, (2) understaffing, (3) mental/emotional stress of patients/visitors, (4) insufficient security, and (5) lacking preventative measures. Subsequently, six of the articles wherein data were available, were included in a meta-analysis of the prevalence of WPV.
Figure 1.
Flow diagram of the inclusion process. Number of articles after removing duplicates: Medline (n = 466), PsycInfo (n = 718), CINAHL (n = 334), and EMBASE (n = 636)
All of the studies included were descriptive and cross-sectional in nature.5,18,23-26,28,29,31-33, Eight included mental/emotional correlates associated with WPV against doctors.5,18,25,28,30-32, For example, perpetrators of WPV were those with an altered state of mind or with behavioral issues such as aggression5,26,32 or substance use such as alcohol or drugs32. Verbal insults, witnessing WPV, threats, and physical aggression were also contributing factors to WPV.25
One study identified insufficient organizational resources, understaffing, and lack of management support as the main causes of WPV. Baykan, et al, found that 86.4% of physicians were exposed to physical, verbal, and sexual violence during their employment.24 Factors associated with WPV included environmental factors and excessive demands of patients on doctors and using doctors as their scapegoat.
Insufficient security was another factor associated with increased WPV among doctors. Specifically, physical violence led to decreased doctors retention in their current position; both bullying and physical violence led to reduced job satisfaction.27,29 Evidence also suggests WPV occurred more frequently in remote or underserved areas.23 Furthermore, contributing factors to WPV were related to the absence of organizational policies, inadequate staffing and lack of communication skills.23 Male doctors were more often the subject of physical abuse (27.6%) than female doctors (16.2%). On the other hand, females (64.1%) were victims of non-physical violence more often than males (53.1%).29
The organizational climate included lack of preventive measures to impede WPV. Doctors who did not attend preventative violence training sessions due to a gap in hospital management, lack of experience, and higher workloads were more prone to WPV.33
Quality Assessment
The overall risk of bias for all but one of the studies was low across the six domains of biases studied (Table 1). One study was categorized as “unclear” due to insufficient information provided. Overall, the study signifies the necessity of job control as a buffer for stressful working environments subjected to WPV.
| Table 1: Characteristics and antecedent factors of type II and type III studies of workplace violence among doctors | ||||
| Author, year, country |
Sample size, years examined, study
design, type of violence |
Antecedent factors | CASP grade | Summary risk of bias |
| 1. AbuAlRub and Al Khawaldeh, 2014, Jordan | n=521, 2013–2014, descriptive/exploratory research design, type II |
> Patient on worker violence: - Factors related to administration (ie, no assertive legislations, ineffective solutions for violent incidents, long shift hours, short level of staff, inappropriate work environments, lack of sources provided) - Factors related to staff (ie, lack of communication, poor quality care, lack of proper training giving rise to inexperienced staff) - Factors related to their patients and families (ie, increased level of anxiety and tension, notions of poor-quality health care, life stress, no/lack of health insurance) - Factors related to security (ie, inexperienced or simply unqualified security staff, increased traffic of public and visitors' access, uncontrolled visiting time) |
7 | Low risk |
| 2. Baykan et al, 2015, Turkey | n=597, 2012, descriptive study, type II |
> Patient on worker violence: - Environmental factors - Attitudes of politician/managers, media and uneducated locals - Excessive demands of patients - Patients using doctors as their scapegoat, immediate resolvent |
10 | Low risk |
| 3. da Silva et al, 2015, Brazil | n=2940, unspecified, cross-sectional, type II |
> Patient on worker violence: - Depressive symptoms and major depression (ie, more prone to react when faced with complaints or aggressive behavior) - Patients being disappointed from having high expectations of service |
8 | Low risk |
| 4. Hahn et al, 2012, Switzerland | n=2495, 2007, cross-sectional survey, type II |
> Patient on worker violence: - Those trained in aggression management - Professionals working with patients over the age of 65 - Professionals who work in emergency rooms, outpatient rooms, intensive care units, recovery rooms, anesthesia, intermediate care and step-down units |
9 | Low risk |
| 5. Heponiemi et al, 2014, Finland | n=1515, 2006–2010, cohort study, type III |
> Worker on worker violence: - Decrease in job control (ie, lack of opportunities to learn and improve on skills, lack a variety of tasks) > Patient on worker violence: - No direct measures like no metal detectors for metal weapons, no security dog teams, no cameras and security personnel all-in-all to decrease/prevent WPV |
9 | Low risk |
| 6. Hills and Joyce, 2014, Australia | n=9449, 2010–2011, cross-sectional descriptive, type II |
> Patient on worker violence: - Patient with a medical condition or undergoing psychosocial circumstances - Patient with cognitive impairment or arousal, frustration or distress > Worker on worker violence: - Less experienced clinicians |
9 | Low risk |
| 7. Kitaneh and Hamdan, 2012, Jerusalem | n=271, 2011, cross-sectional, type II |
> Patient on worker violence: - Less experience, low level of education, under-reporting due to fear of consequences, lack of management support |
9 | Low risk |
| 8. Mantzouranis et al, 2015, Greece | n=175, 2013, descriptive study using questionnaire, type II |
> Patient on worker violence: - Long wait times - Patient with drug and alcohol abuse - Patient with psychiatric disorders - Disobedience of patients, relatives and friends - Lack of sufficient personnel on site |
9 | Low risk |
| 9. Pompeii et al, 2015, USA | n=2098, unspecified, descriptive, type II |
> Patient on worker violence: - Altered mental status, behavioral issues - Patient with pain/medication - Patient dissatisfied with care |
7 | Low risk |
| 10. Vezyridis, Samoutis, and Mayrikiou, 2015, Cyprus | n=220, 2012–2013, cross-sectional, type II |
> Patient on worker violence: - Altered mental status, behavioral issues - Patient with pain/medication - Patient dissatisfied with care |
9 | Low risk |
| 11. Vorderwulbeck, et al, 2015, Germany | n=831, 2013, questionnaire-based, type II |
> Patient on worker violence: - Patient who uses alcohol - Patient who uses drugs - Patient with mental illness |
8 | Low risk |
| 12. Wu et al, 2015, Taiwan | n=189, 2009, cross-sectional, type II |
> Patient on worker violence: - Vast increase in health services volume and so as a consequence, short consultations occur which in turn will anger patients - Safety climate (a protective factor for WPV that mediates the relationship between work-derived violence and negative consequences, job satisfaction and work engagement) - Excessive volume of physicians' job demands which can result to poor quality service leading to angered patients - Hospital administration needing to ensure enough health care staffing levels to prevent WPV |
7 | Unclear risk; used convenient sampling for recruitment may pose some bias |
| 13. Zafar et al, 2016, Pakistan | n=179, 2013, cross-sectional, type II |
> Patient on worker violence: - Mental health |
10 | Low risk |
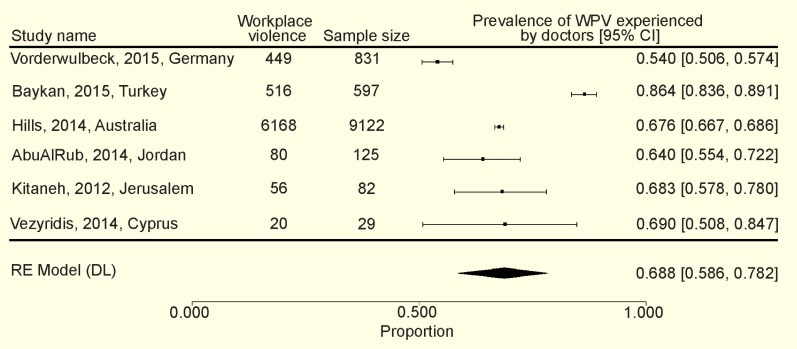
Meta-analysis
The overall prevalence of WPV pooled from the results reported in six studies was 69% (95% CI 58% to 78%) (Fig 2).23,24,28,29,31,32 The I2 statistic was 0.974. Thus, a random-effect model was used.34
Figure 2.
Prevalence of workplace violence among physicians
Discussion
Violence in the workplace can appear in many ways (physical, verbal, sexual, etc) and lead to a multitude of negative consequences for physicians worldwide, as demonstrated by this study. The perpetrators, causes, and consequences of WPV are not always clear, because of under-reporting and lack of investigative efforts by managing bodies.24,29,30 However, given the severity of WPV on physician well-being, it is crucial to better understand WPV itself, and the impact of inaction.
Our systematic review identified that the majority of incidents reported by participating physicians were preventable. Most respondents were also very dissatisfied with the way their violent incidents were handled/investigated.25,29 This evidence further accentuates the need for attention and action from international administrative bodies to confront WPV by implementing additional protocols. Specifically, financial investments should be made to mitigate WPV and help workers who have already experienced WPV (regardless of the type of violence).18
The study found that most doctors were susceptible to type II WPV (92% of articles) regardless of their work environment, organizational culture and structure, and access to resources. The prevalence of WPV against doctors in health care settings is high, however these data are difficult to compare.35 In the literature, comparisons of WPV prevalence rates across countries range from 54% in Thailand36 to 70% in Morocco37. The results are heterogenous, making comparison across countries challenging. Nonetheless, this systematic review supports the argument that exposure to WPV has deleterious health outcomes for doctors and provides an opportunity for target workplace interventions.38 Specifically, mental health interventions could examine the consequences of burnout,39 decreased job performance,40 depression,41 and post-traumatic stress disorder42 in doctors who experience WPV. These interventions may include health promotion strategies (eg, mindfulness meditation), limiting the exposure to violence or providing resources to reduce workload demands.
At the policy level, prevention must be placed into existing occupational health and safety legislations to provide strategies for prevention and management of WPV, promote its reporting and follow up, and provide supports to physicians who experienced violence. Furthermore, the systematic review outlines predictors and consequences by type of WPV against physicians; it also implies possible solutions that can rectify these incidents and tackle their consequences. Specifically, studies from Brazil, Germany, Pakistan, Taiwan, and the USA emphasize the importance of addressing the mental health needs of physicians who have experienced WPV implementing strategies to prevent WPV.
The consequences of inaction against violent incidents towards physicians are severe. Some of these include (1) waste of time, (2) mental health problems (PTSD, depression, burnout, depersonalization), (3) lack of sense of safety/protection, and (4) emotional distress (anger, humiliation, fear, guilt).18,30 One such approach would be to implement mental health first aid training so that physicians are more confident about interacting with individuals experiencing a mental health problem or crisis. Furthermore, there should be an increase in resources available to physicians in crisis (as a result of experiencing WPV) or experiencing mental health problems. The available evidence shows that 69% of physicians were subjected to various types of WPV (physical, verbal, sexual, etc). Physical, verbal, and sexual violence were different types of WPV reported in 62% of physicians who faced moderate WPV; 38% experienced severe WPV.10 Furthermore, this review supports evidence from a 2014 survey on hospital crime that type II WPV accounted for 75% of aggravated assaults and 93% of all assaults against workers.43
Despite all efforts we made to estimate the prevalence of WPV, the study has several limitations. WPV is a complex health and social issue with a multifactorial etiology.35 As a result, the comprehensiveness of this meta-analysis is difficult to reach. For instance, it is not feasible to infer a homogenous association between all the factors linked with WPV among physicians. Nonetheless, we included these studies because they offer important factors that are different from one another and each could provide a meaningful and distinct contribution to the meta-analysis. Another limitation was that the data were limited by what the authors reported, and upon additional solicitation, six of the 13 studies shared their physician data for this meta-analysis. Moreover, the studies included in the systematic review were cross-sectional and exploratory in nature, restricting the inferences that are possible.
The impact of WPV on health care institutions is profound and far-reaching. Therefore, steps must be taken to promote an organizational culture where there are measures to protect and promote the well-being of doctors. Our recommendations are to encourage policy amendments that may begin to alleviate the negative impacts of WPV against physicians, including to (1) create clear and reliable procedures for reporting aggressive acts (regardless of the type of violence), (2) establish thorough organizational guidelines to protect doctors, (3) utilize assessment teams (eg, through the use of existing joint occupational health and safety committees) to increase security in vulnerable areas, and (4) improve staffing methods and permit doctors time off work to recover and return to work. Furthermore, there is a need for training and workshops for health professionals in advance to recognize the signs and situations that increase the risk of WPV and ways to defuse aggression. Such workshops should be implemented as part of health and safety training and include refresher courses on a regular basis.
Conflicts of Interest:
None declared.
Cite this article as: Nowrouzi-Kia B, Chai E, Usuba K, et al. Prevalence of type II and type III workplace violence among physicians: A systematic review and meta-analysis. Int J Occup Environ Med 2019;10: 99-110. doi: 10.15171/ijoem.2019.1573
References
- 1.Kowalenko T, Gates D, Gillespie GL. et al. Prospective study of violence against ED workers. Am J Emerg Med. 2013;31:197–205. doi: 10.1016/j.ajem.2012.07.010. [DOI] [PubMed] [Google Scholar]
- 2.Kowalenko T, Walters BL, Khare RK. et al. Workplace violence: a survey of emergency physicians in the state of Michigan. Ann Emerg Med. 2005;46:142–7. doi: 10.1016/j.annemergmed.2004.10.010. [DOI] [PubMed] [Google Scholar]
- 3.Nowrouzi B, Huynh V. Citation analysis of workplace violence: A review of the top 50 annual and lifetime cited articles. Aggression and Violent Behavior. 2016;28:21–8. [Google Scholar]
- 4.Phillips JP. Workplace violence against health care workers in the United States. N Engl J Med. 2016;374:1661–9. doi: 10.1056/NEJMra1501998. [DOI] [PubMed] [Google Scholar]
- 5.Pompeii LA, Schoenfisch AL, Lipscomb HJ. et al. Physical assault, physical threat, and verbal abuse perpetrated against hospital workers by patients or visitors in six US hospitals. Am J Ind Med. 2015;58:1194–204. doi: 10.1002/ajim.22489. [DOI] [PubMed] [Google Scholar]
- 6.Gerberich SG, Church TR, McGovern PM. et al. An epidemiological study of the magnitude and consequences of work related violence: the Minnesota Nurses' Study. Occup Environ Med. 2004;61:495–503. doi: 10.1136/oem.2003.007294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Howard J. State and local regulatory approaches to preventing workplace violence. Occup Med. 1995;11:293–301. [PubMed] [Google Scholar]
- 8.Peek-Asa C, Howard J, Vargas L, Kraus JF. Incidence of non-fatal workplace assault injuries determined from employer's reports in California. J Occup Environ Med. 1997;39:44–50. doi: 10.1097/00043764-199701000-00009. [DOI] [PubMed] [Google Scholar]
- 9.Wassell JT. Workplace violence intervention effectiveness: A systematic literature review. Safety Science. 2009;47:1049–55. [Google Scholar]
- 10.Ahmed F, Memon MK, Memon S. Violence against doctors, a serious concern for health care organizations to ponder about. Ann Med Surg (Lond) 2018;25:3–5. doi: 10.1016/j.amsu.2017.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Joshi SC, Joshi R. Doctor becomes a patient: a qualitative study of health care work place violence related perception among junior doctors working in a teaching hospital in India. Int J Community Med Public Health. 2018;5:1775–86. [Google Scholar]
- 12.Miedema B, Tatemichi S, Hamilton R. et al. Effect of colleague and coworker abuse on family physicians in Canada. Can Fam Physician. 2011;57:1424–31. [PMC free article] [PubMed] [Google Scholar]
- 13.Privitera M, Weisman R, Cerulli C. et al. Violence toward mental health staff and safety in the work environment. Occup Med (Lond) 2005;55:480–6. doi: 10.1093/occmed/kqi110. [DOI] [PubMed] [Google Scholar]
- 14.Blando J, Ridenour M, Hartley D, Casteel C. Barriers to effective implementation of programs for the prevention of workplace violence in hospitals. Online J Issues Nurs. 2015;20 [PMC free article] [PubMed] [Google Scholar]
- 15.Camargo CA, Tsai CL, Sullivan AF. et al. Safety climate and medical errors in 62 US emergency departments. Ann Emerg Med. 2012;60:555–63 e20. doi: 10.1016/j.annemergmed.2012.02.018. [DOI] [PubMed] [Google Scholar]
- 16.Fahrenkopf AM, Sectish TC, Barger LK. et al. Rates of medication errors among depressed and burnt out residents: prospective cohort study. BMJ. 2008;336:488–91. doi: 10.1136/bmj.39469.763218.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hunter M, Carmel H. The cost of staff injuries from inpatient violence. Hosp Community Psychiatry. 1992;43:586–8. doi: 10.1176/ps.43.6.586. [DOI] [PubMed] [Google Scholar]
- 18.Zafar W, Khan UR, Siddiqui SA. et al. Workplace violence and self-reported psychological health: coping with post-traumatic stress, mental distress, and burnout among physicians working in the emergency departments compared to other specialties in Pakistan. J Emerg Med. 2016;50:167–77 e1. doi: 10.1016/j.jemermed.2015.02.049. [DOI] [PubMed] [Google Scholar]
- 19. Critical Appraisal Skills Programme (CASP) Checklist. Critical Appraisal Skills Programme (CASP) Checklist. Middle Way, Oxford, United Kingdom: CASP UK, 2016.
- 20. Higgins J, Altman D, Sterne J. Assessing risk of bias in included studies. In: Higgins J, Green S, eds. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. 2011.
- 21. Team RC. R: A language and environment for statistical computing. 2015.
- 22. Viechtbauer W. Conducting meta-analyses in R with the metafor package. J Stat Softw 2010;36.
- 23.AbuAlRub RF, Khawaldeh A, Talal A. Workplace physical violence among hospital nurses and physicians in underserved areas in Jordan. J Clin Nurs. 2014;23:1937–47. doi: 10.1111/jocn.12473. [DOI] [PubMed] [Google Scholar]
- 24.Baykan Z, Öktem İS, Çetinkaya F, Naçar M. Physician exposure to violence: a study performed in Turkey. Int J Occup Saf Ergon. 2015;21:291–7. doi: 10.1080/10803548.2015.1073008. [DOI] [PubMed] [Google Scholar]
- 25.da Silva ATC, Peres MFT, de Souza Lopes C. et al. Violence at work and depressive symptoms in primary health care teams: a cross-sectional study in Brazil. Soc Psychiatry Psychiatr Epidemiol. 2015;50:1347–55. doi: 10.1007/s00127-015-1039-9. [DOI] [PubMed] [Google Scholar]
- 26.Hahn S, Müller M, Hantikainen V. et al. Risk factors associated with patient and visitor violence in general hospitals: Results of a multiple regression analysis. Int J Nurs Stud. 2013;50:374–85. doi: 10.1016/j.ijnurstu.2012.09.018. [DOI] [PubMed] [Google Scholar]
- 27.Heponiemi T, Kouvonen A, Virtanen M. et al. The prospective effects of workplace violence on physicians' job satisfaction and turnover intentions: the buffering effect of job control. BMC Health Serv Res. 2014;14:19. doi: 10.1186/1472-6963-14-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hills D, Joyce CM. Workplace aggression in clinical medical practice: associations with job satisfaction, life satisfaction and self-rated health. Med J Aust. 2014;201:535–40. doi: 10.5694/mja13.00152. [DOI] [PubMed] [Google Scholar]
- 29.Kitaneh M, Hamdan M. Workplace violence against physicians and nurses in Palestinian public hospitals: a cross-sectional study. BMC Health Serv Res. 2012;12:469. doi: 10.1186/1472-6963-12-469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mantzouranis G, Fafliora E, Bampalis VG, Christopoulou I. Assessment and analysis of workplace violence in a Greek tertiary hospital. Arch Environ Occup Health. 2015;70:256–64. doi: 10.1080/19338244.2013.879564. [DOI] [PubMed] [Google Scholar]
- 31.Vezyridis P, Samoutis A, Mavrikiou PM. Workplace violence against clinicians in Cypriot emergency departments: a national questionnaire survey. J Clin Nurs. 2015;24:1210–22. doi: 10.1111/jocn.12660. [DOI] [PubMed] [Google Scholar]
- 32.Vorderwülbecke F, Feistle M, Mehring M. et al. Aggression and violence against primary care physicians—a nationwide questionnaire survey. Dtsch Arztebl Int. 2015;112:159. doi: 10.3238/arztebl.2015.0159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wu J-C, Tung T-H, Chen PY. et al. Determinants of workplace violence against clinical physicians in hospitals. J Occup Health. 2015;57:540–7. doi: 10.1539/joh.15-0111-OA. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–60. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ferri P, Silvestri M, Artoni C, Di Lorenzo R. Workplace violence in different settings and among various health professionals in an Italian general hospital: a cross-sectional study. Psychol Res Behav Manag. 2016;9:263. doi: 10.2147/PRBM.S114870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Saines J. Violence and aggression in A&E: recommendations for action. Accid Emerg Nurs. 1999;7:8–12. doi: 10.1016/s0965-2302(99)80094-0. [DOI] [PubMed] [Google Scholar]
- 37.Belayachi J, Berrechid K, Amlaiky F. et al. Violence toward physicians in emergency departments of Morocco: prevalence, predictive factors, and psychological impact. J Occup Med Toxicol. 2010;5:27. doi: 10.1186/1745-6673-5-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sun T, Gao L, Li F. et al. Workplace violence, psychological stress, sleep quality and subjective health in Chinese doctors: a large cross-sectional study. BMJ Open. 2017;7:e017182. doi: 10.1136/bmjopen-2017-017182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hanson GC, Perrin NA, Moss H. et al. Workplace violence against homecare workers and its relationship with workers health outcomes: a cross-sectional study. BMC Public Health. 2015;15:11. doi: 10.1186/s12889-014-1340-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mirza NM, Amjad AI, Bhatti ABH. et al. Violence and abuse faced by junior physicians in the emergency department from patients and their caretakers: a nationwide study from Pakistan. J Emerg Med. 2012;42:727–33. doi: 10.1016/j.jemermed.2011.01.029. [DOI] [PubMed] [Google Scholar]
- 41.Gong Y, Han T, Chen W. et al. Prevalence of anxiety and depressive symptoms and related risk factors among physicians in China: a cross-sectional study. PloS One. 2014;9:e103242. doi: 10.1371/journal.pone.0103242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Malinauskiene V, Einarsen S. Workplace bullying and post-traumatic stress symptoms among family physicians in Lithuania: an occupation and region specific approach. Int J Occup Med Environ Health. 2014;27:919–32. doi: 10.2478/s13382-014-0328-y. [DOI] [PubMed] [Google Scholar]
- 43.Vellani KH. The 2014 IHSSF crime survey. J Healthc Prot Manage. 2014;30:28–35. [PubMed] [Google Scholar]