Abstract
Middle East Respiratory Syndrome Coronavirus (MERS-CoV) is one of the major threats to the healthcare systems in some countries, especially in the Arabian Peninsula. MERS-CoV is considered an ideal example of the One Health concept. This is due to the animals, especially dromedary camels, play important roles in the transmission and sustainability of the virus, and the virus can be transmitted through aerosols of infected patients into the environment. However, there is some debate regarding the origin of MERS-CoV either from bats or other unknown reservoirs. The dromedary camel is the only identified animal reservoir to date. These animals play important roles in sustaining the virus in certain communities and may act as an amplifier of the virus by secreting it in their body fluids, especially in nasal and rectal discharges. MERS-CoV has been detected in the nasal and rectal secretions of infected camels, and MERS-CoV of this origin has full capacity to infect human airway epithelium in both in vitro and in vivo models. Other evidence confirms the direct transmission of MERS-CoV from camels to humans, though the role of camel meat and milk products has yet to be well studied. Human-to-human transmission is well documented through contact with an active infected patient or some silently infected persons. Furthermore, there are some significant risk factors of individuals in close contact with a positive MERS-CoV patient, including sleeping in the same patient room, removing patient waste (urine, stool, and sputum), and touching respiratory secretions from the index case. Outbreaks within family clusters have been reported, whereby some blood relative patients were infected through their wives in the same house were not infected. Some predisposing genetic factors favor MERS-CoV infection in some patients, which is worth investigating in the near future. The presence of other comorbidities may be another factor. Overall, there are many unknown/confirmed aspects of the virus/human/animal network. Here, the most recent advances in this context are discussed, and the possible reasons behind the emergence and sustainability of MERS-CoV in certain regions are presented. Identification of the exact mechanism of transmission of MERS-CoV from camels to humans and searching for new reservoir/s are of high priority. This will reduce the shedding of the virus into the environment, and thus the risk of human infection can be mitigated.
Keywords: Dromedary camel, Transmision, Zoonosis, One Health concept, MERS-CoV, Human, Reservoir
Introduction
The main reason behind developing this article is to summarize the current understanding about MERS-CoV in the context of the One Health concept. In this article, I highlight the known information about the MERS-CoV infection and its pathogenesis in humans, the patterns of MERS-CoV in dromedary camels, the potential roles of other animals in the transmission cycle of MERS-CoV, and the interaction of MERS-CoV/humans/animals. I elaborate on how some strategies can be used to stop or reduce the frequencies of MERS-CoV outbreaks based on the One Health concept, identified some gaps in the literature, and drew conclusions. The One Health concept established to ensure the good health and well beings of the human, animal and the environment. Human health is mainly affected by environment health as well as animal health (Lerner & Berg, 2015).
Survey methodology
For this review article, I conducted a literature search of the most up-to-date published articles on MERS-CoV in the past 7 years. First, I focused the introduction section on the historical background of coronaviruses and the One Health concept. Then, I highlighted the most up-to-date literature from PubMed central, Google Scholar and ResearchGate on the interaction of MERS-CoV/humans/animals. I identified some important gaps in the research dealing with MERS-CoV/human/environment in the context of the One Health concept. I also summarized the current acceptable theories on the emergence and evolution of MERS-CoV. Finally, I highlighted progress to date in the control of MERS-CoV. Historically, MERS-CoV was first identified in Saudi Arabia in a patient suffered from severe pneumonia and shortening of breath. The virus was called the novel coronavirus at that time (Zaki et al., 2012). Another retrospective study conducted in Jordan early 2012 revealed the detection of this novel coronavirus in 11 patients. Eight out of them were from the health care workers (Hijawi et al., 2013).
Coronaviruses: the Past, Present, and Future
Coronaviruses are a large group of viruses causing many health problems (respiratory, enteric, and nervous syndromes) in various species of animals and humans. Six human coronaviruses that have been identified to date (HCoV-229E, HCoV-OC43, HCoV-NL-63, HCoV-HUK-1, SARS-CoV, and MERS-CoV). Two out of them emerged in the past 15 years (Lau & Chan, 2015), namely, the severe acute respiratory syndrome coronavirus (SARS-CoV) and the Middle East Respiratory Syndrome Coronavirus (MERS-CoV). SARS-CoV emerged in 2003 in China and spread to many countries throughout the world (Peiris et al., 2003). Approximately 8,000 people were infected, and 10% of them died (Aronin & Sadigh, 2004). Only 9 years later, MERS-CoV emerged in Saudi Arabia (Zaki et al., 2012). This is a relatively short period for the emergence of a new coronavirus. One of the main reasons behind the rapid emergence of new coronaviruses is the poor proofreading capability of their RNA polymerases (Hofer, 2013). This is in addition to the possibility of the recombination of different coronaviruses (Makino et al., 1986), and it will not be surprising if new coronaviruses emerge in the near future. MERS-CoV continues to pose great challenges to the healthcare system of some countries in the Middle East and Arabian Peninsula. Since its discovery late in 2012 (Zaki et al., 2012), there are ongoing reports to the World Health Organization (WHO) from some countries in the Middle East, especially the Arabian Peninsula, with spread to other countries around the globe. According to the latest WHO statistics, there have been a total of 2,428 laboratory-confirmed cases of MERS-CoV infection including at least 838 deaths (reported case fatality rate of 35.0%) (WHO, 2018). The continuous ongoing reports on MERS-CoV suggesting the presence of some factors favor its sustainability in certain regions. There are many uncertain aspects of the virus evolution, pathogenesis, and transmission cycle. Unfortunately, recently, there was some decline in the rate of research on the virus from different aspects (Hemida et al., 2017b). This hampered the production of new data about the MERS-CoV from different aspects. Below, I summarize the current understanding of the virus in the context of the One Health concept.
Coronaviruses and the One Health Concept
The One Health concept is an interesting concept outlining the close interaction among humans, animals and the environment (Destoumieux-Garzon et al., 2018). Currently, there are two coronaviruses candidates representing the One Health concept, SARS-CoV and MERS-CoV. Animals play important roles in the transmission cycle of both viruses (Alshukairi et al., 2018; Wang et al., 2005). Both viruses were proven to be of zoonotic origin (Gao et al., 2016). The palm civet cat played important role in the transmission cycle of SARS-CoV (Wang et al., 2005). Some patients proved to visit one restaurant serving the civet cats as a meal (Wang et al., 2005). Culling of the civet cats resulted in marked decline in the reported SARS-CoV cases and now become extinct. Many studies made a direct link between the exposure to camel and its meat and milk products and MERS-CoV human cases (Reusken et al., 2014). Several studies reported the presence of MERS-CoV specific antibodies in sera of human came in close contact with camels (Reusken et al., 2014; Reusken et al., 2016). Meanwhile, MERS-CoV was isolated from air pf positive dromedary camel herds in Saudi Arabia (Azhar et al., 2014).
MERS-CoV in Humans
MERS-CoV may infect a wide group of people ranging from very young ages, even infants less than one year of age, to 109 years of age (CDC, 2016). However, children are less likely to be infected with MERS-CoV when compared to adults and, if infected, they tend to have asymptomatic or mild disease (Arwady et al., 2016). The reason for this is still not entirely clear and requires further study.
The case fatality rate is always very high in case of the immunocompromised infected patients especially those who are suffering from chronic diseases such as cancer, diabetes, blood pressure, kidney problems, etc. (Arwady et al., 2016).
Human-to-human transmission is reported in many cases. MERS-CoV replicates efficiently in various in vitro and ex vivo models (Chan et al., 2014). Moreover, many family clusters and hospital outbreaks were reported in the past 5 years (Arwady et al., 2016; Drosten et al., 2014; Memish et al., 2013). This confirms the potential spread of MERS-CoV among those who are in close contact in the population (Mollers et al., 2015). The most at-risk groups are healthcare workers including nurses, medical doctors and other hospital staff and the elderly with underlying chronic diseases (Arabi et al., 2014).
The prevalence rate of MERS-CoV in primary cases among males is relatively higher than that of females (Darling et al., 2017), which may be because exposure to infected dromedary camels is much higher in males than in females.
MERS-CoV infection triggers some unique interferons and cytokine gene expression profiles. The virus seems to be a poor interferon inducer (Chan et al., 2014). This suggests the potential immune evasion strategies triggered by the virus to hijack the host immune system and may be responsible for the high fatality rate, at least in part. Viral spreading among people seems to not yet be very efficient. Those in close contact are among the at-risk groups for infection (Drosten et al., 2014), as observed in many hospital outbreaks as well as family clusters (Alfaraj et al., 2018; Choi et al., 2017; Xiao et al., 2018). This suggests that transmission of the virus among people requires exposure to a high viral load, which will sometimes produce active infection in people who are in close contact. Several MERS-CoV family clusters have been reported (Drosten et al., 2014). Interestingly, MERS-CoV is reported in the dromedary camels in many African countries (Egypt, Nigeria, Tunisia, and Ethiopia), but no primary human cases have been reported in these countries to date (Ali et al., 2017; Roess et al., 2016; Van Doremalen et al., 2017), which may be related to some variation in the circulating Asian and African strains of MERS-CoV.
Some important deletions in the MERS-CoV currently circulating in dromedary camels from Africa were recently reported (Chu et al., 2018). These deletions may explain at least in part the reason behind the variations in the pathogenesis among the Asian and African strains of MERS-CoV. Another potential reason behind the absence of human cases in the African countries is the diverse cultural habits among people in Africa and the Arabian Peninsula (FAO, 2016). People in Arabian Peninsula get in more close touch with camels during the camel show, sports, trade than in Africa. This make the human risk of exposure much higher in the AP than Africa. MERS-CoV infection varies from severe respiratory illness accompanied by a high fever and respiratory distress to mild asymptomatic cases. Patients are usually admitted to the intensive care unit (ICU) and provided with a source of oxygen. Most cases result in pneumonia, which is fatal in almost 40% of the affected patients (Hong et al., 2017; Rubio et al., 2018). Some patients may develop renal failure [13]. Several MERS-CoV travel-associated infections were in many cases associated with the Middle East (Bayrakdar et al., 2015; Rubio et al., 2018). Among these reported was the Korean outbreak in early 2015 (Choi et al., 2017; Kim, Andrew & Jung, 2017; Xiao et al., 2018). One Korean citizen visited some countries in the Middle East and then returned home ill. This person visited several healthcare facilities in Korea. This resulted in the largest MERS-CoV human outbreak outside the Arabian Peninsula (AP) (Xiao et al., 2018). This outbreak confirmed the human-to-human transmission. During this outbreak, MERS-CoV was isolated from air samples from the hallways of the healthcare facilities close to the hospitalized patients (Xiao et al., 2018). This at least explains in part the rapid development of MERS-CoV hospital outbreaks.
MERS-CoV in Animals
Since the discovery of MERS-CoV late in 2012 (Zaki et al., 2012), many research groups have searched for its potential animal reservoir/s. Dromedary camels are the only currently proven reservoir for MERS-CoV (Hemida et al., 2014; Hemida et al., 2017b; Reusken et al., 2014; Reusken et al., 2016). Interestingly, others were able to trace the virus back 30 years ago in dromedary camel specimens in retrospective studies (Corman et al., 2014; Hemida et al., 2014; Reusken et al., 2014). All these data suggest that the virus has been circulating for decades without being recognized. Although the actual and typical clinical features of the MERS-CoV natural infection in dromedary camels is not well documented to date, very few studies reported these patterns under experimental infection approaches (Adney et al., 2014). Based on these findings, camels do not show any pathognomonic signs despite a subtle fever and mild nasal discharge for up to 6 days post-infection (dpi) (Hemida et al., 2014). Meanwhile, shedding of the infectious virus was reported in the experimentally infected camels started at 2 dpi up to the 7th dpi (Adney et al., 2014). Interestingly, viral RNA was still detected at 35 dpi (Adney et al., 2014), though it is not known whether the viral RNAs may act as potential sources of infection similar to some other positive-sense RNA viruses. No viral shedding in the oral secretions, rectal swabs, urine, or sera of these animals has been reported (Adney et al., 2014), in contrast to the detection of the virus in the fecal specimens and swabs under natural viral field infection (Hemida et al., 2014). These finding suggesting differential patterns of MERS-CoV infection between natural and experimental approaches. Further studies are required to understand the natural MERS-CoV infection in dromedary camels, which may be achieved by conducting long-term longitudinal studies as well as careful monitoring of the virus infection in large populations of camels. On necropsy examination of MERS-CoV, experimentally infected dromedary camels revealed only mild-to-moderate inflammatory reactions in the upper respiratory tract (Khalafalla et al., 2015). Detection of the viral antigens in the tissue sections of the turbinate bone and the upper respiratory tract was reported (Adney et al., 2014). Interestingly, seroconversion of the inoculated animals was reported to begin at 14 dpi (Hemida et al., 2014), indicating that MERS-CoV induces a robust humoral immune response after infection. More recently, one longitudinal study reported the possibility of MERS-CoV infection in seropositive animals. This raises concern about the role of the antibodies in the protection of the MERS-CoV infection (Hemida et al., 2017a). It seems that all the members of the family Camelidae (dromedary, alpaca, and llamas) are susceptible to MERS-CoV infection (Corman et al., 2014; Vergara-Alert et al., 2017). David et al. (2018) reported the presence of antibodies against MERS-CoV in some alpacas and llamas in Israel but only used commercial ELISA kits, and they did not address the possibility of cross-reactivity with other coronaviruses especially BCoV. It had been previously showed that there is clear cross-reactivity between MERS-CoV and BCoV in dromedary camels (David et al., 2018). Interestingly, one study showed an absence of any detectable antibodies of MERS-CoV in the sera of Bactrian camels (Chan et al., 2015), though this is the only study to report this finding concerning the seronegativity of Bactrian camels to MERS-CoV. It is not well known whether the absence of detectable MERS-CoV antibodies in the sera of Bactrians camels is due to the geographical location of the tested animals in Mongolia, far from the Middle East and Africa. This may be supported by similar findings in dromedary camels in Australia and the Canary Islands (Crameri et al., 2015). Another possibility is that this might be due to some genetic factors, which contribute to the resistance of Bactrians to MERS-CoV infections; this point is worthy of further investigation. Experimental MERS-CoV infection in both alpacas and llamas showed a similar pattern to that of dromedary camels (Crameri et al., 2016; Vergara-Alert et al., 2017), which suggested that both animals might act as a model animal for the study of MERS-CoV in vivo. However, the experimental infection of pigs with MERS-CoV did not reveal as much infection as that reported in alpacas and llamas (Vergara-Alert et al., 2017). Active MERS-CoV particles were neither retrieved from the experimentally infected animals nor from the close contact non-infected animals during the duration of this study (Vergara-Alert et al., 2017). This result suggested that pigs might not play an active role in the transmission of MERS-CoV. Although bats are considered the main reservoir for many coronaviruses, their roles in the MERS-CoV still need further clarifications. One study reported the presence of MERS-CoV in one specimen collected from bats in Saudi Arabia (Memish et al., 2013). The genome sequence of this particular virus showed almost 100% identity to a MERS-CoV index case (Memish et al., 2013). More recently, Jamaican fruit bats were found to be permissible for MERS-CoV infection (Munster et al., 2016). However, MERS-CoV-infected bats did not show any apparent clinical signs; however, viral shedding was reported in the swabs from bats up to 9 dpi. The clinical profiles and viral shedding curve during the course of the MERS-CoV infection in these bats look similar to that of dromedary camels (Munster et al., 2016), yet the amount of infectious viral shedding in bats is less compared to that in dromedary camels. This species of bat is not the most relevant for MERS-CoV infection, but this study offers some insights into the molecular pathogenesis of MERS-CoV in bats. Interestingly, another study revealed the expression of MERS-CoV receptors (dipeptidyl peptidase-4, DPP4) in the respiratory and digestive tracts of some insectivorous bats (Widagdo et al., 2017). An interesting study tested the potential roles of other species in the transmission of MERS-CoV such as cattle, sheep, goats, donkeys, buffaloes, mules, and horses from Egypt, Tunisia and Senegal (Kandeil et al., 2019). This study revealed the presence of neutralizing antibodies in the sera of some sheep and goats. Meanwhile, viral RNA was detected in swabs collected from some sheep, goats and donkeys from these countries (Kandeil et al., 2019). Several attempts were made to identify an appropriate experimental animal model for MERS-CoV. The Syrian hamster was non-permissive to MERS-CoV infection (De Wit et al., 2013). Experimental infection of this animal neither develops any clinical signs or pathology nor produces any cytokines after infection (De Wit et al., 2013). This was in contrast to New Zealand white rabbits, which showed active infection after inoculation with the MERS-CoV (Monchatre-Leroy et al., 2017). Furthermore, both rhesus macaques and common marmosets supported MERS-CoV infection (Yu et al., 2017). Additionally, both the transgenic and the transduced mice expressing the dipeptidyl peptidase 4 human receptors worked as a model for MERS-CoV studies (Zhao et al., 2015). Interestingly, a new study reported the seropositivity of some sheep and goat to MERS-CoV from Tunisia, Senegal and Egypt (Kandeil et al., 2019). Same study reported the detection of the viral RNAs in samples from cow, sheep, goat and donkeys from Egypt (Kandeil et al., 2019). This highlights the importance of continuous surveillance and searching for new reservoir/s for the MERS-CoV transmission cycle.
MERS/human/animal Interaction
It is now well accepted that human exposure to MERS-CoV-infected dromedary camels is a predisposing factor to human infection, particularly in immunocompromised people (Zumla et al., 2015). Based on the latest WHO reports, the prognosis of MERS-CoV infection is poor for elderly patients who have chronic diseases such as cancer, diabetes, kidney failure, etc. (Arabi et al., 2014). Transmission of MERS-CoV from dromedary camels to humans has been proven indirectly in some previous reports (Azhar et al., 2014). One study showed strong evidence of direct transmission of MERS-CoV from an infected camel to its owner, which was confirmed by comparing the viral genome sequencing of the virus isolated from the infected dromedary camel to that isolated from its owner. Both viruses were almost a 100% match (Azhar et al., 2014). Meanwhile, this study reported the detection of MERS-CoV nucleic acid in air samples from the indicated dromedary camel barn during the active course of the viral infection (Azhar et al., 2014).
There is a debate about the role of the dromedary camel’s milk and meat products and by-products in the transmission of MERS-CoV. Experimental introduction of MERS-CoV to raw milk revealed little difference between the virus stock in milk and that kept in DMEM (Van Doremalen et al., 2014). Due to their culture, some people in the Middle East would drink raw camel milk in efforts to seek treatment for some diseases such as diabetes. The authors acknowledge that MERS-CoV was introduced into the dromedary camel milk at a high dose and that the viral RNA was detected in a limited concentration in the camel’s milk (Van Doremalen et al., 2017). Thus, drinking the raw camel milk poses a great risk to the people consuming this milk without any heat treatment or pasteurization (van Doremalen et al. 2014; (Zhou et al., 2017). One study connected the infection of some people to the drinking of the milk from one infected camel (Memish et al., 2015). However, another study was conducted in Qatar to assess the possibility of acquiring the infection from contaminated teats and udders of infected she-camels during the process of milking (Reusken et al., 2014), though no active MERS-CoV shedding in milk has yet to be reported. Further studies are encouraged to come to a conclusion about the potential role of raw camel milk in the transmission of MERS-CoV. Nonetheless, the role of camel meat in the transmission of MERS-CoV has not been studied carefully to date. Thus, special attention should be paid to the efficient cooking of camel meat and its products as well as thorough boiling of camel milk. It is suggested that people not drink raw camel milk to avoid any risk of infection not only with MERS-CoV but also with other pathogens such as Brucellosis (Garcell et al., 2016). Some studies reported that MERS-CoV is one of the occupational zoonotic viral diseases, as was claimed based on some studies investigating the seroconversion of some at-risk group of people to MERS-CoV. This study reported the presence of specific MERS-CoV antibodies in approximately 3% of the workers in some slaughterhouses in Qatar (Farag et al., 2015). On the other hand, some studies reported the absence of any detectable antibodies in the sera of some herdsmen, veterinarians, and slaughterhouses in Saudi Arabia (Hemida et al., 2015). One possible explanation for the variations between the two studies is the difference in the sensitivity of the techniques used. Those two studies used two different techniques to report the presence/absence of the MERS-CoV antibodies in the sera of at-risk people (Farag et al., 2015; Hemida et al., 2015). Regardless, further investigation on a large-scale basis is required to solidify this conclusion about MERS-CoV.
Gaps on the MERS-CoV-related Research
There is more to be known about the molecular biology of MERS-CoV. Identification of the DPP-4 as viral receptors does not rule out the presence of other co-receptors or transcription/translation factors that favor the virus infection in a certain host. There are many immune evasion strategies triggered by MERS-CoV to hijack the host immune responses, and the mechanisms of such strategies have not been well studied. Moreover, there are many unknown aspects especially in the context of the MERS-CoV/human/animal interaction. Meanwhile, some studies were conducted on a small scale or with low numbers of animals/specimens and reported some important conclusion. These studies need further confirmation, and refinement of some of these observations is urgently needed in the near future. Here, we highlight some gaps in the research regarding the evolution and transmission of MERS-CoV. Presumably, there might be an unidentified reservoir in the transmission cycle of MERS-CoV. Although respiratory infection still is the main route of MERS-CoV infection, the exact mechanism of transmission of MERS-CoV from dromedary camels to humans is still not well understood. The possibility of another reservoir in the transmission cycle of MERS-CoV has not been ruled out. Thus, there might be a missing link in the chain of the human/camel interaction. Meanwhile, the exact modes of transmission of MERS-CoV from dromedary camels to humans have not been well clarified, and the typical pattern of the natural MERS-CoV infection in dromedary camels has not been well studied. Additionally, the potential role of most camel secretions and excretions has not been fully understood. The seroprevalence of MERS-CoV was reported in the dromedary camels from different countries in Africa and Asia (Ali et al., 2017; Hemida et al., 2014), though feral camels in Australia and the Canary islands were found to be seronegative (Crameri et al., 2015). The reason behind this phenomenon may be due to these regions being isolated lands and away from the MENA region as described above; it may also be due to the absence of an active camel movement between the Middle East and Africa and these regions of the world. Very few studies reported the cross-reactivity between MERS-CoV and other coronaviruses such as the bovine coronavirus (BCoV) that might infect dromedary camels. It is unknown if this might be the reason behind the high seroprevalence of MERS-CoV among the dromedary camel population. This may be due to the high frequency of exposure to the MERS-CoV infection during the camel’s life, the cross-reactivity of other coronaviruses, or an unknown mechanism related to the dromedary camel’s immune system. These considerations require further studies. There is ongoing demand for the development of novel diagnostic assays for coronaviruses, and special interest should be paid to those techniques that enable the simultaneous detection of the viral nucleic acids and those that can simultaneously distinguish between the antibodies for several coronaviruses. Furthermore, it is not well understood why only the Bactrian camels among the family Camelidae did not seroconvert to MERS-CoV infection (Chan et al., 2015). The genetic susceptibility of certain human populations, especially blood-related people, is not clear in the context of MERS-CoV infection. There are several levels of human exposure to dromedary camels, such as camel attendants, workers in camel abattoirs, veterinarians inspecting their carcasses, and camel owners. Those groups of people are in close contact with camels for various amounts of time and are considered to be a high-risk group of people due to the long time they spend in close contact with the dromedary camels. Meanwhile, there is an urgent need to develop a risk scoring system for human exposure to the dromedary camels.
Current Theories in the MERS-CoV/human/animals Interaction
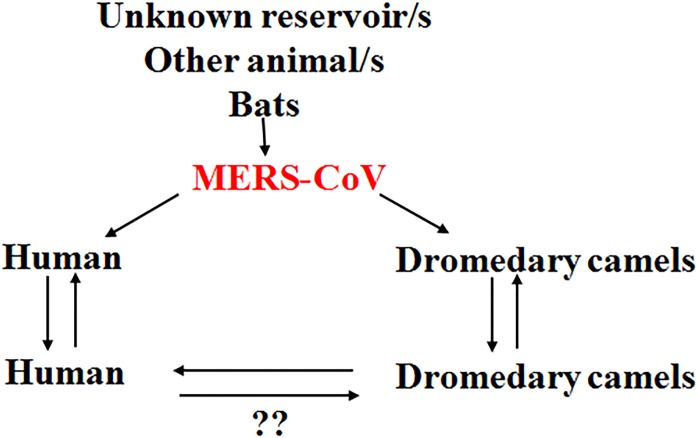
It is believed that there is some unidentified reservoirs in the context of MERS-CoV transmission presenting the virus to the community. This virus is able to infect dromedary camels, which act as an amplifier host for the virus, favoring the circulation of the virus in some camel herds. The virus has the ability to circulate among the animals in the same herd and the camel herds in close proximity to them (Fig. 1). MERS-CoV in camels has the full potential to infect the human especially immunocompromised persons. Once the virus infects a human, there is always a possibility of infecting other people, especially closely-related individuals (Fig. 1), including household relatives and workers plus healthcare workers such as doctors and nurses. Infection depends on the level of exposure to the infected person, and MERS-CoV infection in humans ranges from very severe cases of pneumonia to death. Currently available data indicate that severely infected individuals can shed the infectious virus into the environment (Kim et al., 2016), though there are few data regarding the capacity of mildly infected individuals to transmit the virus. Asymptomatic individuals, however, are unlikely to transmit the virus (Moon & Son, 2017).
Figure 1. Current theories regarding the MERS-CoV/human/animal interaction.
There might be an unknown reservoir in the transmission cycle of MERS-CoV. Bats play a role in the context of MERS-CoV transmission. The virus is transmitted to dromedary camels through an unknown mechanism. The dromedary camels act as amplifying hosts for the virus. MERS-CoV is transmitted from dromedary camels to humans through the respiratory aerosols and some other unknown mechanisms. The virus is then transmitted among the human population through respiratory routes. The human-to-human transmission has been confirmed. The human-to-camel transmission still needs further clarification. Question marks indicate the non-confirmed phenomenon.
Potential Reasons for the Emergence and the Spread of MERS-CoV
There are many factors behind the emergence, sustainability and spread of MERS-CoV. The presence of an unidentified MERS-CoV reservoir in the transmission cycle is still considered, and this unknown reservoir may contribute substantially to the suitability of the virus in certain regions. Dromedary camels remain the amplifier of the virus; the close contact of these animals to the human population in certain regions of Africa and Asia may pose a great risk for human infection and indirectly contribute to the spread of the virus. Additionally, public animal markets, especially for dromedary camels, may act as an amplifier of the virus. This poses a great risk to the surrounding community. Interesting study addressed the mapping of MERS-CoV cases in association with the environmental conditions and camel exposure (Reeves, Samy & Peterson, 2015). This study revealed that camel exposure is a key predisposing factor for some of MERS-CoV human cases (Reeves, Samy & Peterson, 2015). The lack of active surveillance programs for respiratory viruses, especially coronaviruses, may result in many subclinical or mild cases of MERS-CoV being missed in a certain population. These patients may shed the virus in their secretions and may act as a source of infection to other persons in close contact with them. Although many MERS-CoV vaccine and drug candidates are being researched, none are available yet. All these factors may favor the sustainability of MERS-CoV in certain regions.
Current Progress on the Control of MERS-CoV
Interestingly, the case fatality rate of MERS-CoV among the affected population dropped from almost 50% in 2012 to 34% early 2019 (WHO, 2018), and we may relate this progress in the control of MERS-CoV over the past 7 years to many factors. First, identification of the main reservoir of the virus, namely, the dromedary camel (Hemida et al., 2014). Second, continuous molecular and serological surveillance of MERS-CoV among the dromedary camel population in the Arabian Peninsula and Africa (Corman et al., 2014; Farag et al., 2015; Hemida et al., 2017a; Hemida et al., 2017b; Khalafalla et al., 2015; Reusken et al., 2014). Currently, testing the population of camels in regional camel markets is associated with shutting down of the market in case of positive shedding of MERS-CoV by the animals. I believe this will substantially minimize the risk of community-acquired infections through these positive populations. Third, vaccination of dromedary camels, especially animals under two years of age, will have a great impact on the reduction of the viral shedding from these animals to the surrounding community. This will also have a great positive impact on the reduction of the number of reported human infections. Fourth, there has been progress in the current understanding of viral tropism, pathogenesis, and mode of transmission in the past five years (Chan et al., 2014; Widagdo et al., 2017). Fifth, new strategies have been adopted to reduce the spread of infection in health care units (Rajakaruna et al., 2017). Sixth, some therapeutic and control approaches for MERS-CoV such as cyclosporine, ribavirin and interferon show promising trends for the treatment of MERS-CoV-infected patients (Al-Tawfiq et al., 2014; De Wilde et al., 2013). Meanwhile, good progress has been made in screening large numbers of drugs/therapies for the treatment of MERS-CoV (Han et al., 2018; He et al., 2019; Niu et al., 2018; Totura & Bavari, 2019). This may lead to the development of some effective novel drugs against MERS-CoV infection in the near future.
One Health-based Interventions to Stop MERS-CoV Outbreaks
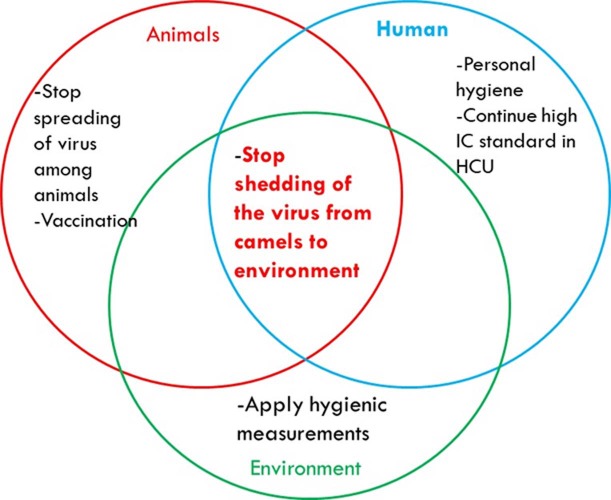
To stop MERS-CoV outbreaks, there are several strategies to be adopted in the context of the One Health concept. Some strategies are related to the animal, while others are related to human health. The main objective is to minimize or stop the viral shedding from dromedary camels to the environment (Fig. 2). This may be achieved in many ways including regular monitoring of the population of dromedary camels. Active animal shedders need to be identified, and quarantine measures should applied until they stop shedding the virus. Vaccination of young dromedary camel calves should occur during their first 6 months of life, which will minimize the chances of these animals becoming infected and actively passing the virus to older animals and then to the environment. Reorganization and reshaping of the camel industry includes allocating the camel markets away from the cities. Global awareness concerning the necessity of thorough boiling and cooking of the camel milk and meat products, respectively, should take place. Animal abattoirs should be established far away from large cities. They should not use mixed-animal platforms, and each platform should deal with one species of animal. Thorough decontamination of animals’ biological wastes in abattoirs should occur using the appropriate standard protocols. Regular surveillance of MERS-CoV among the population especially during the active peak of virus shedding by the animals should occur during November to April every year. People who are in close contact with the camels should wear proper personal protective equipment at all times.
Figure 2. Some interventions based on the One Health-based to stop MERS-CoV outbreaks.
Conclusions
At almost 7 years after its emergence, there are ongoing reports of MERS-CoV infection from time to time. This may be related to many unknown aspects of the viral evolution and pathogenesis. Some of these unknown aspects are the following. (1) Little is still known about virus/host interactions and how MERS-CoV hijacks the host immune system. (2) Potential reservoirs in the context of the MERS-CoV/human/animal network need to be identified. (3) Why do MERS-CoV-infected dromedary camels not exhibit obvious clinical signs during active viral shedding? (4) Does the presence of neutralizing antibodies in the sera of animals protect them against future active infection by the virus? (5) Does vaccination of dromedary camels have a positive impact on controlling the spread of MERS-CoV among dromedary camels? More research is urgently needed to explore the unknown aspects of the MERS-CoV/human/animal network.
Funding Statement
This work was funded by a grant from the King Abdul-Aziz City for Science and Technology (KACST), through the MERS-CoV research grant program (number 20-0004), which is part of the Targeted Research Program (TRP). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Additional Information and Declarations
Competing Interests
The author declares there are no competing interests.
Author Contributions
Maged Gomaa Hemida conceived and designed the experiments, performed the experiments, analyzed the data, contributed reagents/materials/analysis tools, prepared figures and/or tables, authored or reviewed drafts of the paper, approved the final draft.
Data Availability
The following information was supplied regarding data availability:
This is a literature review; there is no raw data.
References
- Adney et al. (2014).Adney DR, Van Doremalen N, Brown VR, Bushmaker T, Scott D, De Wit E, Bowen RA, Munster VJ. Replication and shedding of MERS-CoV in upper respiratory tract of inoculated dromedary camels. Emerging Infectious Diseases. 2014;20:1999–2005. doi: 10.3201/eid2012.141280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al-Tawfiq et al. (2014).Al-Tawfiq JA, Momattin H, Dib J, Memish ZA. Ribavirin and interferon therapy in patients infected with the Middle East respiratory syndrome coronavirus: an observational study. International Journal of Infectious Diseases. 2014;20:42–46. doi: 10.1016/j.ijid.2013.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alfaraj et al. (2018).Alfaraj SH, Al-Tawfiq JA, Altuwaijri TA, Alanazi M, Alzahrani N, Memish ZA. Middle East respiratory syndrome coronavirus transmission among health care workers: implication for infection control. American Journal of Infection Control. 2018;46:165–168. doi: 10.1016/j.ajic.2017.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ali et al. (2017).Ali MA, Shehata MM, Gomaa MR, Kandeil A, El-Shesheny R, Kayed AS, El-Taweel AN, Atea M, Hassan N, Bagato O, Moatasim Y, Mahmoud SH, Kutkat O, Maatouq AM, Osman A, McKenzie PP, Webby RJ, Kayali G. Systematic, active surveillance for Middle East respiratory syndrome coronavirus in camels in Egypt. Emerging Microbes & Infections. 2017;6:e1. doi: 10.1038/emi.2016.130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alshukairi et al. (2018).Alshukairi AN, Zheng J, Zhao J, Nehdi A, Baharoon SA, Layqah L, Bokhari A, Al Johani SM, Samman N, Boudjelal M, Ten Eyck P, Al-Mozaini MA, Zhao J, Perlman S, Alagaili AN. High prevalence of MERS-CoV infection in camel workers in Saudi Arabia. MBio. 2018;9(5):e01985-18. doi: 10.1128/mBio.01985-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arabi et al. (2014).Arabi YM, Arifi AA, Balkhy HH, Najm H, Aldawood AS, Ghabashi A, Hawa H, Alothman A, Khaldi A, Al Raiy B. Clinical course and outcomes of critically ill patients with Middle East respiratory syndrome coronavirus infection. Annals of Internal Medicine. 2014;160:389–397. doi: 10.7326/M13-2486. [DOI] [PubMed] [Google Scholar]
- Aronin & Sadigh (2004).Aronin SI, Sadigh M. Severe acute respiratory syndrome. Connecticut Medicine. 2004;68:207–215. [PubMed] [Google Scholar]
- Arwady et al. (2016).Arwady MA, Alraddadi B, Basler C, Azhar EI, Abuelzein E, Sindy AI, Sadiq BM, Althaqafi AO, Shabouni O, Banjar A, Haynes LM, Gerber SI, Feikin DR, Madani TA. Middle East respiratory syndrome coronavirus transmission in extended family, Saudi Arabia, 2014. Emerging Infectious Diseases. 2016;22:1395–1402. doi: 10.3201/eid2208.152015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Azhar et al. (2014).Azhar EI, Hashem AM, El-Kafrawy SA, Sohrab SS, Aburizaiza AS, Farraj SA, Hassan AM, Al-Saeed MS, Jamjoom GA, Madani TA. Detection of the middle east respiratory syndrome coronavirus genome in an air sample originating from a camel barn owned by an infected patient. MBio. 2014;5:e01450–e01414. doi: 10.1128/mBio.01450-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bayrakdar et al. (2015).Bayrakdar F, Altas AB, Korukluoglu G, Topal S. Molecular diagnosis and phylogenetic analysis of the first MERS case in Turkey. Mikrobiyoloji Bulteni. 2015;49:414–422. doi: 10.5578/mb.9247. [DOI] [PubMed] [Google Scholar]
- CDC (2016).Centers for Disease Control (CDC) Coronavirus — Home — CDC. (2016) gov. 2016. [26 December 2016]. https://www.cdc.gov/coronavirus/ https://www.cdc.gov/coronavirus/
- Chan et al. (2014).Chan RW, Hemida MG, Kayali G, Chu DK, Poon LL, Alnaeem A, Ali MA, Tao KP, Ng HY, Chan MC, Guan Y, Nicholls JM, Peiris JS. Tropism and replication of Middle East respiratory syndrome coronavirus from dromedary camels in the human respiratory tract: an in-vitro and ex-vivo study. The Lancet Respiratory Medicine. 2014;2:813–822. doi: 10.1016/S2213-2600(14)70158-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan et al. (2015).Chan SM, Damdinjav B, Perera RA, Chu DK, Khishgee B, Enkhbold B, Poon LL, Peiris M. Absence of MERS-coronavirus in Bactrian Camels, Southern Mongolia, 2014. Emerging Infectious Diseases. 2015;21:1269–1271. doi: 10.3201/eid2107.150178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi et al. (2017).Choi S, Jung E, Choi BY, Hur YJ, Ki M. High reproduction number of Middle East respiratory syndrome coronavirus in nosocomial outbreaks: mathematical modelling in Saudi Arabia and South Korea. Journal of Hospital Infection. 2017 doi: 10.1016/j.jhin.2017.09.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chu et al. (2018).Chu DKW, Hui KPY, Perera R, Miguel E, Niemeyer D, Zhao J, Channappanavar R, Dudas G, Oladipo JO, Traore A, Fassi-Fihri O, Ali A, Demissie GF, Muth D, Chan MCW, Nicholls JM, Meyerholz DK, Kuranga SA, Mamo G, Zhou Z, So RTY, Hemida MG, Webby RJ, Roger F, Rambaut A, Poon LLM, Perlman S, Drosten C, Chevalier V, Peiris M. MERS coronaviruses from camels in Africa exhibit region-dependent genetic diversity. Proceedings of the National Academy of Sciences of the United States of America. 2018;115(12):3144–3149. doi: 10.1073/pnas.1718769115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corman et al. (2014).Corman VM, Jores J, Meyer B, Younan M, Liljander A, Said MY, Gluecks I, Lattwein E, Bosch BJ, Drexler JF, Bornstein S, Drosten C, Muller MA. Antibodies against MERS coronavirus in dromedary camels, Kenya, 1992–2013. Emerging Infectious Diseases. 2014;20:1319–1322. doi: 10.3201/eid2008.140596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crameri et al. (2015).Crameri G, Durr PA, Barr J, Yu M, Graham K, Williams OJ, Kayali G, Smith D, Peiris M, Mackenzie JS, Wang LF. Absence of MERS-CoV antibodies in feral camels in Australia: implications for the pathogen’s origin and spread. One Health. 2015;1:76–82. doi: 10.1016/j.onehlt.2015.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crameri et al. (2016).Crameri G, Durr PA, Klein R, Foord A, Yu M, Riddell S, Haining J, Johnson D, Hemida MG, Barr J, Peiris M, Middleton D, Wang LF. Experimental infection and response to rechallenge of alpacas with middle east respiratory syndrome coronavirus. Emerging Infectious Diseases. 2016;22:1071–1074. doi: 10.3201/eid2206.160007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Darling et al. (2017).Darling ND, Poss DE, Schoelen MP, Metcalf-Kelly M, Hill SE, Harris S. Retrospective, epidemiological cluster analysis of the Middle East respiratory syndrome coronavirus (MERS-CoV) epidemic using open source data. Epidemiology and Infection. 2017;145:3106–3114. doi: 10.1017/S0950268817002345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- David et al. (2018).David D, Rotenberg D, Khinich E, Erster O, Bardenstein S, Van Straten M, Okba NMA, Raj SV, Haagmans BL, Miculitzki M, Davidson I. Middle East respiratory syndrome coronavirus specific antibodies in naturally exposed Israeli llamas, alpacas and camels. One Health. 2018;5:65–68. doi: 10.1016/j.onehlt.2018.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Wilde et al. (2013).De Wilde AH, Raj VS, Oudshoorn D, Bestebroer TM, Van Nieuwkoop S, Limpens RW, Posthuma CC, Van der Meer Y, Barcena M, Haagmans BL, Snijder EJ, Van den Hoogen BG. MERS-coronavirus replication induces severe in vitro cytopathology and is strongly inhibited by cyclosporin A or interferon-alpha treatment. Journal of General Virology. 2013;94:1749–1760. doi: 10.1099/vir.0.052910-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Wit et al. (2013).De Wit E, Prescott J, Baseler L, Bushmaker T, Thomas T, Lackemeyer MG, Martellaro C, Milne-Price S, Haddock E, Haagmans BL, Feldmann H, Munster VJ. The middle east respiratory syndrome coronavirus (MERS-CoV) does not replicate in Syrian hamsters. PLOS ONE. 2013;8:e69127. doi: 10.1371/journal.pone.0069127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Destoumieux-Garzon et al. (2018).Destoumieux-Garzon D, Mavingui P, Boetsch G, Boissier J, Darriet F, Duboz P, Fritsch C, Giraudoux P, Le Roux F, Morand S, Paillard C, Pontier D, Sueur C, Voituron Y. The One Health concept: 10 years old and a long road ahead. Frontiers in Veterinary Science. 2018;5:14. doi: 10.3389/fvets.2018.00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drosten et al. (2014).Drosten C, Meyer B, Muller MA, Corman VM, Al-Masri M, Hossain R, Madani H, Sieberg A, Bosch BJ, Lattwein E, Alhakeem RF, Assiri AM, Hajomar W, Albarrak AM, Al-Tawfiq JA, Zumla AI, Memish ZA. Transmission of MERS-coronavirus in household contacts. New England Journal of Medicine. 2014;371:828–835. doi: 10.1056/NEJMoa1405858. [DOI] [PubMed] [Google Scholar]
- Farag et al. (2015).Farag EA, Reusken CB, Haagmans BL, Mohran KA, Stalin Raj V, Pas SD, Voermans J, Smits SL, Godeke GJ, Al-Hajri MM, Alhajri FH, Al-Romaihi HE, Ghobashy H, El-Maghraby MM, El-Sayed AM, Al Thani MH, Al-Marri S, Koopmans MP. High proportion of MERS-CoV shedding dromedaries at slaughterhouse with a potential epidemiological link to human cases, Qatar 2014. Infection Ecology & Epidemiology. 2015;5:28305. doi: 10.3402/iee.v5.28305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- FAO (2016).Food and Agriculture Organization of the United Nations (FAO) Understanding MERS-CoV at the animal-human interface. Technical meeting, 21–22 2016, Rome, Italy 2016.
- Gao et al. (2016).Gao H, Yao H, Yang S, Li L. From SARS to MERS: evidence and speculation. Frontiers in Medicine. 2016;10:377–382. doi: 10.1007/s11684-016-0466-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcell et al. (2016).Garcell HG, Garcia EG, Pueyo PV, Martin IR, Arias AV, Alfonso Serrano RN. Outbreaks of brucellosis related to the consumption of unpasteurized camel milk. Journal of Infection and Public Health. 2016;9:523–527. doi: 10.1016/j.jiph.2015.12.006. [DOI] [PubMed] [Google Scholar]
- Han et al. (2018).Han HJ, Liu JW, Yu H, Yu XJ. Neutralizing monoclonal antibodies as promising therapeutics against middle east respiratory syndrome coronavirus infection. Viruses. 2018;10(12):680. doi: 10.3390/v10120680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- He et al. (2019).He L, Tai W, Li J, Chen Y, Gao Y, Li J, Sun S, Zhou Y, Du L, Zhao G. Enhanced ability of oligomeric nanobodies targeting MERS coronavirus receptor-binding domain. Viruses. 2019;11(2):166. doi: 10.3390/v11020166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hemida et al. (2015).Hemida MG, Al-Naeem A, Perera RA, Chin AW, Poon LL, Peiris M. Lack of middle East respiratory syndrome coronavirus transmission from infected camels. Emerging Infectious Diseases. 2015;21:699–701. doi: 10.3201/eid2104.141949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hemida et al. (2017a).Hemida MG, Alnaeem A, Chu DK, Perera RA, Chan SM, Almathen F, Yau E, Ng BC, Webby RJ, Poon LL, Peiris M. Longitudinal study of Middle East Respiratory Syndrome coronavirus infection in dromedary camel herds in Saudi Arabia, 2014–2015. Emerging Microbes & Infections. 2017a;6:e56. doi: 10.1038/emi.2017.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hemida et al. (2014).Hemida MG, Chu DK, Poon LL, Perera RA, Alhammadi MA, Ng HY, Siu LY, Guan Y, Alnaeem A, Peiris M. MERS coronavirus in dromedary camel herd, Saudi Arabia. Emerging Infectious Diseases. 2014;20:1231–1234. doi: 10.3201/eid2007.140571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hemida et al. (2017b).Hemida MG, Elmoslemany A, Al-Hizab F, Alnaeem A, Almathen F, Faye B, Chu DK, Perera RA, Peiris M. Dromedary camels and the Transmission of Middle East Respiratory Syndrome Coronavirus (MERS-CoV) Transboundary and Emerging Diseases. 2017b;64(2):344–353. doi: 10.1111/tbed.12401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hijawi et al. (2013).Hijawi B, Abdallat M, Sayaydeh A, Alqasrawi S, Haddadin A, Jaarour N, Alsheikh S, Alsanouri T. Novel coronavirus infections in Jordan, 2012: epidemiological findings from a retrospective investigation. Eastern Mediterranean Health Journal. 2013;19(Suppl 1):S12–S18. doi: 10.26719/2013.19.supp1.S12. [DOI] [PubMed] [Google Scholar]
- Hofer (2013).Hofer U. Viral evolution: fooling the coronavirus proofreading machinery. Nature Reviews. Microbiology. 2013;11:662–663. doi: 10.1038/nrmicro3125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hong et al. (2017).Hong KH, Choi JP, Hong SH, Lee J, Kwon JS, Kim SM, Park SY, Rhee JY, Kim BN, Choi HJ, Shin EC, Pai H, Park SH, Kim SH. Predictors of mortality in Middle East respiratory syndrome (MERS) Thorax. 2017;73(3):286–289. doi: 10.1136/thoraxjnl-2016-209313. [DOI] [PubMed] [Google Scholar]
- Kandeil et al. (2019).Kandeil A, Gomaa M, Shehata M, El-Taweel A, Kayed AE, Abiadh A, Jrijer J, Moatasim Y, Kutkat O, Bagato O, Mahmoud S, Mostafa A, El-Shesheny R, Perera RA, Ko RL, Hassan N, Elsokary B, Allal L, Saad A, Sobhy H, McKenzie PP, Webby RJ, Peiris M, Ali MA, Kayali G. Middle East respiratory syndrome coronavirus infection in non-camelid domestic mammals. Emerg Microbes Infect. 2019;8:103–108. doi: 10.1080/22221751.2018.1560235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khalafalla et al. (2015).Khalafalla AI, Lu X, Al-Mubarak AI, Dalab AH, Al-Busadah KA, Erdman DD. MERS-CoV in upper respiratory tract and lungs of dromedary camels, Saudi Arabia, 2013–2014. Emerging Infectious Diseases. 2015;21:1153–1158. doi: 10.3201/eid2107.150070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim, Andrew & Jung (2017).Kim K, Andrew SA, Jung K. Public Health Network Structure Effectiveness during the 2015 MERS outbreak in South Korea: an institutional collective action framework. International Journal of Environmental Research and Public Health. 2017;14(9):1064. doi: 10.3390/ijerph14091064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim et al. (2016).Kim SH, Chang SY, Sung M, Park JH, Bin Kim H, Lee H, Choi JP, Choi WS, Min JY. Extensive Viable Middle East Respiratory Syndrome (MERS) coronavirus contamination in air and surrounding environment in MERS isolation wards. Clinical Infectious Diseases. 2016;63:363–369. doi: 10.1093/cid/ciw239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lau & Chan (2015).Lau SK, Chan JF. Coronaviruses: emerging and re-emerging pathogens in humans and animals. Virology Journal. 2015;12:209. doi: 10.1186/s12985-015-0432-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lerner & Berg (2015).Lerner H, Berg C. The concept of health in One Health and some practical implications for research and education: what is One Health? Infection Ecology & Epidemiology. 2015;5:25300. doi: 10.3402/iee.v5.25300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Makino et al. (1986).Makino S, Keck JG, Stohlman SA, Lai MM. High-frequency RNA recombination of murine coronaviruses. Journal of Virology. 1986;57:729–737. doi: 10.1128/jvi.57.3.729-737.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Memish et al. (2015).Memish ZA, Al-Tawfiq JA, Alhakeem RF, Assiri A, Alharby KD, Almahallawi MS, Alkhallawi M. Middle East respiratory syndrome coronavirus (MERS-CoV): A cluster analysis with implications for global management of suspected cases. Travel Medicine and Infectious Disease. 2015;13:311–314. doi: 10.1016/j.tmaid.2015.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Memish et al. (2013).Memish ZA, Mishra N, Olival KJ, Fagbo SF, Kapoor V, Epstein JH, Alhakeem R, Durosinloun A, Al Asmari M, Islam A, Kapoor A, Briese T, Daszak P, Al Rabeeah AA, Lipkin WI. Middle East respiratory syndrome coronavirus in bats, Saudi Arabia. Emerging Infectious Diseases. 2013;19:1819–1823. doi: 10.3201/eid1911.131172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mollers et al. (2015).Mollers M, Jonges M, Pas SD, Van der Eijk AA, Dirksen K, Jansen C, Gelinck LB, Leyten EM, Thurkow I, Groeneveld PH, Van Gageldonk-Lafeber AB, Koopmans MP, Timen A, Netherlands ME-COITot Follow-up of contacts of middle east respiratory syndrome coronavirus-infected returning travelers, the Netherlands, 2014. Emerging Infectious Diseases. 2015;21:1667–1669. doi: 10.3201/eid2109.150560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monchatre-Leroy et al. (2017).Monchatre-Leroy E, Boue F, Boucher JM, Renault C, Moutou F, Ar Gouilh M, Umhang G. Identification of alpha and beta coronavirus in wildlife species in France: bats, rodents, rabbits, and hedgehogs. Viruses. 2017;9(12):364. doi: 10.3390/v9120364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moon & Son (2017).Moon SY, Son JS. Infectivity of an asymptomatic patient with middle east respiratory syndrome coronavirus infection. Clinical Infectious Diseases. 2017;64:1457–1458. doi: 10.1093/cid/cix170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Munster et al. (2016).Munster VJ, Adney DR, Van Doremalen N, Brown VR, Miazgowicz KL, Milne-Price S, Bushmaker T, Rosenke R, Scott D, Hawkinson A, De Wit E, Schountz T, Bowen RA. Replication and shedding of MERS-CoV in Jamaican fruit bats (Artibeus jamaicensis) Scientific Reports. 2016;6(21878) doi: 10.1038/srep21878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niu et al. (2018).Niu P, Zhao G, Deng Y, Sun S, Wang W, Zhou Y, Tan W. A novel human mAb (MERS-GD27) provides prophylactic and postexposure efficacy in MERS-CoV susceptible mice. Science China Life Sciences. 2018;61:1280–1282. doi: 10.1007/s11427-018-9343-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peiris et al. (2003).Peiris JS, Lai ST, Poon LL, Guan Y, Yam LY, Lim W, Nicholls J, Yee WK, Yan WW, Cheung MT, Cheng VC, Chan KH, Tsang DN, Yung RW, Ng TK, Yuen KY, group Ss Coronavirus as a possible cause of severe acute respiratory syndrome. Lancet. 2003;361:1319–1325. doi: 10.1016/S0140-6736(03)13077-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rajakaruna et al. (2017).Rajakaruna SJ, Liu WB, Ding YB, Cao GW. Strategy and technology to prevent hospital-acquired infections: lessons from SARS, Ebola, and MERS in Asia and West Africa. Military Medical Research. 2017;4:32. doi: 10.1186/s40779-017-0142-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reeves, Samy & Peterson (2015).Reeves T, Samy AM, Peterson AT. MERS-CoV geography and ecology in the Middle East: analyses of reported camel exposures and a preliminary risk map. BMC Research Notes. 2015;8:801. doi: 10.1186/s13104-015-1789-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reusken et al. (2014).Reusken CB, Farag EA, Jonges M, Godeke GJ, El-Sayed AM, Pas SD, Raj VS, Mohran KA, Moussa HA, Ghobashy H, Alhajri F, Ibrahim AK, Bosch BJ, Pasha SK, Al-Romaihi HE, Al-Thani M, Al-Marri SA, AlHajri MM, Haagmans BL, Koopmans MP. Middle East respiratory syndrome coronavirus (MERS-CoV) RNA and neutralising antibodies in milk collected according to local customs from dromedary camels, Qatar, 2014. Euro Surveill. 2014;19 doi: 10.2807/1560-7917.es2014.19.23.20829. [DOI] [PubMed] [Google Scholar]
- Reusken et al. (2016).Reusken CB, Schilp C, Raj VS, De Bruin E, Kohl RH, Farag EA, Haagmans BL, Al-Romaihi H, Le Grange F, Bosch BJ, Koopmans MP. MERS-CoV infection of alpaca in a region where MERS-CoV is endemic. Emerging Infectious Diseases. 2016;22:1129–1131. doi: 10.3201/eid2206.152113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roess et al. (2016).Roess A, Carruth L, Lahm S, Salman M. Camels, MERS-CoV, and other emerging infections in east Africa. The Lancet Infectious Diseases. 2016;16:14–15. doi: 10.1016/S1473-3099(15)00471-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubio et al. (2018).Rubio E, Martinez MJ, Gonzalo V, Barrachina J, Torner N, Martinez AI, Jane M, Vilella A, Del Rio A, Rodriguez-Valero N, Pinazo MJ, Munoz J, Soriano A, Trilla A, Vila J, Marcos MA. Definitive diagnosis in suspected middle east respiratory syndrome coronavirus cases. Expert Opinion on Drug Discovery. 2018;25 doi: 10.1093/jtm/tax084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Totura & Bavari (2019).Totura AL, Bavari S. Broad-spectrum coronavirus antiviral drug discovery. Expert Opin Drug Discov. 2019;14:397–412. doi: 10.1080/17460441.2019.1581171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Doremalen et al. (2014).Van Doremalen N, Bushmaker T, Karesh WB, Munster VJ. Stability of Middle East respiratory syndrome coronavirus in milk. Emerging Infectious Diseases. 2014;20:1263–1264. doi: 10.3201/eid2007.140500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Doremalen et al. (2017).Van Doremalen N, Hijazeen ZS, Holloway P, Al Omari B, McDowell C, Adney D, Talafha HA, Guitian J, Steel J, Amarin N, Tibbo M, Abu-Basha E, Al-Majali AM, Munster VJ, Richt JA. High prevalence of middle east respiratory coronavirus in young dromedary camels in Jordan. Vector-borne and Zoonotic Diseases. 2017;17:155–159. doi: 10.1089/vbz.2016.2062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vergara-Alert et al. (2017).Vergara-Alert J, Van den Brand JM, Widagdo W, Munoz MT, Raj S, Schipper D, Solanes D, Cordon I, Bensaid A, Haagmans BL, Segales J. Livestock susceptibility to infection with middle east respiratory syndrome coronavirus. Emerging Infectious Diseases. 2017;23:232–240. doi: 10.3201/eid2302.161239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang et al. (2005).Wang M, Yan M, Xu H, Liang W, Kan B, Zheng B, Chen H, Zheng H, Xu Y, Zhang E, Wang H, Ye J, Li G, Li M, Cui Z, Liu YF, Guo RT, Liu XN, Zhan LH, Zhou DH, Zhao A, Hai R, Yu D, Guan Y, Xu J. SARS-CoV infection in a restaurant from palm civet. Emerging Infectious Diseases. 2005;11:1860–1865. doi: 10.3201/eid1112.041293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Widagdo et al. (2017).Widagdo W, Begeman L, Schipper D, Run PRV, Cunningham AA, Kley N, Reusken CB, Haagmans BL, Van den Brand JMA. Tissue distribution of the MERS-coronavirus receptor in bats. Scientific Reports. 2017;7:1193. doi: 10.1038/s41598-017-01290-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO (2018).World Health Organization (WHO) Middle East Respiratory syndrome cornavirus (MERS-CoV) 2018. http://wwwwhoint/emergencies/mers-cov/en/ http://wwwwhoint/emergencies/mers-cov/en/
- Xiao et al. (2018).Xiao S, Li Y, Sung M, Wei J, Yang Z. A study of the probable transmission routes of MERS-CoV during the first hospital outbreak in the Republic of Korea. Indoor Air. 2018;28:51–63. doi: 10.1111/ina.12430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu et al. (2017).Yu P, Xu Y, Deng W, Bao L, Huang L, Xu Y, Yao Y, Qin C. Comparative pathology of rhesus macaque and common marmoset animal models with Middle East respiratory syndrome coronavirus. PLOS ONE. 2017;12:e0172093. doi: 10.1371/journal.pone.0172093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zaki et al. (2012).Zaki AM, Van Boheemen S, Bestebroer TM, Osterhaus AD, Fouchier RA. Isolation of a novel coronavirus from a man with pneumonia in Saudi Arabia. New England Journal of Medicine. 2012;367:1814–1820. doi: 10.1056/NEJMoa1211721. [DOI] [PubMed] [Google Scholar]
- Zhao et al. (2015).Zhao G, Jiang Y, Qiu H, Gao T, Zeng Y, Guo Y, Yu H, Li J, Kou Z, Du L, Tan W, Jiang S, Sun S, Zhou Y. Multi-organ damage in human dipeptidyl peptidase 4 transgenic mice infected with middle east respiratory syndrome-coronavirus. PLOS ONE. 2015;10:e0145561. doi: 10.1371/journal.pone.0145561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou et al. (2017).Zhou J, Li C, Zhao G, Chu H, Wang D, Yan HH, Poon VK, Wen L, Wong BH, Zhao X, Chiu MC, Yang D, Wang Y, Au-Yeung RKH, Chan IH, Sun S, Chan JF, To KK, Memish ZA, Corman VM, Drosten C, Hung IF, Zhou Y, Leung SY, Yuen KY. Human intestinal tract serves as an alternative infection route for Middle East respiratory syndrome coronavirus. Science Advances. 2017;3(11):eaao4966. doi: 10.1126/sciadv.aao4966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zumla et al. (2015).Zumla A, Azhar EI, Arabi Y, Alotaibi B, Rao M, McCloskey B, Petersen E, Maeurer M. Host-directed therapies for improving poor treatment outcomes associated with the middle east respiratory syndrome coronavirus infections. International Journal of Infectious Diseases. 2015;40:71–74. doi: 10.1016/j.ijid.2015.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The following information was supplied regarding data availability:
This is a literature review; there is no raw data.