INTRODUCTION:
Fecal incontinence (FI) is a common complaint and is often associated with diarrhea and urgency. Foods high in fermentable oligo-, di-, and mono-saccharides and polyols (FODMAP) cause symptoms of diarrhea and urgency. Therefore, this study assesses the impact of a low FODMAP diet on the occurrence of FI due to loose stool.
METHODS:
This study is a retrospective chart review of patients with FI seen in the Michigan Bowel Control Program clinic between August 2012 and December 2017. Patients who had FI with loose stool without red flag signs and who were recommended a low FODMAP diet and underwent formal dietary instruction with a Michigan Medicine dietician were included.
RESULTS:
Sixty-five patients with FI who underwent formal dietary teaching were included in this study. Eighty-eight percent of the patients were white, and 87% were women with a mean age of 62 years (±14 years). Additionally, the chart review showed that 35% of the patients had FI daily, 21.5% had FI weekly, and 5% had FI monthly. About 64.6% of the patients (42) had reported a reduction in their FI symptoms with the low FODMAP diet. There was no demographic or clinical characteristic that predicted the response to a low FODMAP diet.
DISCUSSION:
In this case series, dietary manipulation with a low FODMAP diet was a useful tool to treat patients who suffer from FI due to loose stool. Further confirmatory, prospective randomized controlled trials are required to see the true efficacy of a low FODMAP diet in patients who suffer with FI.
INTRODUCTION
Fecal incontinence (FI), defined as involuntary loss of solid or liquid stool, is a common complaint. A large population-based survey using the National Institutes of Health gastrointestinal (GI) patient-reported outcomes measurement information system questionnaires recently reported that 1 in 7 people suffered from FI in their lifetime and approximately 1 in 20 had an episode of FI in the last 7 days (1). This and numerous other studies have reported that diarrhea and urgency are the most potent risk factors for the development of FI (2–6). Up to two-thirds of patients associate their episodes of FI with loose or watery stool (2,3,7).
It is also well known that foods high in fermentable oligo-, di-, and mono-saccharides and polyols (FODMAP) can cause symptoms of diarrhea and urgency (8). These carbohydrates are osmotically active, inducing secretion of water in the GI lumen, and rapidly fermented by bacteria in the distal small intestine and colon, leading to an increased production of short-chain fatty acids and gas. This in turn causes luminal distension, alters the gut microbiota, and modulates stool characteristics including volume and viscosity (9,10). Foods high in FODMAP are common in the western diet. Additionally, recent studies suggest that reducing dietary FODMAP intake is associated with improved symptoms in patients with irritable bowel syndrome (IBS) and diarrhea (11–14).
Given these observations, it is reasonable to hypothesize that improving stool volume and viscosity may lead to improved clinical outcomes in patients with FI and loose stools. Therefore, this retrospective pilot study assesses the impact of a low FODMAP diet on the occurrence of FI in patients with loose stools.
METHODS
Study population
This was a retrospective chart review of patients with FI seen in the Michigan Bowel Control Program clinic between August 12, 2012, and December 31, 2017. Inclusion criteria were the following: individuals who had the diagnosis of FI associated with their encounter, had loose or watery stool documented, had no red flag signs (i.e., nocturnal diarrhea, blood in the stool, weight loss, recommended a low FODMAP diet, and underwent formal dietary instruction with a Michigan Medicine dietician). Exclusion criteria were FI associated with formed or hard stool. Institutional Review Board approval was obtained at the University of Michigan before study initiation.
Baseline subject data
Using a standardized data collection sheet, information was collected on age, gender, race/ethnicity, body mass index, tobacco use, comorbidities including inflammatory bowel disease, IBS, celiac disease, diabetes mellitus, and a history of cholecystectomy, and previous diagnostic workup including anorectal manometry (ARM) and glucose hydrogen breath test (GHBT). Specific bowel habits including baseline stool consistency based on the Bristol Stool Form Scale, occurrence of diarrhea/loose stool daily or weekly (both dichotomous and continuous variables), and occurrence of FI daily, weekly, or monthly (both dichotomous and continuous variables) were recorded.
Outcomes
The primary outcome was dichotomous (Yes/No) and assessed for a reduction in FI symptoms as determined by patient self-report by dietician or physician on follow-up after a 4-week elimination phase. A separate, semiquantitative analysis gauging response using a 0–100% scale (0% = no response, 1%–25% response, 26%–49% response, 50%–74% response, 75%–99% response, 100% or a complete response) is also routinely conducted by our GI dieticians during follow-up visits. If a semiquantitative analysis was not available (n = 13), documented note responses included “a little” (assigned 0–25% response category), “improved, normal bowel movements,” “good response” (assigned 50%–74% response category), “significant improvement” (assigned 75%–99% response category), or “no episodes of FI since following diet” (assigned 100% or complete clinical response category). Additionally, any concurrent treatment during the elimination phase such as loperamide, antibiotic treatment of small intestinal bacterial overgrowth (SIBO), or physical therapy was collected.
Statistical analysis
Statistical analysis was performed with SAS 9.4 (SAS Institute, Cary, NC). Descriptive statistics of demographic and clinical characteristics were performed. Bivariate analysis of categorical and continuous variables with χ2 test and student t test was performed to assess for predictors of clinical response to a low FODMAP diet, respectively. In a separate analysis, subjects who were treated with antibiotics for SIBO were excluded to eliminate possible confounding of our primary outcome.
RESULTS
Demographics
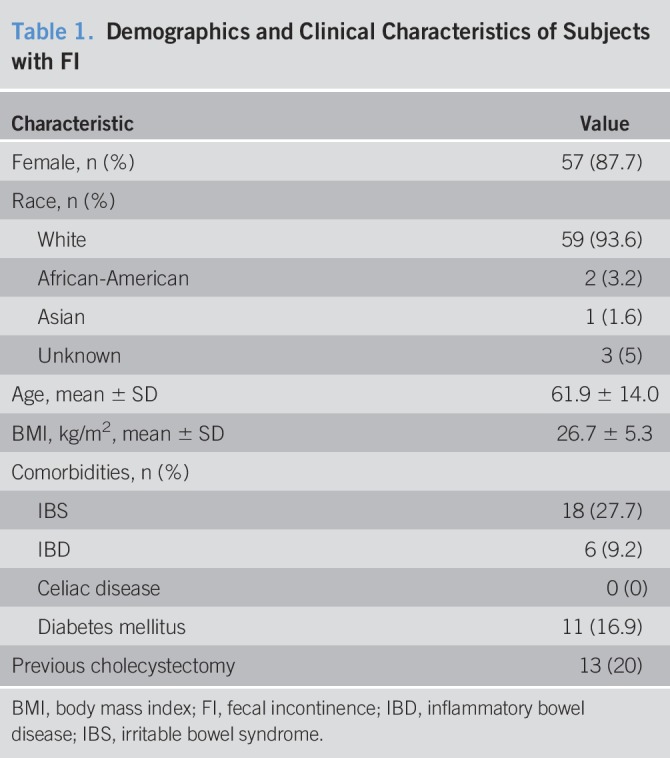
Sixty-five patients with FI who underwent formal dietary teaching were included in this study. Most were white and were female patients with a mean age of 62 years (±14 years) (Table 1). Comorbidities included diabetes mellitus (16.9%), IBS (28%), and inflammatory bowel disease (9.2%). Twenty percent of patients had a previous cholecystectomy. Thirty subjects (46.2%) had diarrhea or loose stool daily, with a mean of 6.1 loose stools daily (range: 2–20). Of the 65 patients, 23 (35.3%) had FI daily, with a mean of 2.26 FI episodes per day (range: 1–10 per day). Fourteen of the 65 patients (21.5%) had weekly episodes of FI, with a mean of 3.54 weekly FI episodes (range: 1–13 per week). Three patients reported FI monthly, with a mean of 1.5 episodes per month (range: 1–2). Bristol Stool Form Scale was reported by 27 patients, yielding a mean score of 4.6 (+1.2).
Table 1.
Demographics and Clinical Characteristics of Subjects with FI
Diagnostic testing
Ancillary testing included GHBT (35%, 23 of 65) and ARM (49%, 32 of 65). Thirteen subjects (56%) had positive GHBT. For ARM, 67% of subjects had a weak external anal sphincter and 73% had a weak internal anal sphincter. Fifty-three percent of patients had rectal hypersensitivity and 12% had rectal hyposensitivity.
Primary outcome
For our primary outcome, 42 subjects (64.6%) reported a reduction in their FI symptoms with a low FODMAP diet (Figure 1). Based on the semiquantitative analysis of the response, 88.1% had a reduction of 50% in FI episodes, 76.2% had at least a 75% reduction in symptoms, and 35.7% had a complete response, in that they had no further episodes of FI while on the diet (Figure 2). If we exclude the 11 subjects who received concurrent antibiotic treatment of SIBO, 64.8% of the subjects (35 of 54) reported a reduction in their FI symptoms with a low FODMAP diet. With reintroduction of FODMAP into their diet, the most common triggers identified were garlic and onion. There was no demographic or clinical characteristic that predicted the response to a low FODMAP diet. Manometrically, there was no level of internal anal sphincter or external anal sphincter pressure that predicted the response to a low FODMAP diet. The numbers for the other manometric parameter are too small to be able to make any statements on treatment outcomes. Additionally, no serious adverse events were observed in this study population.
Figure 1.
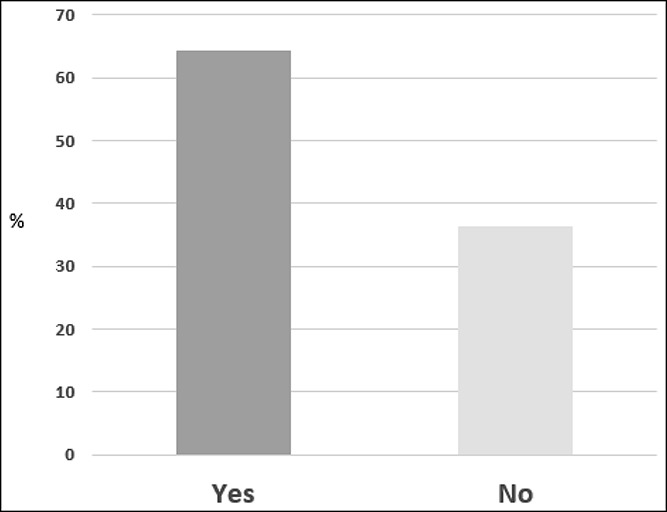
Patients reporting reduction in their fecal incontinence symptoms with a low FODMAP (fermentable oligo-, di-, and mono-saccharides and polyols) diet.
Figure 2.
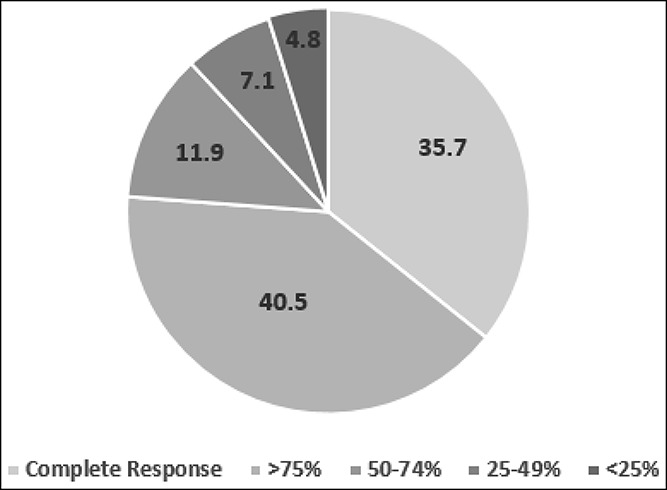
Percent reduction in fecal incontinence episodes among responders.
Concomitant treatment
Concurrent treatment included medications and pelvic floor physical therapy. Fourteen subjects (21.5%) used either loperamide (11 of 65), diphenoxylate/atropine (1 of 65), or dicyclomine (2 of 65). Twelve of the 14 subjects did not have a clinical response to the low FODMAP diet. The remaining 2 patients responded to the diet and maintained their dicyclomine dosing. For the subjects who had a positive GHBT, 11 were treated with antibiotics. Seven of these subjects had a clinical response to the low FODMAP diet. Last, 48% of the subjects (31 of 65) had pelvic floor physical therapy ordered. Most subjects (77%) had physical therapy after meeting with the dietician. However, of those who had physical therapy around the time of meeting the dietician, 1 did not try the diet, 2 had no response, but the remaining 4 had a good clinical response to the low FODMAP diet documented by the dietician. In those 4 patients, the physician noted that physical therapy helped their symptoms also.
Nonresponders
Further assessment of the “no response” group (n = 23) revealed that 15 patients failed to have either a positive or clinical response, 7 failed to follow-up after the dietician appointment, and 1 did not try the diet. Of those patients without a documented positive response, 3 had a history of postinfection IBS, 2 had resulting constipation that made them prefer a looser stool consistency, 1 had active ulcerative colitis, 1 had rectal prolapse, and 8 reported no response without any other defining comorbidities or characteristics.
Last, long-term follow-up of responders varied from a minimum of 3 months to a maximum of 5.4 years, with a mean of 2.0 years. Thirty-five of 42 patients reported continued control of their FI symptoms. Seven people did not have the following notations: “Had forgotten the diet,” “Lost their handouts,” or “Diet was too restrictive.”
DISCUSSION
In this exploratory and retrospective case series, dietary manipulation with a low FODMAP diet was a useful tool to treat patients who suffer from FI and loose stool. Almost two-thirds reported that the low FODMAP diet improved their FI. Of the patients who reported improvement with the low FODMAP diet, over a third had a complete clinical response, with no further episodes of FI.
In patients who have FI and loose stool, careful attention to the timing of the episodes of loose stool and FI is important. If bowel movements and episodes are nocturnal, other causes than an osmotic diarrhea should be sought. However, if episodes occur predominantly during the day, and in particular, if symptoms are meal related, taking a systematic approach to dietary manipulation can be useful in reducing FI symptoms as demonstrated by our case series. Previous efforts at dietary manipulation in patients with FI have focused on increasing the fiber intake. Joh et al. (15) demonstrated a 2.66 higher likelihood of FI in elderly women who consumed the lowest amount of weekly dietary fiber. Last, 2 randomized controlled trials found a decrease in incontinent stools with psyllium powder (16,17).
Early work performed by the Monash group demonstrated the utility of a diet low in fermentable carbohydrates in patients with IBS (18,19). This has also been replicated within a US population by our group demonstrating the efficacy of a low FODMAP diet in subjects with IBS-diarrhea (11). Fermentable carbohydrates can be powerful osmotic agents, and dietary trends within the United States show an increasing consumption of FODMAP-rich food (20). Therefore, a low FODMAP diet might offer clinical benefits to patients with FI where up to two-thirds of patients experience loose, frequent stools and urgency. This was what led us to offer a low FODMAP diet to patients with FI and loose stool in clinical practice. It is important to emphasize that a low FODMAP diet consists of 3 phases: Elimination, Reintroduction of foods containing individual FODMAP to determine a patient's sensitivities, and Personalization of the diet based on the information obtained during the Reintroduction phase. Due to the complexity of this diet plan, it is important for the patient to be under the care of a dietician who has been adequately trained in administering the 3 phases of the diet plan.
Patients did undergo reintroduction of FODMAP to help identify possible triggers of loose stools and FI episodes. The reintroduction stage is critical and should be done under the guidance of a seasoned dietician. The most common triggers that were noted by our dieticians were garlic and onion. Both these are common cooking ingredients that patients often overlook as possible triggers for their symptoms.
Our study does have a number of limitations. Most importantly, this is an uncontrolled, retrospective chart review in a limited number of patients from a tertiary care center. Our case series is subject to the vagaries of obtaining data from patient charts. We are fortunate that all included patients were evaluated and instructed by one of 2 highly experienced GI dieticians who have standardized the way in which they collect baseline and follow-up clinical data. Our specialized GI dieticians likely increase the quality of data collected and instruction provided but along with other factors already mentioned may limit the generalizability of our results to routine clinical practice. The lack of blinding of patients to the intervention also increases the likelihood of a placebo effect. Last, it is important to acknowledge the potential confounding effects of concomitant therapies that occurred with the low FODMAP diet. However, this study is important as it is a hypothesis-generating report and there is little way to address these confounders.
In the first case series of a low FODMAP diet in patients with FI and loose stool, a low FODMAP diet improved FI in almost two-thirds of patients. These results require confirmation in a prospective randomized controlled trial. Currently, we are nearing completion of a confirmatory, prospective randomized controlled trial to confirm the efficacy of a low FODMAP diet in patients who suffer with FI and loose stools.
CONFLICTS OF INTEREST
Guarantor of the article: Stacy B. Menees, MD, MS.
Specific author contributions: S.B.M.: study concept and design, analysis and interpretation of data, drafting of the manuscript, and draft revision. D.C. and E.L.L.: data acquisition and draft revision. W.D.C.: analysis and interpretation of data and critical revision of the manuscript for important intellectual content.
Financial support: None.
Potential competing interests: W.D.C. is a consultant for Allergan, Biomerica, IM Health, Ironwood, Outpost, QOL Medical, Salix, Shire, and Urovant, and received research grants from Biomerica, Commonwealth Diagnostics, Nestle, QOL Medical, and Zespri. W.D.C. is also patent holders and principals at My Total Health. S.B.M. is a consultant for Synergy Pharmaceuticals. D.C. and E.L.L. do not have any relevant disclosures.
Study Highlights.
WHAT IS KNOWN
✓ FI is a common disorder associated with loose stool.
✓ Diets high in fermentable carbohydrates can cause loose stools.
WHAT IS NEW HERE
✓ Almost two-thirds of patients with FI and loose stool reported a response to a low FODMAP diet.
✓ Over a third of patients who responded to a low FODMAP diet had a complete response.
✓ No serious adverse events were noted in this study population.
TRANSLATIONAL IMPACT
✓ Our study provides preliminary evidence for the use of dietary-based therapy in patient with FI and loose stool.
REFERENCES
- 1.Menees SB, Almario CV, Spiegel BMR, et al. Prevalence of and factors associated with fecal incontinence: Results from a population-based survey. Gastroenterology 2018;154:1672–81.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Whitehead WE, Borrud L, Goode PS, et al. Fecal incontinence in US adults: Epidemiology and risk factors. Gastroenterology 2009;137:512–7, 517.e1–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bharucha AE, Seide BM, Zinsmeister AR, et al. Relation of bowel habits to fecal incontinence in women. Am J Gastroenterol 2008;103:1470–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bharucha AE, Zinsmeister AR, Locke GR, et al. Risk factors for fecal incontinence: A population-based study in women. Am J Gastroenterol 2006;101:1305–12. [DOI] [PubMed] [Google Scholar]
- 5.Bharucha AE, Zinsmeister AR, Schleck CD, et al. Bowel disturbances are the most important risk factors for late onset fecal incontinence: A population-based case-control study in women. Gastroenterology 2010;139:1559–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rey E, Choung RS, Schleck CD, et al. Onset and risk factors for fecal incontinence in a US community. Am J Gastroenterol 2010;105:412–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Smith TM, Menees SB, Xu X, et al. Factors associated with quality of life among women with fecal incontinence. Int Urogynecol J 2013;24:493–9. [DOI] [PubMed] [Google Scholar]
- 8.Dolan R, Chey WD, Eswaran S. The role of diet in the management of irritable bowel syndrome: A focus on FODMAPs. Expert Rev Gastroenterol Hepatol 2018;12:607–15. [DOI] [PubMed] [Google Scholar]
- 9.Berghouse L, Hori S, Hill M, et al. Comparison between the bacterial and oligosaccharide content of ileostomy effluent in subjects taking diets rich in refined or unrefined carbohydrate. Gut 1984;25:1071–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Barrett JS, Gearry RB, Muir JG, et al. Dietary poorly absorbed, short-chain carbohydrates increase delivery of water and fermentable substrates to the proximal colon. Aliment Pharmacol Ther 2010;31:874–82. [DOI] [PubMed] [Google Scholar]
- 11.Eswaran SL, Chey WD, Han-Markey T, et al. A randomized controlled trial comparing the low FODMAP diet vs. Modified NICE guidelines in US adults with IBS-D. Am J Gastroenterol 2016;111:1824–32. [DOI] [PubMed] [Google Scholar]
- 12.Staudacher HM, Lomer MCE, Farquharson FM, et al. A diet low in FODMAPs reduces symptoms in patients with irritable bowel syndrome and a probiotic restores bifidobacterium species: A randomized controlled trial. Gastroenterology 2017;153:936–47. [DOI] [PubMed] [Google Scholar]
- 13.Bohn L, Storsrud S, Liljebo T, et al. Diet low in FODMAPs reduces symptoms of irritable bowel syndrome as well as traditional dietary advice: A randomized controlled trial. Gastroenterology 2015;149:1399–407 e2. [DOI] [PubMed] [Google Scholar]
- 14.Halmos EP, Power VA, Shepherd SJ, et al. A diet low in FODMAPs reduces symptoms of irritable bowel syndrome. Gastroenterology 2014;146:67–75 e5. [DOI] [PubMed] [Google Scholar]
- 15.Joh HK, Seong MK, Oh SW. Fecal incontinence in elderly Koreans. J Am Geriatr Soc 2010;58:116–21. [DOI] [PubMed] [Google Scholar]
- 16.Bliss DZ, Jung HJ, Savik K, et al. Supplementation with dietary fiber improves fecal incontinence. Nurs Res 2001;50:203–13. [DOI] [PubMed] [Google Scholar]
- 17.Markland AD, Burgio KL, Whitehead WE, et al. Loperamide versus psyllium fiber for treatment of fecal incontinence: The fecal incontinence prescription (Rx) management (FIRM) randomized clinical trial. Dis Colon Rectum 2015;58:983–93. [DOI] [PubMed] [Google Scholar]
- 18.Shepherd SJ, Gibson PR. Fructose malabsorption and symptoms of irritable bowel syndrome: Guidelines for effective dietary management. J Am Diet Assoc 2006;106:1631–9. [DOI] [PubMed] [Google Scholar]
- 19.Shepherd SJ, Parker FC, Muir JG, et al. Dietary triggers of abdominal symptoms in patients with irritable bowel syndrome: Randomized placebo-controlled evidence. Clin Gastroenterol Hepatol 2008;6:765–71. [DOI] [PubMed] [Google Scholar]
- 20.Bray GA, Nielsen SJ, Popkin BM. Consumption of high-fructose corn syrup in beverages may play a role in the epidemic of obesity. Am J Clin Nutr 2004;79:537–43. [DOI] [PubMed] [Google Scholar]


