Supplemental Digital Content is available in the text
Keywords: Parkinson disease, Multiple system atrophy, Autonomic dysfunction, Cardiovascular autonomic indexes
Abstract
Background:
Differential diagnosis of idiopathic Parkinson disease (IPD) and multiple system atrophy-Parkinson type (MSA-P) is challenging since they share clinical features with parkinsonism and autonomic dysfunction. To distinguish MSA-P from IPD when the symptoms are relatively mild, we investigated the usefulness of the quantitative fractionalized autonomic indexes and evaluated the correlations of autonomic test indexes and functional status.
Methods:
Thirty-six patients with parkinsonism (22 with IPD and 14 with MSA-P) in Soonchunhyang University Bucheon Hospital from February 2014 to June 2015 were prospectively enrolled in the study. We compared fractionalized autonomic indexes and composite autonomic scoring scale between patients with IPD and MSA-P with Hoehn and Yahr (H&Y) score ≤3. Parasympathetic indexes included expiratory/inspiratory ratio during deep breathing, Valsalva ratio (VR), and regression slope of systolic blood pressure (BP) in early phase II (vagal baroreflex sensitivity) during Valsalva maneuver. Sympathetic adrenergic indexes were pressure recovery time (PRT) and adrenergic baroreflex sensitivity (BRSa) (BP decrement associated with phase 3 divided by the PRT), sympathetic index 1, sympathetic index 3, early phase II mean BP drop, and pulse pressure reduction rate. Additionally, we compared the unified multiple system atrophy rating scale (UMSARS) and H&Y scores and the autonomic indexes in all patients.
Results:
PRT was significantly different between the IPD and MSA-P groups (P = 0.004) despite the similar BP drop during tilt. Cut-off value of PRT was 5.5 s (sensitivity, 71.4%; specificity, 72.7%). VR (r = −0.455, P = 0.009) and BRSa (r = −0.356, P = 0.036) demonstrated a significant correlation with UMSARS and H&Y scores.
Conclusions:
Among the cardiovascular autonomic indexes, PRT can be a useful parameter in differentiating the early stage of MSA-P from that of IPD. Moreover, VR, and BRSa may be the optimal indexes in determining functional symptom severity.
Introduction
Idiopathic Parkinson disease (IPD) and multiple system atrophy-Parkinson type (MSA-P) share clinical features with parkinsonism and autonomic dysfunction. Multiple system atrophy (MSA) mainly involves the preganglionic pathway of the autonomic nervous system, and autonomic dysfunction appears to develop early and is noticeable.[1,2] In contrast, IPD mainly damages the postganglionic pathway of the autonomic nervous system, and autonomic dysfunction is not prominent at an early stage.[2,3] Thus, the early and prominent manifestation of autonomic failure is the main characteristic to differentiate MSA from IPD.[4,5] Since the differentiation between patients with IPD and MSA-P is important in predicting the response to therapy and prognosis of the disease, there have been several studies that determined the difference in autonomic functions in both diseases.[4–6] However, the results were inconsistent and failed to demonstrate the selectivity of the clinical and laboratory parameters in autonomic function.[6,7] Therefore, an effective tool for differentiation has not yet been identified, and the differential diagnosis of IPD and MSA-P remains challenging.[3,6,8] With the advent of the equipment for noninvasive and quantitative autonomic function test (AFT), there has been an effort to improve the diagnostic accuracy using more fractionalized autonomic indexes.[4,5,7] Several autonomic test indexes have been validated to represent the degree of autonomic dysfunction and the selective damage of sympathetic or parasympathetic dysfunction. Ewing battery[9] and composite autonomic scoring scale (CASS)[10] are widely used as standard tests for autonomic function. In patients with autonomic failure, quantitative autonomic test indexes, such as sympathetic indexes (SIs) including pressure recovery time (PRT) during the Valsalva maneuver (VM), are valuable indicators of sympathetic dysfunction.[11,12] Vagal baroreflex sensitivity (BRSv) and adrenergic baroreflex sensitivity (BRSa) calculated during VM reflect the degree of baroreflex sensitivity.[13] We aimed to determine the usefulness of these quantitative autonomic test indexes with CASS to distinguish MSA-P from IPD. To evaluate the usefulness of quantitative autonomic test, we aimed to assess the correlations between fractionalized autonomic indexes and unified Parkinson disease rating scale (UPDRS), unified multiple system atrophy rating scale (UMSARS), and Hoehn and Yahr (H&Y) scale, which are commonly used to predict disease severity and progression.
Methods
Ethical approval
All experiments followed the tenets of the Declaration of Helsinki, and this study was approved by the Institutional Review Board of Soonchunhyang University Bucheon Hospital. Written informed consent was obtained from each participant/guardian prior to their enrollment in this study.
Patients
We prospectively recruited 36 patients who presented with parkinsonism in Soonchunhyang University Bucheon Hospital from February 2014 to June 2015. A total of 22 patients were diagnosed with definite IPD according to the diagnosis criteria of the United Kingdom Parkinson's Disease Society Brain Bank.[14] A total of 14 patients had probable MSA-P, which is a sporadic, progressive adult-onset disorder including rigorously defined autonomic failure and poorly levodopa-responsive parkinsonism according to Gilman diagnosis criteria.[15] We performed brain magnetic resonance imaging for all patients and [18F]N-(3-fluoropropyl)-2β-carbon ethoxy-3β-(4-iodophenyl) nortropane (FP-CIT) positron emission tomography (PET) for 86% of patients (22 patients with IPD and nine patients with MSA-P). To clearly distinguish the two diseases, we performed [18F]fluorodeoxyglucose (FDG) PET or metaiodobenzylguanidine (MIBG) scintigraphy selectively when abnormal autonomic symptoms were observed. We performed [18F]FDG PET selectively in 18 patients (50%) who showed decreased metabolism in the basal ganglia (seven patients with MSA-P) and normal or mild increased metabolism in the same area (11 patients with IPD) [Figure 1]. Two patients with IPD showed abnormal MIBG test results, and two patients with MSA-P showed normal MIBG test results. We excluded patients with parkinsonism due to drugs or other causes, history of stroke, and structural brain disease or injury. Additional exclusion criteria were: (1) inability to effectively perform VM such as those in dementia, chronic obstructive pulmonary disease, or heart failure; (2) diabetes; and (3) cardiac arrhythmias. As a result, our study included only patients within H&Y score of 3 who were able to perform VM.
Figure 1.
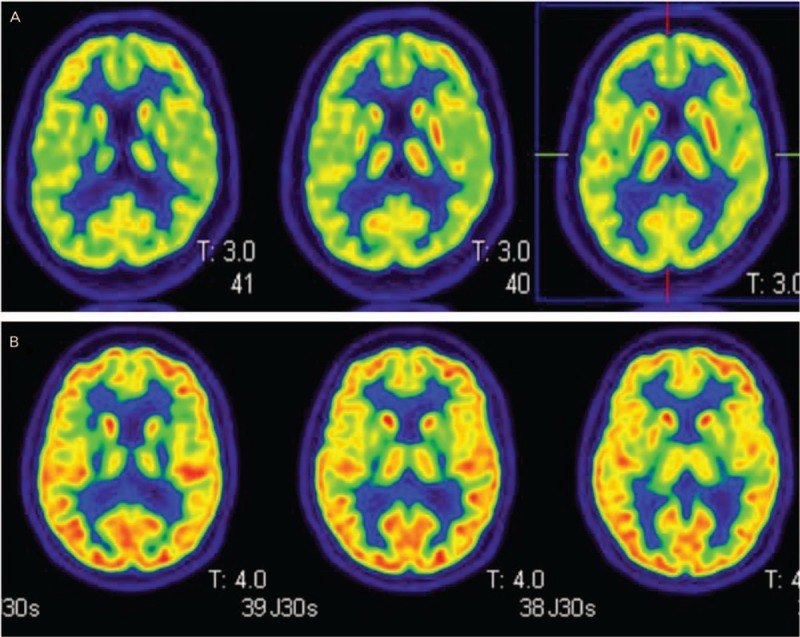
Representative images of [18F]FDG PET results in patients with idiopathic Parkinson disease or multiple system atrophy-Parkinson type. (A) Representative images of [18F]FDG PET results in a patient with idiopathic Parkinson disease. (B) Representative images of [18F]FDG PET results in a patient with multiple system atrophy-Parkinson type. [18F]FDG PET: [18F]fluorodeoxyglucose positron emission tomography.
Autonomic function tests
Exercise was avoided 24 h before the test. Fasting was done after midnight for the AFT in the morning and after early in the morning for the test in the afternoon. Coffee and cigarettes were prohibited 6 h before the test. Patients stopped medications at least 48 h before the test including anticholinergics and antihistamines that could interfere with autonomic function. Anti-Parkinson medications were administered alone or in combination: levodopa, amantadine, and anticholinergics. All patients did not take anti-Parkinson medication on the day the AFT was performed.
All patients underwent heart rate response to deep breathing (HRDB) test, VM test, and head-up tilt test (HUTT) using the Finometer®Pro (FMS, Amsterdam, the Netherlands) and quantitative sudomotor axon reflex test (QSART using the Quantitative Sweat Measurement System, WR Medical Electronics Co., MN, USA).
-
(1)
Heart rate response to deep breathing test
Expiratory-inspiratory (E:I) ratio: E:I ratio is the ratio of the longest RR interval during expiration and the shortest RR interval during inspiration from six cycles.
-
(2)
Valsalva maneuver test
-
(a)
Valsalva ratio (VR): VR was derived from the longest RR interval in phase IV divided by the shortest RR interval in phase II.
-
(b)
Regression slope of systolic blood pressure (SBP) in early phase II during VM (BRSv): BRSv was measured by a regression slope in which SBP was reduced per millisecond in early phase II.
-
(c)
PRT: PRT was defined as the recovery time from the bottom of phase III to baseline SBP.
-
(d)
BP decrement associated with phase 3 divided by the PRT (BRSa): BRSa was calculated by dividing the degree to which SBP dropped in phase III divided by PRT.
-
(e)
SI1: SI1 was defined as the degree of SBP fall during early phase II.
-
(f)
SI3: SI3 was defined as the difference in SBP between baseline and the end of phase II.
-
(g)
Early phase II mean BP drop: It was defined as the degree of degradation of mean BP at early phase II.
-
(h)
Pulse pressure reduction rate (PPR, %): Pulse pressure (PP) is the difference between SBP and diastolic BP. PPR was calculated by the ratio of the reduced PP before VM and smallest PP during VM.
-
(a)
-
(3)
Head-up tilt test
Orthostatic hypotension (OH): OH was defined as the sustained reduction in SBP of at least 30 mmHg or diastolic BP of 15 mmHg in the HUTT.
-
(4)
Quantitative sudomotor axon reflex test
The latency and amount of perspiration were measured after injection of 10% acetylcholine and stimulation for 5 min at 2 mA and compared them against age-sex-specific corrected values.
Three parasympathetic indexes were included: E:I ratio, VR, and BRSv. The seven SIs were PRT, SI1, SI3, BRSa, early phase II mean BP drop, PPR, and QSART [Supplementary Figure 1]. We also used the CASS consisting of cardiovagal (3 points), adrenergic (4 points), and sudomotor (3 points) subscales.
Functional status scales in idiopathic Parkinson disease and multiple system atrophy-Parkinson type
We obtained the total UPDRS, Part I (non-motor symptom), Part III (motor symptom), UMSARS, and H&Y scores to determine the clinical progression of patients with IPD and MSA-P. To demonstrate the correlation of disease severity and autonomic abnormality, we compared the UPDRS, UMSARS, and H&Y scores and the abnormalities in these autonomic indexes.
Statistical analysis
Demographic and clinical data were compared between groups using Student t test or the Mann-Whitney U test for continuous variables and Pearson χ2 test for categorical variables. To determine the relationship between autonomic indexes and functional status scales or subjective autonomic symptoms score, we performed Pearson correlation analysis. Statistical analyses were performed with a commercially available software package, IBM SPSS Statistics version 24.0 (IBM Corporation, Armonk, NY, USA). A P value <0.05 was considered statistically significant.
Results
Patients
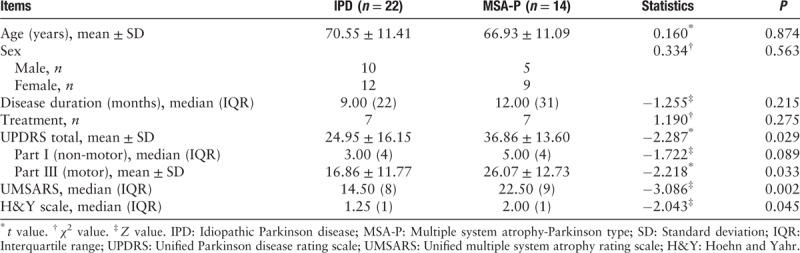
We recruited 22 patients with IPD and 14 patients with probable MSA-P. Demographic and clinical details of the enrolled subjects are presented in Table 1. There was no significant difference in sex, age, and disease duration between the two groups. Only patients within the H&Y 3 were included consequently because patients who were unable to perform the VM were excluded. In addition, it is clinically meaningful to distinguish to two groups before symptoms are severe or in the early phase. Although there was no difference in the disease duration between two groups, H&Y in the MSA-P were slightly higher than in the IPD (P = 0.045) because of early functional impairment in the MSA-P. Likewise, the degrees of functional deficit (UPDRS, UMSARS) in the MSA-P were higher than in the IPD.
Table 1.
Demographic characteristics of patients with idiopathic Parkinson disease and multiple system atrophy-Parkinson type.
Autonomic function tests
We recruited 22 patients with IPD and 14 patients with probable MSA-P. Demographic and clinical data of the enrolled subjects are presented in Table 1. There was no significant difference in sex, age, and disease duration between the two groups. Only patients within the H&Y stage 3 were included, and patients who were unable to perform VM were excluded. Moreover, it is clinically meaningful to distinguish the two groups before symptoms are severe or in the early phase. Although there was no difference in the disease duration between the two groups, H&Y scores in the MSA-P group were slightly higher than those in the IPD group (P = 0.045) because of early functional impairment in MSA-P. Likewise, the degrees of functional deficit (UPDRS, UMSARS) in the MSA-P group were higher than those in the IPD group.
Three parasympathetic indexes and seven SIs were compared between patients with IPD and MSA-P [Table 2]. There was no significant difference in BRSa, E:I ratio, VR, BRSv, SI1, SI3, early mean BP drop, and PPR between the two groups. PRT (P = 0.004) was significantly different between the IPD and MSA-P groups. Area under the receiver operating characteristic curve was 0.713 (95% CI, 0.615–0.910) [Figure 2]. Cut-off value of PRT was 5.5 s (sensitivity, 71.4%; specificity, 72.7%).
Table 2.
Comparisons of parasympathetic and sympathetic indexes between idiopathic Parkinson disease and multiple system atrophy-Parkinson type.
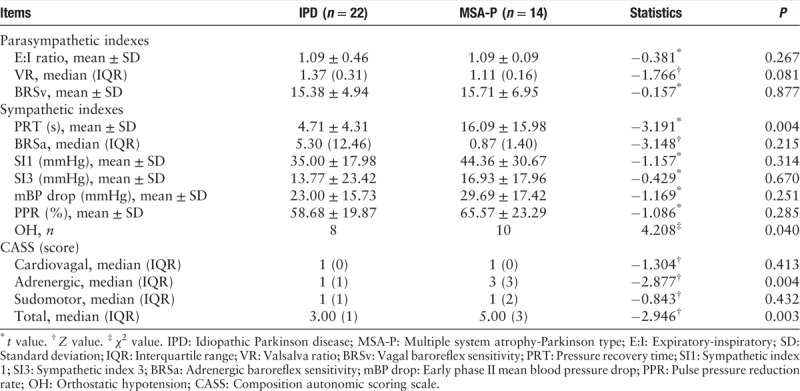
Figure 2.
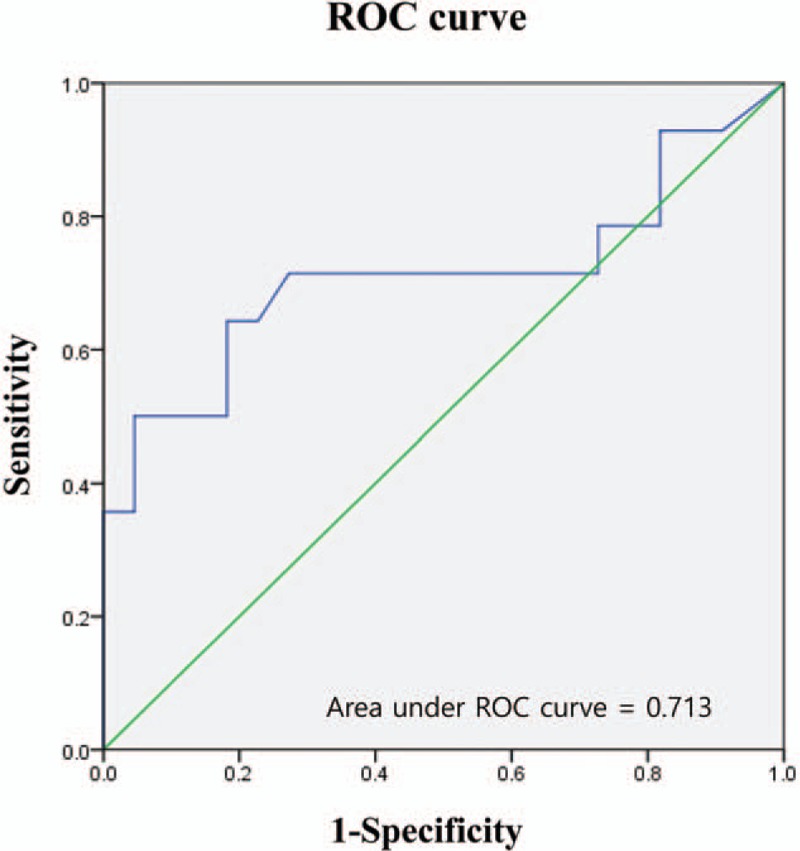
Receiver-operating characteristic curve of pressure recovery time as a predictor of multiple system atrophy-Parkinson type in patients with autonomic dysfunction and parkinsonism. Cut-off value is 5.5 s (sensitivity, 71.4%; specificity, 72.7%). Area under the ROC curve is 0.713 (95% CI, 0.615–0.910). ROC: Receiver-operating characteristic; CI: Confidence interval.
OH in HUTT was significantly frequent in the MSA-P group (71.4%) than the IPD group (36.4%). Total (P = 0.003) and adrenergic CASS scores (P = 0.004) were significantly different between the IPD and MSA-P groups. There was no significant difference between cardiovagal and sudomotor score in CASS. This means that the autonomic adrenergic dysfunction in MSA-P was more severe than that in IPD.
Correlation between clinical disease progression and autonomic function indexes
We compared the correlations of UPDRS, UMSARS, and H&Y scales with each autonomic test index. BRSa (r = −0.356, P = 0.036) and VR (r = −0.455, P = 0.009) significantly decreased in patients with high UMSARS scores [Supplementary Figure 2]. This correlation was also observed in H&Y scores (BRSa, r = −0.364, P = 0.041; VR, r = −0.357, P = 0.035). However, the UPDRS scores were not correlated with autonomic function indexes. These results revealed that BRSa and VR demonstrated a significant correlation with clinical disease severity as shown in UMSARS and H&Y scores.
Discussion
The prevalence of autonomic dysfunction in patients with IPD varies from 14% to 80%.[16–18] Furthermore, severe autonomic abnormalities may develop even in the untreated early stages of IPD.[19] Therefore, it is difficult to distinguish IPD and MSA-P only with subjective autonomic symptoms at the early stage of the disease. Previous reports showed AFTs help to distinguish MSA from IPD with or without autonomic dysfunction.[2,4,5,20] However, some studies failed to demonstrate consistent results regarding differentiation in MSA from that in IPD using those AFTs.[6,8,21] A previous study proposed that cardiovagal baroreflex sensitivity from phase IV of VM can potentially differentiate IPD and MSA.[22,23] Presently, additional quantitative autonomic functional indicators using Finometer®Pro can be obtained by continuous recording of BP and heart rate. Therefore, we attempted to identify the specific quantitative autonomic indexes that can help differentiate IPD and MSA-P with relatively mild symptoms (H&Y score ≤3). Patients with MSA-P showed significantly increased PRT than patients with IPD in an early stage. This indicated that sympathetic dysfunction in MSA-P is more predominant than that in IPD in the early stage. Moreover, prolonged PRT (>5.5 s) is potentially useful in differentiating MSA-P from IPD. According to consensus guidelines, OH is defined as a sustained fall in SBP by at least 20 mmHg or diastolic BP by 10 mmHg within 3 min of standing or head-up tilt.[24] However, reduction in SBP of 30 mmHg in a patient with supine hypertension may be a more appropriate criterion for OH.[25] Therefore, we defined OH as a reduction in SBP of at least 30 mmHg or diastolic BP of 15 mmHg in the HUTT. In our study, OH was present in 71.4% of patients with MSA-P and significantly more common in MSA-P than IPD. However, because OH was observed even in 36.4% of patients with IPD, the presence of OH could not independently distinguish the two groups. Although urinary difficulties and OH are reckoned to be the important symptoms in the early phase of MSA, orthostatic intolerance may not be noted in patients with MSA within 1 year of onset.[26] We also assessed the relationship of UPDRS, UMSARS, and H&Y scores with each autonomic test index. The VR in the parasympathetic index and BRSa in SI revealed a significant correlation with the progression of the diseases. Therefore, these indexes may be the optimal parameters revealing the symptom severity in patients with parkinsonism and autonomic dysfunction. Without a histologic diagnosis, clinical grouping of IPD and MSA-P can be ambiguous in this study, but we adopted the widely used reliable diagnostic criteria and proper neuroimaging study including [18F]FP-CIT PET, [18F]FDG PET, and cardiac MIBG scintigraphy if needed for diagnostic accuracy. Our study has some limitations. First, we did not obtain a pathologic confirmation and could not follow-up AFTs. Although we attempted to clarify the diagnosis by performing [18F]FDG PET or MIBG scintigraphy selectively, we did not perform these tests in all patients. Second, our study does not rule out the effects of anti-Parkinson medication on AFT. Although the influence of anti-Parkinson medication on AFT has been reported,[27] our patients did not use the medication only on the day of the test to reduce tremor-induced recording artifact and well perform VM and deep breathing. Third, for the statistical aspect, more patients with parkinsonism and normal controls are needed to obtained reliability. Moreover, the mean duration of onset in patients with MSA-P was relatively long, although no statistically significant difference was found. Lastly, although there was no difference in the disease duration between two groups, H&Y, UPDRS, and UMSARS score in the MSA-P group were slightly higher than those in the IPD group (P = 0.045) despite our efforts to enroll patients within the H&Y score of 3. This is because patients with MSA-P have a relatively early functional impairment. Further studies are needed to investigate whether AFTs can serve as a biomarker in patients with parkinsonism and autonomic dysfunction through various prospective studies.
Funding
This work was supported by a grant from the Soonchunhyang University Research Fund.
Conflicts of interest
None.
Supplementary Material
Footnotes
How to cite this article: Park JY, Yang D, Yang HJ, Kim HA, Kim S, Heo D, Park JH, Lee ES, Lee TK. Quantitative autonomic function test in differentiation of multiple system atrophy from idiopathic Parkinson disease. Chin Med J 2019;00:00–00. doi: 10.1097/CM9.0000000000000359
Ji-Yun Park and Dongseok Yang contributed equally to this work.
References
- 1.Wenning GK, Tison F, Ben Shlomo Y, Daniel SE, Quinn NP. Multiple system atrophy: a review of 203 pathologically proven cases. Mov Disord 1997; 12:133–147. doi: 10.1002/mds.870120203. [DOI] [PubMed] [Google Scholar]
- 2.Lipp A, Sandroni P, Ahlskog JE, Fealey RD, Kimpinski K, Iodice V, et al. Prospective differentiation of multiple system atrophy from Parkinson disease, with and without autonomic failure. Arch Neurol 2009; 66:742–750. doi: 10.1001/archneurol.2009.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bonuccelli U, Lucetti C, Del Dotto P, Ceravolo R, Gambaccini G, Bernardini S, et al. Orthostatic hypotension in de novo Parkinson disease. Arch Neurol 2003; 60:1400–1404. doi: 10.1001/archneur.60.10.1400. [DOI] [PubMed] [Google Scholar]
- 4.Baschieri F, Calandra-Buonaura G, Doria A, Mastrolilli F, Palareti A, Barletta G, et al. Cardiovascular autonomic testing performed with a new integrated instrumental approach is useful in differentiating MSA-P from PD at an early stage. Parkinsonism Relat Disord 2015; 21:477–482. doi: 10.1016/j.parkreldis.2015.02.011. [DOI] [PubMed] [Google Scholar]
- 5.Kimpinski K, Iodice V, Burton DD, Camilleri M, Mullan BP, Lipp A, et al. The role of autonomic testing in the differentiation of Parkinson's disease from multiple system atrophy. J Neurol Sci 2012; 317:92–96. doi: 10.1016/j.jns.2012.02.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Reimann M, Schmidt C, Herting B, Prieur S, Junghanns S, Schweitzer K, et al. Comprehensive autonomic assessment does not differentiate between Parkinson's disease, multiple system atrophy and progressive supranuclear palsy. J Neural Transm (Vienna) 2010; 117:69–76. doi: 10.1007/s00702-009-0313-y. [DOI] [PubMed] [Google Scholar]
- 7.Magalhaes M, Wenning GK, Daniel SE, Quinn NP. Autonomic dysfunction in pathologically confirmed multiple system atrophy and idiopathic Parkinson's disease--a retrospective comparison. Acta Neurol Scand 1995; 91:98–102. doi: 10.1111/j.1600-0404.1995.tb00414.x. [DOI] [PubMed] [Google Scholar]
- 8.Riley DE, Chelimsky TC. Autonomic nervous system testing may not distinguish multiple system atrophy from Parkinson's disease. J Neurol Neurosurg Psychiatry 2003; 74:56–60. doi: 10.1136/jnnp.74.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ewing DJ, Clarke BF. Diagnosis and management of diabetic autonomic neuropathy. Br Med J (Clin Res Ed) 1982; 285:916–918. doi: 10.1136/bmj.285.6346.916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Low PA. Composite autonomic scoring scale for laboratory quantification of generalized autonomic failure. Mayo Clin Proc 1993; 68:748–752. doi: 10.1016/s0025-6196(12)60631-4. [DOI] [PubMed] [Google Scholar]
- 11.Vogel ER, Sandroni P, Low PA. Blood pressure recovery from Valsalva maneuver in patients with autonomic failure. Neurology 2005; 65:1533–1537. doi: 10.1212/01.wnl.0000184504.13173.ef. [DOI] [PubMed] [Google Scholar]
- 12.Novak P. Assessment of sympathetic index from the Valsalva maneuver. Neurology 2011; 76:2010–2016. doi: 10.1212/WNL.0b013e31821e5563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schrezenmaier C, Singer W, Swift NM, Sletten D, Tanabe J, Low PA. Adrenergic and vagal baroreflex sensitivity in autonomic failure. Arch Neurol 2007; 64:381–386. doi: 10.1001/archneur.64.3.381. [DOI] [PubMed] [Google Scholar]
- 14.Daniel SE, Lees AJ. Parkinson's Disease Society Brain Bank, London: overview and research. J Neural Transm Suppl 1993; 39:165–172. [PubMed] [Google Scholar]
- 15.Gilman S, Wenning GK, Low PA, Brooks DJ, Mathias CJ, Trojanowski JQ, et al. Second consensus statement on the diagnosis of multiple system atrophy. Neurology 2008; 71:670–676. doi: 10.1212/01.wnl.0000324625.00404.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Micieli G, Tosi P, Marcheselli S, Cavallini A. Autonomic dysfunction in Parkinson's disease. Neurol Sci 2003; 24 suppl 1:S32–S34. doi: 10.1007/s100720300035. [DOI] [PubMed] [Google Scholar]
- 17.Merola A, Romagnolo A, Rosso M, Suri R, Berndt Z, Maule S, et al. Autonomic dysfunction in Parkinson's disease: a prospective cohort study. Mov Disord 2018; 33:391–397. doi: 10.1002/mds.27268. [DOI] [PubMed] [Google Scholar]
- 18.Magerkurth C, Schnitzer R, Braune S. Symptoms of autonomic failure in Parkinson's disease: prevalence and impact on daily life. Clin Auton Res 2005; 15:76–82. doi: 10.1007/s10286-005-0253-z. [DOI] [PubMed] [Google Scholar]
- 19.Goldstein DS. Orthostatic hypotension as an early finding in Parkinson's disease. Clin Auton Res 2006; 16:46–54. doi: 10.1007/s10286-006-0317-8. [DOI] [PubMed] [Google Scholar]
- 20.Sandroni P, Ahlskog JE, Fealey RD, Low PA. Autonomic involvement in extrapyramidal and cerebellar disorders. Clin Auton Res 1991; 1:147–155. doi: 10.1007/BF01826212. [DOI] [PubMed] [Google Scholar]
- 21.Schmidt C, Herting B, Prieur S, Junghanns S, Schweitzer K, Globas C, et al. Valsalva manoeuvre in patients with different Parkinsonian disorders. J Neural Transm (Vienna) 2009; 116:875–880. doi: 10.1007/s00702-009-0239-4. [DOI] [PubMed] [Google Scholar]
- 22.Holmberg B, Kallio M, Johnels B, Elam M. Cardiovascular reflex testing contributes to clinical evaluation and differential diagnosis of Parkinsonian syndromes. Mov Disord 2001; 16:217–225. doi: 10.1002/mds.1062. [DOI] [PubMed] [Google Scholar]
- 23.Roy S, Jaryal AK, Srivastava AK, Deepak KK. Cardiovagal baroreflex sensitivity in Parkinson's disease and multiple-system atrophy. J Clin Neurol 2016; 12:218–223. doi: 10.3988/jcn.2016.12.2.218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lahrmann H, Cortelli P, Hilz M, Mathias CJ, Struhal W, Tassinari M. EFNS guidelines on the diagnosis and management of orthostatic hypotension. Eur J Neurol 2006; 13:930–936. doi: 10.1111/j.1468-1331.2006.01512.x. [DOI] [PubMed] [Google Scholar]
- 25.Freeman R, Wieling W, Axelrod FB, Benditt DG, Benarroch E, Biaggioni I, et al. Consensus statement on the definition of orthostatic hypotension, neurally mediated syncope and the postural tachycardia syndrome. Auton Neurosci 2011; 161:46–48. doi: 10.1016/j.autneu.2011.02.004. [DOI] [PubMed] [Google Scholar]
- 26.Coon EA, Sletten DM, Suarez MD, Mandrekar JN, Ahlskog JE, Bower JH, et al. Clinical features and autonomic testing predict survival in multiple system atrophy. Brain 2015; 138:3623–3631. doi: 10.1093/brain/awv274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Takeuchi S, Sugiyama Y, Mano T, Iwase S, Matsukawa T. Effect of L-dopa on human muscle sympathetic nerve activity. Environ Med 1993; 37:99–102. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


