Abstract
Rationale:
Multiple myeloma is the second most common hematological malignancy. Extramedullary involvement is one of the indicators of poor prognosis. There is no consensus in treatment options and the efficacy. This article reports a case of multiple myeloma with onset of pancreas involvement. Amyloidosis secondary to multiple myeloma and a partial response to the chemotherapy treatment further emphasized its rarity.
Patient concerns:
In this article, we report a 59-year-old male patient with a chief complaint of fatigue for 8 months and upper abdominal pain for 2 months.
Diagnosis:
The patients were diagnosed as amyloidosis secondary to multiple myeloma with pancreatic occupying (head–neck junction area) lesion based on laboratory examination and pathology from lymph node puncture and skin biopsy.
Interventions:
An intensive chemotherapy treatment as bortezomib, lenalidomide, dexamethasone, cisplatin, epirubicin, cyclophosphamide, and etoposide was given. Due to intolerance, treatment regimen was further adjusted to bortezomib, lenalidomide, and dexamethasone.
Outcomes:
The patient was 12 months alive. After 4 cycles of chemotherapy, a partial response was achieved and abdominal magnetic resonance imaging suggested a reduced pancreatic occupying lesion.
Lessons:
This case demonstrates that pancreatic involvement, digestive system neoplasm, and amyloidosis-related clinical features may be the earliest manifestations of multiple myeloma. For these patients, an intensive chemotherapy regimen may be a possible treatment approach.
Keywords: amyloidosis, extramedullary involvement, multiple myeloma, pancreas, plasmacytoma
1. Introduction
Multiple myeloma is the second most common hematological malignancy characterized by neoplastic proliferation of monoclonal plasma cells in the bone marrow.[1,2] It can only occur in bone marrow or extramedullary sites and the latter is relatively less frequent, especially the involvement of pancreas.[3] It is reported that these pancreas involved patients are mostly diagnosed as multiple myeloma first and then present pancreas involvement subsequently.[4] We herein report a case of multiple myeloma with onset of pancreas involvement. Amyloidosis secondary to myeloma confirmed by skin biopsy further emphasized the rarity of this case.
2. Case report
A 59-year-old male patient was hospitalized on May 2, 2018 with a chief complaint of fatigue for 8 months and upper abdominal pain for 2 months. His abdominal enhanced computed tomography scan (CT scan) in August 2017 indicated a suspicious soft tissue mass (2.3 × 2.6 cm) in the space between hilar and head of pancreas, and he was recommended a follow-up observation. In February 2018, he presented a burning pain with 2 to 3 points visual analog score in the upper abdomen, which was not related to eating or body position. There was no other digestive system discomfort and the routine blood test was normal. Blood tests showed increase in globulin (42.6 g/L) as well as β2-microglobulin (4.69 mg/L) and decrease in calcium (1.97 mmol/L). Total protein and creatinine were normal. Enhanced CT scan detected a 2.8 cm soft tissue nodule in the head of pancreas and swelling of retroperitoneal lymph node (2.3 cm) shown in Figure 1. T9 vertebral body and accessory bone were destroyed and L2 vertebral presented compression changes from X-ray scan (Fig. 2). He received a puncture of retroperitoneal lymph node guided by ultrasound on April 20th. Small round tumor cells were observed under light microscope. The results of immunohistochemistry as shown below: AAT (2+), ACT (2+), CD138 (2+), CD79α(2+), CD20 (local focus 2+), Kappa (1+), Lamda (>2+), MUM1 (2+), Pax-5 (1+), AE1/AE3, LCA, CD3, CD56, ChrA, PD-1, PD-L1, Syno (−), Ki-67 (+, 5%). Combined with the results of immunohistochemistry, the lymph node was considered as a plasmacytoma.
Figure 1.
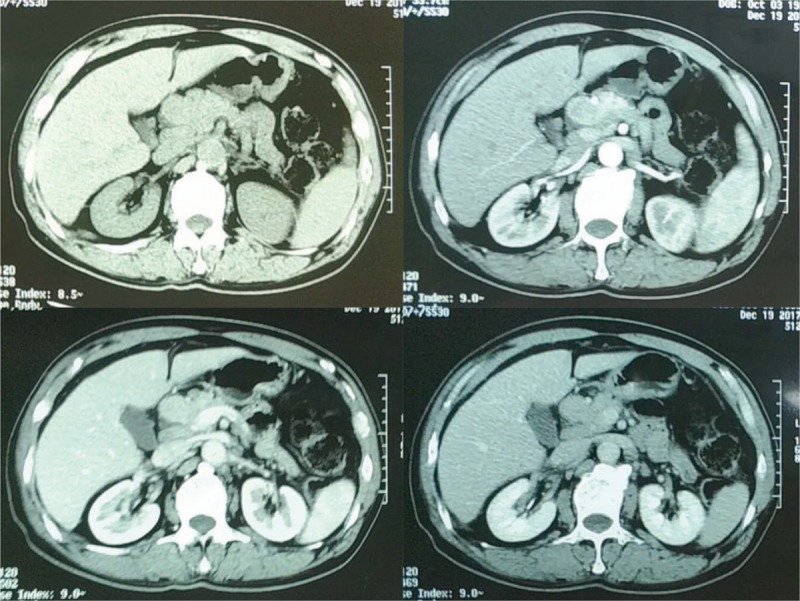
Abdominal enhanced CT scan (upper left: plain scan phase, upper right: arterial phase, lower left: venous phase, lower right: delayed phase). CT = computed tomography.
Figure 2.
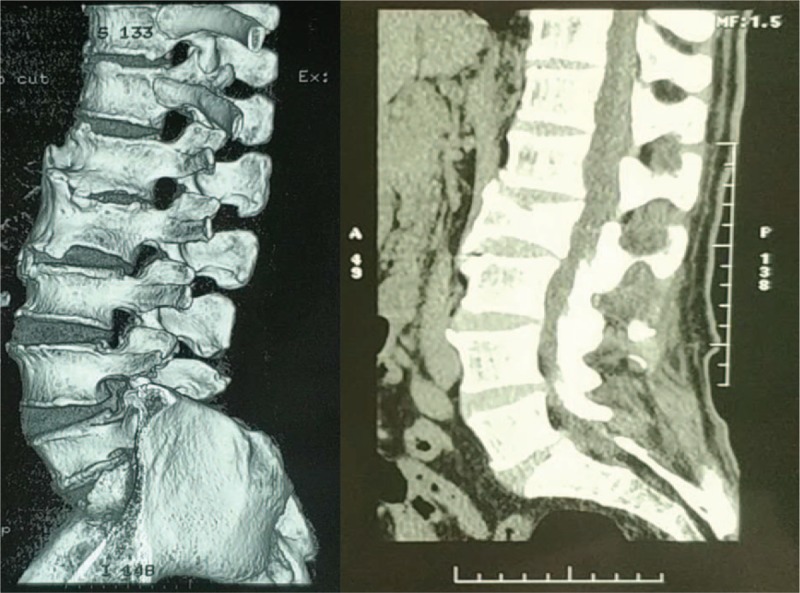
Lumbar X-ray film and reconstruction.
After admission, further evaluations were performed. The immunoglobulin test showed an immunoglobulin A level of 22.96 g/L and a M protein level of 21.20 g/L (accounting for 29.6%). Serum immunofixation electrophoresis indicated the presence of immunoglobulin A lambda lanes and the level of serum-free light chain were 1595.0 mg/L for lambda lanes and 11.3 mg/L for the kappa lanes. Urine tests showed a lambda lanes level of 7210 mg/24 h and a kappa lanes level of 82 mg/24 h. Urinary immunofixation electrophoresis also indicated the presence of free light chain lambda lanes. The bone marrow smear indicated the proportion of plasma cells was 10.5%; and some of the cells were featured by disappearing primordial areas, flamboyant shape, and binuclear appearance. The flow cytometry of bone marrow revealed the proportion of atypical cells was 3.6%. It expressed lambda lanes restrictively, expressed CD38 and CD138 strongly and CD117, CD56 simultaneously, which was consistent with features of the multiple myeloma. No common chromosome translocation was observed by fluorescence in situ hybridization. The immunohistochemistry from posterior iliac bone marrow biopsy showed CD3 (diffused distribution +), CD20 (−), CD138 (+), CD38 (+), CD15 (+), MPO (+), which was in accordance with plasmacytoma. Combined with the results of laboratory examinations, he was diagnosed as multiple myeloma.
Furthermore, the patient showed a blood pressure fluctuation between 75 mm Hg to 90 mm Hg for systolic pressure and 45 mm Hg to 55 mm Hg for diastolic pressure. His physical examination indicated swellings of both hands fingertips (Fig. 3). The level of 24 hours urine protein was 3 g to 5 g and glomerular protein accounting for 90%. Atrial septum thickening and echo enhancement were shown by echocardiogram which suggested a possible infiltration in myocardium by amyloid deposition. A fingertip skin biopsy finally revealed amyloid deposition, which indicated an amyloidosis secondary to multiple myeloma.
Figure 3.
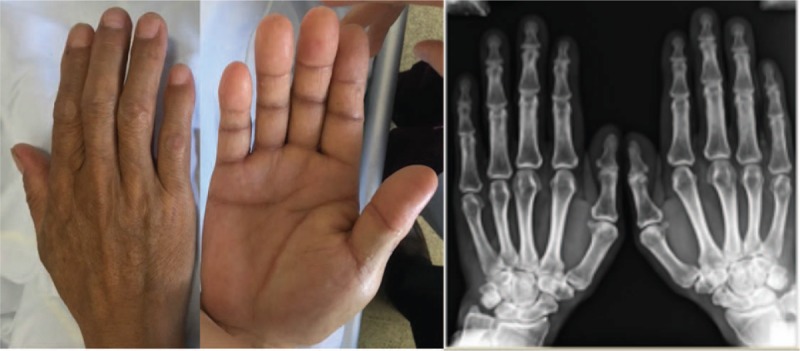
Hands physical examination and X-ray film.
Since patients with extramedullary multiple myeloma tended to show poor prognosis, we prescribed an intensive chemotherapy treatment as bortezomib, lenalidomide, dexamethasone, cisplatin, epirubicin, cyclophosphamide, and etoposide (V + R + DT − PACE). Due to intolerance, including III degree thrombocytopenia and IV degree neutropenia based on the common terminology criteria for adverse events version 4.03,[5] the treatment regimen was further adjusted to bortezomib, lenalidomide, and dexamethasone (VRD). After 4 cycles of chemotherapy, according to the guidelines for the diagnosis and management of multiple myeloma,[1–3] a partial response was achieved and abdominal magnetic resonance imaging suggested a reduced pancreatic occupying (head–neck junction area) than that before the treatment (Fig. 4). Since the intensive chemotherapy rigmen showed good response, we maintained this reigmen for the patient. The patient is in good general condition during the follow-up period and still alive 12 months after diagnosis.
Figure 4.
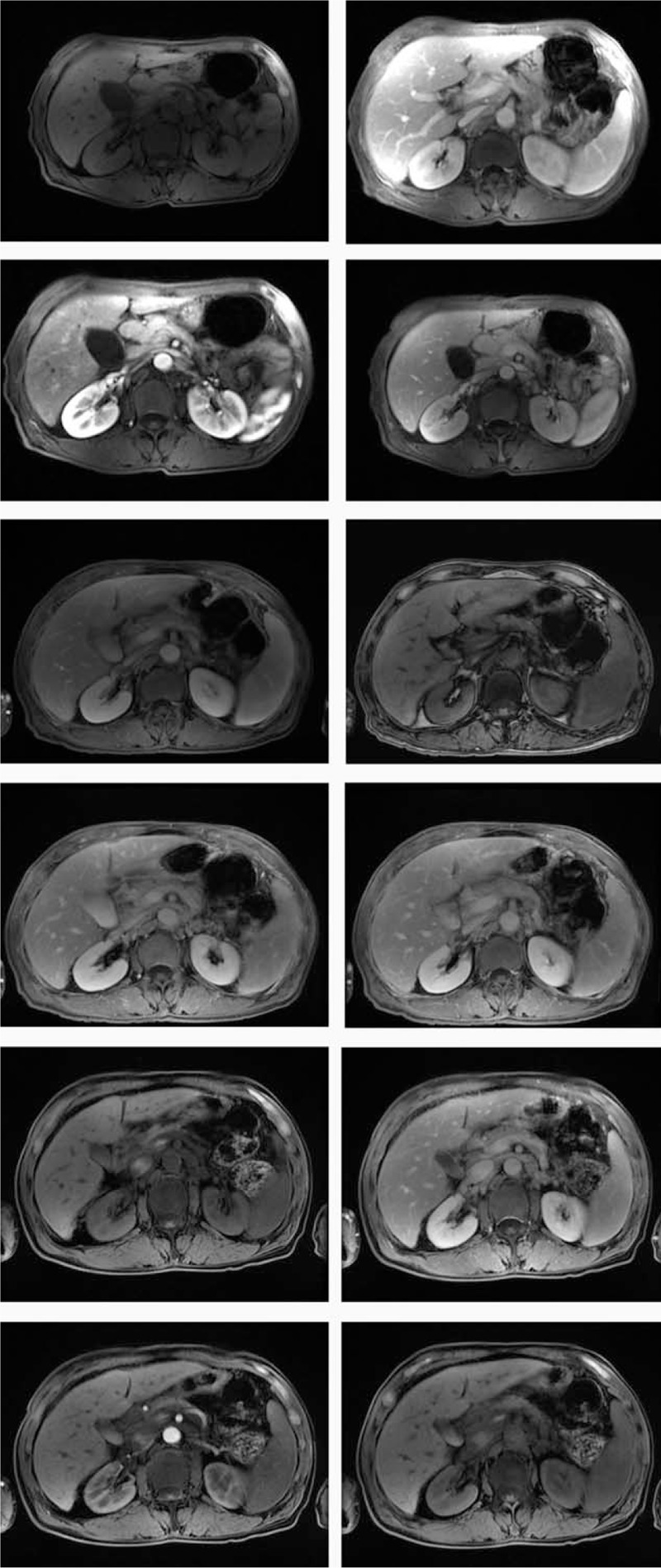
Pancreas enhanced MRI. (A) Pancreas enhanced MRI before treatment (the upper 4 pictures). Note: para-hilar area, head of pancreas, areas around the body and tail of pancreas, and retroperitoneum showed equal T1 signal, long T2 signal, and mild enhancement in enhanced scan, the boundary between partial lesions and pancreas and stomach wall was unclear. (B) Pancreas enhanced MRI after 1 course of chemotherapy treatment (the middle 4 pictures) Pancreatic occupying (head–neck junction area) was reduced than Figure 4A, with new T2 signal. Abnormal signals shown in para-hilar, pancreatic head, body and tail, and retroperitoneal area may be lymph node swollen. (C) Pancreas enhanced MRI after 4 courses of chemotherapy treatment (4 pictures at the bottom). Pancreatic occupying (head–neck junction area) was reduced with long T2 signal. Abnormal signals shown in para-hilar, pancreatic head, body and tail, and retroperitoneal area may be lymph node swollen. MRI magnetic resonance imaging.
3. Discussion
Multiple myeloma is a disease characterized by malignant proliferation of plasma cells typically involving medullary bones.[6] It can present as solitary multiple myeloma and extramedullary plasmacytoma. Extramedullary plasmacytoma representing less than 5% of all plasma cell neoplasms is often diagnosed after multiple myeloma and patients with onset of extramedullary lesions are relatively rare.[4] Extramedullary plasmacytoma may present multiple lesions including lymph nodes, soft tissue, and upper respiratory tract which are more common. The digestive system is less involved and the most cases are usually shown as amyloid deposition in the liver and spleen. Involvement of pancreas is rather rare.[7]
Currently, there are about 70 cases of pancreas plasmacytoma reported, 34 cases of multiple myeloma involving the pancreas, which are mostly diagnosed multiple myeloma first and then present pancreas involvement subsequently.[8] Multiple myeloma with onset of pancreas involvement was first reported in 1958 and 8 cases have been reported so far (Table 1).[9–16]
Table 1.
Case reports of solitary pancreatic plasmacytoma.
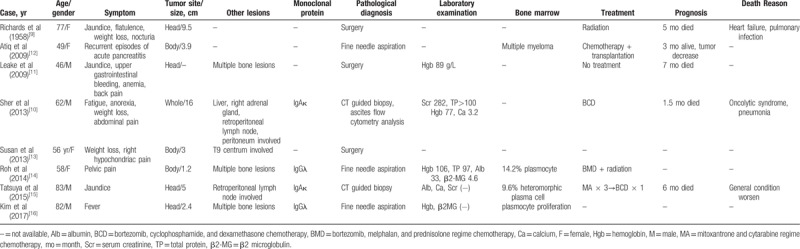
Among cases of multiple myeloma involving the pancreas reported, currently no patients showed the amyloidosis secondary to myeloma like our report, which emphasize on its rarity and diagnostic issues. Besides, among cases of multiple myeloma with onset of pancreas involvement, different from atypical symptoms such as upper abdominal pain and fatigue in this case, most patients have severe symptoms including jaundice, anemia, hypercalcemia, and so on rising a challenge for differential diagnosis with pancreatic cancer and a requirement for pathology biopsy consequently. Among the 8 patients, 3 patients (37.5%) were confirmed as plasmacytoma by surgery pathology. Other patients (62.5%) obtained pathology by fine needle aspiration as same as this case.
Treatments have been reported in the literature include conservative treatment, radiotherapy, stem cell transplantation, and different regimens of chemotherapy, such as bortezomib, cyclophosphamide, dexamethasone regimen, and so on. However, for the multiple myeloma patients with onset of pancreas, there is no consensus in treatment options and the efficacy of these treatments still need to be verified.[9–16] In this case, an intensive chemotherapy regimen of V + R + DT − PACE and VRD showed a relatively good response, indicating a possible treatment approach to patients with multiple myeloma involving the pancreas further.
Extramedullary involvement is one of the indicators of poor prognosis in multiple myeloma, with an average overall survival time of 36 months.[7] Patients with onset of pancreas usually have a worse prognosis than other extramedullary lesions. Nevertheless, there are no large-scale retrospective studies about this yet. According to the case reports, the longest survival time is 7 months.[11] Reasons of death are mostly infections during chemotherapy treatment[9,10] and only 1 patient died of systemic failure.[15]
In conclusion, we reported a case of multiple myeloma with onset of pancreatic plasmacytoma and secondary amyloidosis. By analyzing the clinical manifestations, diagnosis, and treatment, this case demonstrates pancreatic lesion, digestive system neoplasm, and amyloidosis-related clinical manifestations may be the earliest manifestations of multiple myeloma, which is worth being concerned by clinicians.
Author contributions
Conceptualization: Lu Zhang.
Formal analysis: Xin Wang.
Investigation: Xin Wang, Huaiya Xie.
Supervision: Lu Zhang.
Writing – original draft: Xin Wang.
Writing – review and editing: Huaiya Xie, Lu Zhang.
Footnotes
Abbreviations: CT = computed tomography, V + R + DT − PACE = bortezomib, lenalidomide, dexamethasone, cisplatin, epirubicin, cyclophosphamide, and etoposide, VRD = bortezomib, lenalidomide, and dexamethasone.
The patient has provided informed consent for publication of this case and accompanying images.
The authors have no conflicts of interest to disclose.
References
- [1].Chinese Hematology Association; Chinese Society of Hematology; Chinese Myeloma Committee-Chinese Hematology Association. The guidelines for the diagnosis and management of multiple myeloma in China (2017 revision). Zhonghua Nei Ke Za Zhi 2017;56:866–70. [DOI] [PubMed] [Google Scholar]
- [2].Moreau P, San MJ, Ludwig H, et al. Multiple myeloma: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 2013;24suppl 6:vi133–7. [DOI] [PubMed] [Google Scholar]
- [3].Iida S, Ishida T, Murakami H, et al. JSH practical guidelines for hematological malignancies, 2018: III. Myeloma-1. Multiple myeloma (MM). Int J Hematol 2019;109:509–38. [DOI] [PubMed] [Google Scholar]
- [4].Hirata S, Yamaguchi K, Bandai S, et al. Secondary extramedullary plasmacytoma involving the pancreas. J Hepatobiliary Pancreat Surg 2002;9:111–5. [DOI] [PubMed] [Google Scholar]
- [5].US Department of Health and Human Services. “Common terminology criteria for adverse events (CTCAE) version 4.0.” National Institutes of Health, National Cancer Institute 4.03 (2009). [Google Scholar]
- [6].Campo E, Swerdlow SH, Harris NL, et al. The 2008 WHO classification of lymphoid neoplasms and beyond: evolving concepts and practical applications. Blood 2011;117:5019–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Weinstock M, Ghobrial IM. Extramedullary multiple myeloma. Leuk Lymphoma 2013;54:1135–41. [DOI] [PubMed] [Google Scholar]
- [8].Williet N, Kassir R, Cuilleron M, et al. Difficult endoscopic diagnosis of a pancreatic plasmacytoma: case report and review of literature. World J Clin Oncol 2017;8:91–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Richards WG, Katzmann FS, Coleman FC. Extramedullary plasmacytoma arising in the head of the pancreas; report of a case. Cancer 1958;11:649–52. [DOI] [PubMed] [Google Scholar]
- [10].Sher T, Bhat S, Jitawatanarat P, et al. Multiple myeloma mimicking metastatic pancreas cancer. J Clin Oncol 2013;31:297–9. [DOI] [PubMed] [Google Scholar]
- [11].Leake PA, Coard KC, Plummer JM. Extramedullary plasmacytoma of the pancreas as an uncommon cause of obstructive jaundice: a case report. J Med Case Rep 2009;3:8785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Atiq M, Ali SA, Dang S, et al. Pancreatic plasmacytoma presenting as variceal hemorrhage: life threatening complication of a rare entity. J Pancreas 2009;10:187–8. [PubMed] [Google Scholar]
- [13].Hue SS, Azhar R. Plasmacytoma of the pancreas: an unusual manifestation of multiple myeloma. Singapore Med J 2013;54:e105–7. [DOI] [PubMed] [Google Scholar]
- [14].Hoon RY, Youn HS, Seon-Mi L, et al. Extramedullary plasmacytoma of the pancreas diagnosed using endoscopic ultrasonography-guided fine needle aspiration. Clin Endosc 2014;47:115–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Utsumi T, Sasajima J, Goto T, et al. The detection of pancreatic and retroperitoneal plasmacytoma helped to diagnose multiple myeloma: a case report. Medicine 2015;94:e914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Kim JH, Paik WH, Joo M, et al. Extramedullary plasmacytoma mimicking pancreatic cancer: a case report and literature review. Endosc Ultrasound 2017;6:269–72. [DOI] [PMC free article] [PubMed] [Google Scholar]


