Abstract
Background:
Most clinical and laboratory smoking research studies require that participants smoke at a certain level to be eligible for enrollment. However, there is limited evidence that use of these cutoffs differentiates groups of smokers along clinically meaningful criteria.
Methods:
Using receiver operating characteristic curves, we analyzed data from daily smokers in the National Epidemiologic Study of Alcohol Use and Related Conditions - III (NESARC-III) to examine the utility of smoking rates for determining whether participants met DSM-5 criteria for tobacco use disorder, experienced nicotine withdrawal or had a history of failed quit attempts. We also examined whether relationships between these variables differed as a function of key sample characteristics.
Results:
Smoking rate exhibited a weak relationship with the presence of tobacco use disorder (AUC = .664), whether individuals experience nicotine withdrawal (AUC = .672) and whether individuals had a history of failed quit attempts (AUC = .578). The relationship between smoking rate and a history of failed quit attempts was weaker for women than men (p < .05). Otherwise, utility did not differ as a function of sex, race/ethnicity, education, income, or use of multiple tobacco products. Optimal cutoffs varied somewhat across indices, but the largest number of correct classifications occurred at very low smoking rates.
Conclusions:
Researchers should consider abandoning the use of smoking rate cutoffs to determine study eligibility. If smoking rate cutoffs are used, a rationale should be presented along with justification for the specific cutoff chosen.
Keywords: Smoking, tobacco, cigarettes, nicotine dependence, withdrawal, methodology
1. INTRODUCTION
Investigators routinely require participants to smoke a minimum number of cigarettes per day to be eligible to participate in clinical and laboratory smoking research studies. A review of papers published in the journals Nicotine & Tobacco Research, Drug and Alcohol Dependence, and Addictive Behaviors between January, 2017 and December, 2018 identified 134 clinical trials and 131 human laboratory studies, of which 74.3% reported an explicit smoking rate cutoff as an eligibility requirement, with specific cutoffs varying from 4 cigarettes every 2 weeks to 20 cigarettes per day (CPD). Of studies that used a cutoff, 72.6% used cutoffs of either ≥ 5 CPD or ≥ 10 CPD. No author explicitly stated a rationale for the chosen cutoff. However, an implicit assumption appeared to be that restricting the sample to heavier smokers provides some assurance participants will meet criteria for tobacco use disorder, experience withdrawal, or otherwise have difficulty quitting. Yet despite the relatively ubiquitous application of smoking rate cutoffs as an eligibility criterion, few have scrutinized their utility for this purpose.
Individual smoking rates are unquestionably driven by multiple factors, including ones external to the smoker – such as local tobacco control policies.1 Accordingly, it seems reasonable to question whether the relationship between smoking rate and other clinical variables is strong enough to justify the use of smoking rate as a diagnostic indicator. Such a seemingly minor decision carries important scientific and ethical implications. Even light smoking poses substantial health risks, so understanding the reasons for smoking in this population and developing effective interventions is critical.2,3 Despite the assumption that light smokers are readily able to quit without intervention, many light smokers struggle with cessation.4,5 Smoking rate cutoffs directly impact study generalizability and could contribute to health disparities by excluding disproportionate numbers of racial and ethnic minorities.6,7 Moreover, smoking rates have declined over time, and approximately half the population of current smokers would be classified as light smokers.8 This effect is likely to compound as the smoking rate continues to decline, which has important practical implications for conducting research.9,10
Prior research has noted an apparent weak or modest relationship between smoking rate and tobacco use disorder. Dierker et al. (2007) examined this issue among college students and reported a positive relationship between smoking rate and DSM-IV nicotine dependence (renamed tobacco use disorder in DSM-5). Yet the strength of this relationship was modest, with approximately 35% of individuals smoking 16–25 cigarettes/week meeting criteria for dependence and only 60% of those smoking > 100/week meeting criteria for dependence.11 Another study found that among the U.S. general population, nearly 40% of daily smokers never met criteria for nicotine dependence.12 A follow-up study examined this issue among individuals with depression, alcohol use disorders, or specific phobias and found that the general population was less likely to meet criteria for dependence, even at the same smoking rate, relative to those with psychiatric illness –revealing one way factors besides smoking rate contribute to dependence.13 Similar evidence exists indicating psychiatric illness impacts the experience of nicotine withdrawal and plays a role in difficulty with cessation.14,15 Although there is some evidence indicating smoking rate prospectively predicts cessation outcome in clinical trials, this relationship nonetheless appears relatively modest.16 Taken together, these findings suggest only a modest and seemingly linear relationship between smoking rate and variables of immediate clinical interest. In the absence of either an extremely robust relationship or an obvious breakpoint in smoking rate above which the presence of tobacco use disorder or other clinically relevant variables (e.g., withdrawal, difficulty quitting) is exponentially more likely, the utility of smoking rate cutoffs is unclear.
Despite the research described above, use of smoking rate cutoffs has become standard in clinical and laboratory smoking research. The present project emerged from our collective concern with the continued use of CPD cutoffs in tobacco research, despite the potential untoward consequences, previous calls to reconsider their merit and lack of empirical data to justify their use.1,7 The primary aim of the present project is to clearly highlight the utility of smoking rate as a singular determinant of whether an individual is likely to meet criteria for tobacco use disorder, experience nicotine withdrawal, or report difficulty quitting. We present results using receiver operating characteristic curves, a familiar method commonly applied in many studies of diagnostic testing. In addition, we present data on the sensitivity/specificity across specific cutoff values. This will allow readers to clearly see the impact of specific cutoff values and can help identify the most appropriate cutoff in cases where their use is appropriate or necessary. Lastly, we examine whether the relative utility of CPD as a determinant of tobacco use disorder/withdrawal/difficulty quitting varies as a function of key population characteristics (e.g., race/ethnicity, sex, socioeconomic status, multiple tobacco product use), in order to determine if its use may be more or less appropriate for specific populations of smokers.
2. MATERIAL AND METHODS
2.1. Participants and Procedures
We analyzed data from daily smokers in the National Epidemiological Study of Alcohol and Related Conditions – III (NESARC-III). A detailed description of study procedures is available elsewhere.18 In brief, the NESARC-III is a nationally representative study of the noninstitutionalized adult civilian population in the United States. Data collection for NESARC-III occurred from April, 2012 to June, 2013 and responses were obtained from 36,309 individuals. The overall survey response rate was 60.1%. The present study only considered individuals who reported daily cigarette use as their typical smoking pattern over the past year and had smoking rate (CPD) data available (n = 6,822).
2.2. Measures
In-person computer-assisted interviews were conducted using the Alcohol Use Disorder and Associated Disabilities Interview Schedule (AUDADIS-5). Presence of past-year tobacco use disorder was assessed according to DSM-5 criteria. Prior research indicates good test-retest reliability of the tobacco use disorder module of the AUDADIS-5, as well as strong convergence between this module and other tobacco use disorder measures.19,20 Nicotine withdrawal symptoms included the seven DSM-5 nicotine withdrawal symptoms, as well as use of tobacco or other nicotine products to relieve or avoid withdrawal symptoms, waking up in the middle of the night to use tobacco or nicotine, often using tobacco just after getting up in the morning, or using tobacco just after being in a situation where use was not permitted. For purposes of the present analyses, individuals were considered to experience nicotine withdrawal if they endorsed experiencing any of these symptoms over the past year. Individuals were considered to have difficulty quitting if they reported having more than once tried to stop or cut down on tobacco use and been unable to do so. In this instance only, we opted to use lifetime history in lieu of past-year because many smokers do not make multiple quit attempts within a given year. Smoking rate was recorded as the usual number of CPD smoked over the past year. Individuals were coded as multiple tobacco product users if they reported any use of non-cigarette nicotine or tobacco products (e.g., cigars, pipes, snuff/chew or e-cigarettes) over the past year. In addition, individuals reported on a variety of demographic variables including sex, race/ethnicity, education and household income. Due to the relatively small number of daily smokers who identified as American Indian/Alaska Native (n = 137) or Asian/Native Hawaiian/Other Pacific Islander (n = 178), these were collapsed into a single category (i.e., “Other”) for purposes of analyses. Income was dichotomized based on annual household income < $25,000 versus ≥ $25,000 and education was dichotomized based on highest degree being ≤ High School Diploma/GED versus at least some post-secondary education. In both cases, cutoffs were based on median splits.
2.3. Analysis Plan
We used Receiver Operating Characteristic (ROC) curve analysis to examine the overall utility of CPD in determining whether an individual would meet criteria for tobacco use disorder, experience nicotine withdrawal or have difficulty quitting. We calculated sensitivity (i.e., probability of a positive test given a known positive disease state) and specificity (i.e., probability of a negative test given a known negative disease state) for the three variables across all possible CPD cutoff values. The ROC curve is a graphical representation of sensitivity relative to the false positive rate (1-specificity), with the area under the curve (AUC) representing the overall utility of CPD in classification. The present study employed a non- parametric approach to ROC curve analysis. We also used several empirical techniques to identify the optimal cut point on a ROC curve by calculating: 1) Youden’s J Statistic; 2) Liu’s Index; and 3) Minimal Distance to the 0,1 Coordinate; in an effort to identify the value of CPD that offered the optimal balance of sensitivity and specificity.21–23 In addition to examining AUC for tobacco use disorder, nicotine withdrawal and difficulty quitting across the overall sample of daily smokers, we also examined whether AUC differed as a function of sex, race/ethnicity, education, income, or use of multiple tobacco products. AUC comparisons were done using the DeLong method.24
3. RESULTS
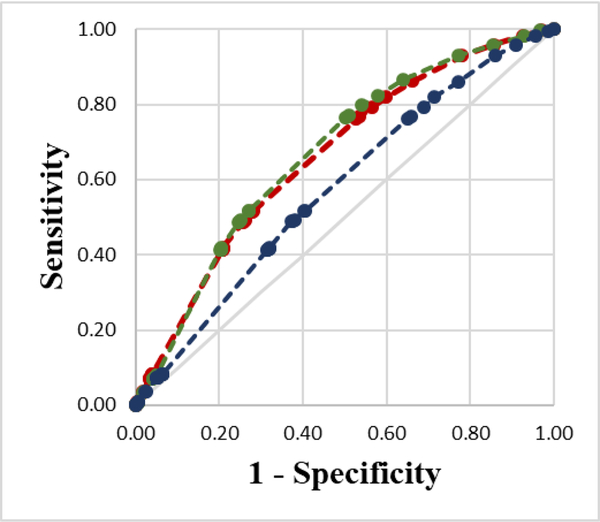
See Table 1 for a detailed breakdown of smoking rates and classification results by CPD cutoff. ROC plots are presented in Figure 1.
Table 1.
Sensitivity and specificity of cigarette per day cut points
| Cigarettes Per Day |
Tobacco Use Disorder N = 6,822 |
Nicotine Withdrawal N = 6,819 |
Difficulty Quitting N = 6,818 |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Cutoff Value | Cumulative % of Smokers | Sensitivity | Specificity | % Correctly Classified |
Sensitivity | Specificity | % Correctly Classified |
Sensitivity | Specificity | % Correctly Classified |
| ≥ 1 | 100.00% | 100.00% | 0.00% | 85.25% | 100.00% | 0.00% | 85.34% | 100.00% | 0.00% | 68.48% |
| ≥ 2 | 99.27% | 99.66% | 2.98% | 85.40% | 99.69% | 3.20% | 85.54% | 99.55% | 1.35% | 68.60% |
| ≥ 3 | 97.46% | 98.30% | 7.36% | 84.89% | 98.26% | 7.20% | 84.91% | 98.29% | 4.33% | 68.67% |
| ≥ 4 | 94.33% | 95.82% | 14.31% | 83.80% | 95.86% | 14.60% | 83.94% | 95.84% | 8.98% | 68.47% |
| ≥ 5 | 90.84% | 93.04% | 21.87% | 82.54% | 93.18% | 22.80% | 82.86% | 93.06% | 14.01% | 68.14% |
| ≥ 6 | 83.26% | 86.21% | 33.80% | 78.48% | 86.54% | 35.90% | 79.12% | 86.10% | 22.94% | 66.19% |
| ≥ 7 | 78.63% | 81.88% | 40.16% | 75.73% | 82.20% | 42.20% | 76.33% | 81.92% | 28.48% | 65.08% |
| ≥ 8 | 76.06% | 79.42% | 43.34% | 74.10% | 79.82% | 45.90% | 74.85% | 79.42% | 31.18% | 64.21% |
| ≥ 9 | 73.32% | 76.75% | 46.52% | 72.30% | 77.16% | 49.10% | 73.05% | 76.70% | 33.97% | 63.23% |
| ≥ 10 | 72.63% | 76.07% | 47.22% | 71.81% | 76.46% | 49.70% | 72.53% | 76.14% | 34.95% | 63.16% |
| ≥ 11 | 48.21% | 51.70% | 71.97% | 54.69% | 51.81% | 72.90% | 54.91% | 51.77% | 59.52% | 54.21% |
| ≥ 12 | 48.05% | 51.53% | 72.07% | 54.56% | 51.64% | 73.00% | 54.77% | 51.68% | 59.84% | 54.25% |
| ≥ 13 | 45.76% | 49.14% | 73.76% | 52.77% | 49.29% | 74.90% | 53.04% | 49.35% | 62.03% | 53.34% |
| ≥ 14 | 45.46% | 48.83% | 74.06% | 52.55% | 48.96% | 75.10% | 52.79% | 49.05% | 62.35% | 53.24% |
| ≥ 15 | 45.18% | 48.56% | 74.35% | 52.36% | 48.69% | 75.40% | 52.60% | 48.83% | 62.77% | 53.23% |
| ≥ 20 | 38.16% | 41.20% | 79.42% | 46.83% | 41.21% | 79.80% | 46.87% | 41.25% | 68.59% | 49.87% |
| ≥ 25 | 7.42% | 8.01% | 96.02% | 20.99% | 7.84% | 95.10% | 20.63% | 8.07% | 94.00% | 35.16% |
| ≥ 30 | 6.54% | 7.08% | 96.62% | 20.29% | 6.94% | 95.90% | 19.99% | 7.22% | 94.93% | 34.86% |
| ≥ 35 | 3.25% | 3.52% | 98.31% | 17.50% | 3.47% | 98.00% | 17.33% | 3.64% | 97.58% | 33.25% |
| ≥ 40 | 3.12% | 3.39% | 98.41% | 17.40% | 3.37% | 98.30% | 17.29% | 3.47% | 97.63% | 33.15% |
Note. Additional cutoffs >15 were evaluated and are included in ROC plots and analyses, but detailed findings are not included in the table given poor performance and infrequent use in the literature.
Figure 1.
ROC curve showing the utility for cigarettes per day in predicting tobacco use disorder (red; AUC = 0.664), withdrawal symptoms (green; AUC = 0.672) and difficulty quitting (blue; AUC = 0.578). A reference line representing change performance is presented in light grey.
3.1. Tobacco Use Disorder
Among all past-year daily smokers, 85.2% met DSM-5 criteria for tobacco use disorder within the past year. The Area Under the Curve (AUC) was .664 (95% CI 0.645–0.682), indicating CPD was a relatively poor determinant of whether an individual met criteria for tobacco use disorder. Optimal cutoff scores converged across Youden’s Statistic, Liu’s Index and Minimal Distance to the 0,1 Coordinate to indicate optimal performance occurred at a cutoff of ≥ 11 CPD. However, this cutoff only led to correct classification of 54.7% of smokers. A total of 79.5% of individuals smoking < 11 CPD met criteria for tobacco use disorder and 91.4% of individuals smoking ≥ 11 CPD met criteria for tobacco use disorder. The highest proportion (85.4%) of correct classifications occurred at ≥ 2 CPD.
Moderator analyses indicated the AUC did not differ as a function of sex [X2 (1) = 3.05, p = .081], race [X2 (3) = 7.12, p = .068], education [X2 (1) = 0.30, p = .584], income [X2 (1) = 0.34, p = .562], or use of multiple tobacco products [X2 (1) = 0.74, p = .391].
3.2. Withdrawal
With regards to withdrawal, 85.3% of past-year daily smokers reported experiencing at least one nicotine withdrawal symptom within the past year. The AUC was .672 (95% CI 0.6540.691), indicating that CPD also had relatively poor performance for discriminating smokers who experience nicotine withdrawal from those who do not. Optimal cutoff scores differed slightly across indices (Youden’s Statistic: ≥ 9 CPD; Liu’s Index: ≥ 10 CPD; Minimal Distance to 0,1: ≥ 11 CPD). The proportion of correct classifications ranged from 54.9% to 73.0%. When a cutoff of ≥ 10 CPD was used, 73.4% of participants smoking < 10 CPD and 89.8% of participants smoking ≥ 10 CPD reported experiencing nicotine withdrawal. However, as above, the highest proportion of correct classifications (85.5%) occurred at ≥ 2 CPD.
Moderator analyses indicated the AUC did not differ as a function of sex [X2 (1) = 1.14, p = .287], race/ethnicity [X2 (3) = 4.40, p = .222], education [X2 (1) = 1.54, p = .215], income [X2 (1) = 0.58,p = .447], or use of multiple tobacco products [X2 (1) = 0.22,p = .640].
3.3. Difficulty Quitting
Among all past-year daily smokers, 68.5% reported having tried to stop or cut down on tobacco use more than once and been unsuccessful over their lifetime. The AUC was .578 (95% CI 0.563–0.592), indicating that CPD was also a poor indicator of whether individuals have a history of failed quit attempts. Optimal cutoff scores differed across indices (Youden’s Statistic: ≥ 15 CPD; Liu’s Index: ≥ 12 CPD; Minimal Distance to 0,1: ≥ 12 CPD). The proportion of correct classifications was 54.3% for ≥ 12 CPD and 53.2% for ≥ 15 CPD. When a cutoff of ≥ 12 CPD was used, 63.7% of participants smoking < 12 CPD and 73.7% of participants smoking ≥ 11 CPD reported a history of failed quit attempts. However, as with the other two metrics, the highest proportion of correct classifications occurred at a much lower cutoff (≥ 3 CPD; 68.7%).
Moderator analyses indicated the AUC did not differ as a function of race/ethnicity [X2 (3) = 5.76,p = .124], education [X2 (1) = 0.00,p = .986], income [X2 (1) = 0.55,p = .460], or use of multiple tobacco products [X2 (1) = 0.49, p = .485]. However, it did differ as a function of sex [X2 (1) = 5.81,p = .012], with the relationship between cigarettes per day and difficulty quitting being slightly weaker for women (AUC = 0.562; 95% CI 0.542–0.583) than for men (AUC = 0.598, 95% CI 0.578–0.618).
4. DISCUSSION
Overall, results indicate that heavier smokers are more likely than lighter smokers to meet criteria for tobacco use disorder, experience nicotine withdrawal and report difficulty quitting. However, the strength of this relationship is weak, as evidenced by low AUC values. In all cases, these values fell far short of conventional guidelines for a test to be considered a reliable diagnostic indicator (i.e. ≥ .8 AUC).25 Empirically-derived optimal cutoff scores differed somewhat across the three clinical variables and three empirical indices for identifying optimal cut points (ranging from ≥ 9 CPD to ≥ 15 CPD) and were often misaligned with cutoffs commonly observed in the literature.26,27 Despite having poor specificity, the greatest number of correct classifications for both tobacco use disorder and nicotine withdrawal occurred at ≥ 2 cigarettes per day and at ≥ 3 cigarettes per day for difficulty quitting. The relatively high prevalence rates for the variables examined – even among light smokers – likely contributed to this finding. Notably, these cutoffs are substantially less than the most commonly applied cutoffs (i.e. ≥ 5 CPD, ≥ 10 CPD). Although the focus of the present paper is on inclusion/exclusion criteria, these findings also have direct implications for issues (e.g. the utility and use of light/moderate/heavy smoker categories, merits of including smoking rate in dependence measures).
Our intent is certainly not to discredit other researchers for prior use of these cutoffs. Indeed, we have done so routinely in our own work.28–36 However, our impression is that this is often being done out of convention, with only minimal consideration of the implications of these decisions and with surprisingly limited research to guide decisions about the most appropriate cutoff. Findings indicate a majority of light smokers meet criteria for tobacco use disorder, experience nicotine withdrawal, and have difficulty quitting yet as others have noted these individuals are excluded from most research studies.1 This severely limits our knowledge about both the etiology of smoking behavior and efficacious interventions for a substantial portion of smokers. As the number of light smokers continues to increase due to both uptake of low-level smoking and heavy smokers converting to light smoking, this problem is likely to worsen.9,37 Moreover, given that light smokers are disproportionately more likely to be racial/ethnic minorities, continued reliance on these cutoffs may inadvertently contribute to health disparities.38,39 This is particularly unfortunate given our analysis suggests the scientific benefits of using these cutoffs is likely minimal, given their very modest association with the constructs of interest. Even worse, cutoff selection appears to have been arbitrary or driven by convention, suggesting the specific cutoffs used likely failed to optimize whatever benefits could be realized. The present study certainly has some limitations. Foremost, findings are derived from national survey data and thus limitations inherent to survey methodology are present (e.g. inability to accurately self-report, bias attributable to retrospective reporting). Yet the lack of clinical and laboratory data that can rigorously address this topic is the very problem we seek to address. Only by opening up clinical and laboratory studies to the full range of smoking rates can we definitively determine the implications for doing so and continued evaluation of this issue may allow for more nuanced inclusion decisions over time. Furthermore, we only assessed daily smokers in these analyses due to the heterogeneous patterns and challenges to quantifying smoking rate among non-daily smokers. Analyses were conducted on adult smokers in the United States, and researchers are cautioned not to assume these necessarily extend to adolescents or smokers in other nations. Perhaps most notably, these findings only assess the presence/absence of tobacco use disorder, nicotine withdrawal symptoms or a history of failed quit attempts and cannot address other individual symptoms or symptom severity. It remains possible that additional clinically-relevant variables not assessed here (e.g. likelihood of benefitting from intervention, motivation to quit) would exhibit a stronger relationship with CPD. Similarly, alternative methods of assessing the constructs of interest (e.g. continuous measures of withdrawal severity, number of failed quit attempts) could also show stronger relationships with CPD. Both of these issues warrant further exploration. Early research contrasting groups using smoking rate cutoffs rarely seen in modern literature (e.g. ≥ 35 CPD) did find substantial differences in dependence level and withdrawal severity as a function of smoking rate.40,41 However, more recent studies have sometimes failed to find consistent differences between light and moderate-heavy smokers in withdrawal severity.42 Regardless, the potential existence of modest group differences in symptom severity seems a poor rationale for using CPD as a proxy variable to determine study inclusion. Researchers wishing to restrict their samples to smokers who meet formal criteria for tobacco use disorder, those who experience severe withdrawal or those likely to difficulty quitting would be far better served by assessing these constructs directly in lieu of relying on an arbitrary smoking rate cutoff for this purpose. Lastly, as we note above, data collection for the NESARC-III took place from 2012–2013. Both smoking rates and the tobacco product marketplace have continued to evolve during the intervening period. However, major changes during this time (e.g. continued reductions in smoking rate, changes in tobacco control policies, proliferation of electronic cigarettes) would likely only further suppress the relationship between CPD and clinical variables if any impact was found. Despite this, we believe continued research on this issue is vital. Not only because the nature of these relationships is likely to evolve along with tobacco control policies, but also to identify subgroups (e.g. individuals with psychiatric or medical comorbidities, other vulnerable populations) where these relationships may differ.
5. CONCLUSIONS
We do not believe the use of smoking rate cutoffs is necessarily inappropriate in all cases. However, we do believe their use has become reflexive. It is vital we question our assumptions in such instances, particularly with regards to such a fundamental matter as what population we wish to study. This concern could extend equally to other common inclusion/exclusion criteria. In sum, we believe the scientific community would be best served if researchers began to give pause and reflect on the appropriateness of utilizing CPD cutoffs in their work and consider alternatives. For example, researchers could require participants meet formal criteria for dependence or exceed certain thresholds on dependence measures for enrollment, select only participants with a history of failed quit attempts for intensive interventions, or assess the severity of nicotine withdrawal versus inferring its presence based on a CPD cutoff. When used, researchers should explicitly state justification for doing so and rationale for the proposed cutoff. The data presented here can help identify the optimal cut point when the desire is to restrict the population to individuals who meet criteria for tobacco use disorder, experience nicotine withdrawal or have difficulty quitting, though we emphasize that our approach is only one of many viable methods for identifying a defensible cutoff. Regardless, we hope this manuscript will draw sufficient attention to the issue that a greater number of researchers will open their trials and laboratory studies to the wider population of smokers.
HIGHLIGHTS.
Cigarettes per day (CPD) cutoffs are common in clinical and laboratory smoking research
Cigarettes per day is only weakly related to dependence, withdrawal and difficulty quitting
Strength of these relationships is weak regardless of sex, race/ethnicity and SES
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
CONFLICT OF INTEREST
All authors declare they have no conflicts of interest.
REFERENCES
- 1.Shiffman S. Light and intermittent smokers: background and perspective. Nicotine Tob Res. 2009; 11(2): 122–125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schane RE, Ling PM, Glantz SA. Health effects of light and intermittent smoking: a review. Circulation. 2010; 121(13): 1518–1522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Inoue-Choi M, Liao LM, Reyes-Guzman C, Hartge P, Caporaso N, Freedman ND. Association ofLong- term, Low-Intensity Smoking With All-Cause and Cause-Specific Mortality in the National Institutes of Health-AARP Diet and Health Study. JAMA Intern Med. 2017;177(1):87–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Okuyemi KS, Harris KJ, Scheibmeir M, Choi WS, Powell J, Ahluwalia JS. Light smokers: issues and recommendations. Nicotine & Tobacco Research. 2002;4(Suppl_2):S103–S112. [DOI] [PubMed] [Google Scholar]
- 5.Ni K, Wang B, Link A, Sherman S. Does smoking intensity predict cessation rates? A study oflight- intermittent, light-daily, and heavy smokers enrolled in two telephone-based counseling interventions. Nicotine Tob Res. 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Webb Hooper M, Asfar T, Unrod M, et al. Reasons for Exclusion from a Smoking Cessation Trial: An Analysis by Race/Ethnicity. EthnDis. 2019;29(1):23–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fagan P, Rigotti NA. Light and intermittent smoking: the road less traveled. Nicotine Tob Res. 2009; 11(2): 107–110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Reyes-Guzman CM, Pfeiffer RM, Lubin J, et al. Determinants of Light and Intermittent Smoking in the United States: Results from Three Pooled National Health Surveys. Cancer Epidemiol Biomarkers Prev. 2017;26(2):228–239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Goodwin RD, Wall MM, Gbedemah M, et al. Trends in cigarette consumption and time to first cigarette on awakening from 2002 to 2015 in the USA: new insights into the ongoing tobacco epidemic. Tob Control. 2018;27(4):379–384. [DOI] [PubMed] [Google Scholar]
- 10.Blanco L, Nydegger LA, Sakuma KL, Tong EK, White MM, Trinidad DR. Increases in light and intermittent smoking among Asian Americans and non-Hispanic Whites. Nicotine Tob Res. 2014; 16(6): 904–908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dierker LC, Donny E, Tiffany S, et al. The association between cigarette smoking and DSM-IV nicotine dependence among first year college students. Drug Alcohol Depend. 2007;86(2–3): 106–114. [DOI] [PubMed] [Google Scholar]
- 12.Donny EC, Dierker LC. The absence of DSM-IV nicotine dependence in moderate-to-heavy daily smokers. Drug Alcohol Depend. 2007;89(1): 93–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dierker L, Donny E. The role of psychiatric disorders in the relationship between cigarette smoking and DSM-IV nicotine dependence among young adults. Nicotine Tob Res. 2008;10(3):439–446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hitsman B, Papandonatos GD, McChargue DE, et al. Past major depression and smoking cessation outcome: a systematic review and meta-analysis update. Addiction. 2013;108(2):294–306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pomerleau OF, Pomerleau CS, Mehringer AM, Snedecor SM, Ninowski R, Sen A. Nicotine dependence, depression, and gender: characterizing phenotypes based on withdrawal discomfort, response to smoking, and ability to abstain. Nicotine Tob Res. 2005;7(1):91–102. [DOI] [PubMed] [Google Scholar]
- 16.Hendricks PS, Prochaska JJ, Humfleet GL, Hall SM. Evaluating the validities of different DSM–IV-based conceptual constructs oftobacco dependence. Addiction. 2008; 103(7):1215–1223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Heatherton TF, Kozlowski LT, Frecker RC, Fagerstrom KO. The Fagerstrom Test for Nicotine Dependence: a revision of the Fagerstrom Tolerance Questionnaire. Br J Addict. 1991;86(9): 1119–1127. [DOI] [PubMed] [Google Scholar]
- 18.Grant B, Amsbary M, Chu A, et al. Source and Accuracy Statement: National Epidemiologic Survey on Alcohol and Related Conditions-III (NESARC-III). Rockville, MD: National Institute on Alcohol Abuse and Alcoholism; 2014. [Google Scholar]
- 19.Hasin DS, Greenstein E, Aivadyan C, et al. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-5 (AUDADIS-5): procedural validity of substance use disorders modules through clinical re-appraisal in a general population sample. Drug and alcohol dependence. 2015;148:40–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Grant BF, Goldstein RB, Smith SM, et al. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-5 (AUDADIS-5): reliability of substance use and psychiatric disorder modules in a general population sample. Drug and alcohol dependence. 2015;148:27–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Youden WJ. Index for rating diagnostic tests. Cancer. 1950; 3(1): 32–3 5. [DOI] [PubMed] [Google Scholar]
- 22.Liu X Classification accuracy and cut point selection. StatMed. 2012;31(23):2676–2686. [DOI] [PubMed] [Google Scholar]
- 23.Perkins NJ, Schisterman EF. The inconsistency of “optimal” cutpoints obtained using two criteria based on the receiver operating characteristic curve. Am J Epidemiol. 2006;163(7):670–675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.DeLong ER DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics. 1988;44(3):837–845. [PubMed] [Google Scholar]
- 25.Zhu W, Zeng N, W ang N. Sensitivity, specificity, accuracy, associated confidence interval and ROC analysis with practical SAS implementations. NESUG proceedings: health care and life sciences, Baltimore, Maryland. 2010;19:67. [Google Scholar]
- 26.Ben Taleb Z,W ard KD, Asfar T, Jaber R, Bahelah R, Maziak W. Smoking cessation and changes in body mass index findings from the first randomized cessation trial in a low-income country setting. Nicotine & Tobacco Research. 2017; 19(3):351–356. [DOI] [PubMed] [Google Scholar]
- 27.Hansson A, Rasmussen T, Kraiczi H. Single-dose and multiple-dose pharmacokinetics of nicotine 6 mg gum Nicotine & Tobacco Research. 2017;19(4):477–483. [DOI] [PubMed] [Google Scholar]
- 28.Oliver JA, Blank MD, Van Rensburg KJ, MacQueen DA, Brandon TH, Drobes DJ. Nicotine interactions with low-dose alcohol: pharmacological influences on smoking and drinking motivation. J Abnorm Psychol. 2013; 122(4): 1154–1165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Oliver JA, Jentink KG, Drobes DJ, Evans DE. Smokers exhibit biased neural processing of smoking and affective images. Health Psychol. 2016;35(8):866–869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Stevenson JG, Oliver JA, Hallyburton MB, Sweitzer MM, Conklin CA, McClernon FJ. Smoking environment cues reduce ability to resist smoking as measured by a delay to smoking task. AddictBehav. 2017;67:49–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tidey JW, Pacek LR, Koopmeiners JS, et al. Effects of 6-week use of reduced-nicotine content cigarettes in smokers with and without elevated depressive symptoms. Nicotine & Tobacco Research. 2016; 19(1): 59–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hendricks PS, Ditre JW, Drobes DJ, Brandon TH. The early time course of smoking withdrawal effects. Psychopharmacology (Berl). 2006;187(3):385–396. [DOI] [PubMed] [Google Scholar]
- 33.Hendricks PS, Wood SB, Baker MR, Delucchi KL, Hall SM. The Smoking Abstinence Questionnaire: measurement of smokers’ abstinence-related expectancies. Addiction. 2011;106(4):716–728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fish LJ, Peterson BL, Namenek Brouwer RJ, et al. Adherence to nicotine replacement therapy among pregnant smokers. Nicotine & Tobacco Research. 2009; 11 (5):514–518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pollak KI, Oncken CA, Lipkus IM, et al. Nicotine replacement and behavioral therapy for smoking cessation in pregnancy. American journal of preventive medicine. 2007;33(4):297–305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pollak KI, Lyna P, Bilheimer A, et al. A pilot study testing SMS text delivered scheduled gradual reductionto pregnant smokers. Nicotine TobRes. 2013; 15(10): 1773–1776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Fish LJ, Pollak KI, Scheuermann TS, Cox LS, Mathur C, Ahluwalia JS. Comparison of native light daily smokers and light daily smokers who were former heavy smokers. Nicotine Tob Res. 2015; 17(5):546–551. [DOI] [PubMed] [Google Scholar]
- 38.Trinidad DR, Perez-Stable EJ, Emery SL, White MM, Grana RA, Messer KS. Intermittent and light daily smoking across racial/ethnic groups in the United States. Nicotine Tob Res. 2009;11(2):203–210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tong EK, Nguyen T, Vittinghoff E, Perez-Stable EJ. Light and intermittent smoking among California’s Asian Americans. Nicotine & Tobacco Research. 2009;11(2):197–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Killen JD, Fortmann SP, Telch MJ, Newman B. Are heavy smokers different from light smokers? A comparison after 48 hours without cigarettes. JAMA. 1988;260(11):1581–1585. [PubMed] [Google Scholar]
- 41.Cummings KM, Giovino G, Jaen CR, Emrich LJ. Reports of smoking withdrawal symptoms over a 21 day period of abstinence. Addict Behav. 1985; 10(4) :373–381. [DOI] [PubMed] [Google Scholar]
- 42.Reitzel LR, Costello TJ, Mazas CA, et al. Low-level smoking among Spanish-speaking Latino smokers: Relationships with demographics, tobacco dependence, withdrawal, and cessation. Nicotine & Tobacco Research. 2009; 11(2): 178–184. [DOI] [PMC free article] [PubMed] [Google Scholar]