Abstract
Objective:
To explore the clinical efficacy and safety of Qigong in reducing the self-rating depression scale (SDS) and self-rating anxiety scale (SAS) scores of patients with chronic obstructive pulmonary disease (COPD).
Methods:
We searched CNKI, Wan fang, Chongqing VIP, China Biology Medicine disc, PubMed, Cochrane Library, and EMBASE for studies published as of Dec 31, 2018. All randomized controlled trials of Qigong in COPD patients, which met the inclusion criteria were included. The Cochrane bias risk assessment tool was used for literature evaluation. RevMan 5.3 software was used for meta-analysis.
Results:
Six studies (combined n = 415 patients) met the inclusion criteria. Compared with conventional therapy alone, Qigong in combination with conventional therapy significantly improved the following outcome measures: SDS score [mean difference (MD) −3.99, 95% CI (−6.17, −1.82), P < .001, I2 = 69%]; SAS score[MD −4.57, 95% CI (−5.67, −3.48), P < .001, I2 = 15%]; forced expiratory volume in one second/prediction (FEV1% pred) [MD 3.77, 95% CI (0.97,6.58), P < .01, I2 = 0]; forced expiratory volume in one second (FEV1) [MD 0.21, 95% CI (0.13, 0.30), P < .001, I2 = 0%]; forced vital capacity (FVC) [MD 0.28, 95% CI (0.16, 0.40), P < .001, I2 = 0]; 6-minute walk test (6MWT) distance [MD 39.31, 95% CI (18.27, 60.34), P < .001, I2 = 32%]; and St. George's Respiratory Questionnaire (SGRQ) total score [MD −11.42, 95% CI (−21.80, −1.03), P < .05, I2 = 72%].
Conclusion:
Qigong can improve the SDS and SAS scores of COPD patients, and has auxiliary effects on improving lung function, 6MWT distance, and SGRQ score.
Keywords: COPD, meta, Qigong, RCT, SAS, SDS
1. Introduction
Anxiety, depression, and cognitive impairment are common comorbid conditions in patients with chronic obstructive pulmonary disease (COPD).[1] In overseas studies, the prevalence of anxiety among patients with COPD ranged from 6% to 74%, while that of depression ranged from 8% to 80%.[2] Studies conducted in China have reported wide variability in the prevalence rates of anxiety and depression in patients with COPD; in addition, there is considerable underreporting of anxiety and depression among COPD patients in China.[3]
Anxiety/depression was shown to be associated with acute exacerbations of COPD.[4] Presence of depression in COPD patients is associated with frequent exacerbations, high utilization of medical resources, low quality of life, and increased mortality.[5] The overall quality of life of patients with depression was shown to be lower than that of those without depression among COPD patients with forced expiratory volume in one second/prediction (FEV1% pred) >50%; in addition, the quality of life index showed a significant correlation with the severity of depression.[5]
The presence of COPD does not affect the treatment of anxiety/depression.[1] Studies have demonstrated the benefit of physical exercise in ameliorating depression; therefore, the potential impact of pulmonary rehabilitation on the disease should be emphasized.[6,7]
Qigong is an ancient psychosomatic discipline, which is part of Traditional Chinese Medicine.[8] There are hundreds of forms of Qigong exercises developed in China, such as Tai Chi, Liuzijue Qigong, Wuqinxi, Baduanjin, Relaxation Qigong. Qigong has been recognized as a low-cost, easy-to-learn, less side effects “medical” exercise and used to improve physical and psychological health and combat diseases. A large number of studies have confirmed the safety and effectiveness of Qigong in arthritis, anxiety, depression, COPD, etc, but the current understanding of its adverse events is still fragmentary.[9–11] The National Center for Complementary and Integrative Health identified that there may be potential risks if Qigong is learned from a video or book instead of studied with a qualified instructor.[11] For example, muscular and joint pain may be exacerbated instead of relieved without appropriate instruction if Tai Chi is not performed properly. A systematic review about the safety of Tai Chi also confirmed that Tai Chi is unlikely to cause serious adverse events, but may be associated with mild musculoskeletal pain.[12] Three meta-analyses showed that Tai Chi can improve the 6-minute walk test (6MWT) and FEV1% pred of patients with COPD; however, the effect of Tai Chi on the symptoms and quality of life of patients with COPD remains controversial.[13–15] Qigong, including Tai Chi, Liuzijue Qigong, Wuqinxi, Baduanjin, Relaxation Qigong, etc, has been shown to improve lung function, activity endurance, and ability of COPD patients to perform activities of daily living.[16–19] However, evidence pertaining to the effect of Qigong on the anxiety scores or depression scores of COPD patients has been largely inconsistent. While some studies suggest that Qigong can improve anxiety and depression scores, symptoms, and quality of life of COPD patients,[20–25] others have drawn the opposite conclusion.[26,27] In this study, we performed a systematic evaluation and meta-analysis of randomized controlled trials that investigated the effects of Qigong on the self-rating depression scale (SDS) and self-rating anxiety scale (SAS) scores of COPD patients. The objective was to synthesize the available evidence pertaining to the efficacy of Qigong in improving the SDS and SAS scores of COPD patients.
2. Research methods
This meta-analysis was conducted in accordance with Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA), and the literature search and screening program was pre-established.
2.1. Search Strategy
The followed databases were searched to retrieve relevant articles published in English and Chinese language as of Dec 31, 2018: CNKI, Wan fang, Chongqing VIP, China Biology Medicine disc, PubMed, Cochrane Library, and EMBASE. The following key words or combinations were used to retrieve studies: “chronic obstructive pulmonary disease” or “COPD,” merging “SDS” or “SAS,” merging “Qigong” (including “Qi Gong,” “Chi Kung,” “Tai Chi,” “Taichi,” “Tai Ji,” “Taiji,” “Mind-body exercise,” “Liuzijue Qigong,” “Wuqinxi,” “Baduanjin,” “Relaxation Qigong”). In addition, the reference lists of relevant reviews and meta-analyses were manually screened to avoid any omissions.
2.2. Inclusion and exclusion criteria
Inclusion criteria: first, COPD patients; second, treatment group received Qigong (including Tai Chi, Mind-body exercise, Liuzijue Qigong, Wuqinxi, Baduanjin, Relaxation Qigong, etc) or Qigong in combination with conventional treatment; third, the control group received only conventional treatment or no treatment; fourth, Main outcomes: SAS and SDS scores. Secondary outcomes: lung function, 6MWT, modified Medical British Research Council (mMRC), and St. George's respiratory questionnaire (SGRQ) scores. Only those studies that reported at least one of the main outcomes were included; and fifth, study type: we searched all types of studies, but only RCT was selected.
Exclusion criteria: first, obvious inconsistency or poor face validity of the reported data and second, studies with incomplete data or for which comprehensive information could not be obtained from the original author.
2.3. Data extraction and quality assessment
Two researchers independently performed literature screening and data extraction. Disagreements, if any, were resolved by consensus or by a third co-author (Du Weisha). The Cochrane Collaboration's risk of bias (ROB) bias risk assessment tool was used for quality evaluation, and each item was rated as high risk, low risk, or unclear.
2.4. Observation indicators
Data pertaining to the following variables were included: researcher information (name, publication time, type of study); research information (sample size, mean age, intervention and control measures, randomized scheme, allocation hiding, blinding method, drop-off, loss of interview, intention analysis, outcome indicators).
2.5. Publication bias assessment
If there were more than ten studies included in the meta-analysis, the data were evaluated for publication bias.[28] Publication bias was assessed by viewing the symmetry of the funnel plot and using the Begg[29] rank correlation method and the Harbord[30] modified linear regression method.
2.6. Data analysis
RevMan 5.3 software was used for statistical analysis. Statistical heterogeneity among studies was evaluated by I2. In the event of no significant heterogeneity (P > .1 and I2 < 50%), the fixed effect model was used for meta-analysis. In case of statistically significant heterogeneity (P < .1 and I2 > 50%), the random effect model was used for meta-analysis. Continuous variables were evaluated by mean (MD). Results are expressed with 95% confidence intervals (CIs). P < .05 was considered as statistically significant.
3. Results
3.1. Literature Search
A total of 1063 articles were retrieved on database search. After review of titles and abstracts, 1034 were eliminated for various reasons (Fig. 1). Full-text of the remaining 29 articles were reviewed, after which 23 articles were excluded and 6 articles[22–27] were included. Figure 1 shows a schematic illustration of the literature search and study selection criteria.
Figure 1.
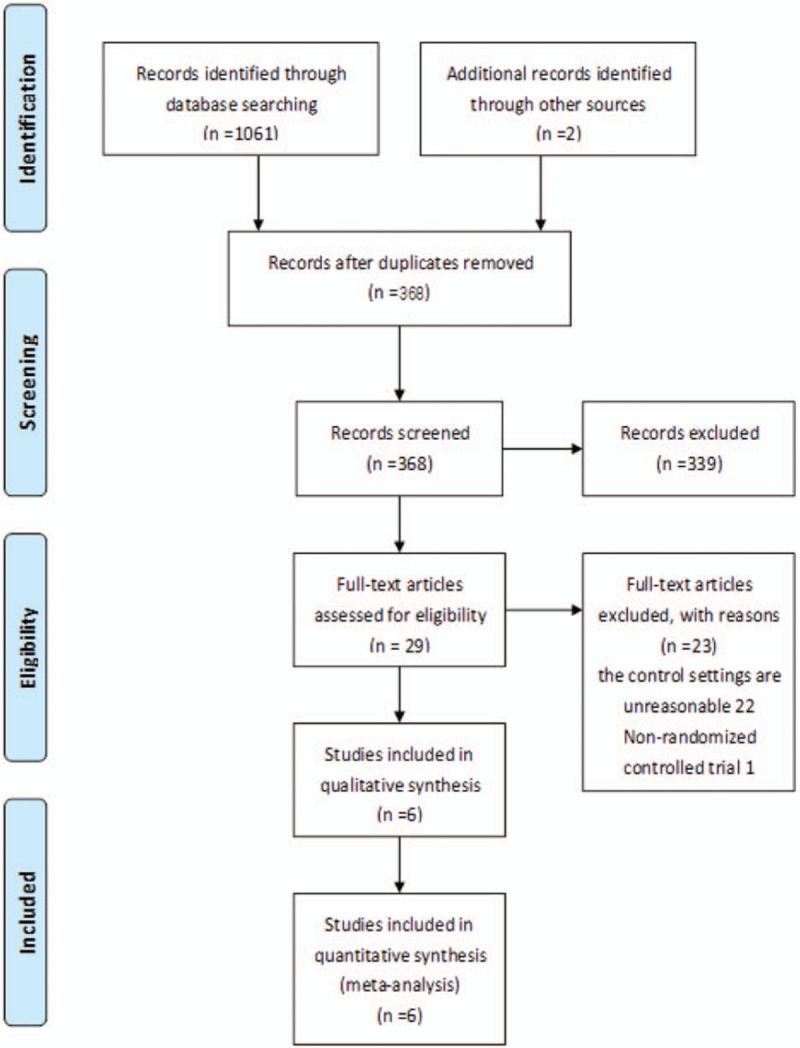
Schematic illustration of literature search and study selection criteria.
3.2. Basic characteristics of the included studies
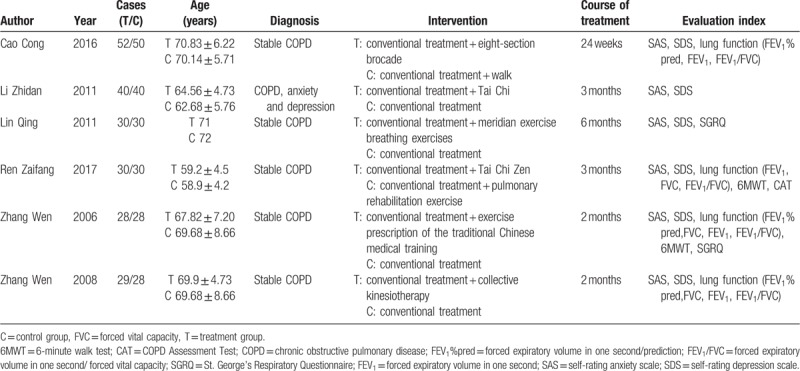
This study included 6 randomized controlled trials with a combined study population of 415 subjects (209 subjects in the treatment group and 206 subjects in the control group); the average number of subjects per group was 34. Average age of subjects was 68 years. None of the included studies had specified the methodology used to determine the sample size. The characteristics of the included studies are shown in Table 1.
Table 1.
Characteristics of the included studies.
3.3. Quality evaluation
The studies were evaluated by Cochrane bias risk assessment. The risk of bias in the selected studies is illustrated in Figures 2 and 3.
Figure 2.
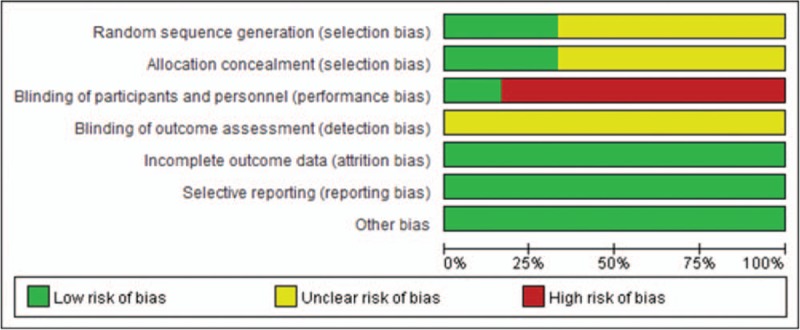
Risk bias diagram.
Figure 3.

Risk of bias summary.
3.4. Evaluation of the effect of Qigong on SDS and SAS scores of COPD patients
3.4.1. Evaluation of the effect of Qigong on SDS scores
Six studies had reported posttreatment SDS scores. In four studies,[22–25] Qigong combined with conventional treatment improved the SDS scores of COPD patients, while opposite results were observed in the other two studies.[26,27] Owing to significant heterogeneity between the samples, the random effect model was used for analysis. Meta-analysis showed that compared with conventional therapy alone, Qigong in combination with conventional therapy significantly improved the SDS score of COPD patients [MD −3.99, 95% CI (−6.17, −1.82), P < .001, I2 = 69%] (Fig. 4). Sensitivity analysis suggested that the study by Li[22] was the main contributors to heterogeneity. Even after excluding the results of these studies from the analysis, Qigong in combination with conventional treatment significantly improved the SDS scores of COPD patients as compared to that in the control group.
Figure 4.
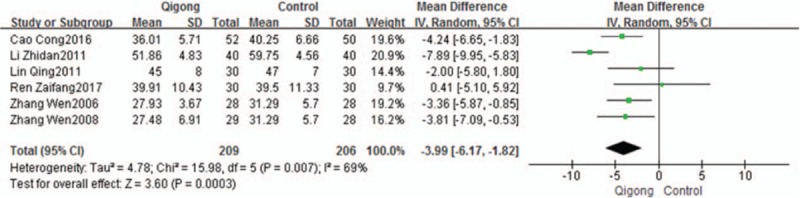
Evaluation of the effect of Qigong on SDS scores of COPD patients.
3.4.2. Evaluation of the effect of Qigong on SAS scores of COPD patients
Six studies had reported posttreatment anxiety scores. In five studies,[22–26] Qigong in combination with conventional treatment significantly improved SAS scores of COPD patients, while one study[27] showed the opposite results. Meta-analysis showed that compared with conventional therapy, Qigong in combination with conventional therapy significantly improved the SAS scores of COPD patients [MD −4.57, 95% CI (−5.67,−3.46), P < .001, I2 = 15%] (Fig. 5).
Figure 5.
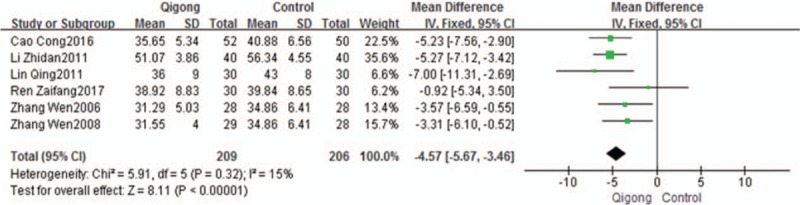
Evaluation of the effect of Qigong on SAS scores of COPD patients.
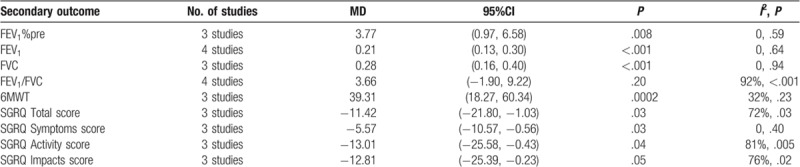
3.5. Evaluation of the effect of Qigong on lung function, 6MWT and SGRQ
The Evaluation of the effect of Qigong on lung function, 6MWT and SGRQ are shown in Table 2.
Table 2.
Evaluation of the effect of Qigong on lung function, 6MWT, and SGRQ.
4. Discussion
Our results showed that Qigong in combination with conventional treatment improved the SDS and SAS scores of COPD patients, improved FEV1% pre, FEV1, FVC, 6MWT, SGRQ total score, SGRQ symptom score, SGRQ activity score.
The role of Qigong in anxiety/depression and COPD has been demonstrated. Studies have shown its beneficial effects both in patients with anxiety/depression as well as in patients with COPD, with minimal side effects. Qigong may be helpful in the treatment and management of depression, anxiety, and related mood disorders.[31,32] Qigong may be an effective and safe nonpharmacological therapy for preventing and managing mood disorders.[31] Studies have shown that acupuncture and Qigong can improve the quality of sleep and life and reduce depression scores of patients with depression.[33] Meditation exercise (Tai Chi, Qigong, Yoga) can improve the 6MWT distance, FEV1, FEV1%pred, and enhance physical activity in COPD patients.[34] Liuzijue exercise has been shown to improve respiratory muscle strength and peripheral skeletal muscle function in patients with COPD, and to enhance upper limb endurance and strength, and lower limb endurance.[35] However, the effect of Qigong on anxiety and depression scores of COPD patients with or without anxiety and depression is not clear. This study found that, Qigong can effectively reduce the SDS and SAS scores of COPD patients. We observed considerable heterogeneity among the studies included in the meta-analysis of the effect of Qigong on SDS scores of COPD patients, which is likely attributable to the enrollment of patients with or without anxiety and depression.
This study shows that Qigong can improve lung function of COPD patients, including FEV1%pre, FEV1, FVC, but not FEV1/FVC. Three of the studies reported posttreatment FVC. Meta-analysis found that Qigong combined with conventional treatment may improve FVC of COPD patients compared with conventional treatment (MD 0.28, 95% CI [0.16, 0.40], P < .001, I2 = 0). In a 6-month-long study conducted in China, Qigong did not improve the FVC of COPD patients,[36] while another study in China found the opposite results.[37] This inconsistency may be related to the sample size or the study group; further high-quality study with a large sample is required to obtain more definitive evidence.
Out of the four studies that reported posttreatment FEV1/FVC, two studies[23,27] reported that Qigong combined with conventional treatment could improve FEV1/FVC, while two studies[24,25] presented the opposite conclusion. Meta-analysis found significant heterogeneity among these studies, and the random effects model was used for the meta-analysis. Compared with conventional treatment, Qigong combined with conventional therapy did not improve FEV1/FVC in COPD patients [MD 3.66, 95% CI (−1.90,9.22), P = .2, I2 = 92%]. Sensitivity analysis revealed that the heterogeneity was mainly contributed by the study by Ren et al;[27] but after exclusion of this study from the meta-analysis, Qigong combined with conventional therapy was not improve FEV1/FVC [MD 1.94, 95% CI (−0.33,4.21), P = .34, I2 = 8%]. The reason may be related to the sample size, which calls for a high-quality study with a large sample size.
Only one included study[27] mentioned adverse events, while other five trials did not. Due to insufficient information regarding the safety of Qigong for COPD, more studies will be needed to confirm its safety.
4.1. Study limitations
In this study, the lung function of COPD patients was concentrated between 30%≤FEV1%pred < 80%, which suggests that patients with moderate to severe obstructive ventilatory dysfunction patients can benefit from Qigong. The effect of Qigong in patients with FVE1%pred>80% and <30% is not clear. Different grades of lung function or different stages may have different responses to treatment. For a more comprehensive evaluation of the responsiveness of different COPD patients to Qigong, future studies should stratify patients according to clinical status (stable and acute exacerbation) or according to the pulmonary function (mild, moderate, severe, and very severe COPD).
Among the COPD patients enrolled in this study, some of them had a definitive diagnosis of anxiety and depression. The order of onset of COPD and anxiety/depression is not clear. However, whether combined with anxiety/depression, Qigong can effectively reduce the SDS and SAS scores of COPD patients.
There are many tools used to evaluate anxiety and depression. In addition to the SDS and SAS scores used in this study, there are general hospital anxiety and depression (HAD) scale or quality of life (QOL) or Hamilton Depression Scale (HAMD) and Hamilton Anxiety Scale (HAMA). Some studies reported the effect of Qigong on HAD or QOL or HAMA, HAMD scores in COPD patients.[20,21,36] However, due to the lack of relevant clinical research, meta-analysis of relevant indicators has not been carried out. It is also suggested that future clinical trials should refer to international standards or recognized indicators for efficacy evaluation, so that the results can be easily evaluated.
It is difficult to exclude the placebo effect because Qigong therapy is difficult to blind patients and researchers.
The study cycle may have an impact on the outcome. The study period included in this study ranges from 2 to 6 months, which may have some impact on the conclusion of the study.
5. Conclusion
Qigong can improve the SDS and SAS scores of COPD patients, and has auxiliary effect on improving lung function, 6MWT distance, and SGRQ scores.
Author contributions
Conceptualization: Jian-jun Wu, Liang-duo Jiang, Jin-min Liu, Mei Han.
Supervision: Jian-jun Wu, Rui-feng Jin, Hui-yong Yu.
Visualization: Jian-jun Wu, Ying-xue Zhang.
Writing – original draft: Jian-jun Wu, Ying-xue Zhang, Wei-sha Du.
Writing – review & editing: Jian-jun Wu, Rui-feng Jin, Hui-yong Yu.
Footnotes
Abbreviations: 6MWT = 6-minute walk test, CIs = confidence intervals, COPD = chronic obstructive pulmonary disease, FEV1 = forced expiratory volume in one second, FEV1% pred = forced expiratory volume in one second/prediction, FVC = forced vital capacity, MD = mean, mMRC = modified Medical British Research Council, SAS = self-rating anxiety scale, SDS = self-rating depression scale, SGRQ = St. George's Respiratory Questionnaire.
The work was supported by Beijing Municipal Natural Science Foundation (Project No. 7182100).
The authors have no conflicts of interest to disclose.
References
- [1].GOLD. Global Strategy for the Diagnosis, Management and Prevention of COPD, Global Initiative for Chronic Obstructive Lung Disease (GOLD) 2018; 2018 (https://goldcoped.org/ Accessed July 17, 2018). [Google Scholar]
- [2].Graat-Verboom L, Smeenk FW, van den Borne BE, et al. Progression of osteoporosis in patients with COPD: a 3-year follow up study. Respir Med 2012;106:861–70. [DOI] [PubMed] [Google Scholar]
- [3].Li X, Zhang Y, Yu C, et al. Risk factors and comorbidities of hospitalized patients with chronic obstructive pulmonary disease. Soft Sci Health 2017;31:58–61. [Google Scholar]
- [4].Underner M, Cuvelier A, Peiffer G, et al. The influence of anxiety and depression on COPD exacerbations. Rev Mal Respir 2018;35:604–25. [DOI] [PubMed] [Google Scholar]
- [5].Lee JH, Park MA, Park MJ, et al. Clinical characteristics and related risk factors of depression in patients with early COPD. Int J Chron Obstruct Pulmon Dis 2018;15:1583–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Bolton CE, Singh SJ, Walker PP. Commentary: the British Thoracic Society guideline on pulmonary rehabilitation in adults. Thorax 2013;68:887–8. [DOI] [PubMed] [Google Scholar]
- [7].Coventry PA, Bower P, Keyworth C, et al. The effect of complex interventions on depression and anxiety in chronic obstructive pulmonary disease: systematic review and meta-analysis. PLoS One 2013;8:e60532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Guo Y, Xu M, Ji M, et al. The effect of Imaginary Working Qigong on the psychological well-being of college students: study protocol for a randomized controlled trial. Medicine (Baltimore) 2018;97:e13043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Oh B, Yeung A, Klein P, et al. Accreditation standard guideline initiative for Tai Chi and Qigong instructors and training institutions. Medicines (Basel) 2018;5:51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Baumgarden J, Klein P, Picard G. Qigong and a tale of two back complaints. Medicines (Basel) 2018;5:60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].NCCIH Tai Chi and Qi Gong: In Depth. Available at: https://nccih.nih.gov/health/taichi/introduction.htm [access date January 1, 2018)]. [Google Scholar]
- [12].Wayne PM, Berkowitz DL, Litrownik DE, et al. What do we really know about the safety of Tai Chi? A systematic review of adverse event reports in randomized trials. Arch Phys Med Rehabil 2014;95:2470–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Wu W, Liu X, Wang L, et al. Effects of Tai Chi on exercise capacity and health-related quality of life in patients with chronic obstructive pulmonary disease: a systematic review and meta-analysis. Int J Chron Obstruct Pulmon Dis 2014;9:1253–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Luo X, Zhang J, Castelberg R, et al. The effects of traditional Chinese exercise in patients with chronic obstructive pulmonary disease: a meta-analysis. PLoS One 2016;11:e0161564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Ngai SP, Jones AY, Tam WW. Tai Chi for chronic obstructive pulmonary disease (COPD). Cochrane Database Syst Rev 2016;6:CD009953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Lorenc AB, Wang Y, Madge SL, et al. Meditative movement for respiratory function: a systematic review. Respir Care 2014;59:427–40. [DOI] [PubMed] [Google Scholar]
- [17].Ding M, Zhang W, Li K, et al. Effectiveness of T’ai Chi and Qigong on chronic obstructive pulmonary disease: a systematic review and meta-analysis. J Altern Complement Med 2014;20:79–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Ng BH, Tsang HW, Ng BF, et al. Traditional Chinese exercises for pulmonary rehabilitation: evidence from a systematic review. J Cardiopulm Rehabil Prev 2013;34:367–77. [DOI] [PubMed] [Google Scholar]
- [19].Wang L, Wu W, Liu X, et al. Rehabilitative effect of traditional fitness method on patients with stable chronic obstructive pulmonary disease: a meta analysis. Chin J Rehabil Med 2014;29:957–62. [Google Scholar]
- [20].Wang Z, Gu C, Huang Y, et al. Effect of minimally invasive thread-embedding at acupoints in patients with moderate to severe chronic obstructive pulmonary disease in stable phase: a randomized controlled clinical study. Shanghai J Tradit Chin Med 2015;49:38–42. [Google Scholar]
- [21].Wang Z, Tang J, Huang H, et al. A multi-center randomized controlled clinical study on the clinical efficacy of strengthened “Liu Zi Jue” on COPD in stable phrase. Shanghai J Tradit Chin Med 2014;48:51–4. [Google Scholar]
- [22].Li Z. Clinical effect of Taijiquan on relieving depression and anxiety of chronic obstructive pulmonary disease. Chin J Aesthetic Med 2011;20(s6):129–30. [Google Scholar]
- [23].Cao C, Guo X, Chen N, et al. Research of effects of eight-section brocade TCM on treating anxiety and depression in the elderly patients with lung-spleen Qi deficiency in stable period of COPD. J Liaoning Univ TCM 2016;18:120–3. [Google Scholar]
- [24].Zhang W. Exercise prescription of traditional Chinese medical training for patients with stable COPD. ShangHai: Fudan University; 2006. [Google Scholar]
- [25].Zhang W, Chen W, Jin X, et al. The effects of collective kinesiotherapy on anxiety and depression in COPD patients at stable stage. Chin J Rehabil Med 2008;23:732–4. [Google Scholar]
- [26].Lin Q, Cao D, Li R, et al. Effect of meridian exercise and breathing exercises on quality of life in patients with chronic obstructive pulmonary disease. Clin J Tradit Chin Med 2011;23:774–5. [Google Scholar]
- [27].Ren Z, Zhang X, Hou G, et al. Effects of Tai Chi Zen on exercise ability and quality of life in chronic obstructive pulmonary disease. China J Tradit Chin Med Pharm 2017;32:3507–10. [Google Scholar]
- [28].Sterne JA, Sutton AJ, Ioannidis JP, et al. Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ 2011;343:d4002. [DOI] [PubMed] [Google Scholar]
- [29].Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics 1994;50:1088–101. [PubMed] [Google Scholar]
- [30].Harbord RM, Egger M, Sterne JA. A modified test for small-study effects in meta-analyses of controlled trials with binary endpoints. Stat Med 2006;25:3443–57. [DOI] [PubMed] [Google Scholar]
- [31].Osypiuk K, Thompson E, Wayne PM. Can Tai Chi and Qigong postures shape our mood? Toward an embodied cognition framework for mind-body research. Front Hum Neurosci 2018;12:174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Chan JS, Ho RT, Chung KF, et al. Qigong exercise alleviates fatigue, anxiety, and depressive symptoms, improves sleep quality, and shortens sleep latency in persons with chronic fatigue syndrome-like illness. Evid Based Complement Alternat Med 2014;2014:106048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Cheng X, Wang DM, Chen X, et al. Health Qigong Wuqinxi improves hydrogen proton magnetic resonance spectra in prefrontal cortex and hippocampus in college students with mild depression. Nan Fang Yi Ke Da Xue Xue Bao 2016;36:1468–76. [PubMed] [Google Scholar]
- [34].Wu LL, Lin ZK, Weng HD, et al. Effectiveness of meditative movement on COPD: a systematic review and meta-analysis. Int J Chron Obstruct Pulmon Dis 2018;13:1239–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Wu LL, Lin ZK, Weng HD, et al. Effectiveness of water-based Liuzijue exercise on respiratory muscle strength and peripheral skeletal muscle function in patients with COPD. Int J Chron Obstruct Pulmon Dis 2018;13:1713–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Liu XD, Jin HZ, Ng BHP, et al. Therapeutic effects of Qigong in patients with COPD: a randomized controlled trial. Hong Kong J Occup Ther 2012;22:38–46. [Google Scholar]
- [37].Chan AW, Lee A, Suen LK, et al. Tai Chi Qigong improves lung functions and activity tolerance in COPD clients: a single blind, randomized controlled trial. Complementary Ther Med 2011;19:3–11. [DOI] [PubMed] [Google Scholar]


