Abstract
Surgical site infection (SSI) is a well-known complication in older adults. However, there have been no studies on SSI after gastrectomy in older adults. Therefore, we aimed to investigate the incidence, risk factors, and outcomes of SSIs after gastrectomy in older adults.
We performed a retrospective cohort study of older adults, aged 65 years or older, who underwent gastrectomy between January 2015 and December 2015 at the Severance Hospital in Seoul, Korea. The incidence and outcomes of SSIs after gastrectomy were evaluated, and the risk factors for SSI were identified using multivariate analyses.
We identified 353 older adults who underwent gastrectomy. Of these, 25 patients (7.1%) developed an SSI. Multivariate analysis indicated that open surgery (odds ratio, 2.71; 95% confidence interval, 1.13–6.51; P = .03) and a longer operation time (odds ratio, 1.01; 95% confidence interval, 1.00–1.01; P = .04) were independent risk factors for SSI after gastrectomy. In the SSI group, the incidence of postoperative fever (84.0% vs 51.8%; P < .001), length of postoperative hospital stay (13 days vs 6 days; P < .001), and re-admission rates within 30 days postoperatively (32.0% vs 3.4%; P < .001) were significantly higher than those in the non-SSI group.
The risk factors for SSI in older adults after gastrectomy were open surgery and a longer operation time. When an SSI occurred, the postoperative hospital stay was prolonged and the chances of having a postoperative fever and being re-admitted within 30 days increased.
Keywords: gastrectomy, gastric cancer, gastric cancer surgery, older adults, surgical site infection
1. Introduction
According to the worldwide data for 2015, gastric cancer is the fifth most common malignancy in the world and the third leading cause of cancer-related death.[1] Gastrectomy is one of the main treatment methods for gastric cancer and among the most common surgical procedures carried out in South Korea. Although advances in surgical techniques and improvements in surgical devices have resulted in reduced mortality after gastrectomy, postoperative complications remain a clinically significant problem.[2]
One of the most common postoperative complications is surgical site infection (SSI). SSI is associated with prolonged hospitalization, decreased quality of life for patients, increased treatment costs, and increased mortality.[3–5] In older adults, 11% of all nosocomial infections are SSIs.[6] Moreover, the number of older adults is steadily increasing; according to 1 study, it is expected to double by 2030.[7] The importance of studying SSIs in older adults is related not only to the increase in the number of older adults, but also to the fact that older adults have various comorbidities, such as diabetes mellitus, poor nutrition, chronic hypoalbuminemia, and decreased body fat, which are known predictors of SSIs.[8] Nevertheless, despite the frequency of SSIs and the adverse effects it has on older adults’ clinical outcomes, there are limited data pertaining to the risk factors for SSI in older adults.[9] Furthermore, to the best of our knowledge, there have been no studies on the incidence and risk factors of SSIs after gastric cancer surgery in older adults. Therefore, it is important to study the incidence and risk factors of SSIs after gastric cancer surgery in the population of older adults with a high incidence of gastric cancer in South Korea. The purpose of this study was to investigate the incidence, risk factors, and outcomes of SSIs after gastric cancer surgery in older adults.
2. Materials and methods
2.1. Study design and population
A retrospective cohort study was conducted to investigate the incidence and risk factors for SSIs in older adults with gastric cancer who underwent gastrectomy. Between January 1, 2015 and December 31, 2015, a total of 1067 patients underwent gastric cancer surgery in the Severance Hospital in Seoul, Korea. We excluded the patients who required an emergency surgery, those who underwent an additional surgery for another disease at the time of gastrectomy, as well as the patients with active infections, massive ascites, mental disease, and severe cardiopulmonary disease. Finally, we enrolled 353 patients, aged 65 years or older, who underwent gastric cancer surgery and did not qualify for exclusion. The patients of age 65 years or older were considered older adults based on the age criteria established in the Journal of the American Geriatrics Society.[10] The study was approved by the Institutional Review Board (IRB) of Yonsei University Health System Clinical Trial Center (4-2017-1252). Since the study was retrospective and the study subjects were anonymized, the IRB waived the requirement for patients’ written consent.
2.2. Definition of SSI
Surgeons checked for SSIs every day during the hospital stay and at every outpatient clinic visit until 30 days post-surgery.[11] A SSI was defined based on the 1999 Centers for Disease Control and Prevention National Nosocomial Infection Surveillance System manual.[3] The definition included an incisional SSI and organ/space SSI. Incisional SSI was diagnosed if at least 1 of the following criteria was met:
-
1.
purulent drainage from the incision site, with or without laboratory confirmation of an infection;
-
2.
organisms isolated from an aseptically obtained culture of fluid or tissue from the incision;
-
3.
at least 1 sign or symptom of an infection (pain, tenderness, localized swelling, redness, or local heat), in addition to the incision being deliberately opened by the surgeon, unless the incision was culture negative; or
-
4.
diagnosis of incisional SSI by the surgeon or attending physician.[11]
Briefly, incisional SSI was diagnosed when the infection was confined to the incisional site, involving the skin, subcutaneous tissue, fascial, and muscular layers.[12] Organ/space SSI was diagnosed in the presence of at least 1 of the following criteria:
-
(1)
purulent drainage from a drain placed through a stab wound into an organ/space;
-
(2)
organisms isolated from an aseptically obtained culture of fluid or tissue in the organ/space;
-
(3)
an abscess or other evidence of an infection involving the organ/space that is found upon examination, during reoperation, or by histopathologic or radiologic examination; or
-
(4)
diagnosis of organ/space SSI made by a surgeon or an attending physician.
2.3. Surgical procedures and perioperative management
The typical surgical procedures for open, laparoscopic, and robotic gastrectomy have been previously described in detail.[13–16] First-generation cephalosporins were administered to all study population within an hour of skin incision according to Centers for Disease Control guidelines.[17] Most surgical procedures were performed in a similar manner among the surgeons. The da Vinci System (Intuitive Surgical, Sunnyvale, CA) was used to perform robotic surgeries. Depending on the location of the tumors, a total or partial gastrectomy was performed. Lymph node dissection, D1, D1+, or D2 was performed according to the 2014 Japanese gastric cancer treatment guidelines.[18] The reconstruction type (Roux-en-Y esophagojejunostomy, gastroduodenostomy, gastrojejunostomy or double tract reconstruction), and method (intra- or extracorporeal) were selected according to the surgeons’ preferences.[19]
2.4. Clinical and surgical outcomes
We reviewed the patients’ medical records and collected the following information: age, sex, body mass index (BMI), American Society of Anesthesiologists (ASA) score, smoking history, comorbidities (hypertension, diabetes mellitus, cerebrovascular disease, cardiovascular disease, pulmonary disease, chronic kidney disease, and thyroid disease), presence of anemia and hypoalbuminemia, type of gastrectomy, extent of lymph node dissection (LND), and operation time. Cerebrovascular disease included a past history of intracranial hemorrhage or brain infarction. Cardiovascular disease included a coronary artery occlusive disease treated by catheter interventions, arrhythmia, and congestive heart failure. Chronic kidney disease was defined as a glomerular filtration rate of <60 ml/minute/1.73 m2 for >3 months, irrespective of the presence of other signs of kidney damage.[20] Hypoalbuminemia was defined as a serum albumin concentration of <3.5 g/dl.[21] Anemia was defined according to the World Health Organization criteria (<13 g/dl in males and <12 g/dl in females).[21] Tumor stages were determined according to the 7th Tumor, Node, Metastasis classification of the American Joint Committee on Cancer/International Union Against Cancer.[22] Body temperatures were measured by a thermometer through the tympanic route.[23] Postoperative fever was defined as a temperature >100°F (38°C) on 2 consecutive postoperative days, or >102.2°F (39°C) on any 1 postoperative day.[24–26] Hospital re-admission was defined according to the Centers for Medicare and Medicaid Services guidelines.[27] Data regarding mortality, postoperative fever, length of the postoperative hospital stay, re-admission within 30 days, incidence of SSI, and type of SSI were also collected as clinical outcomes of interest.
2.5. Statistical analysis
Patients were divided into 2 groups according to the occurrence of SSIs. In order to verify the normality of the continuous variables, Kolmogorov–Smirnov test and Shapiro–Wilk test were conducted, and Mann–Whitney U test was used to compare the continuous variables between the 2 groups. Chi-Squared or Fisher exact tests were used to compare the categorical variables. In analyses of risk factors for SSI, all variables with P < .05 in the univariate analyses were entered into the multivariate logistic regression model to identify the independent risk factors for SSI. These variables were stage III and IV gastric cancer (P = .02), total gastrectomy (P = .03), open surgery (P = .02), and a longer operation time (P = .04). Along with these variables, male gender, generally considered risk factor for SSIs after gastric cancer surgery,[28] was selected as variable of multivariate logistic regression analysis. P values of <.05 were considered statistically significant. All statistical analyses were performed using the Statistical Package for Social Sciences software, version 23.0 (IBM, Armonk, NY, USA).
3. Results
3.1. Clinical characteristics of older adults with an SSI after gastrectomy
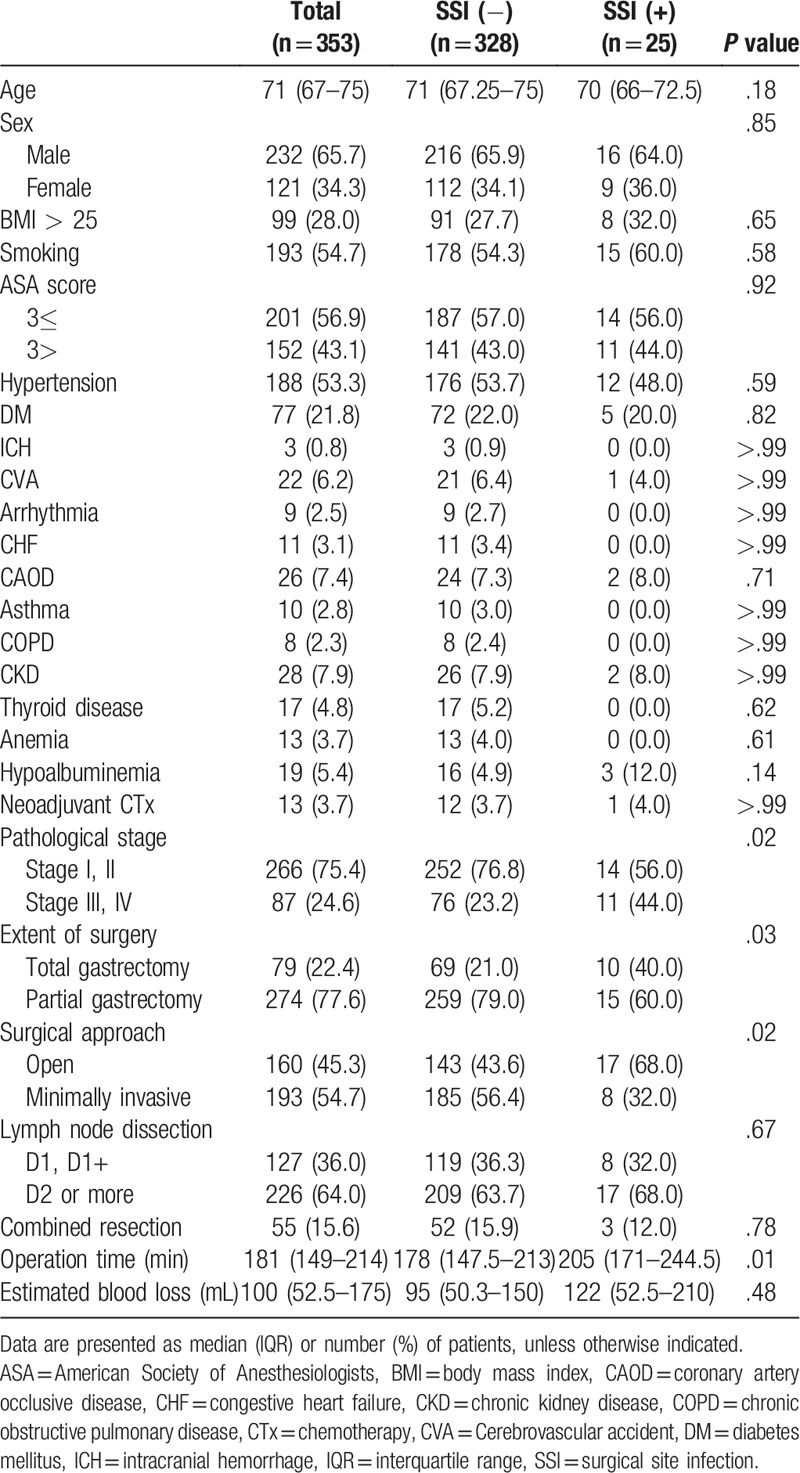
The clinical and surgical characteristics of the 353 patients who had undergone gastrectomy for stomach cancer are shown in Table 1. The differences in age, sex, obesity, and smoking status between the SSI- and non-SSI groups were not statistically significant. There was no statistically significant difference in the comorbidities, including diabetes mellitus, between the 2 groups. In addition, there was no statistically significant difference between the 2 groups in the ASA score, presence of anemia, presence of hypoalbuminemia, and neoadjuvant chemotherapy, conditions which may affect a patient's condition before surgery.
Table 1.
Clinical characteristics of older adults with surgical site infection after gastric cancer surgery.
3.2. Incidence, type, and treatment outcomes of SSIs
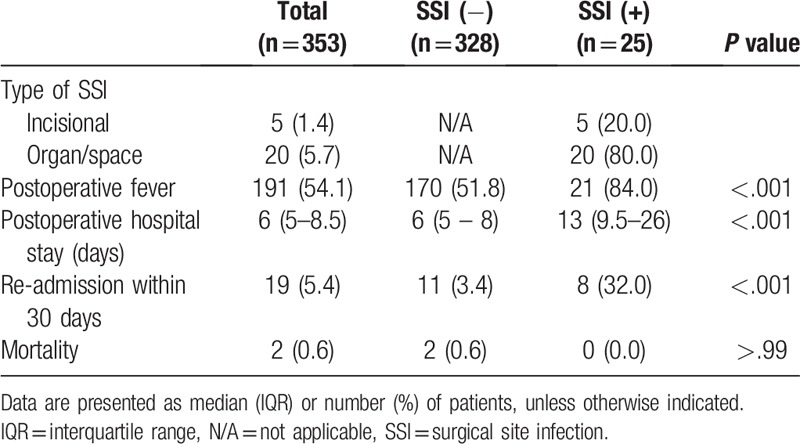
Table 2 shows the incidence, type, and treatment outcomes of the SSIs. Among the 353 patients who underwent gastrectomy, 25 (7.1%) developed an SSI. The incidence rates of SSIs in older adults were higher than younger adults but not statistically significant (7.1% vs 4.8%, respectively; P = .09). Of the 25 patients in the SSI group, 5 were diagnosed with an incisional SSI, and 20 were diagnosed with an organ/space SSI. In the SSI group, the frequency of postoperative fever was significantly higher than that in the non-SSI group (84.0% vs 51.8%, respectively; P < .001). The length of the postoperative hospital stay was significantly longer in the SSI group than in the non-SSI group (13 days vs 6 days, respectively; P < .001). The rate of re-admission within 30 days was also significantly higher in the SSI group than in the non-SSI group (32.0% vs 3.4%, respectively; P < .001). Of the 8 re-hospitalized patients in SSI group, 4 were re-admitted due to anastomosis site leakage and 4 were re-admitted with intra-abdominal fluid collection. In cases of the 11 re-hospitalized patients in the non-SSI group, 6 were re-admitted with delayed gastric emptying, 3 were re-admitted with upper gastrointestinal bleeding, and 2 were re-admitted due to intestinal obstruction. However, there was no significant difference in the mortality rate between the 2 groups (0.0% vs 0.6%, respectively, P > .99).
Table 2.
Treatment outcomes of surgical site infection in older adults after gastric cancer surgery.
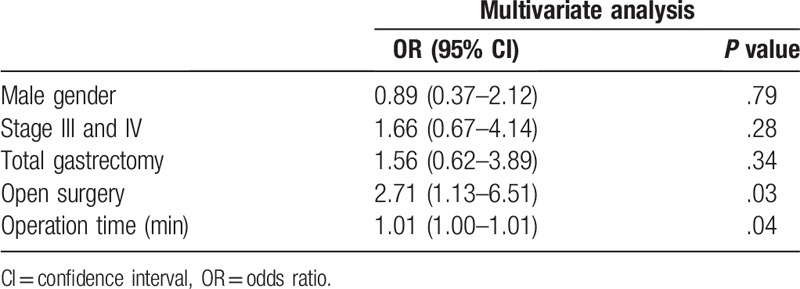
3.3. Risk factors for SSI
The results of the univariate analysis indicated that the following factors were significantly associated with the incidence of SSIs after gastrectomy: stage III and IV gastric cancer (P = .02), total gastrectomy (P = .03), open surgery (P = .02), and a longer operation time (P = .04). The results of the multivariate analysis revealed that an open surgery (odds ratio, 2.71; 95% confidence interval, 1.13–6.51; P = .03) and a longer operation time (odds ratio, 1.01; 95% confidence interval, 1.00–1.01; P = .04) were the independent risk factors for SSI in older adults after gastric cancer surgery (Table 3).
Table 3.
Multivariate logistic regression analysis to identify independent risk factors for surgical site infection in older adults after gastric cancer surgery.
4. Discussion
In the present study, the incidence of SSIs after gastric cancer surgery in older adults was 7.1%. Open surgery and a longer operation time were risk factors for the development of an SSI. In the SSI group, the length of the postoperative hospital stay was longer, and the incidence of the postoperative fever as well as the rate of re-admission within 30 days were also higher than those in the non-SSI group.
It is well known that SSIs occur more frequently in older adults, and the related risk factors have been investigated in many studies.[8,9,29,30] In addition, SSIs for specific surgeries in older adults have also been studied.[31,32] However, to the best of our knowledge, there are no existing studies on the incidence of SSIs in older adults who have undergone gastrectomy for gastric cancer.
In general, risk factors for SSIs after gastric cancer surgery have been determined through various studies, and there have also been studies on the risk factors for SSIs according to the surgical method used.[11,28,33] The range of possible surgical procedures, especially in the field of stomach cancer surgery, has been further widened by the availability of various options, such as laparoscopic and robotic surgery.[19,34,35] In general, minimally invasive surgery is known to have fewer postoperative complications than the open surgery; however, the results have not been confirmed in older adults.[36,37] Therefore, it is useful to identify the incidence and risk factors of SSIs after gastric cancer surgery in older adults.
In this study, the incidence of SSIs in older adults was 7.1% (25/353). The incidence of SSIs in minimally invasive surgery was 4.2% (8/193), and that in open surgery was 10.6% (17/160). These results demonstrated that the incidence of SSIs in minimally invasive surgery, such as laparoscopic or robotic surgery, was significantly lower than that in the open surgery (P = .02). Advances in minimally invasive surgery have benefited patients with stomach cancer. Although the indications for laparoscopy or robotic surgery remain controversial, many studies have shown that in comparison to open gastrectomy, minimally invasive surgery is associated with less postoperative pain, faster return of gastrointestinal function, better pulmonary function, decreased stress response, shorter hospital stay, and better postoperative quality of life.[38,39] In addition, as identified in this study, the risk of SSIs in older adults is also lower in minimally invasive surgery; therefore, this type of surgery could be recommended in older adults even in terms of postoperative infection prevention. And it remained robust after comparing open surgery with minimally invasive surgery in some variables like age, BMI, ASA score and pathological stage. The age, BMI, and ASA score of the patients were not different between 2 groups. Rather, in advanced stage gastric cancer, minimally invasive surgery was performed more than open surgery. Thus, if open gastrectomy is unavoidable, greater attention should be paid to the prevention of SSIs.
Another risk factor for SSI identified in the multivariate logistic regression was a longer operating time. Kurmann et al reported that the operation time was a risk factor for SSI in sigmoid colon resection.[40] As this has been verified in older adults who have undergone gastrectomy, surgeons will need to make efforts to reduce the operating time in order to prevent SSIs. Conversely, a BMI of >25 and male sex, which are known risk factors for SSI after gastric cancer surgery, as presented in previous studies, were not significant in this study.[12,41]
In this study, there was no increase in the mortality rate in the SSI group. However, the postoperative hospital stay length and re-admission rate within 30 days were significantly higher in the SSI group than in the non-SSI group. Therefore, surgeons are advised to select minimally invasive surgery, such as laparoscopic or robotic gastrectomy, rather than open gastrectomy, when choosing an operative method. In addition, if fever occurs after surgery, the possibility of a surgical site infection should be considered.
This study had some limitations. First, it was a nonrandomized, retrospective study. Therefore, patient characteristics among the groups might be biased because the patients with relatively advanced-stage gastric cancer were not considered candidates for minimally invasive surgery at our institution during the study period.[36] However, open gastrectomy still remained an independent risk factor because the stage III and IV gastric cancers were not found to be independent risk factors in the multivariate analysis. Second, the sample size of the SSI group was particularly small because the study was limited to older adults over 65 years of age. Third, since this study was conducted in an institution where advanced surgical techniques, such as laparoscopy and robotic surgery, are routinely used in gastric cancer operations, it might be difficult to generalize the findings to other institutions.
5. Conclusions
Open surgery and a longer operation time were determined to be the risk factors for SSI in older adults after gastrectomy. When SSIs occurred, the duration of the patient's postoperative hospital stay was prolonged, and the chances of experiencing postoperative fever and being re-admitted within 30 days also increased. Therefore, surgeons should consider these findings when planning gastric cancer surgery in older adults.
Acknowledgments
The authors thank all participants for participating in this study.
Author contributions
Conceptualization: Jung Ho Kim, Heun Choi, Jin Young Ahn, Nam Su Ku, Taeil Son, Jun Yong Choi, Woo Jin Hyung, Young Goo Song, June Myung Kim.
Data curation: Jung Ho Kim, Jinnam Kim, Woon Ji Lee, Hye Seong.
Formal analysis: Jinnam Kim, Hye Seong, Woo Jin Hyung.
Funding acquisition: Nam Su Ku.
Investigation: Jung Ho Kim, Woon Ji Lee, Hye Seong, Heun Choi, Jin Young Ahn, Taeil Son, Jun Yong Choi.
Methodology: Jung Ho Kim, Heun Choi, Jin Young Ahn, Taeil Son, Sang Hoon Han, Joon-Sup Yeom, Young Goo Song, June Myung Kim.
Project administration: Jung Ho Kim, Nam Su Ku.
Resources: Jinnam Kim, Taeil Son, Hyoung-Il Kim, Sang Hoon Han, Jun Yong Choi, Chang Oh Kim, Joon-Sup Yeom, Woo Jin Hyung, Sung Hoon Noh, June Myung Kim.
Supervision: Nam Su Ku, Taeil Son.
Validation: Jin Young Ahn, Taeil Son, Hyoung-Il Kim, Young Goo Song.
Visualization: Jung Ho Kim, Su Jin Jeong.
Writing – original draft: Jung Ho Kim.
Writing – review & editing: Jung Ho Kim.
Footnotes
Abbreviations: ASA = American Society of Anesthesiologists, BMI = body mass index, CAOD = coronary artery occlusive disease, CHF = congestive heart failure, CKD = chronic kidney disease, COPD = chronic obstructive pulmonary disease, CTx = chemotherapy, CVA = cerebrovascular accident, DM = diabetes mellitus, ICH = intracranial hemorrhage, IRB = Institutional Review Board, LND = lymph node dissection, SSI = surgical site infection.
This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korea government (MSIT) (2017R1C1B5017875). This study was supported by a faculty research grant of Yonsei University College of Medicine (6-2017-0054).
The authors declare that they have no conflicts of interest.
The data used to support the findings of this study are available from the corresponding author upon request.
References
- [1].Fitzmaurice C, Allen C, Barber RM, et al. Global, regional, and national cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life-years for 32 cancer groups, 1990 to 2015: A systematic analysis for the global burden of disease study. JAMA Oncol 2017;3:524–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Sano T, Sasako M, Yamamoto S, et al. Gastric cancer surgery: morbidity and mortality results from a prospective randomized controlled trial comparing D2 and extended para-aortic lymphadenectomy--Japan Clinical Oncology Group study 9501. J Clin Oncol 2004;22:2767–73. [DOI] [PubMed] [Google Scholar]
- [3].Mangram AJ, Horan TC, Pearson ML, et al. Guideline for prevention of surgical site infection, 1999. Hospital infection control practices advisory committee. Infect Control Hosp Epidemiol 1999;20:250–78. quiz 279–280. [DOI] [PubMed] [Google Scholar]
- [4].Smith RL, Bohl JK, McElearney ST, et al. Wound infection after elective colorectal resection. Ann Surg 2004;239:599–605. discussion 605–597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Kirkland KB, Briggs JP, Trivette SL, et al. The impact of surgical-site infections in the 1990 s: attributable mortality, excess length of hospitalization, and extra costs. Infect Control Hosp Epidemiol 1999;20:725–30. [DOI] [PubMed] [Google Scholar]
- [6].Culver DH, Horan TC, Gaynes RP, et al. Surgical wound infection rates by wound class, operative procedure, and patient risk index. National nosocomial infections surveillance system. Am J Med 1991;91:152s–7s. [DOI] [PubMed] [Google Scholar]
- [7].Centers for Disease Control and Prevention. Trends in aging–United States and worldwide. MMWR Morb Mortal Wkly Rep 2003;52:101–4. 106. [PubMed] [Google Scholar]
- [8].Kaye KS, Schmader KE, Sawyer R. Surgical site infection in the elderly population. Clin Infect Dis 2004;39:1835–41. [DOI] [PubMed] [Google Scholar]
- [9].Kaye KS, Sloane R, Sexton DJ, et al. Risk factors for surgical site infections in older people. J Am Geriatr Soc 2006;54:391–6. [DOI] [PubMed] [Google Scholar]
- [10].Lundebjerg NE, Trucil DE, Hammond EC, et al. When it comes to older adults, language matters: Journal of the American Geriatrics Society adopts modified American Medical Association style. J Am Geriatr Soc 2017;65:1386–8. [DOI] [PubMed] [Google Scholar]
- [11].Endo S, Tsujinaka T, Fujitani K, et al. Risk factors for superficial incisional surgical site infection after gastrectomy: analysis of patients enrolled in a prospective randomized trial comparing skin closure methods. Gastric Cancer 2016;19:639–44. [DOI] [PubMed] [Google Scholar]
- [12].Kosuga T, Ichikawa D, Komatsu S, et al. Clinical and surgical factors associated with organ/space surgical site infection after laparoscopic gastrectomy for gastric cancer. Surg Endosc 2017;31:1667–74. [DOI] [PubMed] [Google Scholar]
- [13].Song J, Oh SJ, Kang WH, et al. Robot-assisted gastrectomy with lymph node dissection for gastric cancer: lessons learned from an initial 100 consecutive procedures. Ann Surg 2009;249:927–32. [DOI] [PubMed] [Google Scholar]
- [14].Song J, Kang WH, Oh SJ, et al. Role of robotic gastrectomy using da Vinci system compared with laparoscopic gastrectomy: initial experience of 20 consecutive cases. Surg Endosc 2009;23:1204–11. [DOI] [PubMed] [Google Scholar]
- [15].Hyung WJ, Lim JS, Song J, et al. Laparoscopic spleen-preserving splenic hilar lymph node dissection during total gastrectomy for gastric cancer. J Am Coll Surg 2008;207:e6–11. [DOI] [PubMed] [Google Scholar]
- [16].Hyung WJ, Song C, Cheong JH, et al. Factors influencing operation time of laparoscopy-assisted distal subtotal gastrectomy: analysis of consecutive 100 initial cases. Eur J Surg Oncol 2007;33:314–9. [DOI] [PubMed] [Google Scholar]
- [17].Berrios-Torres SI, Umscheid CA, Bratzler DW, et al. Centers for disease control and prevention guideline for the prevention of surgical site infection, 2017. JAMA Surg 2017;152:784–91. [DOI] [PubMed] [Google Scholar]
- [18].Japanese Gastric Cancer Association. Japanese gastric cancer treatment guidelines 2014 (ver. 4). Gastric Cancer 2017;20:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Kim HI, Han SU, Yang HK, et al. Multicenter prospective comparative study of robotic versus laparoscopic gastrectomy for gastric adenocarcinoma. Ann Surg 2016;263:103–9. [DOI] [PubMed] [Google Scholar]
- [20].Korhonen PE. How to assess kidney function in outpatient clinics. Int J Clin Pract 2015;69:156–61. [DOI] [PubMed] [Google Scholar]
- [21].Inokuchi M, Kato K, Sugita H, et al. Impact of comorbidities on postoperative complications in patients undergoing laparoscopy-assisted gastrectomy for gastric cancer. BMC Surg 2014;14:97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Washington K. 7th Edition of the AJCC Cancer Staging Manual: Stomach. Annals of Surgical Oncology 2010;17:3077–9. [DOI] [PubMed] [Google Scholar]
- [23].Gasim GI, Musa IR, Abdien MT, et al. Accuracy of tympanic temperature measurement using an infrared tympanic membrane thermometer. BMC Res Notes 2013;6:194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Galicier C, Richet H. A prospective study of postoperative fever in a general surgery department. Infect Control 1985;6:487–90. [DOI] [PubMed] [Google Scholar]
- [25].de la Torre SH, Mandel L, Goff BA. Evaluation of postoperative fever: usefulness and cost-effectiveness of routine workup. Am J Obstet Gynecol 2003;188:1642–7. [DOI] [PubMed] [Google Scholar]
- [26].Garibaldi RA, Brodine S, Matsumiya S, et al. Evidence for the non-infectious etiology of early postoperative fever. Infect Control 1985;6:273–7. [DOI] [PubMed] [Google Scholar]
- [27].Chen M, Grabowski DC. Hospital readmissions reduction program: intended and unintended effects. Med Care Res Rev 2017;1077558717744611. [DOI] [PubMed] [Google Scholar]
- [28].Migita K, Takayama T, Matsumoto S, et al. Risk factors for surgical site infections after elective gastrectomy. J Gastrointest Surg 2012;16:1107–15. [DOI] [PubMed] [Google Scholar]
- [29].Horasan ES, Dag A, Ersoz G, et al. Surgical site infections and mortality in elderly patients. Med Mal Infect 2013;43:417–22. [DOI] [PubMed] [Google Scholar]
- [30].Raymond DP, Pelletier SJ, Crabtree TD, et al. Surgical infection and the aging population. Am Surg 2001;67:827–32. discussion 832–823. [PubMed] [Google Scholar]
- [31].Lee J, Singletary R, Schmader K, et al. Surgical site infection in the elderly following orthopaedic surgery. Risk factors and outcomes. J Bone Joint Surg Am 2006;88:1705–12. [DOI] [PubMed] [Google Scholar]
- [32].Kadar A, Eisenberg G, Yahav E, et al. Surgical site infection in elderly patients with hip fractures, silver-coated versus regular dressings: a randomised prospective trial. J Wound Care 2015;24:441–2. 444-445. [DOI] [PubMed] [Google Scholar]
- [33].Tu RH, Huang CM, Lin JX, et al. A scoring system to predict the risk of organ/space surgical site infections after laparoscopic gastrectomy for gastric cancer based on a large-scale retrospective study. Surg Endosc 2016;30:3026–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Park JM, Kim HI, Han SU, et al. Who may benefit from robotic gastrectomy?: a subgroup analysis of multicenter prospective comparative study data on robotic versus laparoscopic gastrectomy. Eur J Surg Oncol 2016;42:1944–9. [DOI] [PubMed] [Google Scholar]
- [35].Shen W, Xi H, Wei B, et al. Robotic versus laparoscopic gastrectomy for gastric cancer: comparison of short-term surgical outcomes. Surg Endosc 2016;30:574–80. [DOI] [PubMed] [Google Scholar]
- [36].Yang SY, Roh KH, Kim YN, et al. Surgical outcomes after open, laparoscopic, and robotic gastrectomy for gastric cancer. Ann Surg Oncol 2017;24:1770–7. [DOI] [PubMed] [Google Scholar]
- [37].Kostakis ID, Alexandrou A, Armeni E, et al. Comparison between minimally invasive and open gastrectomy for gastric cancer in Europe: a systematic review and meta-analysis. Scand J Surg 2017;106:3–20. [DOI] [PubMed] [Google Scholar]
- [38].Cho GS, Kim W, Kim HH, et al. Multicentre study of the safety of laparoscopic subtotal gastrectomy for gastric cancer in the elderly. Br J Surg 2009;96:1437–42. [DOI] [PubMed] [Google Scholar]
- [39].Okumura N, Son T, Kim YM, et al. Robotic gastrectomy for elderly gastric cancer patients: comparisons with robotic gastrectomy in younger patients and laparoscopic gastrectomy in the elderly. Gastric Cancer 2016;19:1125–34. [DOI] [PubMed] [Google Scholar]
- [40].Kurmann A, Vorburger SA, Candinas D, et al. Operation time and body mass index are significant risk factors for surgical site infection in laparoscopic sigmoid resection: a multicenter study. Surg Endosc 2011;25:3531–4. [DOI] [PubMed] [Google Scholar]
- [41].Hirao M, Tsujinaka T, Imamura H, et al. Overweight is a risk factor for surgical site infection following distal gastrectomy for gastric cancer. Gastric Cancer 2013;16:239–44. [DOI] [PubMed] [Google Scholar]


