Abstract
Background:
To systematically review the efficacy of surgical versus nonsurgical treatment for acute patellar dislocation.
Materials and Methods:
PubMed, Cochrane, and Embase were searched up to February 12, 2019. After removing duplicates, preliminary screening, and reading the full texts, we finally selected 16 articles, including 11 randomized controlled trials and 5 cohort studies. The quality of the enrolled studies was evaluated by Jadad score or Newcastle–Ottawa scale. Meta-analyses were performed using odds ratio (OR) and standardized mean difference (SMD) as effect variables. The clinical parameters assessed included mean Kujala score, rate of redislocation, incidence of patellar subluxation, patient satisfaction, and visual analog scale (VAS) for pain. Evidence levels were determined using GRADE profile.
Results:
The 16 included studies involved 918 cases, 418 in the surgical group and 500 in the nonsurgical group. The results of the meta-analysis showed higher mean Kujala score (SMD = 0.79, 95% confidence interval [CI] [0.3, 1.28], P = .002) and lower rate of redislocation (OR = 0.44, 95% CI [0.3, 0.63], P < .00001) in the surgical group than the nonsurgical group, but showed insignificant differences in the incidence of patellar subluxation (OR = 0.61, 95% CI [0.36, 1.03], P = .06), satisfaction of patients (OR = 1.44, 95% CI [0.64, 3.25], P = .38), and VAS (SMD = 0.84, 95% CI [−0.36, 9.03], P = .84).
Conclusion:
For patients with primary acute patellar dislocation, surgical treatment produces a higher mean Kujala score and a lower rate of redislocation than nonsurgical treatment.
Keywords: dislocation or subluxation, functional evaluation, meta-analysis, primary acute patellar dislocation, surgical treatment
1. Introduction
The patella, located below the knee joint, is the largest sesamoid bone in the human body. Acute patellar dislocation is one of the most common diseases of the knee joint. Improper treatment can lead to recurrence, pain, arthritis, or functional disorders. The probability of relapse is up to 40%.[1] Therefore, it is urgent in clinical practice to treat the condition effectively in order to reduce the recurrence rate and to ease the pain of patients.
Nowadays, therapeutic approaches include surgical and nonsurgical methods. The surgical method has a higher cure rate, but can easily cause complications. The nonsurgical method is simpler and safer, but the recurrence rate is higher. Researchers have conducted a large number of basic studies to compare the therapeutic effects of surgical treatment and nonsurgical treatment for acute patellar dislocation, but the results are still controversial. In recent years, several meta-analyses have compared the efficacy of surgical versus nonsurgical treatment for acute patellar dislocations,[2–6] providing clinicians with evidence-based medicine data for clinical practice. There are also some new experimental studies not previously included in meta have emerged in 2017 and 2018, which may have an impact on existing conclusions.
In this review, we conduct an up-to-date meta-analysis, including the latest randomized controlled trials and cohort studies[7–9] published in 2017 and 2018. The purpose of this review is to cover studies that compared outcome indicators for surgical and nonsurgical treatment. We focus on Kujala score and on clearly presenting the level of evidence for each finding,[10] in order to provide evidence-based medical criteria for clinical selection.
2. Materials and methods
2.1. Search strategy
2.1.1. Ethical approval
The Second Hospital of Jilin University, Changchun 130012, China. (Serial number: 2018-167)
2.1.2. Retrieval method
According to the method of Cochrane system evaluation and the list of PRISMA declaration,[11,12] 3 databases, Pubmed, Cochrane, and Embase were retrieved by computer in this paper (all up to February 12, 2019). The references for relevant reviews and systematic reviews were manually retrieved.
2.1.3. Basic PubMed search
The search performed in PubMed was for: ((((Dislocation, Patellar[Title/Abstract]) AND Dislocations, Patellar[Title/Abstract]) OR Patellar Dislocations[Title/Abstract])) OR “Patellar Dislocation”[Mesh] AND (“Surgical Procedures, Operative”[Mesh]) OR (((((((((((Operative Surgical Procedure[Title/Abstract]) OR Operative Surgical Procedures[Title/Abstract]) OR Procedures, Operative Surgical[Title/Abstract]) OR Surgical Procedure, Operative[Title/Abstract]) OR Operative Procedures[Title/Abstract]) OR Operative Procedure[Title/Abstract]) OR Procedure, Operative[Title/Abstract]) OR Procedures, Operative[Title/Abstract]) OR Procedure, Operative Surgical[Title/Abstract]) OR Surgery, Ghost[Title/Abstract]) OR Ghost Surgery[Title/Abstract])
2.2. Assessment of study eligibility
The inclusion criteria comprised randomized controlled trials (RCTs) and cohort studies with scores ≥6 on the Newcastle–Ottawa scale (NOS)[13] that
-
(1)
were written in English,
-
(2)
investigated primary acute patellar dislocation in human patients of any age, and
-
(3)
compared surgical and nonsurgical treatments for acute patellar dislocation.
Surgical treatments included medial structural repair and medial patellofemoral ligament (MPFL) reconstruction, while nonsurgical treatments included fixation, physiotherapy, and so on. We chose both RCT and cohort studies, because these years there are many studies[14–17] that mix RCT and cohort studies, this method could increase the sample size, take more information into account, and also meet the need of later Egger test.
The exclusion criteria comprised studies concerning recurrent or chronic patellar dislocation; animal or cadaver studies; and studies addressing chondromalacia patella, patellar malformation, or patellar subluxation.
2.3. Effect indicators
The 5 effect indicators defined in this study were mean Kujala score, rate of redislocation, incidence of patellar subluxation, satisfaction of patients, and visual analog scale (VAS) for pain.[18] The Kujala score is currently the most commonly used criterion for evaluation of the patella.[3] The scale includes 13 items involving daily function, pain, motor function, and symptoms. The range of possible scores is 0 to 100, with lower scores indicating higher levels of pain or disability. Rate of redislocation and incidence of patellar subluxation are 2 indicators objectively reflecting the risk for redislocation after treatment. Satisfaction of patients and VAS score intuitively reflect the therapeutic effect through the patient's subjective feelings.
2.4. Data extraction
Two researchers (FY, WG) independently extracted the data, recording the first author, publication year, sample size, age, sex, follow-up time, rate of redislocation, incidence of patellar subluxation, satisfaction of patients, mean Kujala score and VAS for each included study. A third researcher (RL) was responsible for resolving any disagreements.
2.5. Literature analysis and quality assessment
Modified Jadad [19,20] and NOS scores were used to assess the quality of the included RCTs and cohort studies. These 2 scales were scored independently by 2 researchers (FY, WG). Any disagreements were resolved by a third researcher (SZ). The modified Jadad score mainly focused on the following 4 aspects: randomization, concealment of allocation, double blinding, withdrawals, and dropouts. The NOS mainly focused on the selection of experimental and control groups, comparability, and outcomes. These 2 methods are quantifiable and helpful for subsequent analysis
2.6. Statistical analysis
Revman5.3 and Stata MP14 were used for the meta-analysis. Odds ratios (OR) were used as combined effect indicators for dichotomous variables (redislocation, patellar subluxation, patient satisfaction), and standardized mean differences (SMD) were used for continuous variables (mean Kujala score, VAS). The chi-square test was adopted to assess heterogeneity, with a threshold of P < .05. A value of I2 > 50% was considered to indicate high heterogeneity. We followed the rule that a random-effects model should be established when I2 > 50%, otherwise a fixed effects model should be used. Subgroup analyses, sensitivity analyses and meta-regression were used to find the sources of heterogeneity. Indicators included in more than 10 studies were tested for bias by funnel plots. Finally, GRADE profile software was used to determine the level of evidence.
3. Results
3.1. Literature search
Two researchers (FY, WG) independently screened the literature. The results of the search are shown in Figure 1: 878 articles from PubMed, 1354 from Embase, and 8 from the Cochrane database, for a total of 2240 studies. After excluding duplicates, 2028 studies were retained. 1646 studies were retained after reading titles, keywords, and abstracts. After reading full texts, 441 studies were assessed for eligibility, and only 14 studies involved not only qualitative but also quantitative synthesis. The remaining 16 articles (11 RCTs and 5 cohort studies) were included in this meta-analysis (see Fig. 1).
Figure 1.
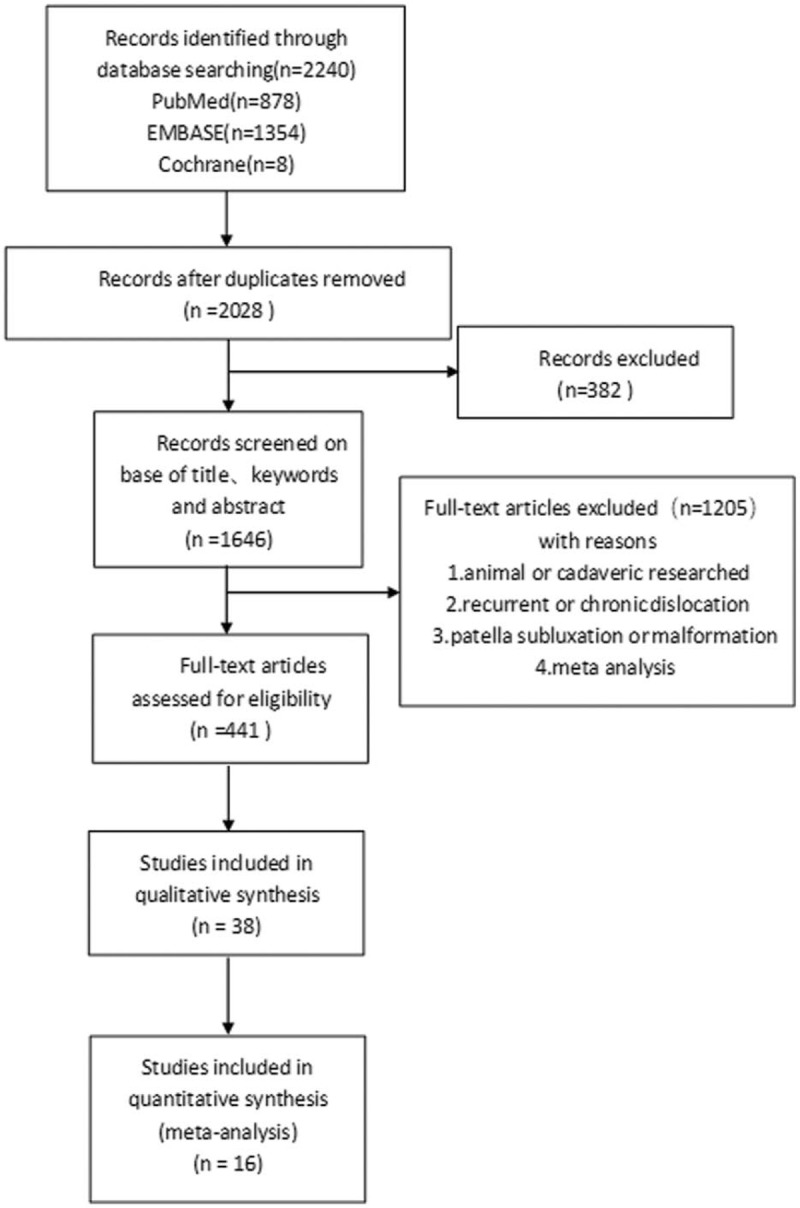
Literature search strategy and results.
3.2. Study characteristics
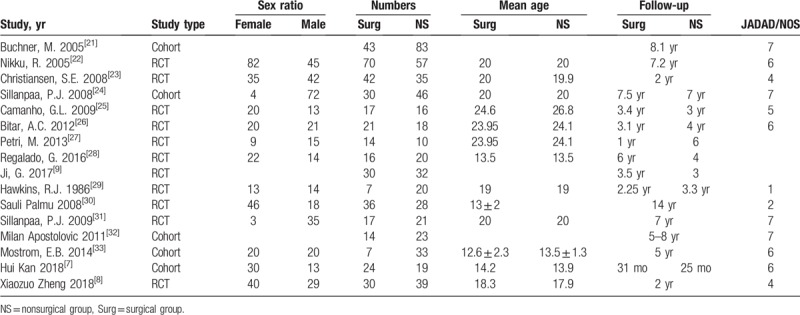
There were a total of 918 patients, with 418 in the surgery group and 500 in the nonsurgery group. The basic characteristics of the subjects are shown in Table 1.
Table 1.
Characteristics of the included trials and participants.
3.3. Meta-analysis results
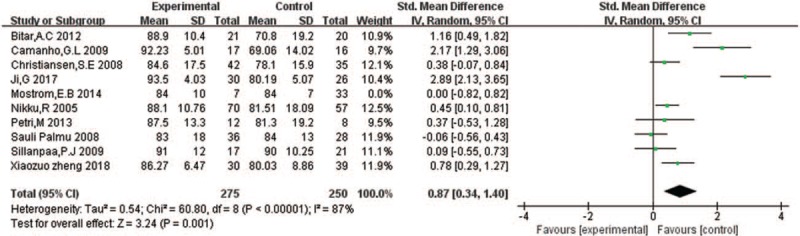
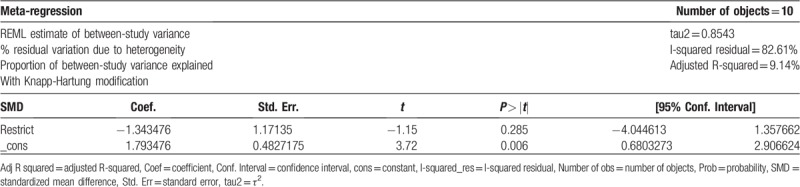
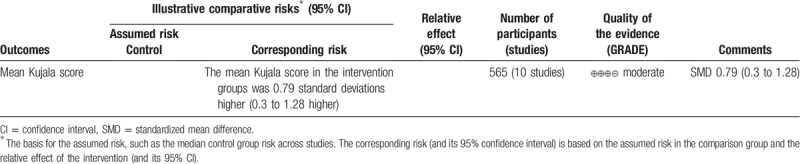
3.3.1. Mean Kujala score
Ten studies reported mean Kujala score, including 282 cases in the surgical group and 283 cases in the nonsurgical group. Among them, the standard deviation of the mean Kujala score was not indicated in Nikku [22] and Camanho.[25] However, we obtained the relevant data through the study of Sheng-nan Wang.[6] We calculated I2 = 86%, so a random effects model was selected. There was a significant difference between the surgical group and the nonsurgical group (SMD = 0.79, 95% confidence interval [CI] = 0.3–1.28, P < .002), with the mean Kujala score of the surgical group higher (see Fig. 2).
Figure 2.
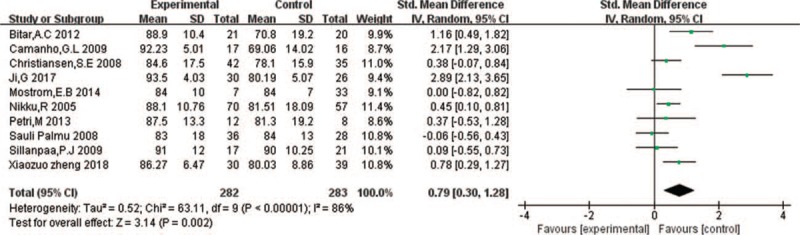
Forest plot for mean Kujala score.
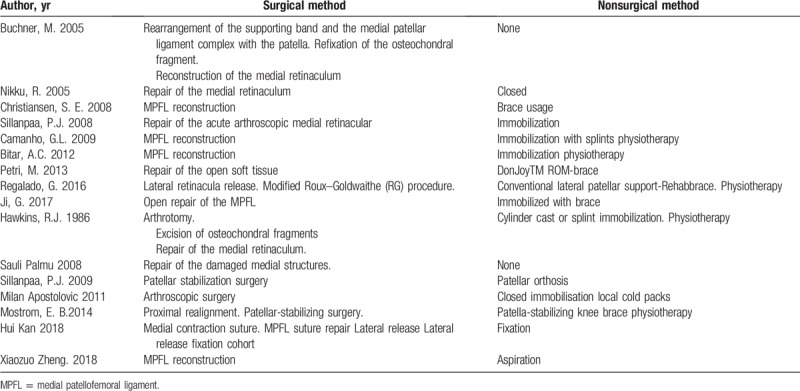
Table 2.
Surgical and nonsurgical treatment.
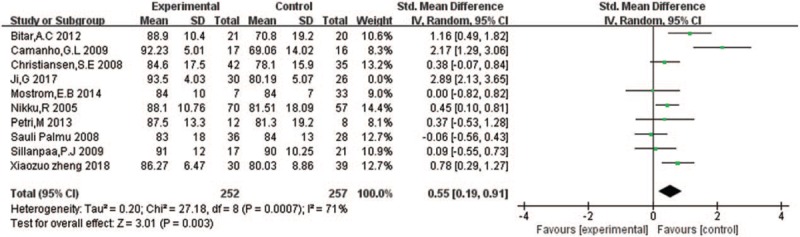
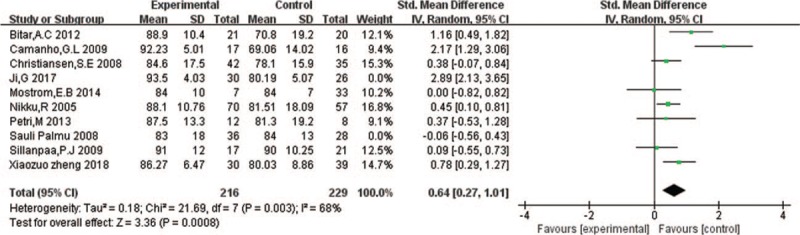
The calculated value of I2 = 86% indicated strong heterogeneity. To find the sources of heterogeneity, a cohort study by Mostrom[33] was removed for sensitivity analysis, low-quality RCTs were removed for sensitivity analysis, and a subgroup analysis was performed according to the year of publication. However, none of these efforts produced any decline in heterogeneity, and the conclusions of the 2 subgroups were consistent with the overall conclusion (see Figs. 3 and 4).
Figure 3.
Sensitivity analysis for mean Kujala score. 3.1 Remove the cohort study. 3.2 Remove the RCT with the lowest score. 3.3 Remove the RCT with the sub-low score.
Figure 3 (Continued).
Sensitivity analysis for mean Kujala score. 3.1 Remove the cohort study. 3.2 Remove the RCT with the lowest score. 3.3 Remove the RCT with the sub-low score.
Results from a meta-regression on the place of residence (Europe, Non-Europe) showed that tau2 = 0.8543 and R2 = 9.14%, indicating that the variation in mean Kujala score resulting from the place of residence was 9.14% (see Table 3).
Table 3.
Meta regression for mean Kujala score.
Univariate and multivariate meta-regression analysis was performed in the order of publication year, research method, original study quality, and place of residence (Europe, Non-Europe). We found excellent meta-regression model fits for the year of publication, original study quality, and place of residence, with a significantly reduced tau2 = 0.09607 and R2 = 89.78%, indicating that the heterogeneity accounted for by these 3 indicators was up to 89.78% (see Table 4).
Table 4.
Meta regression for mean Kujala score.
The quality of the above evidence was evaluated by the GRADE system as moderate (see Table 5).
Table 5.
Evidence evaluation for mean Kujala score.
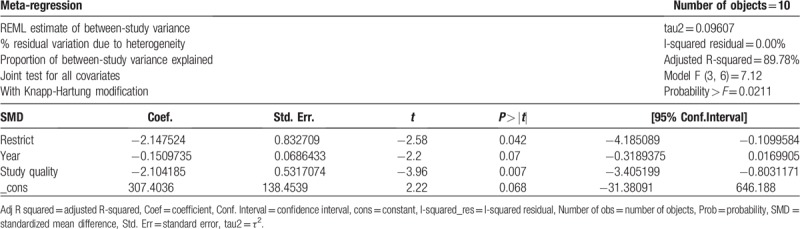
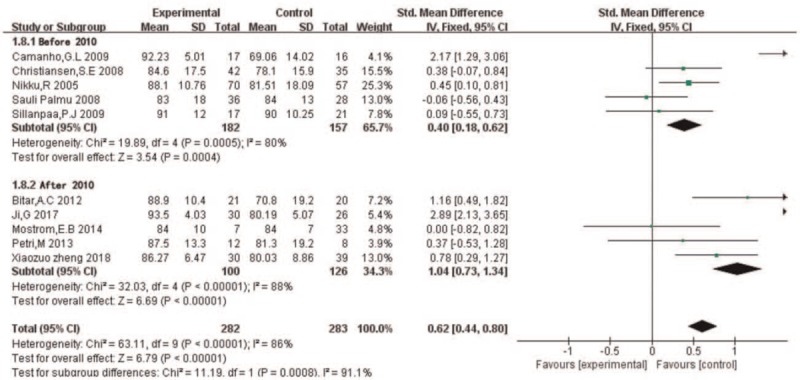
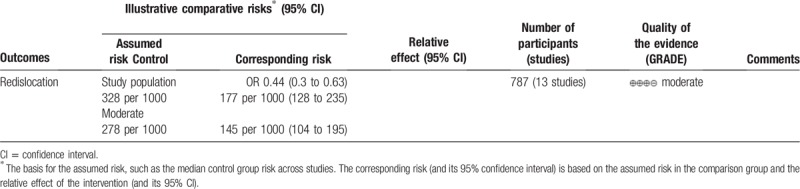
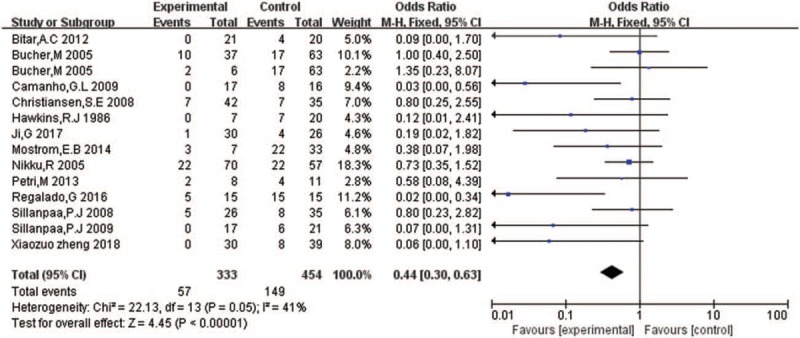
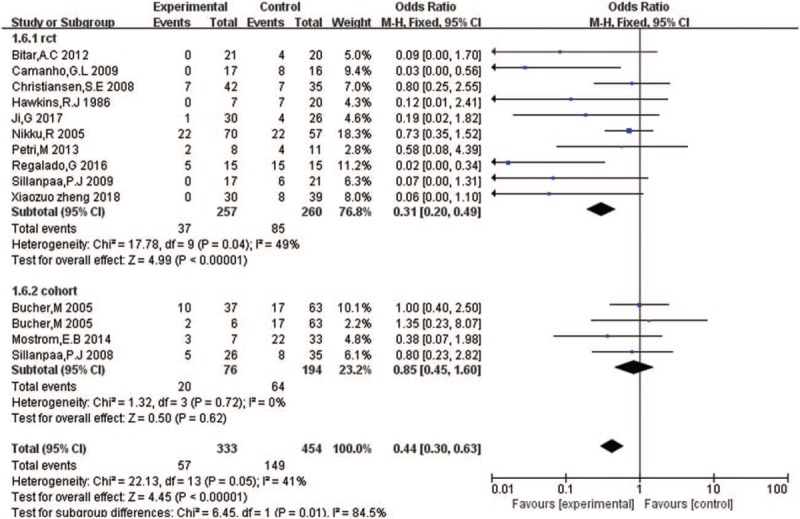
3.3.2. Redislocation
Thirteen studies reported redislocation, including 333 cases in the surgical group and 454 cases in the nonsurgical group. In Buchner,[21] there are 2 different surgical groups, so the nonsurgical group is compared with these 2 surgical groups, separately. We calculated I2 = 41%, so a fixed effects model was selected. There was a significant difference between the surgical group and the nonsurgical group (OR = 0.44, 95% CI = 0.3–0.63, P < .00001), with less redislocation in the surgical group (see Fig. 5).
Figure 3 (Continued).
Sensitivity analysis for mean Kujala score. 3.1 Remove the cohort study. 3.2 Remove the RCT with the lowest score. 3.3 Remove the RCT with the sub-low score.
A subgroup analysis was performed according to the type of researches (RCT, cohort), there was no significant decrease in heterogeneity, and the conclusion of the RCT subgroup was consistent with the overall conclusion (see Fig. 6).
Figure 4.
Subgroup analysis for mean Kujala score.
The quality of the above evidence was evaluated by the GRADE system as moderate (see Table 6).
Table 6.
Evidence evaluation for redislocation.
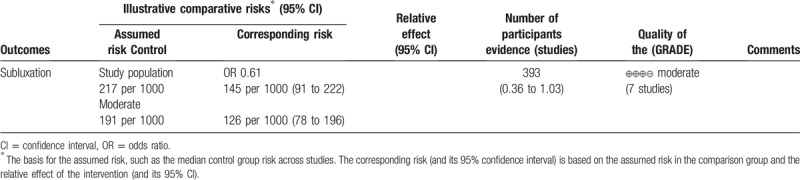
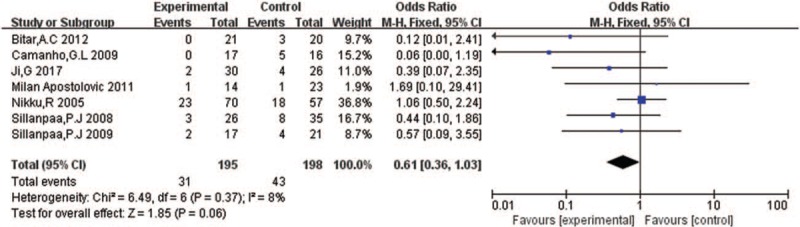
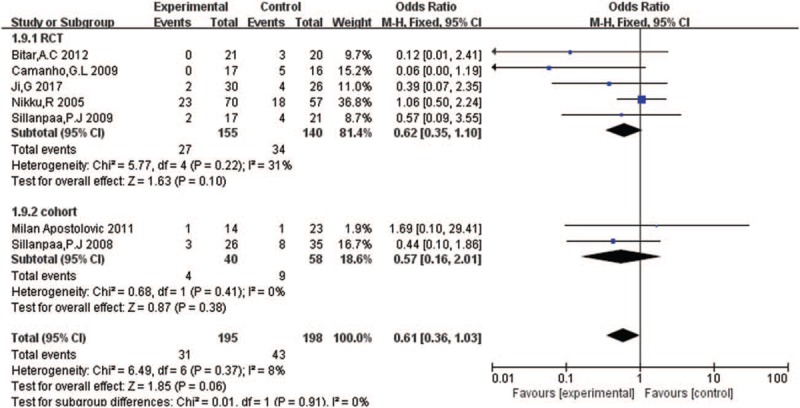
3.3.3. Subluxation
Seven studies reported subluxation, including 195 cases in the surgical group and 198 cases in the nonsurgical group. We calculated I2 = 8%, so a fixed effects model was selected. As shown in Figure 7, there was no significant difference between the surgical group and the nonsurgical group (OR = 0.61, 95% CI = 0.36–1.03, P = .06).
Figure 5.
Forest plot for redislocation.
A subgroup analysis was performed according to the type of researches (RCT, cohort), the results of the 2 subgroups were consistent, and the conclusions of the 2 subgroups were consistent with the overall conclusion (see Fig. 8).
Figure 6.
Subgroup analysis for redislocation.
The quality of the above evidence was evaluated by the GRADE system as moderate (see Table 7).
Table 7.
Evidence evaluation for subluxation.
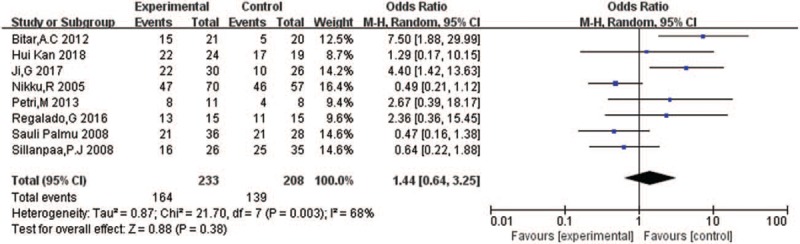
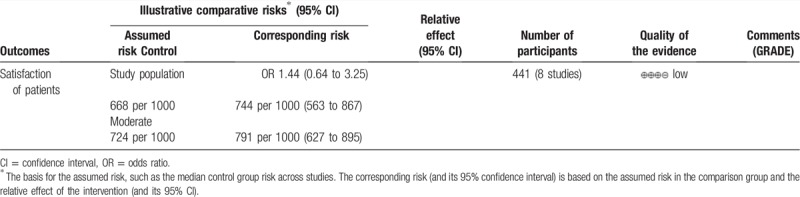
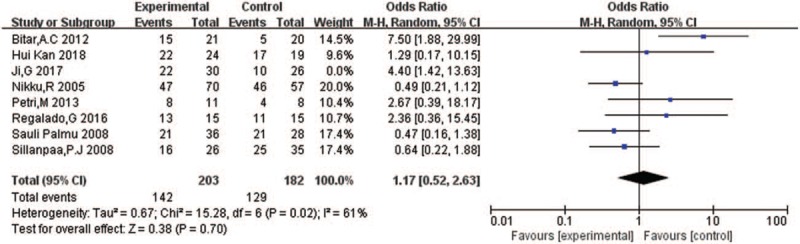
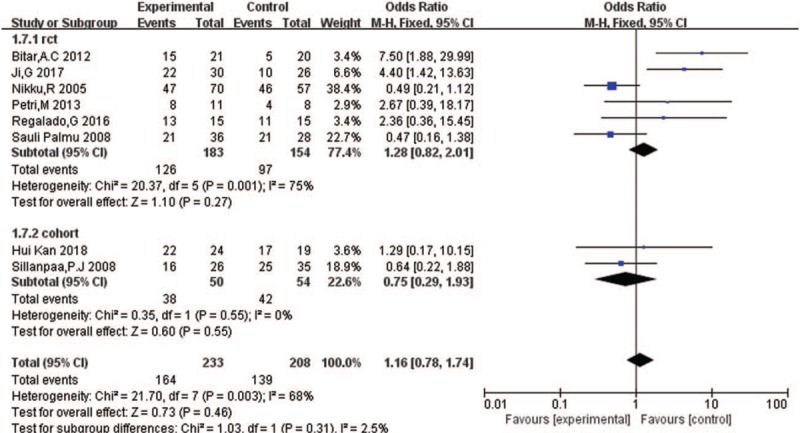
3.3.4. Satisfaction of patients
Eight studies reported satisfaction of patients, including 233 cases in the surgical group and 208 cases in the nonsurgical group. With patient-evaluations of “excellent” or “good” as the criteria for the occurrence of the event, I2 = 68%, so the random effect model was selected. As shown in Figure 9, there was no significant difference between the surgical group and the nonsurgical group (OR = 1.44, 95% CI = 0.64–3.25, P = .38).
Figure 7.
Forest plot for subluxation.
To find the sources of heterogeneity, a RCT of low grade was removed for sensitivity analysis, but the value of I2 was not be decreased (see Fig. 10).
Figure 8.
Subgroup analysis for subluxation.
A subgroup analysis was performed according to the type of researches (RCT, cohort), there was no significant decrease in heterogeneity, indicating that heterogeneity did not come from the literature type, and the conclusions of the 2 subgroups were consistent with the overall conclusion (see Fig. 11).
Figure 9.
Forest plot for satisfaction of patients.
The quality of the above evidence was evaluated by GRADE system as low (see Table 8).
Table 8.
Evidence evaluation for satisfaction of patients.
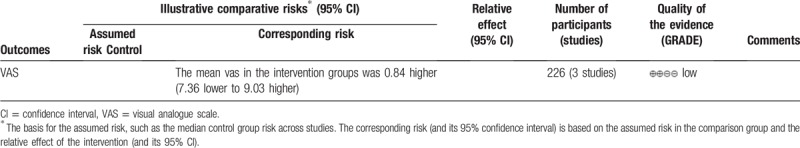
3.3.5. VAS
Three studies reported VAS pain scores, including 113 cases in the surgical group and 113 cases in the nonsurgical group. The standard deviation data for VAS were calculated according to the data conversion formula of the Cochrane method. We calculated I2 = 66%, so a random effects model was selected. As shown in Figure 12, there was no significant difference between the surgical group and the nonsurgical group (SMD = 0.84, 95% CI = −7.36 to 9.03, P = .84).
Figure 10.
Sensitivity analysis for satisfaction of patients.
Figure 12.
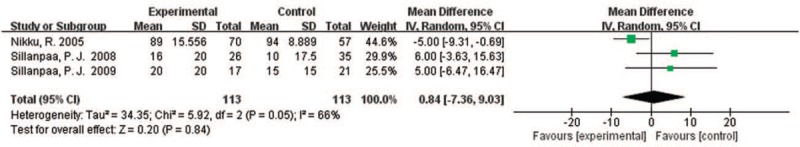
Forest plot for VAS. VAS = visual analog scale.
To find the sources of heterogeneity, a cohort study by Sillanpaa, 2008[24] was removed for sensitivity analysis, and the value of I2 was not be reduced (see Fig. 13).
Figure 11.
Subgroup analysis for satisfaction of patients.
Figure 13.
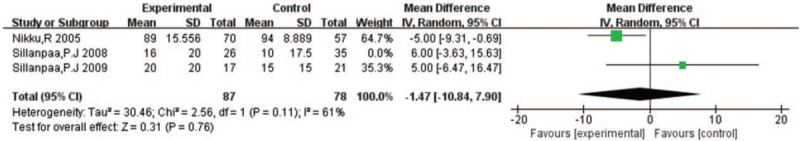
Sensitivity analysis for VAS. VAS = visual analog scale.
The quality of the above evidence was evaluated by the GRADE system as low (see Table 9).
Table 9.
Evidence evaluation for VAS.
4. Discussion
The results of this meta-analysis indicate that surgical treatment method resulted in generally higher Kujala score and lower rate of redislocation than nonsurgical treatment. Therefore, the surgical method has a good curative effect in the treatment of acute patellar dislocation. In clinical practice, an appropriate treatment is chosen with reference to the patient's economic level and prognosis, as far as possible.
This study followed the Cochrane systematic review process, and clear inclusion and exclusion criteria for literature screening were established on the basis of the PRISMA checklist.[11,12] Literature quality was evaluated based on modified Jadad scores or NOS scores. Cohort studies were included to ensure that there were enough studies included for each effect index. In this study, the total number of patients and the number of patients for each index were both higher than those reported in other meta-analyses of surgical and nonsurgical treatment of patellar dislocation published in the last 3 years.[2–4,6,34–36] The average follow-up time was 5.08 years. These factors all ensure the reliability of the results in this study.
In this study, the Kujala score of the surgical group was higher than that of the nonsurgical group. This is inconsistent with the conclusions of meta-analyses published in 2014 and 2016,[3,4,6] in which there were no differences between surgical and nonsurgical treatments in terms of Kujala score. Herein, we reassessed the Kujala score based on the latest researches published in 2017[9] and 2018,[8] together with the preliminary data previously published. As the Kujala score showed strong heterogeneity, the Egger test was performed to ensure the reliability of the results. The results showed no evidence of publication bias (P = .209). Also, the GRADE score indicated that the evidence was moderate (Table 5). These results indicate that the conclusion that the mean Kujala score of the surgical group was higher than that of the nonsurgical group is reliable and valid. Existing evidence from meta-analyses shows that surgical treatment produces less recurrence of patellar dislocation than nonsurgical treatment, but there are no significant differences between the 2 treatments in the incidence of patellar subluxation, satisfaction of patients and VAS score. Our article also confirmed these points based on the latest and preliminary data.
Heterogeneity was tested using sensitivity analysis, subgroup analysis, and meta-regression. For the Kujala score, meta-regression was conducted for the year of publication, original study quality, and place of residence. The heterogeneity that could be explained by the aforementioned meta-regression analysis was up to 89.78%, so it can be concluded that the 3 factors aforementioned were the sources of heterogeneity.
The GRADE system was used in this study to evaluate the quality of the results: the results for Kujala score, rate of redislocation and incidence of patellar subluxation were confirmed as having moderate levels of evidence; the results for patient satisfaction and VAS were confirmed having a low level of evidence. The main factors that reduced the level of evidence were as follows:
In the included studies, the randomization was not fully hidden, and the description of blinding method used was unclear. Due to the feature of this indicator, it was rarely possible to conduct a double-blind experiment. Only in the study reported by Ji et al,[9] was the blinding method clearly described. Moreover, randomization concealment was unclear. It was only in the studies of Petri et al[27] and Sillanpaa et al[31] that the use of “opaque envelopes” was described.
The high values of I2 for the Kujala score and satisfaction of patients indicated high heterogeneity.
There was a certain degree of publication bias in the rate of redislocation, as indicated by the funnel plot.
Studies have shown that 2/3 of acute patellar dislocations occur in young active patients (less than 20 years of age). The main mechanism underlying patellar dislocation is noncontact knee sprain causing dislocation of the knee, accounting for 93% of all cases.[37] Four predisposing factors for patellar dislocation include sulcus angle, Insall-Salvati ratio, tibial tuberosity-trochlear groove distance, and femoral anteversion angle. Among these, sulcus angle is the most important factor.[37] Generally, clinicians choose a favorable treatment, surgical or nonsurgical, for patellar dislocation through a comprehensive evaluation of these factors. After medical imaging examination such as arthroscopy, a surgical or nonsurgical treatment will be performed. Surgical methods include knee replacement and MPFL reconstruction,[38] while nonsurgical methods include physical fixation. Poor outcomes result in recurrence, infection and other complications, of which knee pain is the most common.[39] A recent related study by Lee pointed out that surgical treatment is suitable for both acute and recurrent patellar dislocations,[4,40] and that it can improve knee joint function.[9] More importantly, patients often have a low recurrence rate after surgical treatment.[6,28] Moreover, the risk of redislocation after nonsurgical treatment is 5 times the risk after surgical treatment.[5] Some researchers have proposed that normal or mildly abnormal patella joints can be treated nonsurgically, while surgical treatments are suitable for major abnormalities in the patella.[41] However, Risto Nikku pointed out that patients undergoing surgical treatments may experience serious complications.[42] Yet considering the different definitions and standards of complications in the basic studies, this paper did not do it, which could be done by the follow-up studies.
This study has some limitations. There were differences in target population, follow-up time, and interventions in the included studies, which may lead to partial bias in the results. We also found that there were differences in the efficacy of different surgical methods. Therefore, further investigations on a single surgical method are warranted to analyze the differences between surgical and nonsurgical methods in the treatment of patellar dislocation.
5. Conclusions
Based on the available evidence, surgical treatment of acute patellar dislocation is associated with a higher mean Kujala score and a lower rate of redislocation. The therapeutic method should be selected cautiously based on the physical findings.
Author contributions
Conceptualization: Zhe Zhu.
Data curation: Fan Yang, Wenlai Guo, Congying Guan.
Formal analysis: Fan Yang, Wenlai Guo.
Investigation: Fan Yang, Wenlai Guo.
Methodology: Shishun Zhao, Baoming Yuan.
Project administration: Fan Yang, Wenlai Guo.
Software: Fan Yang, Wenlai Guo.
Supervision: Qian Wang, Zhe Zhu, Baoming Yuan.
Visualization: Fan Yang, Wenlai Guo, Congying Guan.
Writing – original draft: Fan Yang, Wenlai Guo.
Writing – review and editing: Fan Yang, Wenlai Guo.
Shishun Zhao orcid: 0000-0002-1180-9708.
Footnotes
Abbreviation: NS = nonsurgical treatment, Surg = surgical treatment.
FY and WG contributed equally to this work and should be considered co-first authors.
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
The authors have no conflicts of interest to disclose.
Protocol and registration: PROSPERO, registration ID: CRD42018111081.
References
- [1].Fithian DC, Paxton EW, Stone ML, et al. Epidemiology and natural history of acute patellar dislocation. Am J Sports Med 2004;32:1114–21. [DOI] [PubMed] [Google Scholar]
- [2].Cheng B, Wu X, Ge H, et al. Operative versus conservative treatment for patellar dislocation: a meta-analysis of 7 randomized controlled trials. Diagn Pathol 2014;9:60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Shou-Wen SU, Shi DH, Zhi-Yong LI, et al. Conservative versus surgical interventions for treating acute patellar dislocation:a meta-analysis. J Sun Yat-sen Univ (Med Sci) 2014;35:624–31. [Google Scholar]
- [4].Zheng X, Kang K, Li T, et al. Surgical versus non-surgical management for primary patellar dislocations: an up-to-date meta-analysis. Eur J Orthop Surg Traumatol 2014;24:1513–23. [DOI] [PubMed] [Google Scholar]
- [5].Nwachukwu BU, So C, Schairer WW, et al. Surgical versus conservative management of acute patellar dislocation in children and adolescents: a systematic review. Knee Surg Sports Traumatol Arthrosc 2016;24:760–7. [DOI] [PubMed] [Google Scholar]
- [6].Wang SN, Qin CH, Jiang N, et al. Is surgical treatment better than conservative treatment for primary patellar dislocations? A meta-analysis of randomized controlled trials. Arch Orthop Trauma Surg 2016;136:371–9. [DOI] [PubMed] [Google Scholar]
- [7].Kang H, Li J, Chen X-X, et al. Fixation versus excision of osteochondral fractures after patellar dislocations in adolescent patients: a retrospective cohort study. Chin J Med 2018;131:1296–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Zheng X, Hu Y, Xie P, et al. Surgical medial patellofemoral ligament reconstruction versus non-surgical treatment of acute primary patellar dislocation: a prospective controlled trial. Int Orthop 2018;43:1495–501. [DOI] [PubMed] [Google Scholar]
- [9].Ji G, Wang S, Wang X, et al. Surgical versus nonsurgical treatments of acute primary patellar dislocation with special emphasis on the MPFL injury patterns. J Knee Surg 2017;30:378–84. [DOI] [PubMed] [Google Scholar]
- [10].Kujala UM, Jaakkola LH, Koskinen SK, et al. Scoring of patellofemoral disorders. Arthroscopy 1993;9:159–63. [DOI] [PubMed] [Google Scholar]
- [11].Moher D, Cook DJ, Eastwood S, et al. Improving the quality of reports of meta-analyses of randomised controlled trials: the QUOROM statement. QUOROM Group. Br J Surg 2000;87:1448–54. [DOI] [PubMed] [Google Scholar]
- [12].Moher D, Shamseer L, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev 2015;4:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 2010;25:603–5. [DOI] [PubMed] [Google Scholar]
- [14].Mbeye NM, Kuile FO, Davies M-A, et al. Cotrimoxazole prophylactic treatment prevents malaria in children in sub-Saharan Africa: systematic review and meta-analysis. Trop Med Int Health 2014;19:1057–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Chen M, Wei S, Hu J, et al. Can comprehensive chromosome screening technology improve IVF/ICSI outcomes? A meta-analysis. PLoS One 2015;10:e0140779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Cheng X, Tian X, Yan Z, et al. Comparison of the fertility outcome of salpingotomy and salpingectomy in women with tubal pregnancy: a systematic review and meta-analysis. PLoS One 2016;11:e0152343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Smith JD, MacDougall CC, Johnstone J, et al. Effectiveness of N95 respirators versus surgical masks in protecting health care workers from acute respiratory infection: a systematic review and meta-analysis. Cmaj 2016;188:567–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Flandry F, Hunt JP, Terry GC, et al. Analysis of subjective knee complaints using visual analog scales. Am J Sports Med 1991;19:112–8. [DOI] [PubMed] [Google Scholar]
- [19].Jadad AR, Moore RA, Carroll D, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials 1996;17:1–2. [DOI] [PubMed] [Google Scholar]
- [20].Banares R, Albillos A, Rincon D, et al. Endoscopic treatment versus endoscopic plus pharmacologic treatment for acute variceal bleeding: a meta-analysis. Hepatology 2002;35:609–15. [DOI] [PubMed] [Google Scholar]
- [21].Buchner M, Baudendistel B, Sabo D, et al. Acute traumatic primary patellar dislocation: long-term results comparing conservative and surgical treatment. Clin J Sport Med 2005;15:62–6. [DOI] [PubMed] [Google Scholar]
- [22].Nikku R, Nietosvaara Y, Aalto K, et al. Operative treatment of primary patellar dislocation does not improve medium-term outcome: a 7-year follow-up report and risk analysis of 127 randomized patients. Acta Orthop 2005;76:699–704. [DOI] [PubMed] [Google Scholar]
- [23].Christiansen SE, Jakobsen BW, Lund B, et al. Isolated repair of the medial patellofemoral ligament in primary dislocation of the patella: a prospective randomized study. Arthroscopy 2008;24:881–7. [DOI] [PubMed] [Google Scholar]
- [24].Sillanpaa PJ, Maenpaa HM, Mattila VM, et al. Arthroscopic surgery for primary traumatic patellar dislocation: a prospective, nonrandomized study comparing patients treated with and without acute arthroscopic stabilization with a median 7-year follow-up. Am J Sports Med 2008;36:2301–9. [DOI] [PubMed] [Google Scholar]
- [25].Camanho GL, Viegas AdC, Bitar AC, et al. Conservative versus surgical treatment for repair of the medial patellofemoral ligament in acute dislocations of the patella. Arthroscopy 2009;25:620–5. [DOI] [PubMed] [Google Scholar]
- [26].Bitar AC, Demange MK, D’Elia CO, et al. Traumatic patellar dislocation: nonoperative treatment compared with MPFL reconstruction using patellar tendon. Am J Sports Med 2012;40:114–22. [DOI] [PubMed] [Google Scholar]
- [27].Petri M, Liodakis E, Hofmeister M, et al. Operative vs conservative treatment of traumatic patellar dislocation: results of a prospective randomized controlled clinical trial. Arch Orthop Trauma Surg 2013;133:209–13. [DOI] [PubMed] [Google Scholar]
- [28].Regalado G, Lintula H, Kokki H, et al. Six-year outcome after non-surgical versus surgical treatment of acute primary patellar dislocation in adolescents: a prospective randomized trial. Knee Surg Sports Traumatol Arthrosc 2016;24:6–11. [DOI] [PubMed] [Google Scholar]
- [29].Hawkins RJ, Bell RH, Anisette G. Acute patellar dislocations. The natural history. Am J Sports Med 1986;14:117–20. [DOI] [PubMed] [Google Scholar]
- [30].Palmu S, Kallio PE, Donell ST, et al. Acute patellar dislocation in children and adolescents: a randomized clinical trial. J Bone Joint Surg Am 2008;90:463–70. [DOI] [PubMed] [Google Scholar]
- [31].Sillanpää PJ, Mattila VM, Mäenpää H, et al. Treatment with and without initial stabilizing surgery for primary traumatic patellar dislocation: a prospective randomized study. J Bone Joint Surg Am 2009;91:263–73. [DOI] [PubMed] [Google Scholar]
- [32].Apostolovic M, Vukomanovic B, Slavkovic N, et al. Acute patellar dislocation in adolescents: operative versus nonoperative treatment. Int Orthop 2011;35:1483–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Moström EB, Mikkelsen C, Weidenhielm L, et al. Long-term follow-up of nonoperatively and operatively treated acute primary patellar dislocation in skeletally immature patients. Sci World J 2014;2014:473281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Saccomanno MF, Sircana G, Fodale M, et al. Surgical versus conservative treatment of primary patellar dislocation. A systematic review and meta-analysis. Int Orthop 2016;35:1–1. [DOI] [PubMed] [Google Scholar]
- [35].Lee DY, Park YJ, Song SY, et al. Which Technique Is Better for Treating Patellar Dislocation? A Systematic Review and Meta-analysis. Arthroscopy 2018;34:3082–93. [DOI] [PubMed] [Google Scholar]
- [36].Longo UG, Ciuffreda M, Locher J, et al. Treatment of primary acute patellar dislocation: systematic review and quantitative synthesis of the literature. Clin J Sport Med 2017;27:511–23. [DOI] [PubMed] [Google Scholar]
- [37].Duthon VB. Acute traumatic patellar dislocation. Orthop Traumatol Surg Res 2015;101:S59–67. [DOI] [PubMed] [Google Scholar]
- [38].Wang HD, Dong JT, Gao SJ. Medial patellofemoral ligament reconstruction using a bone groove and a suture anchor at patellar: a safe and firm fixation technique and 3-year follow-up study. J Orthop Surg Res 2016;11:138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Turkmen I, Saglam Y, Turkmensoy F, et al. Influence of sagittal plane malpositioning of the patella on anterior knee pain after tibia intramedullary nailing. Eur J Orthop Surg Traumatol 2017;27:133–9. [DOI] [PubMed] [Google Scholar]
- [40].Lee HL, Yau WP. Management of traumatic patellar dislocation in a regional hospital in Hong Kong. Hong Kong Med J 2017;23:122–8. [DOI] [PubMed] [Google Scholar]
- [41].Sillanpaa PJ, Maenpaa HM. First-time patellar dislocation: surgery or conservative treatment? Sports Med Arthrosc Rev 2012;20:128–35. [DOI] [PubMed] [Google Scholar]
- [42].Nikku R, Nietosvaara Y, Kallio PE, et al. Operative versus closed treatment of primary dislocation of the patella. Similar 2-year results in 125 randomized patients. Acta Orthop Scand 1997;68:419–23. [DOI] [PubMed] [Google Scholar]


