Abstract
Rationale:
In this paper, the efficacy and safety of using navigated drilling and arthroscopy (NDA) to assist surgery for ulnar–radial joint dislocation caused by epiphyseal premature closure (EPC) are described. Deformity correction surgery was mentioned in the literature, but there were numerous complications, for example, poor correction, infection, neurovascular injury, osteofascial compartment syndrome, failure of internal fixation, and nonunion after osteotomy. In order to minimize surgical complications, we utilized navigated drilling to finish accuracy bone bridge resection and applied arthroscopy to assess wrist lesions.
Patient concerns:
An 11-year-old male patient showed swelling and pain of the left wrist.
Diagnoses:
The patient was diagnosed with a postoperative of Kirschner wire internal fixation for epiphyseal injury, left lower ulnar–radial joint dislocation, left wrist deformity, and EPC.
Interventions:
A NDA was used to assist the bone bridge resection in this patient.
Outcomes:
Pain was relieved clearly in the patient. Dorsiflexion increased from 60.8° to 85.3°, palmar flexion increased from 45.3° to 65.8°, supination increased from 41.3° to 69.5°, and pronation increased from 31.6° to 62.9°. The preoperative disabilities of the arm, shoulder, and hand (DASH) score was 86.1, which was increased to 16.4 postoperatively. Surgery designing lasted for 2 minutes, bone bridge resection lasted for 56 minutes, and fluoroscopic time was 2.4 minutes. Complications, for example, neurological injury, vascular injury, infection and deformity aggressive, were not found during the 5-month follow up.
Lessons:
The outcome of the present study suggests that the NDA maximizes the bone bridge resection accuracy in EPC treatment, which is made efficient by reducing surgical trauma and avoiding neurovascular injury. An experience was gained that in the process of bone bridge removal, the bit of navigated drill should be continuously washed with normal saline to cool down, so as to avoid damage of nerve caused by heat conduction.
Keywords: arthroscopy, drill, epiphyseal, navigation, radius
1. Introduction
Deformity healing after distal radius fracture is often attributed to instability or high loss of fixation and epiphyseal injury, a complication of distal radius fracture commonly occurring in children.[1–4] The injury of distal radius epiphysis will lead to the impaired growth of radius and closure of epiphysis in early stage.[5] Normal growth of ulna and arrest of radius can cause the separation of ulnar–radial joints and the deviation of wrist joints to radial side, and they often result in pseudo Madelung deformity, which limits the rotation of wrist joint and forearm.[6] In 1935, Meyerding and Overton[7] first proposed the treatment method of corrective osteotomy. However, corrective osteotomy operation has numerous complications, for example, poor correction, infection, neurovascular injury, osteofascial compartment syndrome, failure of internal fixation, and nonunion after osteotomy. Tyler et al[8] reported that corrective osteotomy also decreases the congestion caused by excision of intra-articular lesions, thereby increasing recurrence and secondary osteoarthritis. Oberc et al[9] found the recurrence rate of the injury up to 75%.
The use of computer navigation and arthroscopy in orthopedics is now gaining popularity. Yu et al[10] verified that the computer navigated drilling method has been successfully employed to hemivertebra resection. Arthroscopy can be used to observe and assess wrist lesions.[11–13] Here, NDA was combined to improve bone bridge resection, and the subsequent growth may correct the deformity. To the best of our knowledge, there are very few studies on the combination of NDA in the treatment of EPC.
2. Ethical approval
This paper was approved by the ethics committee of the Second Hospital of Jilin University, Changchun, China. The patient was given a written informed consent for this report, and his anonymity was kept confidential. (2019) Research and Inspection No. (009).
3. Case report
3.1. Patient characteristics
An 11-year-old male patient characterized by swelling and pain of the left wrist (Table 1). According to physical examination, wrist deformity and radial deviation of left hand were revealed. The patient suffered a fracture of the left distal radius caused by trauma a year ago, and he underwent open reduction and Kirschner wire internal fixation surgery. According to the preoperative x-ray examination based on this admission, the distal part of the ulna is longer than that of radial (Fig. 1). Three dimensional (3D) computed tomography (CT) scan images showed that there existed a strip-like high density area below the epiphyseal plate of the distal radius (Fig. 2). Magnetic resonance imaging (MRI) revealed a small amount of long T1 and long T2 water-like signal in the synovial cavity of the left wrist joint (Fig. 3). The patient was diagnosed primarily with a postoperative of Kirschner wire internal fixation for epiphyseal injury, left lower ulnar–radial joint dislocation, left wrist deformity, and EPC.
Table 1.
Basic characteristics of patient.
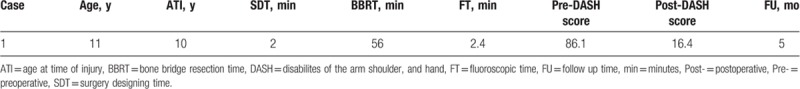
Figure 1.

(A) Frontal and (B) lateral radiographs of left wrist joint. An 11-year-old male patient displayed swelling and pain of the left wrist. According to the preoperative x-ray image, the distal part of the ulna is longer than that of radial (blue arrow).
Figure 2.
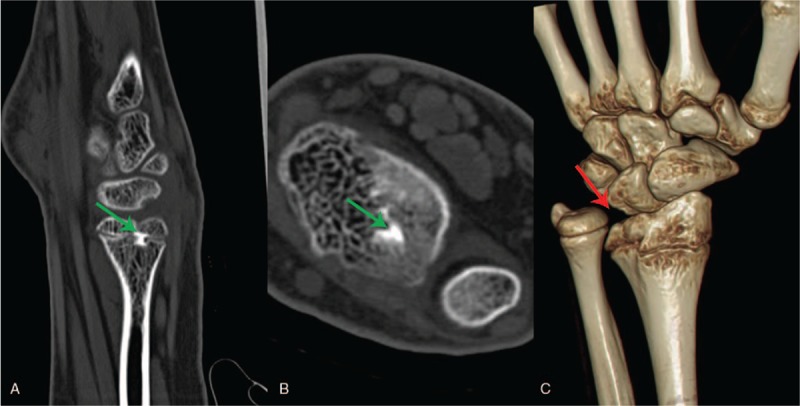
Preoperative 3D CT of left wrist joint. It showed a strip-like high density area (green arrow) below the epiphyseal plate of the distal radius (A–B), and abnormal wrist anatomy (red arrow) (C). 3D = three dimensional, CT = computed tomography.
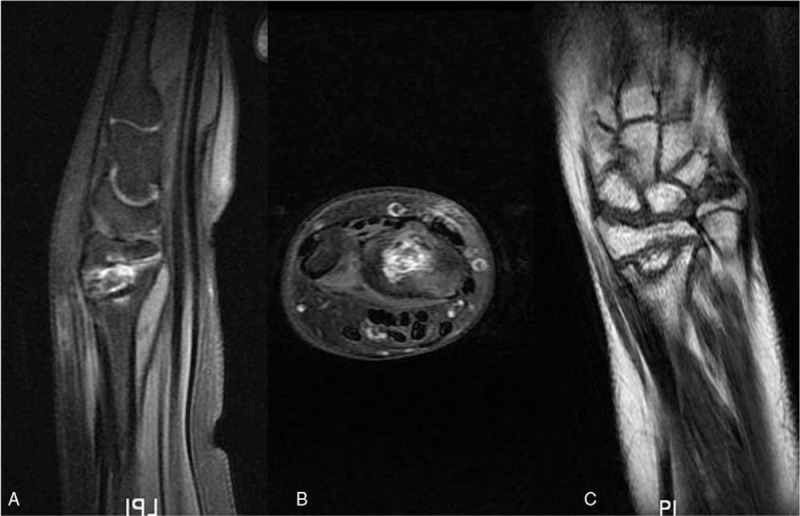
Figure 3.
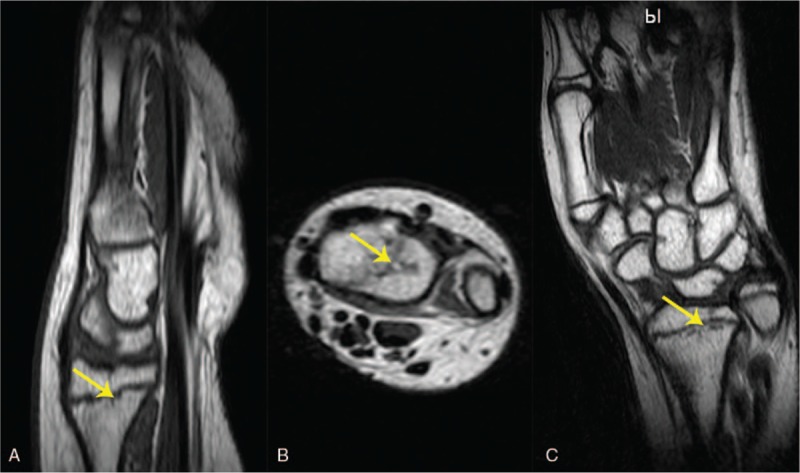
Preoperative MRI of left wrist joint. A small amount of long strip changes (yellow arrow) below epiphyseal plate was observed in sagittal (A), axial (B), and coronal (C) plate. MRI = magnetic resonance imaging.
3.2. Surgical procedures
3.2.1. General preparation
The patient underwent the operation under general anesthesia (intubation: Propofol, 200 μg/kg, Corden Pharma S.P.A. Viale dell’ Industria 320867 Caponago, Italy; fentanyl, 250 μg, RenFu LLC, YiChang, China; midazolam, 2 mg; maintenance: Propofol, 0.2–0.5 mg/kg/h, Enhua Pharmaceutical Limited by Share Ltd., JiangSu, China). Short-acting muscle relaxants were provided during the intubation only. Once the anesthesia took effect, the patient was placed in the supine position with abduction of left upper limb.
3.2.2. Image acquisition
At the beginning of the operation, a patient tracker (Stryker Leibinger GmbH & Co., Freiburg, Germany), piloted with the Navigation System II-CART II using a SpineMap 3D 2.0 software (Stryker Navigation, Kalamazoo, MI), was fixed on the left radius (Fig. 4). C-arm tracker, patient tracker, and guide wire sleeve tracker of the system were all activated. The left upper limb of the patient was tied to the operating table with a sterile bandage (Fig. 4). At the end of a 190° scan performed at the center of the EPC area, 3D images of the lesion were acquired.
Figure 4.

Clinical picture. The fixation method of the patient tracker (white arrow) and left upper limb (black arrow).
3.2.3. Surgical planning
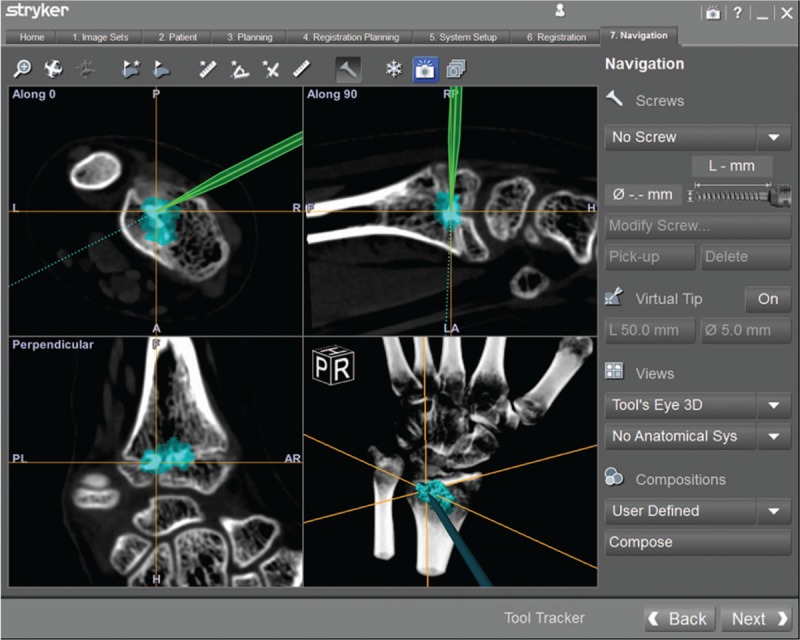
The navigation system presented multi-planar images of the radial epiphysis's bone bridge, helping to find the best surgery trajectory and the appropriate resection range of bone bridge (Fig. 5). In principle, surgical approach can avoid all nerves and vessels and achieve the complete removal of the bridge.
Figure 5.
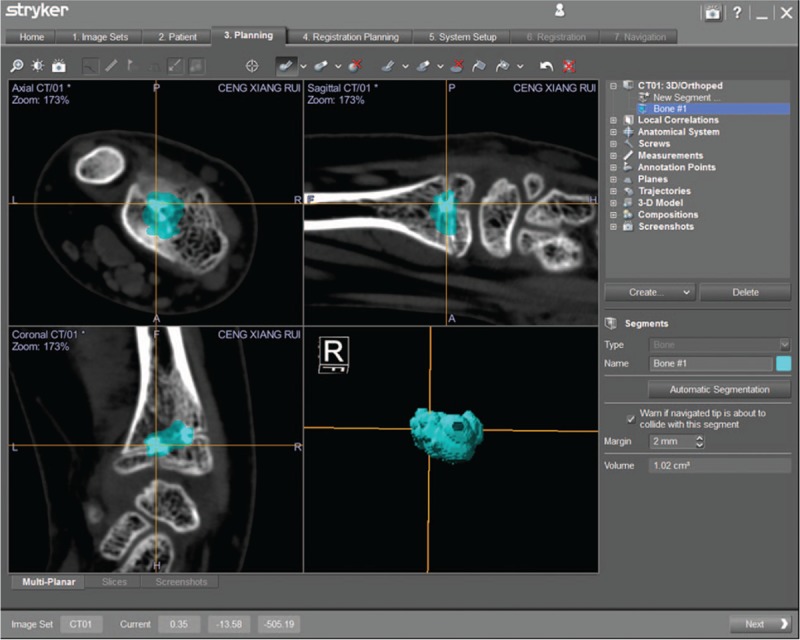
Surgical planning. The bone bridge was marked in blue at the workstation of navigation system.
3.2.4. Bone bridge resection
Tool's Eye model was selected through the navigation system on the workstation. With the use of the infrared camera, the surgeon can accurately determine the optimal entry direction of approach. After identifying the precise approach at the dorsal side of the distal radius, the skin was incised at nearly 1-cm from its center. The infrared camera continuously updated the navigated high-speed drill position on all displayed images simultaneously, giving real-time feedback of the designed resection range and the location of the surgical instruments when the surgeon moved the navigated drill (Fig. 6). It is worth noting that in the process of bone bridge removal, the bit of navigated drill should be continuously washed with normal saline to cool down, so as to avoid damage of nerve caused by heat conduction. Arthroscopic was used to detect whether the bone bridge removed completely (Fig. 7). Finally, exact closure of the wound without drainage was placed.
Figure 6.
Clinical picture. Bone bridge resection using a high-speed drill assisted by navigation.
Figure 7.
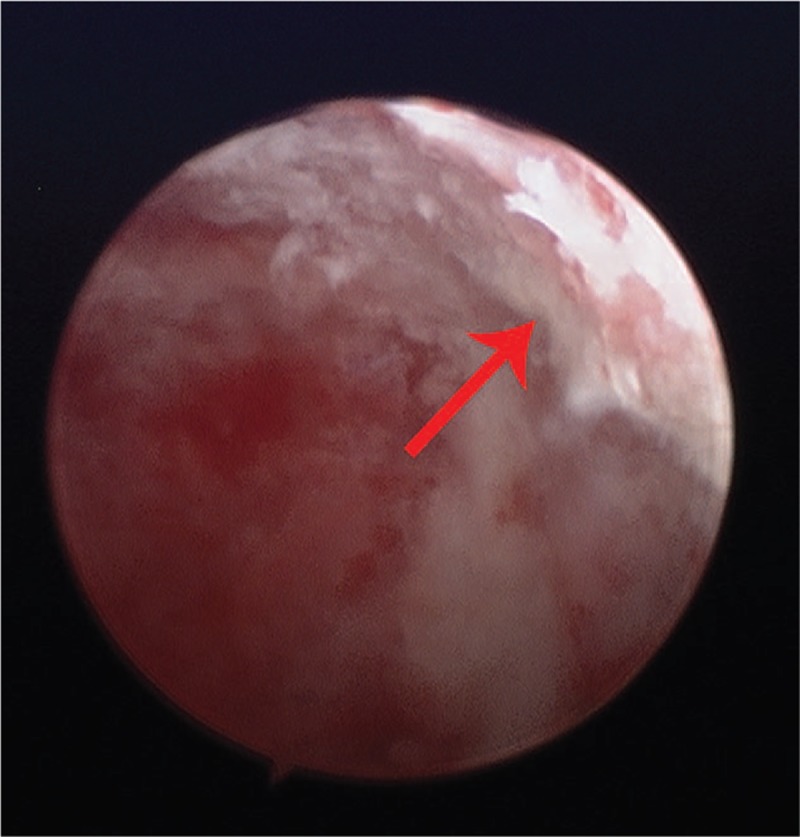
Clinical picture. Arthroscopy was used to check whether the bridge has been completely removed during surgery (red arrow).
3.3. Outcomes and follow-up
The pre- and postoperative disabilites of the arm, shoulder, and hand (DASH) score,[14] the degree of palmar flexion and dorsiflexion before and after surgery, and the degree of pronation and supination before and after operation were assessed. Also, age, sex, age at time of injures, surgery designing time, bone bridge resection time, and fluoroscopic time were assessed.
Postoperative x-ray imaging, three dimensional computed tomography (3D CT) scanning, and MRI (Figs. 8–10) completely showed the outcome of bone bridge resection. Pain was relieved clearly in the patient. Dorsiflexion increased from 60.8° to 85.3°, palmar flexion increased from 45.3° to 65.8°, supination increased from 41.3° to 69.5°, and pronation increased from 31.6° to 62.9° at the final visit time (Table 2). The preoperative DASH score was 86.1, which was increased to 16.4 postoperatively. Surgery designing lasted for 2 minutes, the bone bridge resection time lasted for 56 minutes, and the fluoroscopic time was 2.4 minutes (Table 1). At the fifth month of follow-up, it was found that the difference in length between radius and ulna was reduced (Fig. 8E). Complications, for example, neurological injury, vascular injury, infection and deformity aggressive, were not found during the 5-month follow up.
Figure 8.

Postoperative x-ray imaging 3 days (A, B) after surgery, 3 (C, D), and 5 months (E, F) follow up. The irregular density reduction area (blue arrow) below the epiphyseal plate of the left distal radius can be seen in the frontal and lateral positions. At the fifth month of follow-up, it was found that the difference in length between radius and ulna was reduced (red line).
Figure 10.
Postoperative MRI of sagittal (A), axial (B), and coronal (C) plate. The reexamination of MRI was performed 3 months after the operation. MRI = magnetic resonance imaging.
Table 2.
The degrees of palmarflexion, dorsiflexion, pronation, and supination pre- and postoperative.
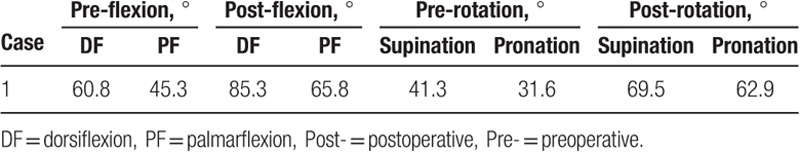
Figure 9.
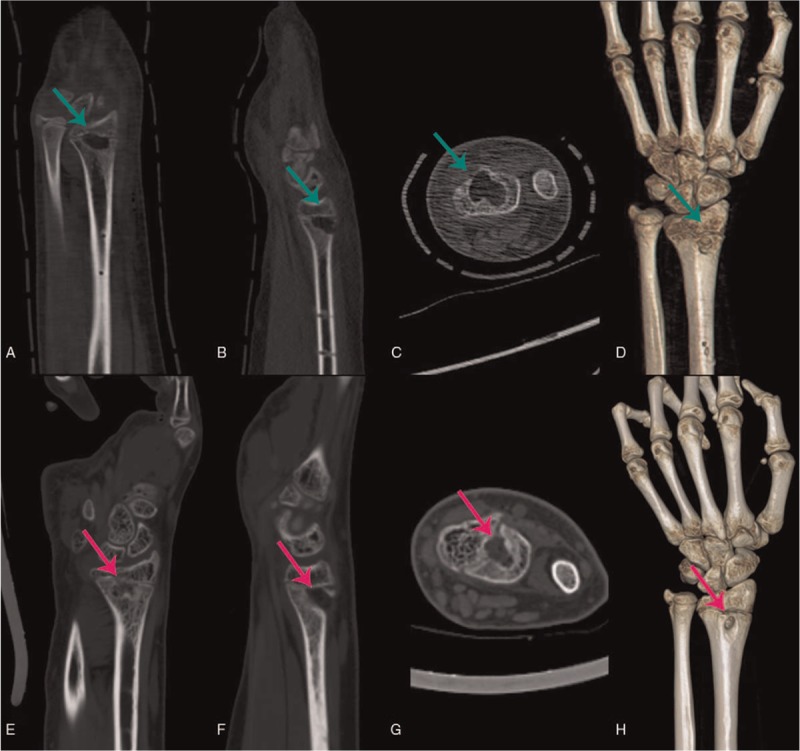
Three days after surgery (A–D) and 5 months (E–H) 3D CT was scanned. The images showed that the bridge has been completely removed (green arrow) and the volume of bone defect was decreased (pink arrow). 3D = three dimensional, CT = computed tomography.
4. Discussion
Corrective osteotomy was the primary treatment method for epiphyseal lesions.[7,9,15] However, there are many harmful complications.[8,9] In recent years, arthroscopy has become more and more popular in management in orthopedic surgery because of its minimally invasive approach.[11–13] In the meantime, computer navigation has been widely used in orthopedic surgery for preoperative design and intraoperative guidance.[10,16–18] To improve the bone bridge resection and minimize surgical risks, the advantages of navigated drilling and arthroscopy (NDA) were combined. An 11-year-old boy with EPC underwent bone bridge resection with the assistance of NDA. Here, dorsiflexion, palmar flexion, supination, pronation, and DASH score were improved effectively without harmful clinical complications postoperatively.
In children, distal radius epiphysis injury are primarily dorsally angulated.[19,20] The distal radius fracture of the forearm shows greater remodeling potential than the medial shaft fracture.[21] Because the distal radius growth plate accounts for 75% of the bone length,[22] with considerable potential for remodeling. Important factors affecting children's remodeling of forearm fracture also includes age and distance from growth plate. Studies have shown that children under 10 years old have the ability to correct 28° with their growth, but the ability to correct decreases when they are over 10 years old or above 28°.[23] Accordingly, many researchers believe that the timing of corrective surgery for angulation deformity should be >10 to 12 years old in children.[21,23–25] In this paper, the 11-year-old patient only showed radial deviation deformity rather than obvious dorsal angulation deformity. Instead of osteotomy, a bone bridge resection was performed, and it was believed that the subsequent growth would correct the deformity.[26] During the follow up, good results were achieved because of the combined application of NDA.
The malunion of this case, together with the relative elongation of the ulna, led us to make a retrospective diagnosis of growth arrest in this case. Here, the patient had a history of trauma and a significant growth potential at the age of 11. Gogna et al[6] claimed that growth retardation often occurs after epiphyseal injury of distal radius in children, leading to asynchronous growth of radius and ulna. The earlier epiphyseal closure is, the more obvious the deformity is. In the normal wrist, the radius and ulna bear 82% and 18% of the axial load, respectively. When the radius is shortened by 2.5 cm, the axial load of ulna increases to 42%.[27] The shorter the radius is, the greater load on the ulna will be, which will eventually lead to the symptoms of ulnocarpal impingement.[6] This is the reason of pain in the distal radioulnar joint and restricted range of motion around the wrist in this patient.
During the removal of the bone bridge with a navigated drill, the surgical assistant felt that the skin temperature of the distal radius of the patient was very high. Although the drill has been cooled with normal saline, we analyze that the heat is generated by the high-speed rotating friction of the navigated drill. To avoid the damage of heat conduction to peripheral soft tissues, such as nerves and blood vessels, we increased the speed of saline scouring high-speed drill, and reduced the speed of drilling. No complications occurred after operation.
Despite a positive outcome has achieved for the use of the NDA in this case, several matters are still under consideration. First, certainly the operation should not be performed at an age when too little growth is left to allow correction of deformity or some gain in bone length, yet the age limits cannot be defined. Second, how large abridge may be resected with an acceptable clinical result remains unclear. A major loss of cartilage from trauma or disease probably suggests that the closure of the entire plate will be premature even if the bridge has been entirely removed. Indeed, the indications and the results of the operation were affected by the variations in the size and situation of a bone bridge causing growth disturbance and vascular problems. Third, the follow-up time was relatively short. These questions may be at least partially answered by further experimental work on animals and long-term follow-up.
5. Conclusions
To sum up, the bone bridge resection assisted by navigated drill and arthroscopy is a simple and highly feasible procedure for surgeons. An experience was gained that in the process of bone bridge removal, the bit of navigated drill should be continuously washed with normal saline to cool down, so as to avoid damage of nerve caused by heat conduction.
Author contributions
Conceptualization: Qi-Wei Li, Xi-Wen Zhang.
Methodology: Yi-Kun Jiang, Li-Heng Kang.
Project administration: Qian Wang.
Writing – original draft: Tong Yu, Bao-Ming Yuan.
Writing – review & editing: Dan-Kai Wu, Jian-Wu Zhao.
Footnotes
Abbreviations: 3D = three dimensional, CT = computed tomography, DASH = disabilites of the arm, shoulder, and hand, EPC = epiphyseal premature closure, MRI = magnetic resonance imaging, NDA = navigated drilling and arthroscopy.
TY and BMY have contributed equally to this work.
This study was supported by department of science and technology of Jilin province (CN) (No. 20190304123YY).
The authors declare that they have no conflict of interest.
References
- [1].Chen AC, Cheng CY, Chou YC. Intramedullary nailing for correction of post-traumatic deformity in late-diagnosed distal radius fractures. J Orthop Traumatol 2017;18:37–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Kardouni JR. Child with dinner fork deformity. Distal radius fracture. Ann Emerg Med 2016;67:165188. [DOI] [PubMed] [Google Scholar]
- [3].Miyake J, Murase T, Yamanaka Y, et al. Three-dimensional deformity analysis of malunited distal radius fractures and their influence on wrist and forearm motion. J Hand Surg Eur Vol 2012;37:506–12. [DOI] [PubMed] [Google Scholar]
- [4].Li M, Liu R, Gao J, et al. Ilizarov technique for treatment of distal radius deformity and bone defect after trauma. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 2018;32:1275–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Singh A, Singh OP. A rare injury of distal radial and ulnar epiphysis. J Indian Med Assoc 2007;105:466468. [PubMed] [Google Scholar]
- [6].Gogna P, Gaba S, Mukhopadhyay R, et al. Neglected epiphyseal injuries of the distal end of the radius with ulnar impaction: analysis of distal osteotomy of both bones using a dorsal midline approach. J Orthop Traumatol 2017;18:31–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Meyerding H, Overton L. Malunited fracture of the lower end of the radius (Colles’ fracture) treated by osteotomy. Minn Med 1935;18:84–9. [Google Scholar]
- [8].Tyler PA, Rajeswaran G, Saifuddin A. Imaging of dysplasia epiphysealis hemimelica (Trevor's disease). Clin Radiol 2013;68:415–21. [DOI] [PubMed] [Google Scholar]
- [9].Oberc A, Sulko J, Szydlowski M. Dysplasia epiphysealis hemimelica - diagnostics and treatment in pediatric patients. Pol Orthop Traumatol 2014;79:41–4. [PubMed] [Google Scholar]
- [10].Yu T, Wang GS, Qu Y, et al. Posterior hemivertebra resection with a navigated drilling method for congenital scoliosis: a case report and description of surgical technique. Int J Clin Exp Med 2017;10:15562–8. [Google Scholar]
- [11].Qian H, Chen G, Liu Z. Treatment of distal radioulnar joint dislocation with spontaneous rupture of extensor tendon by Sauve-Kapandji osteotomy assisted by wrist arthroscopy: a case series and literature review. Medicine (Baltimore) 2018;97:e10752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Hoel RJ, Mittelsteadt MJ, Samborski SA, et al. Preoperative antibiotics in wrist arthroscopy. J Hand Surg Am 2018;43:987.e1–91.e1. [DOI] [PubMed] [Google Scholar]
- [13].Longo UG, Loppini M, Del Vescovo R, et al. Safety of dorsal wrist arthroscopy portals: a magnetic resonance study. Surgeon 2018;16:101–6. [DOI] [PubMed] [Google Scholar]
- [14].Koorevaar RCT, Kleinlugtenbelt YV, Landman EBM, et al. Psychological symptoms and the MCID of the DASH score in shoulder surgery. J Orthop Surg Res 2018;13:246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Vogel T, Skuban T, Kirchhoff C, et al. Dysplasia epiphysealis hemimelica of the distal ulna: a case report and review of the literature. Eur J Med Res 2009;14:272–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Li QJ, Yu T, Liu LH, et al. Combined 3D rapid prototyping and computer navigation facilitate surgical treatment of congenital scoliosis: a case report and description of technique. Medicine (Baltimore) 2018;97:e11701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Chachan S, Bin Abd Razak HR, Loo WL, et al. Cervical pedicle screw instrumentation is more reliable with O-arm-based 3D navigation: analysis of cervical pedicle screw placement accuracy with O-arm-based 3D navigation. Eur Spine J 2018;27:2729–36. [DOI] [PubMed] [Google Scholar]
- [18].Du JP, Fan Y, Wu QN, et al. Accuracy of pedicle screw insertion among 3 image-guided navigation systems: systematic review and meta-analysis. World Neurosurg 2018;109:24–30. [DOI] [PubMed] [Google Scholar]
- [19].Aitken A. The end results of the fractured distal radial epiphysis. J Bone Jt Surg 1935;17:302–8. [Google Scholar]
- [20].Aitken A. Further observations on the fractured distalradial epiphysis. J Bone Jt Surg 1935;17:922–7. [Google Scholar]
- [21].Gandhi RK, Wilson P, Mason Brown JJ, et al. Spontaneous correction of deformity following fractures of the forearm in children. Br J Surg 1962;50:5–10. [DOI] [PubMed] [Google Scholar]
- [22].Salter R, Harris W. Injuries involving the epiphyseal plate. J Bone Jt Surg Am 1963;45:587–622. [Google Scholar]
- [23].Larsen E, Vittas D, Torp-Pedersen S. Remodeling of angulated distal forearm fractures in children. Clin Orthop 1988;237:190–5. [PubMed] [Google Scholar]
- [24].Crawford AH. Pitfalls and complications of fractures of the distal radius and ulna in childhood. Hand Clin 1988;4:403–13. [PubMed] [Google Scholar]
- [25].Davis DR, Green DP. Forearm fractures in children: pitfalls and complications. Clin Orthop Relat Res 1976;172–83. [PubMed] [Google Scholar]
- [26].Langenskiold A. An operation for partial closure of an epiphysial plate in children, and its experimental basis. J Bone Joint Surg Br 1975;57:325–30. [PubMed] [Google Scholar]
- [27].Gogna P, Selhi HS, Mohindra M, et al. Ulnar styloid fracture in distal radius fractures managed with volar locking plates: to fix or not? J Hand Microsurg 2014;6:53–8. [DOI] [PMC free article] [PubMed] [Google Scholar]


