Abstract
Rationale:
For hip or knee arthroplasty, it is essential to develop a satisfied peripheral nerve block method that will benefit elderly patients or patients who are contraindicated to neuraxial anesthesia.
Patients concerns:
Patient in Case 1 suffered from the right intertrochanteric fracture, combined with chronic obstructive pulmonary disease; Patient in Case 2 suffered from hip osteoarthritis; combined with ankylosing spondylitis; Patient in Case 3 suffered from rheumatoid arthritis, combined with ischemic encephalopathy.
Diagnosis:
Case 1: Right intertrochanteric fracture, chronic obstructive pulmonary disease. Case 2: hip osteoarthritis. Case 3: rheumatoid arthritis.
Interventions:
Ultrasound-guided lumbar selective nerve root block (SNRB) plus T12 paravertebral and sacral plexus block were performed in 2 patients who received hip arthroplasty and 1 patient who received knee arthroplasty.
Outcomes:
All patients successfully received surgeries with this peripheral nerve block method and no postoperative complication was reported.
Lessons:
Ultrasound-guided lumbar SNRB plus T12 paravertebral and sacral plexus block not only satisfied the analgesia requirement of surgery, but also reduced the consumption of local anesthetic.
Keywords: arthroplasty, hip, knee, paravertebral block, sacral plexus block, selective nerve root block, ultrasound
1. Introduction
Quick returning to functional training, early oral feeding, reducing postoperative complications were thought to be vital to recovery of patients who received hip and knee arthroplasty.[1] Regional anesthesia, especially peripheral nerve block, could be the preferable anesthesia method to achieve these goals.[2]
Lumbar selective nerve root block (SNRB) is an effective diagnostic and treatment for patients with lumbar radicular pain.[3] With the guidance of CT and ultrasound, the lumbar SNRB has been widely used in pain clinical practice but not anesthetic clinical practice.[4]
In here, we described a novel regional anesthesia method—ultrasound-guided lumbar SNRB plus T12 paravertebral block and sacral plexus block, and reported its application on 3 patients who received hip and knee arthroplasty.
2. Methods
2.1. Ethical approval and patient consent for publication
Ethical approval for this report (PJ2017-08-19) was provided by the Ethical Committee of The First Affiliated Hospital of Anhui Medical University, Hefei, China on August 7, 2015. Prior to surgery, the written informed consent was obtained from the patients and their relatives, and the case details were approved for publication by all patients.
2.2. Anesthetic technique
After a monitor of vital signs was established, light sedation was achieved with a bolus of dexmedetomidine (manufactured by Sichuan Guorui Medicine Co, Sichuan, China) at 0.6 to 0.8 μg/kg (over a period of 20 min) and followed by an infusion at 0.2 to 0.5 μg/kg/h. All patients received the peripheral nerve block 30 minutes after the sedative drugs were infused. The patient was placed in the lateral position with the operated side uppermost. An Edge ultrasound (FUJIFILM SonoSite Inc, Bothell, WA) and a 2 to 5 MHz convex transducer (FUJIFILM SonoSite Inc, Bothell, WA) were used, and the surface anatomic landmarks were made for reference (Fig. 1).
Figure 1.
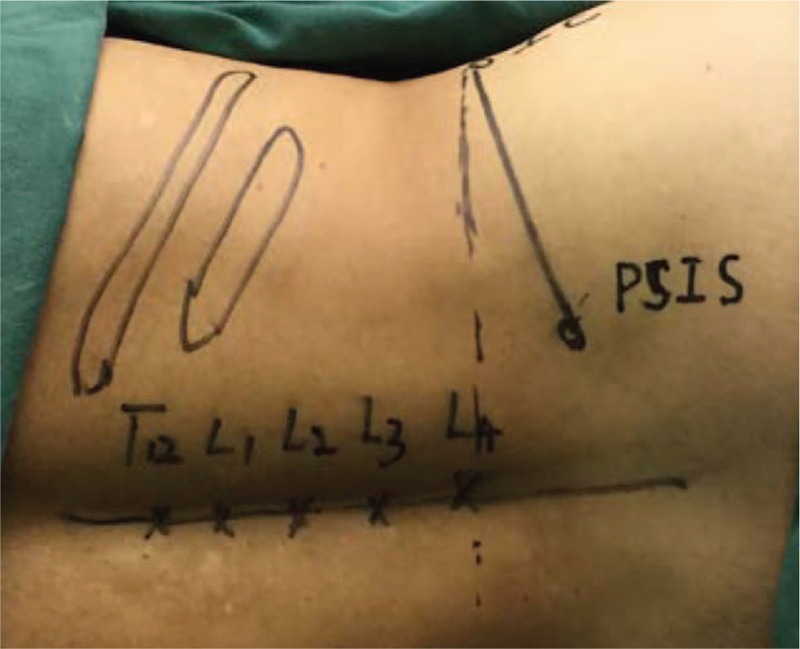
The surface anatomic landmarks for block. IC = iliac crest, PSIS = posterior superior iliac spine.
T12 paravertebral block was performed as described previously.[5] In brief, the ultrasound probe was placed parallel to the posterior median line to identify the 12th rib, and then rotated 90 degrees to visualize the transverse process of the 12th rib (Fig. 2F). After scanning slightly inferiorly, the thoracic paravertebral space (TPVS) was found anterior to the transverse process and appeared as a triangle space bordered by the inferior articular process, intertransverse ligament, and the diaphragm (Fig. 2B). A 9-cm 22G needle (KDL Medical Company, Zhejiang, China) was inserted and advanced in plane with the transducer, in a lateral-to-medial direction. After the needle reached the TPVS, 3 mL of 0.4% ropivacaine was injected.
Figure 2.
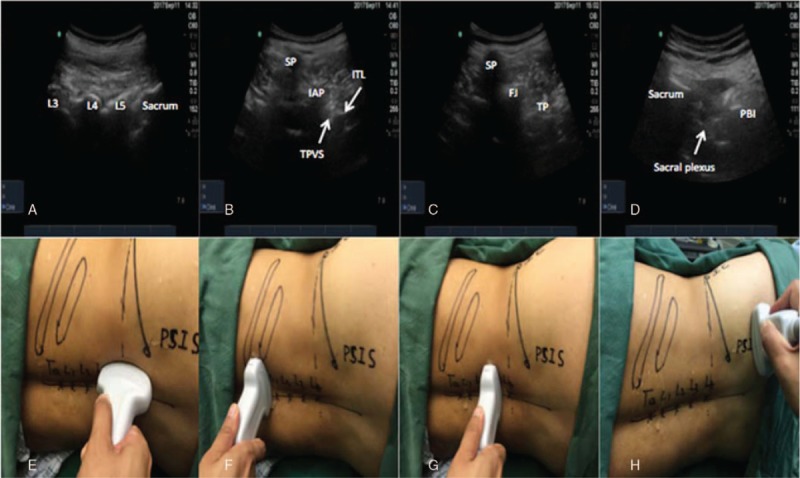
Ultrasonography of blocks and positions of transducer. A, Identify the different spinal segments with longitudinal facet views when placing transducer as in panel E. B, Ultrasonography for T12 paravertebral block, when transducer was positioned as in panel F. C, Ultrasonography for lumbar selective nerve root block, when transducer was positioned as in panel G. D, Ultrasonography for Sacral plexus block, when transducer was positioned as in panel H. AP = articular process, FJ = facet joint, IAP = inferior articular process, ITL = intertransverse ligament, PBI = posterior border of ischium, SP = spinous process, TP = transverse process, TPVS = thoracic paravertebral space.
Selective lumbar SNRB was performed in an order of L4, L3, L2, and L1. To identify different spinal segments, longitudinal facet views were obtained by placing the transducer parallel to the posterior median line (Fig. 2E).[6] Started from L5 (Fig. 2A), at the level of each segment, the probe was rotated 90 degrees to obtain the transverse axial images in which the spinous process, facet joint, and transverse process were found from medial to lateral, respectively (Fig. 2G). Foramen intervertebral was identified as the space between the facet joint and transverse process after scanning slightly cephaladly (Fig. 2C). The needle was inserted and advanced in plane with the transducer, in a lateral-to-medial direction. Once the needle touched the lateral of the facet joint, the angle of needle was increased to over facet joint and then forwarded 1 cm deeper. C-arm was used to evaluate the position of the needle tip (Fig. 3), and 3 mL of 0.4% ropivacaine was injected for each segment.
Figure 3.
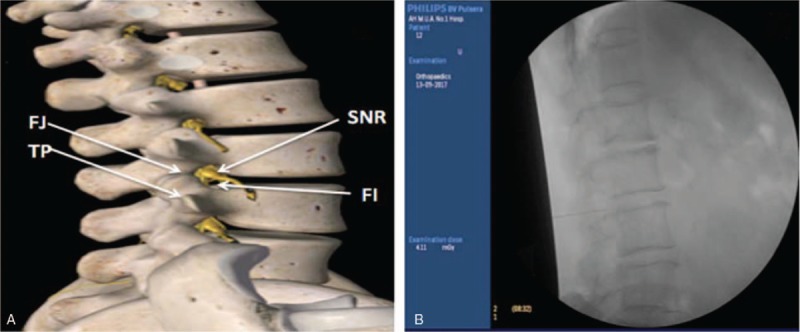
Anatomical drawing of spinal nerve root and confirmation of tip of needle by C-arm. A, Anatomical drawing of spinal nerve root and other related structures of lumbar. B, The final position of tip of needle was confirmed by C-arm in Case 1 when lumbar selective nerve root block was performed. FI = foramen intervertebral, FJ = facet joint, SNR = spinal nerve root, TP = transverse process.
Sacral plexus block was performed as described previously.[7] In brief, the probe was placed transversely at the level of the sacral hiatus lateral to the midline (Fig. 2H) to reveal the posterior border of the ischium as a hyperechoic line. The greater sciatic foramen was found as a gap after sliding the probe caudally. The sacral plexus was identified as a hyperechoic structure, which was deep to the piriformis (Fig. 2D). The needle was inserted and advanced in plane with the transducer. 10 mL of 0.4% ropivacaine was injected once the needle tip nearly reached the target nerve.
The successful nerve block was confirmed by pinprick test 20 minutes after the block. The hip surgery was performed via a posterior approach.
3. Cases description
3.1. Case 1
An 84-year-old female (body weight 56 kg, ASA status III) was scheduled for right artificial femoral head replacement. Her pelvic X-ray revealed a right intertrochanteric fracture. She had hypertension for 35 years and chronic obstructive pulmonary disease (COPD) for 20 years. She took daily oral nifedipine for hypertension, but did not take any treatment for COPD. The result of pulmonary function test showed that the FEV1/FVC was 35% and the bronchodilator test was negative. Cardiac Doppler ultrasonography indicated moderate pulmonary artery hypertension. A chest X-ray revealed pulmonary infection of bilateral lower lobes. Low-molecular-weight heparin was used for prevent thrombus formation at 4000IU per day and stopped 24 hours before surgery. The preoperative visual analogue scale (VAS) score of this patient was 6. The ultrasound guided lumbar SNRB plus T12 paravertebral and sacral plexus blocks were performed on this patient as described in the Methods section, and 25 mL of 0.4% ropivacaine was used for these blocks. The success of these blocks was confirmed by pinprick test. The time of surgery was 42 minutes. She did not complain any painful during surgery and in postanesthesia care unit (PACU). As postoperative analgesia was achieved by patient-controlled analgesia (PCA), the postoperative VAS scores were 0 to 1. This patient discharged on the fifth day after surgery. No postoperative complication was reported with her.
3.2. Case 2
A 46-year-old male (body weight 69 kg, ASA status II) was scheduled for right total hip arthroplasty (THA). He suffered from ankylosing spondylitis for 20 years. Physical examination indicated that the cervical and lumbar spine was rigid and the right hip joint was immobilized. The bamboo-like changes of spine were found in the spinal anterioposterior and lateral radiographs (Fig. 4). X-ray and CT examination indicated degenerative osteoarthrosis of bilateral hip joints and sacroiliitis on the right side. The patient appeared potentially difficult to be intubated as the examination of airway revealed that the interincisor distance was 2 cm and a Mallampati class III. The preoperative visual analog scale (VAS) score of this patient was 4. This patient received ultrasound-guided lumbar SNRB plus T12 paravertebral and sacral plexus blocks, and 25 mL of 0.4% ropivacaine was used. Pinprick test was used to confirm the success of these blocks. The time of surgery was 1 hour and 26 minutes. He also did not complain any painful during surgery and in PACU. With the PCA, the postoperative VAS scores were 0 to 1. This patient discharged on the second day after surgery. No postoperative complication was reported with him.
Figure 4.
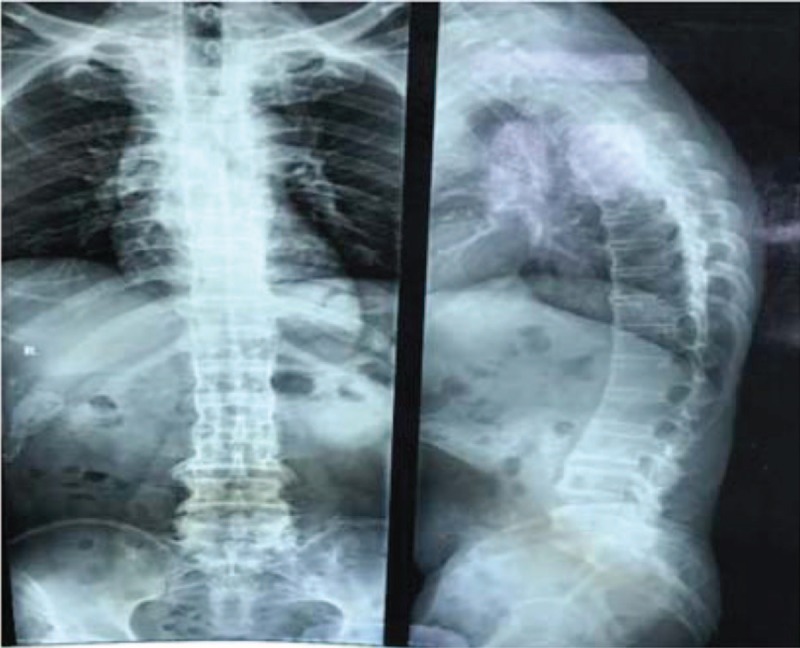
The spinal anterioposterior and lateral radiographs of patient in Case 2. The bamboo-like changes of spine can be found in the radiograph.
3.3. Case 3
A 73-year-old female (body weight 64 kg, ASA status III) who suffered from rheumatoid arthritis (RA) for 30 years was scheduled for right total knee arthroplasty (TKA). X-ray of her bilateral knee joint revealed that the joint cavity of bilateral knee joints was narrow and osteophyte formatted in the right side. The patient had hypertension for 6 years and was treated with oral nitrendipine. She also had a history of cerebral infarction 3 years ago. MRI of brain revealed multiple old softening foci in the right basal ganglia region. She had taken aspirin and ginkgo tablets for anticoagulation therapy and prevention of recurrent stroke. The preoperative visual analog scale (VAS) score of this patient was 4. The ultrasound-guided lumbar SNRB plus T12 paravertebral and sacral plexus blocks were performed with 25 mL of 0.4% ropivacaine. Pinprick test was used to confirm the success of these blocks. This technique completely met the analgesic requirement of this patient during surgery. The time of surgery was 1 hour and 12 minutes. With the PCA, the postoperative VAS scores were 0 to 1. This patient discharged on the third day after surgery. No postoperative complication was reported with her.
4. Discussion
To our knowledge, the innervation of the hip joint was derived from the lumbar plexus (L2–4) and part of the sacral plexus (L4-S1). For analgesia requirement of skin incision of posterolateral approach to hip surgery, it was necessary to block the lateral femoral cutaneous nerve from the lumbar plexus (L2–3), lateral cutaneous branch of iliohypogastric nerve (T12 and L1), and subcostal nerve (T12 thoracic nerve).[8] For knee arthroplasty, the primary relevant target nerves were femoral, obturator, sciatic, and lateral femoral cutaneous.[9] To relieve the uncomfortable stress of application of tourniquet, T12 paravertebral block also was necessary. The ultrasound-guided lumbar SNRB plus T12 paravertebral and sacral plexus block we performed on these 3 patients fully satisfied the analgesia requirement of surgery.
The 3 patients had different clinical conditions, thus managements were slightly different. In case 1, the patient had a long-term hypertension and COPD; artificial airway was avoided and respiratory complications were avoided. In case 2, the patient had ankylosing spondylitis; the probable difficulty of puncture of neuraxial anesthesia was avoided. In case 3, the intraoperative stable hemodynamics were important, which was not too difficult to manage during operation with the blocking method. The nerve blocks only on the side that received surgery facilitated early stage derogation for these patients. However, although neuraxial anesthesia is the most popular anesthesia method for patients who received hip and knee surgery,[10] it has been reported that complications and contraindications, for example, urinary retention, hypotension, spinal hematoma perioperative anticoagulation, meningitis and spinal abscess, may limit the application of neuraxial anesthesia in some patients.[11,12]
Combination of lumbar plexus and parasacral plexus block for hip surgery has been reported before. In previous studies, additional large amount of propofol and infiltration to the incision were used as the supplement, and a large amount of local anesthetic was required to obtain an effective block.[8] In the cases we reported here, we performed multiple selective nerve blocks which satisfied the required of surgery but used much less amount of local anesthetic.
Dexmedetomidine was used for intraoperative sedation in these cases. Intraoperative sedation has benefits of avoiding postural discomfort, preventing intraoperative recall, and reducing sympathetic and parasympathetic reflexes. Recently, dexmedetomidine was also reported having positive effect on elderly patients recovery outcomes.[13] We believe that intraoperative light sedation is an ethical practice and necessary for patient care.
The evidence from 3 cases may be not stronger enough to evaluate the safety and effeteness of the block method described in this study. To avoid the probable nerve root injury and epidural infiltration, controlling volume of local anesthetics and precisely placing the tip of needle must be very important.[6] In the future, additional prospective clinical trial is needed to supply adequate evidence.
Acknowledgments
The authors thank professor Ming Zhang (Department of Anatomy, Otago School of Biomedical Sciences, New Zealand) for suggestions and help regarding the writing in English. The authors also thank all the staff of Department of Anesthesiology, First Affiliated Hospital of Anhui Medical University for being helpful in conducting and finishing this research.
Author contributions
Conceptualization: Bin Mei, Yao Lu.
Formal analysis: Bin Mei.
Investigation: Bin Mei.
Methodology: Ye Zhang, Erwei Gu.
Project administration: Shishou Chen.
Writing – original draft: Bin Mei.
Writing – review & editing: Yao Lu, Xuesheng Liu, Ye Zhang, Erwei Gu.
Shishou Chen orcid: 0000-0003-3400-0466.
Footnotes
Abbreviations: AS = ankylosing spondylitis, ASA = American Society of Anesthesiologists, COPD = chronic obstructive pulmonary disease, PACU = postanesthesia care unit, PCA = patient-controlled analgesia, SNRB = selective nerve root block, THA = total hip arthroplasty, VAS = visual analogue scale.
This study was partly supported by National Natural Science Foundation of China (No. 81770295).
The authors have no conflicts of interest to disclose.
References
- [1].Perlas A, Chan VW, Beattie S. Anesthesia technique and mortality after total hip or knee arthroplasty: a retrospective, propensity score-matched cohort study. Anesthesiology 2016;125:724–31. [DOI] [PubMed] [Google Scholar]
- [2].Husted H, Lunn TH, Troelsen A, et al. Why still in hospital after fast-track hip and knee arthroplasty? Acta Orthop 2011;82:679–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Wolff AP, Groen GJ, Crul BJ. Diagnostic lumbosacral segmental nerve blocks with local anesthetics: a prospective double-blind study on the variability and interpretation of segmental effects. Reg Anesth Pain Med 2001;26:147–55. [DOI] [PubMed] [Google Scholar]
- [4].Manchikanti L, Abdi S, Atluri S, et al. An update of comprehensive evidence-based guidelines for interventional techniques in chronic spinal pain. Part II: guidance and recommendations. Pain Physician 2013;162 suppl:S49–283. [PubMed] [Google Scholar]
- [5].Krediet AC, Moayeri N, van Geffen GJ, et al. Different approaches to ultrasound-guided thoracic paravertebral block: an illustrated review. Anesthesiology 2015;123:459–74. [DOI] [PubMed] [Google Scholar]
- [6].Kim D, Choi D, Kim C, et al. Transverse process and needles of medial branch block to facet joint as landmarks for ultrasound-guided selective nerve root block. Clin Orthop Surg 2013;5:44–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Taha AM. A simple and successful sonographic technique to identify the sciatic nerve in the parasacral area. Can J Anaesth 2012;59:263–7. [DOI] [PubMed] [Google Scholar]
- [8].Ke X, Li J, Liu Y, et al. Surgical anesthesia with a combination of T12 paravertebral block and lumbar plexus, sacral plexus block for hip replacement in ankylosing spondylitis: CARE-compliant 4 case reports. BMC Anesthesiol 2017;17:86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Johnston DF, Sondekoppam RV, Uppal V, et al. Hybrid blocks for total knee arthroplasty: a technical description. Clin J Pain 2017;[Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- [10].Hunt LP, Ben-Shlomo Y, Clark EM, et al. 90-day mortality after 409,096 total hip replacements for osteoarthritis, from the National Joint Registry for England and Wales: a retrospective analysis. Lancet 2013;382:1097–104. [DOI] [PubMed] [Google Scholar]
- [11].Schelew BL, Vaghadia H. Ankylosing spondylitis and neuraxial anaesthesia—a 10 year review. Can J Anaesth 1996;43:65–8. [DOI] [PubMed] [Google Scholar]
- [12].Buckenmaier CC, Xenos JS, Nilsen SM. Lumbar plexus block with perineural catheter and sciatic nerve block for total hip arthroplasty. J Arthroplast 2002;17:499–502. [DOI] [PubMed] [Google Scholar]
- [13].Su X, Meng ZT, Wu XH, et al. Dexmedetomidine for prevention of delirium in elderly patients after non-cardiac surgery: a randomised, double-blind, placebo-controlled trial. Lancet 2016;388:1893–902. [DOI] [PubMed] [Google Scholar]


