Abstract
The number of elective day-case surgeries has considerably increased in recent years, especially in China. Few studies have investigated the ability of mobile applications to assist recovery for patients having undergone day-surgery; however, these studies have indicated that the use of mobile applications is cost-efficient and has a positive effect on recovery after surgery. This study aimed to evaluate the utility and efficacy of using the 317-nursing mobile application program (317NAPP) for monitoring home recovery following day-surgery involving high ligation of the hernial sac in pediatric patients.
Prospective clinical study involving 2 parallel groups.
Patients were randomly divided into the “intervention 317NAPP group” (n = 64) and the control group (n = 63). Patients were followed-up using the 317NAPP in the intervention group and via telephonic consultations in the control group. All patients were enrolled after being provided sufficient guidance with respect to discharge and health education. The health index, including the physiological function, ability to perform daily activities, and the injury response, was evaluated before and 24 hours after surgery. The time duration of each follow-up session was also evaluated in both groups.
The preoperative (T1) health index scores were significantly higher than the postoperative (T0) ones in both groups (P = .00). The quality of recovery (T1–T0) of the intervention group (10.75 ± 5.28) was better than that of the control group (11.78 ± 5.16), but the differences were not significant (P = .27). In the intervention group, the follow-up time duration was significantly lower in comparison to that in the control group (P = .00).
This study demonstrated that 317NAPP had a positive effect on recovery following day-surgery, and the time-duration for follow-up was shorter than that performed using telephonic consultation. Monitoring recovery using 317NAPP was safe, efficient, inexpensive, and relatively easy; therefore, it may help improve the recovery of patients having undergone day-surgery.
Keywords: applications, day surgery, follow-up, nursing care, smartphone
1. Introduction
The concept of elective surgery is undergoing considerable changes, with an increasing emphasis on minimal hospital stays.[1,2] In China, approximately 10% to 20% of elective surgeries are performed via the day-case approach; moreover, the prevalence of day-case surgeries has considerably increased in recent years owing to a shortage in medical supplies resulting from the universal 2-child policy. This increase is equally attributed to advances in minimally invasive laparoscopic surgical techniques, improved anesthetic practices, increased use of short-acting/regional anesthetics, and patient preference for minimal hospital stay.[3–5] However, this has also resulted in reduced nurse–patient/caregiver contact during the acute phase of surgery with the majority of cases involving home recovery with little access to professional support. Generally, brief nurse–patient/caregiver interactions and timely information delivery following day surgery is expected. Here, we investigated additional tools for successful and trouble-free home recovery.
1.1. Background
To assist home recovery after day surgery, several tools have been previously reported. Telephone support after surgery is associated with several valuable aspects, including reassurance, information provision, and the chance to ask questions; however, the disadvantages include excessive time-consumption, interruption of routine work, and a chance to easily miss the delivery of professional support.[6–8] Automated-interactive voice-response telephone calls following discharge have successfully[9] addressed some patients’ requirement for further support (new problems related to surgery, worsening symptoms, and medication-related issues). Patients were given mobile phones with built-in cameras that returned essential information (such as images) to help modify treatment.[10] It was suggested that novel applications could be used to improve postsurgical care with new-generation mobile phones. Mobile applications are portable (convenient), popular, can provide precise information, and are interactive; therefore, they are being gradually implemented in the field of medical care.[11,12] Previous studies have demonstrated the advantages of using mobile applications in managing patients with chronic diseases.[13,14]
While day-surgery retains much public support, home recovery can be problematic resulting from reduced nurse–patient/caregiver contacts, a lack of information, limited adherence to instructions, inadequate analgesia, forgetting of instructions/information, and caregiver responsibility. With such issues, the 317-nursing mobile application program (317NAPP), composed of 3 modules (for the patient, the nurse, and the administrator) was developed to assist home recovery following day surgery in children.
1.2. Aim and objectives of the study
This study aimed to evaluate the utility and efficacy of using the 317NAPP for home recovery following day-surgery in children. Our hypothesis was that patients who receive standard care and are supported by the 317NAPP following day-surgery would experience better recovery with less time-consuming support than those who only receive standard care; moreover, recovery follow-up for day-surgery was expected to be more efficient.
2. Method
2.1. Study design
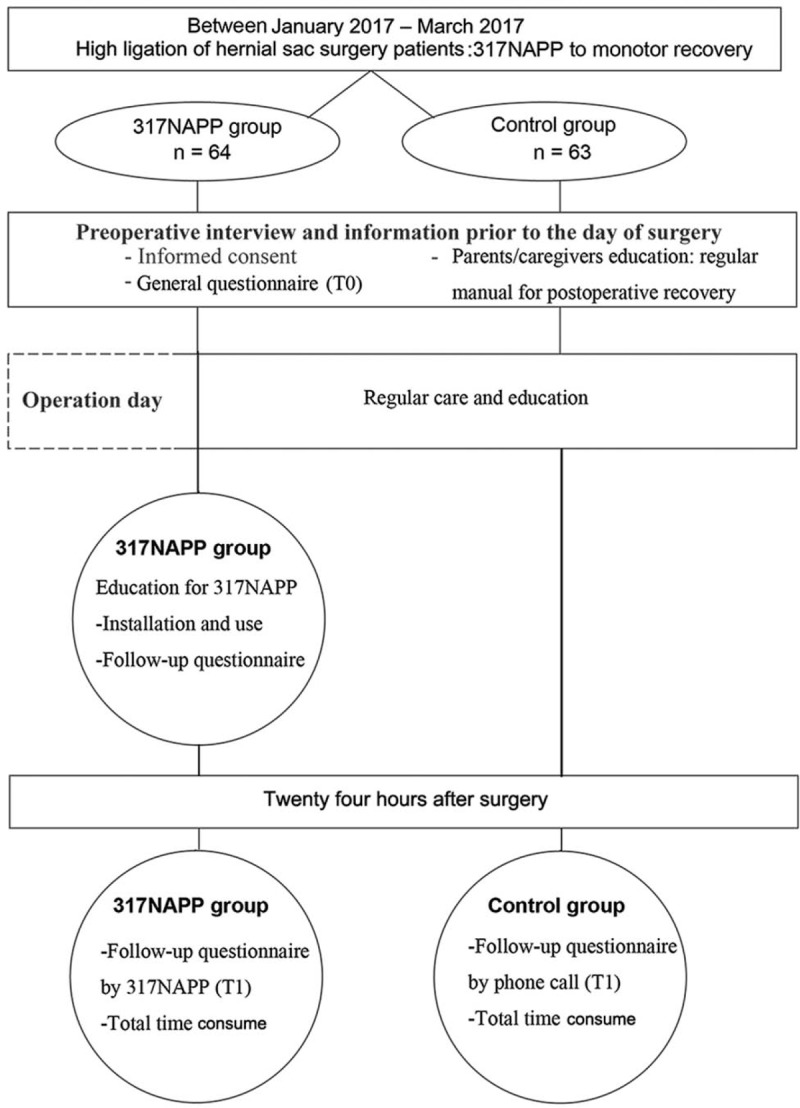
This was a prospective clinical study with patients divided into the 317NAPP group and the telephone-call group (control group). The inclusion criteria were as follows: children diagnosed with indirect inguinal hernia, with American Society of Anesthesiologists grade I–II; postsurgical caregivers had primary levels of education and/or higher; caregivers could answer phone calls; caregivers were equipped with smartphones having the WeChat app installed, and the caregivers were skilled in using the app; and informed consent was obtained from the parents/guardians of the patients. The exclusion criteria were as follows: caregivers were unable to listen using a telephone and were unable to use smartphones to access networks (see Fig. 1).
Figure 1.

Study flow chart.
The parents of participants in both groups were asked to complete a questionnaire before the surgery (mainly including the physical condition and daily activities of children). Caregivers were educated on postsurgical recovery including aspects of rehabilitation, diet, activities, and the information parents need to concern, using a manual. The questionnaire was designed to avoid differences between individuals and to ensure the quality of follow-up (Fig. 2).
Figure 2.
Study design.
2.2. Patients and setting
Between January and March 2017, children (1–18 years) having undergone surgery involving high ligation of the hernial sac at the Children's Hospital School of Medicine Zhejiang University in China, were enrolled in the study to form a total sample size of 179 patients (Fig. 2). Ten patients refused to participate, 4 patients were excluded before the study, and 34 patients were enrolled in pilot tests. Patients undergoing surgery were randomly allocated into either the 317NAPP group (n = 65) or the telephone-call group (n = 66). Overall, 3 patients were lost to follow-up because they were not contacted via telephone in the telephone-call group, and 1 patient was excluded for not finishing the questionnaire in the 317NAPP group.
2.3. Assessment
The work team (including a senior specialist in pediatric surgical nursing, 3 nurses for follow-up, and 2 software programmers) designed the children's short-term recovery quality questionnaire basing on our work experience and previous reports.[15–19] It included questions investigating 3 aspects (a total of 15 items): the physiological function, the ability to perform daily activities, and the nociceptive responses. The physiological conditions that were investigated (5 items) included appetite, sleep, spirit, breath, and comfort; the daily activities investigated (5 items) included standing or walking, sitting, lying down, climbing, and playing; and nociceptive responses investigated (5 items) included pain, nausea and vomiting, fever, fear, or dread. The questionnaire was scored using 5 grades from 1 to 5. The total score of the questionnaire was 75. The Cronbach scale coefficient was 0.882, and the content validity of the K-M-O was 0.718, which showed a good reliability and validity. The parents of participants completed the general information questionnaire before the surgery, and the scores associated with the physiological status and activities of daily living were calculated for quality assessment (T0). At 24 hours after surgery, the scores were calculated to determine the recovery value (T1). The difference between T1 and T0 represented the quality of recovery. The larger value of T1 to T0, the worse the quality of recovery for the patients. The time duration for follow-up was calculated for both groups.
2.4. 317NAPP
The programmer developed the 317NAPP according to the details provided by the team based on their previous work experiences. The 317NAPP could record information including those on admission, discharge, and health education (Table 1 and Fig. 3). The patient would receive a follow-up questionnaire 24 hours after discharge, and a reminder was automatically implemented by the 317NAPP. The background system of the 317NAPP accounted for a lot of prompt functions for the various situations that may have occurred during the follow-up to inform caregivers on how to deal with problems or provide notes. In addition, the text messages, pictures, videos, and other forms of health education were provided to the participants. The background system collected the follow-up data.
Table 1.
The main functions of the 317-nursing mobile application.

Figure 3.

An overview of the main features of 317NAPP.
2.5. The follow-up procedure
For the telephone-call group, the participants were followed-up via telephone at 24 hours after surgery to evaluate recovery; the time required for this procedure was recorded separately by nurses.
For the 317NAPP group, on the day of admission, parents (caregivers) were trained by the nurses regarding the importance of follow-up after surgery and the use of the mobile application (317NAPP), the installation, network connection, WeChat two-dimensional code, and how to use 317NAPP to get the information, submit applications, and fill in follow-up questionnaire. It was confirmed that all caregivers installed applications in their personal smartphones, and thus, they could interact with background system through the application. The time spent on these intensive trainings was recorded by nurses. Caregivers completed the follow-up questionnaires through the 317NAPP to evaluate recovery at 24 hours after the surgery.
2.6. Data analysis
The computer program SPSS 19.0 for Windows (SPSS Inc., IL, USA) was used for all statistical analyses. The significance level was set at P < .05. The data were presented as frequencies, percentages, mean values, and standard deviations. Descriptive statistics were used to describe the characteristics of the groups. Analysis of significant differences between groups were performed as follows: countable data using Chi-square test; normal distributions using t tests (paired or independent samples), and non-normal distributions using the Mann–Whitney U nonparametric test.
2.7. Ethical approval
The study was approved by the Research Ethics Committee of the Children's Hospital School of Medicine Zhejiang University (2016-IRB-043; April 15, 2016). Before any decision was made to participate, all parents (caregivers) were informed about the purpose of the study by the researcher, and were given a written informed consent form that was read out loud before they signed it. Participation was voluntary, and refusal to participate did not affect the care received during hospitalization or after discharging. It was also possible to stop participation without any specific reason.
3. Results
3.1. Comparison of the basic clinic data between the 2 groups
Three patients were not contacted via telephone in the control group, and 1 patient did not finish the questionnaire in the intervention group. The overall ratio of loss was about 3%.
We found that the basic clinic data of patients and the basic data of caregivers between the 2 groups were not significantly different (Table 2). There was no significant difference in satisfaction between the 2 groups (P = .39).
Table 2.
Comparison of the basic clinic data between the 2 groups (mean ± SD).

3.2. Comparison of the recovery quality between the 2 groups
The basic conditions of the participants before surgery were scored as T0, while the conditions 24 hours after surgery were scored as T1. The bigger of the value (T1–T0) indicated the worse recovery for the patients.
We found that the T1 scores were significantly higher than the T0 scores in both groups (P = .00). The value of T1 to T0 (10.75 ± 5.28) in intervention group was lower than that of control group (11.78 ± 5.16), but this difference was not significant (P = .27, Table 3).
Table 3.
Comparison of the quality of recovery between 2 groups (mean ± SD).

3.3. Comparison of time consumed in the follow-up between the 2 groups
The time consumed in the follow-up was calculated for both groups. Our results showed that the time consumed in the intervention group (62.83 ± 17.55 second) was significantly lower than that in the control group (203.75 ± 53.05 second) (P = .00, Table 4).
Table 4.
Comparison of time consume of follow-up (mean ± SD).
![]()
4. Discussion
The present study demonstrates that the mobile application, 317NAPP, can be used to monitor the short-term recovery of children undergoing day surgery, and is a time saver during follow-up. This result was consistent with the findings of previous reports[15,17,19,20] that showed improved recovery of day surgery patients with the use of a mobile application. Nilsson et al[20] applied a mobile application to monitor recovery in adult patients, and showed that it was cost-efficient and had a positive effect on recovery.
The proportion of day surgery has considerably increased in the recent years due to a shortage in medical supply resulting from the universal 2-child policy in China, advances in minimally invasive laparoscopic surgical techniques, improved anesthetic practices, increased use of short-acting/regional anesthesia, and patient preference for minimal hospital stay.[3–5] However, this increasing trend has resulted in few problems for successful and uncomplicated home recovery. Most children discharged just after the pain is controlled may not have actually recovered, and may require further attention for complete recovery. Myles et al[18] found that the most common complications during the recovery period were pain, nausea, vomiting, headache, back pain, and urinary retention. Because infants are unable to express themselves, the evaluation of recovery is based on the caregivers, which is consistent with the tenet of Family-Centered Care. In our study, in terms of toxic reactions, the children experienced different degrees of pain, vomiting, fever, and fear of surgery during recovery (Table 5). Our results indicate that the short-term complications monitored by 317NAPP were equivalent to those evaluated via telephone follow-up led by nurses. Moreover, we also found that the health index scores after surgery were significantly higher than those before surgery in both 317NAPP and telephone follow-up groups. Because the physiological status before surgery might differ among children, we applied the differences between the scores of before and after surgery as a recovery evaluation index. Our results further showed that the recovery evaluation index of 317NAPP group was lower than that of telephone group, indicating that the use of 317NAPP could partially assist the short-term recovery after day surgery. However, further studies with a larger sample are needed to clarify this.
Table 5.
Comparison of nociceptive reactions between 2 groups after surgery.

When children in a high-risk situation, the 317NAPP and its background system would send an alarm to the parents alerting them of the emergency, and alert the medical staff to get in touch with the parents/caregivers immediately, thus enhancing the confidence of the parents. There was no significant difference in satisfaction between the 2 groups, indicating that the acceptability of parental follow-up for 317NAPP was similar to that of telephone calls. Two patients in the intervention group reported redness around the surgical wound on the first day after surgery, which was afterwards confirmed as dressing-caused allergic dermatitis through uploaded photos, therefore effectively avoid unplanned hospital visits. We also found that most parents in the 317NAPP group would accept 317NAPP follow-up if the child underwent surgery again. Apart from these benefits, when patients do not respond to the questionnaire in time, the system will send a reminder every day to remind parents to fill in the questionnaire. In cooperation with the providers, patients can call the personnel after discharge to consult the problems encountered. Patients can upload videos to nurses to make up for content that cannot be expressed through words or pictures.
For a large percentage of the day surgeries, follow-up after surgery took up a lot of labor costs, particularly due to the shortage of nursing resources in China. In this study, the majority of time consumption for the intervention group was on the day of surgery and involved the training of the caregivers. The cost of telephone follow-up mainly involved the aspects such as making phone calls, evaluating the situation after surgery, telephone verbal guidance, and the establishment of follow-up files. This study found that 317NAPP follow-up time (62.83 ± 17.55 second) was significantly shorter than the telephone follow-up time (203.75 ± 53.05 second), indicating that 317NAPP follow-up could reduce the time consumption and the spending of nursing resources.
5. Conclusion
The 317NAPP mobile application has several advantages such as convenience, accessibility, high efficiency, and low cost. It can be used to monitor the short-term recovery of day surgery patients, and the time consumed is shorter than that by telephone follow-up.
5.1. Relevance to clinical practice
One limitation of this study was the limited sample size and the scope of diseases. In addition, doctor–patient interaction of 317NAPP also needs to be improved.
Acknowledgments
The authors thank Liang Jianfeng for sharing his expertise in statistics. The authors of this paper do not have any commercial associations that might pose a conflict of interest in connection with this manuscript. The authors thank all patients and their caregivers who participated in this study.
Author contributions
Conceptualization: Canping Li, Shoujiang Huang.
Data curation: Canping Li.
Formal analysis: Canping Li, Tingting Zhang.
Funding acquisition: Kewen Jiang.
Investigation: Canping Li, Shoujiang Huang, Xiaohua Su, Tingting Zhang.
Methodology: Canping Li, Shoujiang Huang, Xiaohua Su, Tingting Zhang.
Project administration: Xiaohua Su.
Resources: Xiaohua Su.
Software: Xiaohua Su.
Supervision: Kewen Jiang.
Validation: Shoujiang Huang.
Visualization: Shoujiang Huang.
Writing – original draft: Canping Li.
Writing – review & editing: Kewen Jiang.
Kewen Jiang orcid: 0000-0003-3147-6514.
Footnotes
Abbreviation: 317NAPP = 317 nursing mobile application program.
The study was financially supported by the National Natural Science Foundation of China (81571263 and 81871012), and by the Key Laboratory of Reproductive Genetics (Zhejiang University), Ministry of Education, and the Key Laboratory for Diagnosis and Therapy of Neonatal Diseases of Zhejiang Province.
The authors have no conflicts of interest to disclose.
References
- [1].Bontemps G. [Development of day surgery in France: more constraints for more performance?]. Presse Med 2014;43:275–7. [DOI] [PubMed] [Google Scholar]
- [2].Black N, Petticrew M, Hunter D, et al. Day surgery: development of a national comparative audit service. Qual Health Care 1993;2:162–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Berger RA, Sanders SA, Thill ES, et al. Newer anesthesia and rehabilitation protocols enable outpatient hip replacement in selected patients. Clin Orthop Relat Res 2009;467:1424–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Briggs CD, Irving GB, Mann CD, et al. Introduction of a day-case laparoscopic cholecystectomy service in the UK: a critical analysis of factors influencing same-day discharge and contact with primary care providers. Ann R Coll Surg Engl 2009;91:583–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Augestad KM, Revhaug A, Vonen B, et al. The one-stop trial: does electronic referral and booking by the general practitioner (GPs) to outpatient day case surgery reduce waiting time and costs? A randomized controlled trial protocol. BMC Surg 2008;8:14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Le T, Drolet J, Parayno E, et al. Follow-up phone calls after pediatric ambulatory surgery for tonsillectomy: what can we learn from families? J Perianesth Nurs 2007;22:256–64. [DOI] [PubMed] [Google Scholar]
- [7].Paquette J, Le May S, Lachance Fiola J, et al. A randomized clinical trial of a nurse telephone follow-up on paediatric tonsillectomy pain management and complications. J Adv Nurs 2013;69:2054–65. [DOI] [PubMed] [Google Scholar]
- [8].Eisenberg D, Hwa K, Wren SM. Telephone follow-up by a midlevel provider after laparoscopic inguinal hernia repair instead of face-to-face clinic visit. JSLS 2015;19:e2014.00205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Forster AJ, LaBranche R, McKim R, et al. Automated patient assessments after outpatient surgery using an interactive voice response system. Am J Manag Care 2008;14:429–36. [PubMed] [Google Scholar]
- [10].Perez F, Monton E, Nodal MJ, et al. Evaluation of a mobile health system for supporting postoperative patients following day surgery. J Telemed Telecare 2006;12suppl:41–3. [DOI] [PubMed] [Google Scholar]
- [11].Eyles H, McLean R, Neal B, et al. A salt-reduction smartphone app supports lower-salt food purchases for people with cardiovascular disease: findings from the SaltSwitch randomised controlled trial. Eur J Prev Cardiol 2017;24:1435–44. [DOI] [PubMed] [Google Scholar]
- [12].Skrepnik N, Spitzer A, Altman R, et al. Assessing the impact of a novel smartphone application compared with standard follow-up on mobility of patients with knee osteoarthritis following treatment with Hylan G-F 20: a randomized controlled trial. JMIR MHealth UHealth 2017;5:e64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Rong ZH, Luo F, Ma LY, et al. [Evaluation of an automatic image-based screening technique for neonatal hyperbilirubinemia]. Zhonghua Er Ke Za Zhi 2016;54:597–600. [DOI] [PubMed] [Google Scholar]
- [14].Jayakody A, Bryant J, Carey M, et al. Effectiveness of interventions utilising telephone follow up in reducing hospital readmission within 30 days for individuals with chronic disease: a systematic review. BMC Health Serv Res 2016;16:403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Rhondali O, Villeneuve E, Queyrel G, et al. Fast-track recovery after day case surgery. Paediatr Anaesth 2015;25:1007–12. [DOI] [PubMed] [Google Scholar]
- [16].Liao WW, Wang JJ, Wu GJ, et al. The effect of cerebral monitoring on recovery after sevoflurane anesthesia in ambulatory setting in children: a comparison among bispectral index, A-line autoregressive index, and standard practice. J Chin Med Assoc 2011;74:28–36. [DOI] [PubMed] [Google Scholar]
- [17].Armstrong J, Forrest H, Crawford MW. A prospective observational study comparing a physiological scoring system with time-based discharge criteria in pediatric ambulatory surgical patients. Can J Anaesth 2015;62:1082–8. [DOI] [PubMed] [Google Scholar]
- [18].Myles PS, Weitkamp B, Jones K, et al. Validity and reliability of a postoperative quality of recovery score: the QoR-40. Br J Anaesth 2000;84:11–5. [DOI] [PubMed] [Google Scholar]
- [19].Stark PA, Myles PS, Burke JA. Development and psychometric evaluation of a postoperative quality of recovery score: the QoR-15. Anesthesiology 2013;118:1332–40. [DOI] [PubMed] [Google Scholar]
- [20].Nilsson U, Jaensson M, Dahlberg K, et al. RAPP, a systematic e-assessment of postoperative recovery in patients undergoing day surgery: study protocol for a mixed-methods study design including a multicentre, two-group, parallel, single-blind randomised controlled trial and qualitative interview studies. BMJ Open 2016;6:e009901. [DOI] [PMC free article] [PubMed] [Google Scholar]


