Abstract
Background:
Most clinical guidelines recommend a restrictive red-blood-cell (RBC) transfusion threshold. However, indications for transfusion in patients with a hip fracture have not been definitively evaluated or remain controversial. We compared the pros and cons of restrictive versus liberal transfusion strategies in patients undergoing hip fracture surgery.
Methods:
Electronic databases were searched to identify randomized controlled trials (RCTs) and retrospective cohort studies (RCSs) to investigate the effects of a restrictive strategy versus its liberal counterpart in patients undergoing hip fracture surgery. The main clinical outcomes included delirium, mortality, infections, cardiogenic complications, thromboembolic events, cerebrovascular accidents, and length of hospital stay. The meta-analysis program of the Cochrane Collaboration (RevMan version 5.3.0) was used for data analysis. Statistical heterogeneity was assessed by both Cochran chi-squared test (Q test) and I2 test. Both Begg and Egger tests were used to assess potential publication bias.
Results:
We identified 7 eligible RCTs and 2 eligible RCSs, involving 3,575 patients in total. In patients undergoing hip fracture surgery, we found no differences in frequency of delirium, mortality, the incidence rates of all infections, pneumonia, wound infection, all cardiovascular events, congestive heart failure, thromboembolic events or length of hospital stay between restrictive and liberal thresholds for RBC transfusion (P >.05). However, we found that the use of restrictive transfusion thresholds is associated with higher rates of acute coronary syndrome (P <.05) while liberal transfusion thresholds increase the risk of cerebrovascular accidents (P <.05).
Conclusion:
In patients undergoing hip fracture surgery, clinicians should evaluate the patient's condition in detail and adopt different transfusion strategies according to the patient's specific situation rather than merely using a certain transfusion strategy.
Keywords: blood transfusion, hip fracture, liberal transfusion, restrictive transfusion
1. Introduction
With the aging of our society, hip fractures have become a common injury.[1] Approximately half of all hip fracture patients require red-blood-cell (RBC) transfusion because of perioperative hemorrhage.[2,3] RBC transfusions are associated with complications such as allergic reactions, bacterial or viral infections, circulatory overload, acute hemolysis, and acute lung injury.[4,5] All of these complications increase patient morbidity and mortality and patients’ financial burden.[6]
Accordingly, many studies support a restrictive RBC transfusion strategy (hemoglobin threshold less than 10 g/dL, mostly 8 g/dL) instead of a liberal transfusion strategy (hemoglobin threshold more than 10 g/dL, mostly more than 8 g/dL),[7–12] and some scholars even recommend a transfusion threshold of 7 g/dL.[13] A meta-analysis of a range of clinical specialties showed that restrictive transfusion decreased the RBC proportion by 43% but did not impact 30-day mortality or morbidity.[14] A meta-analysis of patients undergoing only hip surgery showed that restrictive transfusion did not affect mortality, functional recovery, or postoperative morbidity, but there was very low-quality evidence of a lower risk of myocardial infarction in the liberal compared with the restrictive transfusion threshold group.[15]
However, not all studies agree with a restrictive RBC transfusion strategy. Some meta-analyses have shown that it may not be safe to use a restrictive transfusion threshold in patients with cardiovascular disease.[16] One meta-analysis showed that restrictive transfusion strategies should be applied with caution in high-risk patients undergoing major surgery.[17] Another meta-analysis showed that liberal transfusion might produce better outcomes than restrictive transfusion in elderly patients.[18]
The majority of patients with hip fracture are geriatric and have a high rate of cardiovascular disease, and hip fracture surgeries are highly traumatic.[19] Consequently, given recent new evidence, we conducted a meta-analysis of randomized controlled trials (RCTs) and retrospective cohort studies (RCSs) to examine whether the restrictive transfusion strategy is more effective and safer than the liberal transfusion strategy in patients undergoing hip fracture surgery.
2. Methods
This meta-analysis was carried out in accordance with the Cochrane Handbook for Systematic Reviews of Interventions and is reported in compliance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement.[20,21]
2.1. Literature search
An online search was performed in the PubMed, Web of Science, Embase, and Springer databases and the Cochrane Library. Search terms included those related to hip fracture, transfusion, and their variants. We present the search strategy as follows: (transfusion OR transfusions OR restrictive transfusion strategy OR liberal transfusion strategy OR restrictive transfusion threshold OR liberal transfusion threshold) AND (hip fracture OR hip fractures OR intertrochanteric fracture OR femoral neck fracture OR subtrochanteric fracture). No restrictions were placed on language or type of publication. Two reviewers (ZC and YJ) selected relevant studies independently. We also searched the references of the retrieved studies and recent reviews. The date of the last search was 06 December 2018. We also contacted some authors of the original studies for additional information, and Professor Leuzinger replied to our inquiry by E-mail.[22]
2.2. Study selection
By screening the titles and abstracts for relevance, 2 teams of reviewers (ZC and XQM; YJ and WB) independently decided which studies to include based on the selection criteria. Discrepancies were resolved through discussion with other reviewers. Studies were included in the meta-analysis if they met the following criteria:
-
(1)
they were RCTs or RCSs;
-
(2)
they used 2 comparator groups in which 1 group received an RBC transfusion with liberal transfusion strategy and the other received an RBC transfusion with a restrictive threshold;
-
(3)
patients undergoing hip fracture repair surgery were enrolled;
-
(4)
adequate data were available to be pooled for the analysis.
Studies were excluded if they were experimental trials, data were incomplete or unavailable, they were non-original articles, or if the data or the sample were duplicated.
2.3. Data extraction
The following data were independently extracted by 2 reviewers (XLY and LW): first author's family name, publication year, origin of patients, age, number of patients, transfusion thresholds and clinical outcomes. The clinical outcomes consisted of delirium, in-hospital mortality, 30-day mortality, 3-month mortality, 1-year mortality, all cardiovascular events, myocardial infarction, congestive heart failure, arrhythmia, all infections, wound infection, pulmonary infection, cerebrovascular accidents, length of hospitalization and thromboembolic events. Disagreements were resolved through discussion with the other authors.
2.4. Assessment of methodological quality
Two reviewers (WH and GS) independently graded the methodological quality of each eligible study. We used the Cochrane Collaboration's tool to assess risk of bias for randomized controlled trials (RCTs). The assessment consisted of random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessors, incomplete outcome data, selective outcome reporting, and other bias, and each RCT was viewed and scored as high, low, or unclear regarding the risk involving these domains. Blinding of participants and personnel was generally not feasible because of the nature of this study, so we categorized trials as having a low risk of bias if only blinding of participants and personnel was not scored as being at low risk of bias. The quality of retrospective cohort studies was assessed using the Newcastle–Ottawa quality assessment scale for non-randomized case-controlled studies and cohort studies. Three aspects were assessed: selection, comparability, and exposure. A quality score of ≥6 on the 9-point Newcastle–Ottawa scale was moderated to represent a relatively high-quality CS.
2.5. Data analysis
Statistical analyses were performed using the Cochrane Collaboration's Review Manager 5.3 software. Statistical heterogeneity was assessed by both Cochran chi-squared test (Q-test) and I2 test. P ≥.1 and I2 <50% were considered to represent no statistical heterogeneity, and a fixed-effects model was used to estimate binary and continuous variables; a P value of .05 was used as the level of statistical significance. Binary variables were presented as risk ratio (RR) and 95% confidence interval (95% CI). Continuous variables were expressed as mean and standard deviation (SD), and assessed using weighted mean differences and respective 95% confidence intervals (Cis). Begg test and Egger test were used to assess potential publication bias, and they were performed using the software Stata11.0 (Stata Corporation, College Station, TX).[23,24] To avoid clinical heterogeneity and false-positive outcomes, if the results were statistically significant using the fixed effects model, we performed a meta-analysis again using a random-effects model.
3. Results
3.1. Characteristics of studies included
The search strategy is detailed in Figure 1. Relevant references were selected and the studies included were manually reviewed. The initial online search generated 649 records after excluding duplicates (n = 176). After screening the titles and abstracts, 623 articles were excluded. Of the remaining 26 relevant studies, 17 were excluded because they were not comparisons or used ineligible comparators (n = 8) and inappropriate data (n = 9); 9 trials were included in the final analysis.[22,25–32]
Figure 1.
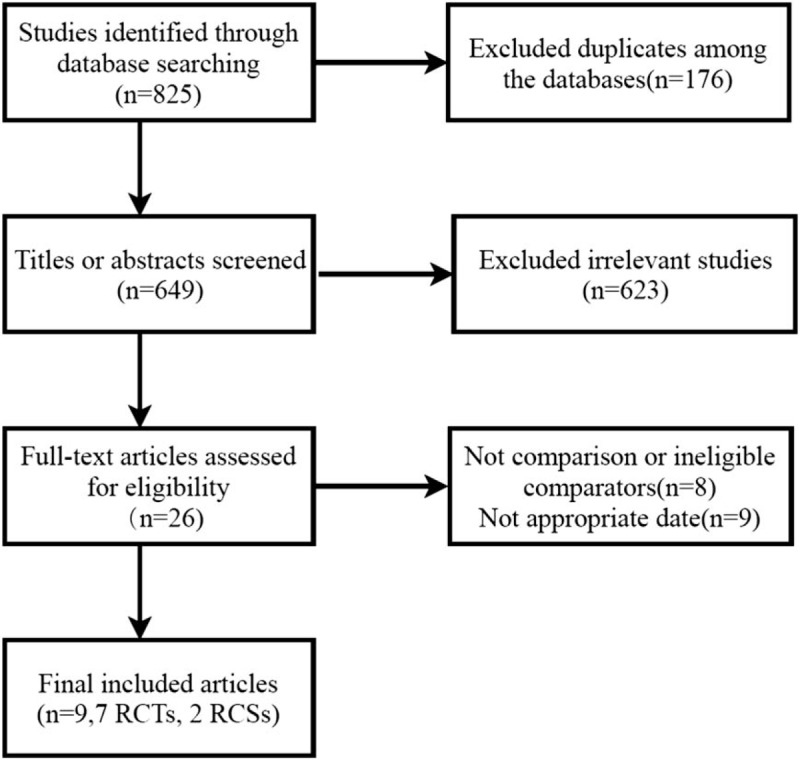
Flow diagram of studies included in the systematic review. RCS = retrospective cohort study, RCT = randomized controlled trial.
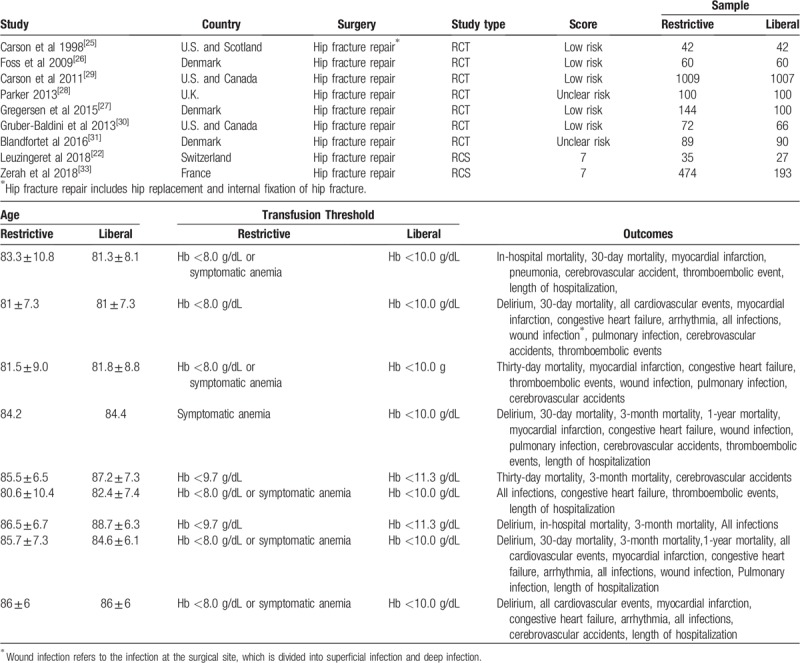
The characteristics of the trials included are summarized in Table 1. The 9 trials included were published between 1998 and 2018, with sample sizes ranging from 62 to 2016 subjects and a total of 3531 subjects. Mean participant age ranged from 81 to 88.7 years. In the restrictive transfusion arm, the hemoglobin threshold level ranged from 8.0 to 9.7 g/dL (mostly 8.0 g/dL). In the liberal transfusion arm, the hemoglobin level ranged from 10.0 to 11.3 g/dL (mostly 10.0 g/dL). The studies of both Gregersen and Blandfort involved participants from the same center, and the samples of Blandfort are included among the samples of Gregersen, but the results they analyzed were mostly different; both were therefore included in our analysis. Professor Leuzinger told us that, in their research into cardiovascular events, there were 4 myocardial infarction patients, 1 congestive heart failure patient and 1 arrhythmia patient in the restrictive transfusion group, and there were 1 myocardial infarction patient and 1 arrhythmia patient in the liberal transfusion group. With regard to infection, 4 patients had pneumonia and 1 patient had an infected wound in the restrictive transfusion group while 3 patients had pneumonia, and 3 patients had infected wounds in the liberal transfusion group.[22]
Table 1.
Characteristics of the included trials.
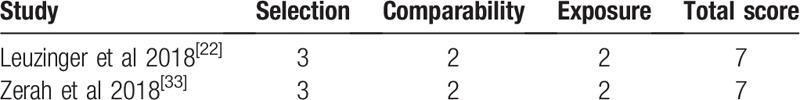
3.2. Quality of studies
Information concerning the risk of bias for each RCT is presented in Figure 2. Five RCTs had a low risk of bias and 2 RCTs were categorized as being unclear. The 2 RCSs were of high quality with a score of 7 points (Table 2).
Figure 2.
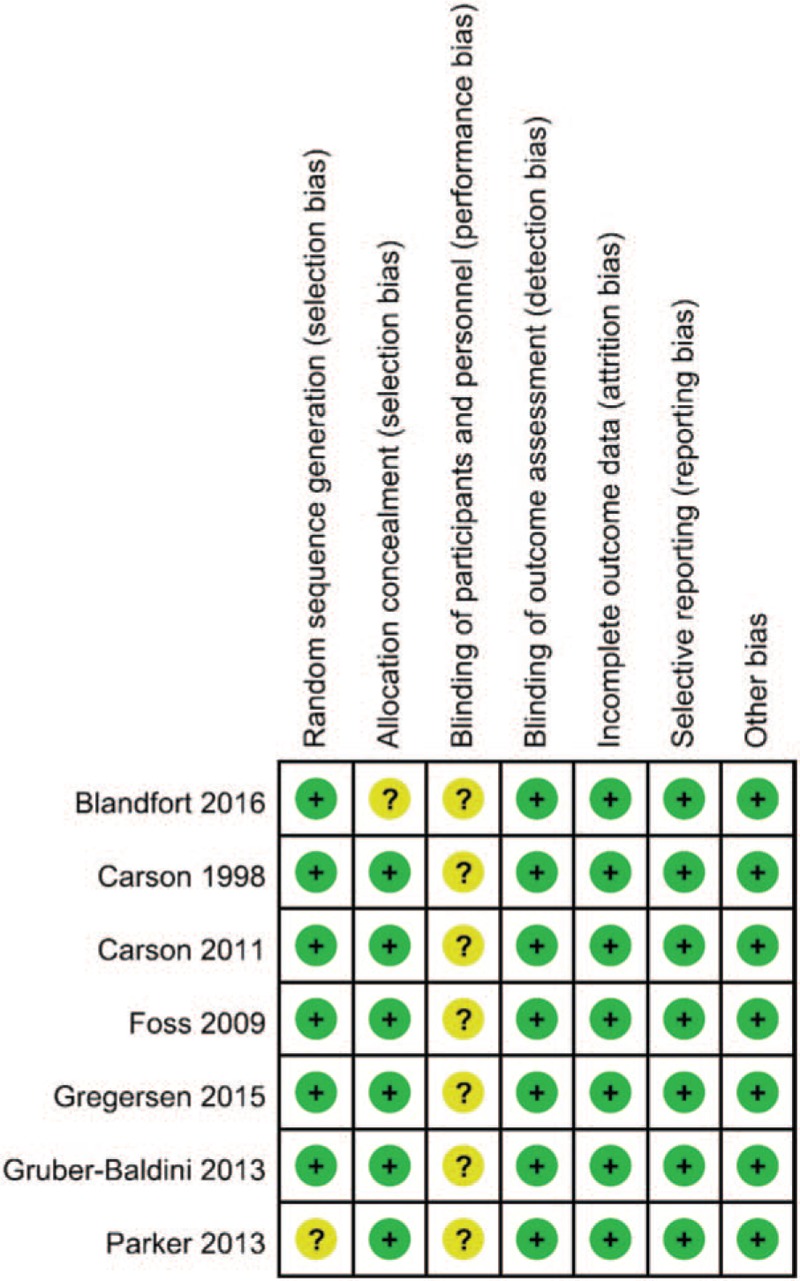
Risk-of-bias summary. + = low risk, and ? = uncertain risk.
Table 2.
Quality assessment according to the Newcastlee–Ottawa scale.
3.3. Meta-analysis of clinical outcomes
3.3.1. Delirium rate
The delirium rate was described in 5 of the 9 articles, which included 748 and 470 patients in restrictive and liberal transfusion threshold groups, respectively. There was no difference in delirium rate after surgery between the 2 groups (RR = 0.98, 95% CI 0.81–1.18; P = .82), and no statistically-significant heterogeneity (χ2 = 6.86; P = .14; I2 = 42%; Fig. 3). No publication bias was found according to Begg test (P = .806) or Egger test (P = .809).
Figure 3.
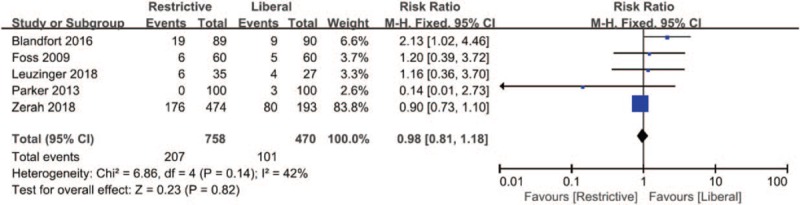
Forest plot of delirium. 95% CI = 95% confidence interval, df = degrees of freedom, Fixed = fixed effects model.
3.3.2. Mortality
The results of in-hospital mortality are shown in Figure 4A. Four studies involving 2943 patients (1613 in the restrictive and 1330 in the liberal transfusion strategy group) reported postoperative in-hospital mortality. No statistically significant difference in in-hospital mortality was observed between the 2 groups (RR = 1.04, 95% CI 0.65–1.67; P = .87), and no statistically significant heterogeneity (χ2 = 3.79; P = .30; I2 = 18%). No publication bias was found in any of the included studies according to Begg test (P = .296) or Egger test (P = .094).
Figure 4.
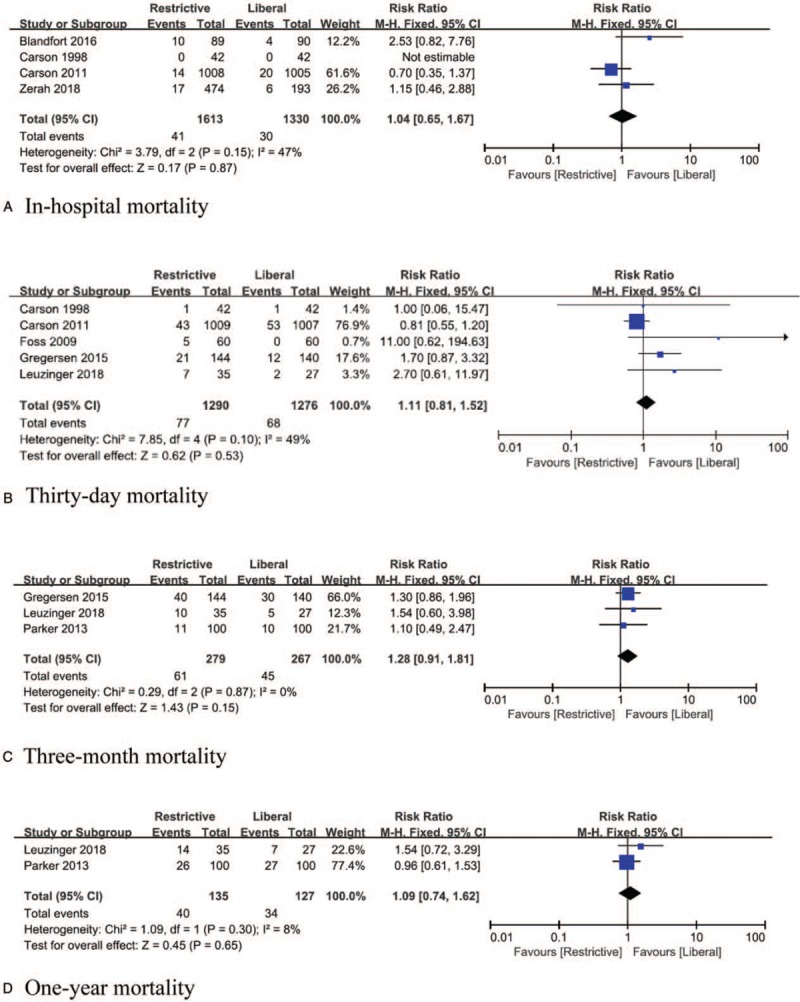
Forest plot of mortality. 95% CI = 95% confidence interval, df = degrees of freedom, Fixed = fixed effects model. A. In-hospital mortality; B. Thirty-day mortality; C. Three-month mortality; D. One-year mortality.
The results of 30-day mortality are shown in Figure 4B. Five studies involving 2566 patients (1290 in the restrictive and 1276 in the liberal transfusion strategy group) reported postoperative 30-day mortality. No statistically significant difference in in-hospital mortality was observed between the 2 groups (RR = 1.11, 95% CI 0.81–1.52; P = .53), and no statistically significant heterogeneity (χ2 = 7.85; P = .10; I2 = 49%). No publication bias was found in any of the included studies according to Begg test (P = .462) or Egger test (P = .148).
The results of 3-month mortality are shown in Figure 4C. Three studies involving 546 patients (279 in the restrictive and 267 in the liberal transfusion strategy groups) reported postoperative 3-month mortality. No statistically significant difference in 3-month mortality was observed between the 2 groups (RR = 1.28, 95% CI 0.91–1.81; P = .15), and no statistically significant heterogeneity (χ2 = 0.29; P = .87; I2 = 0%). No publication bias was found in any of the included studies according to Begg's test (P = .1) or Egger's test (P = .921).
The results of 1-year mortality are shown in Figure 4D. Two studies involving 262 patients (135 in the restrictive and 127 in the liberal transfusion strategy group) reported postoperative 1-year mortality. No statistically significant difference in 1-year mortality was observed between the 2 groups (RR = 1.09, 95% CI 0.74–1.62; P = .65), and no statistically significant heterogeneity (χ2 = 1.09; P = .30; I2 = 8%). No publication bias was found in any of the included studies according to Begg test (P = 1).
3.3.3. Cardiovascular events
Seven of the studies provided relevant data on cardiovascular event incidence rates. The summarized estimates of effect size indicated that the restrictive transfusion strategy group had a significantly higher myocardial infarction incidence rate than the liberal counterpart (RR = 1.77, 95% CI 1.09–2.86; P = .02), and no statistically significant heterogeneity (χ2 = 0.55; P = .91; I2 = 0%; Fig. 5). Similar results were obtained when using a random-effects model. Possible publication bias was found according to Egger test (P = .026). No statistically significant difference in congestive heart failure (RR = 1.34, 95% CI 0.85–2.12; P = .21) and arrhythmia (RR = 0.84, 95% CI 0.53–1.35; P = .48) was observed between the 2 groups, and no statistically significant heterogeneity (χ2 = 1.59; P = .81; I2 = 0%; χ2 = 2.12; P = .55; I2 = 0%). No publication bias was found in any of the studies according to Begg test (P = .806; P = .462) or Egger test (P = .902; P = .614). The pooled estimates of effect size showed that the incidence of all cardiovascular events did not differ significantly between the 2 groups (RR = 1.28, 95% CI 0.98–1.67; P = .07).
Figure 5.
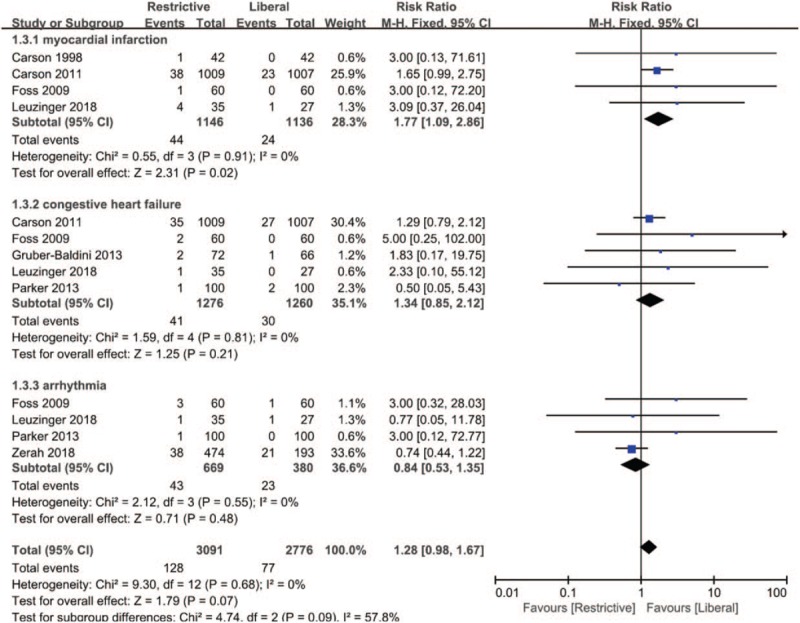
Forest plot of cardiovascular events. 95% CI = 95% confidence interval, df = degrees of freedom, Fixed = fixed effects model.
3.3.4. Infection
Some of the included studies reported only wound or pulmonary infections (pneumonia), while others reported any infectious complication, not limited to pulmonary or wound infections. Consequently, we compared them separately.
The results of wound infection are shown in Figure 6A. Four studies involving 2406 patients (1204 in the restrictive and 1202 in the liberal transfusion strategy group) reported cases of wound infection. No statistically-significant difference in wound infection was observed between the 2 groups (RR = 0.66, 95% CI 0.33–1.30; P = .23), and no statistically significant heterogeneity (χ2 = 3.30; P = .35; I2 = 9%). No publication bias was found in any of the included studies according to Begg test (P = 1) or Egger test (P = .675).
Figure 6.
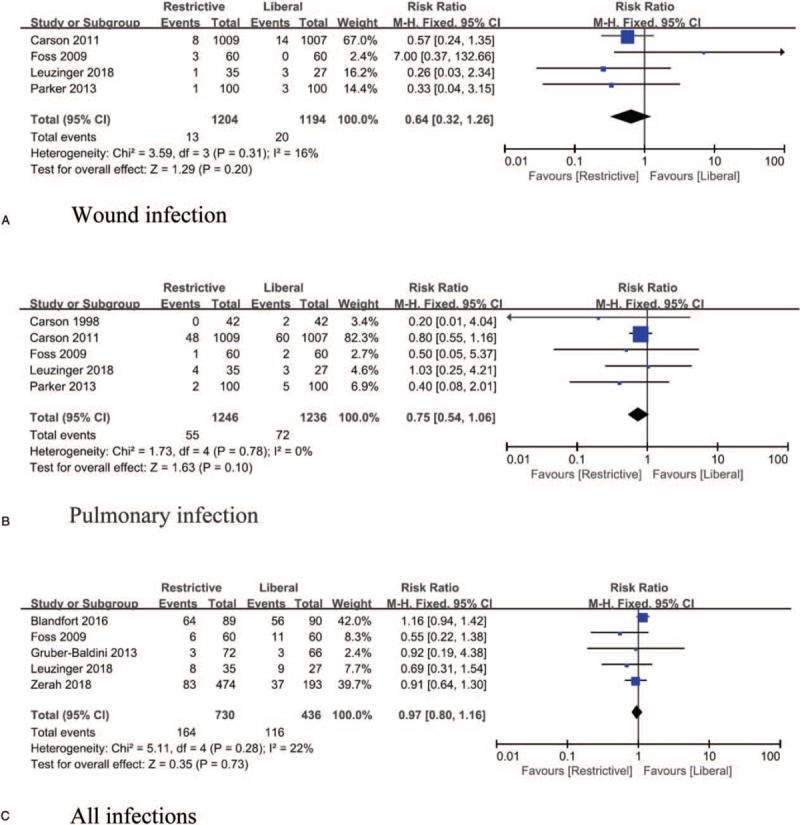
Forest plot of infection. 95% CI = 95% confidence interval, df = degrees of freedom, Fixed = fixed effects model. A. Wound infection; B. Pulmonary infection; C. All infections.
The results of pulmonary infection (pneumonia) are shown in Figure 6B. Five studies involving 2490 patients (1246 in the restrictive group and 1244 in the liberal transfusion strategy group) reported cases of pulmonary infection. No statistically significant difference in pulmonary infection was observed between the 2 groups (RR = 0.76, 95% CI 0.54–1.07; P = .12), and no statistically significant heterogeneity (χ2 = 2.15; P = .71; I2 = 0%). No publication bias was found in any of the included studies according to Begg test (P = .221) or Egger test (P = .353).
The results of all infections are shown in Figure 6C. Five studies involving 1166 patients (730 in the restrictive group and 746 in the liberal transfusion strategy group) reported all cases of infection. No statistically-significant difference in total infection was observed between the 2 groups (RR = 0.97, 95% CI 0.80–1.15; P = .73), and no statistically significant heterogeneity (χ2 = 5.11; P = .28; I2 = 22%). No publication bias was found in any of the included studies according to Begg test (P = .462) or Egger test (P = .147).
3.3.5. Cerebrovascular accident (stroke)
Relevant data concerning cerebrovascular accident (stroke) incidence rates were obtained from 6 of the included studies. Liberal compared with restrictive transfusion was associated with increased risk of cerebrovascular accidents (RR = 0.40, 95% CI 0.19–0.86; P = .02), and no statistically significant heterogeneity (χ2 = 1.54; P = .91; I2 = 0%; Fig. 7). No publication bias was found in any of the included studies according to Begg's test (P = 1) or Egger's test (P = .668). Similar results were obtained using the random-effects model.
Figure 7.
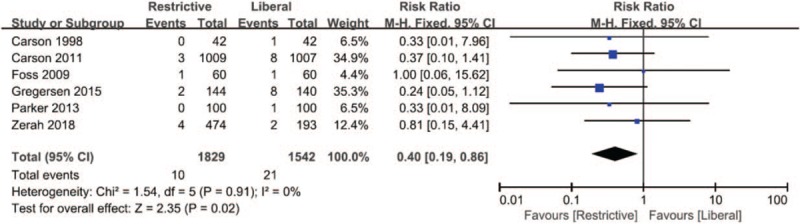
Forest plot of cerebrovascular accident (stroke). 95% CI = 95% confidence interval, df = degrees of freedom, Fixed = fixed effects model.
3.3.6. Thromboembolic events
Four trials involving 2474 participants (1241 in the restrictive group and 1233 in the liberal transfusion strategy group) reported thromboembolic events. There was no significant difference in the rate of thromboembolic events between the liberal and restrictive transfusion threshold groups (RR = 0.71, 95% CI 0.34–1.45; P = .35), and no statistically significant heterogeneity (χ2 = 2.46; P = .48; I2 = 0%; Fig. 8). No publication bias was found in any of the included studies according to Begg's test (P = .308) or Egger test (P = .980).
Figure 8.
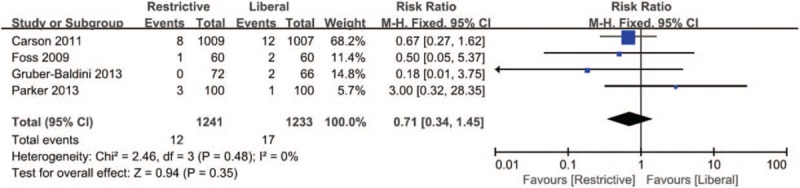
Forest plot of thromboembolic events. 95% CI = 95% confidence interval, df = degrees of freedom, Fixed = fixed effects model.
3.3.7. Length of hospitalization
Five studies reported the length of hospitalization after in the 2 groups. No statistically-significant difference in total infection was found between the 2 groups (RR = −0.44, 95% CI −1.09–0.20; P = .17), and no statistically significant heterogeneity (χ2 = 3.47; P = .17; I2 = 0%; Fig. 9). No publication bias was found in any of the included studies according to Begg's test (P = .587) or Egger's test (P = .263)
Figure 9.
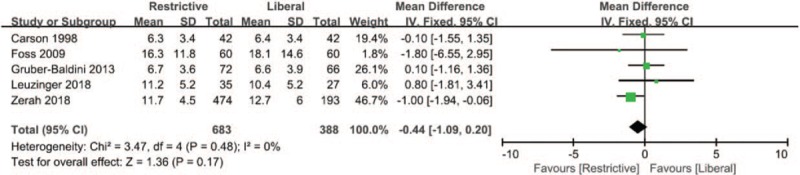
Forest plot of length of hospitalization. 95% CI = 95% confidence interval, df = degrees of freedom, Fixed = fixed effects model, IV = inverse variance, SD = standard deviation.
4. Discussion
This meta-analysis was performed to report the complications and mortality following restrictive RBC transfusion strategies compared to liberal RBC transfusion strategies in patients undergoing hip fracture operations. Seven RCTs and 2 RCSs were included in this research. Since the 2 RCSs were also of high quality, we included them in the study with the RCTs. All comparisons showed good heterogeneity. Additionally, we did not observe obvious publication bias in most of the comparisons, as assessed by Begg and Egger tests.
This meta-analysis demonstrated that there was no significant difference in delirium incidence between the restrictive and liberal transfusion strategy groups. There have been few meta-analysis comparisons of the incidence of post-transfusion delirium. Five articles were included in this comparison. Only Blandfort et al believed that the liberal transfusion strategy reduced the incidence of postoperative delirium up to day 10 for nursing home residents,[31] and the other 4 studies showed that there was no significant difference in delirium incidence between the restrictive and liberal transfusion strategy groups. Gruber-Baldini believed the liberal transfusion strategy was unlikely to influence delirium severity or rate in individuals with hip fracture after surgery.[30] Interestingly, Gregersen found that the liberal transfusion strategy could improve, overall quality of life after hip fracture operation in less severe dementia patients.[27]
This meta-analysis showed that there was no significant difference in in-hospital mortality, 30-day mortality or 3-month mortality between the restrictive and liberal transfusion strategy groups. A meta-analysis of restrictive versus liberal transfusion in patients after hip or knee surgery also showed there was no significant difference in 30-day mortality.[33] A meta-analysis of restrictive versus liberal transfusion in perioperative patients showed that adult patients had improved survival when receiving blood transfusion under a liberal strategy, but this meta-analysis did not take into account differences in follow-up time for the articles included in the analysis.[34] Shokoohi et al reported that among an elderly population with hip fracture, blood transfusion did not change the 6-month mortality.[35] Our meta-analysis also found no significant difference in 1-year mortality between the 2 groups.
Our meta-analysis showed that there were no significant differences in the rates of all infections, wound infection, or pulmonary infection (pneumonia) between the restrictive and liberal transfusion groups. These outcomes are consistent with some previously published meta-analyses. A meta-analysis showed that there was a reduced risk of serious infection in patients undergoing hip or knee replacement surgery in the restrictive transfusion arm. However, we believe that the author was biased in data selection, because, in this study describing the acquisition of data of infection cases, some articles included refer to pneumonia, some articles include refer to wound infection plus pneumonia, and some articles included refer to all types of infections.[36] The same mistake was also found in the other meta-analysis, which showed a significant difference in the rates of infections between the restrictive and liberal transfusion groups.[37] This meta-analysis also indicated that there were no significant differences in the incidence of wound infection or pneumonia. Although our meta-analysis showed no significant difference in the incidence of pneumonia between the 2 groups, the P-value was marginal, and the incidence of pneumonia in the liberal transfusion group was higher than that in the restricted group in most included studies, which should be taken into account. Another meta-analysis found that the allogeneic blood transfusion group had a significantly higher frequency of surgical-site infections than the non-transfused group. Above all, we still need more high-quality prospective studies to resolve this controversy.
Our meta-analysis found a reduced risk of cerebrovascular accidents (stroke) in the restrictive transfusion groups. Rubinstein et al found that intraoperative transfusion of PRBC increased the stroke risk during carotid endarterectomy.[38] Bucerius et al believed that transfusion of a large number of PRBC was the strongest (OR = 5) independent predictor of perioperative stroke.[39] The mechanism by which blood transfusion increases stroke risk remains unclear, and Rubinstein et al believed it could be due to hypercoagulable and inflammatory reactions after transfusion.[38]
At the beginning of the comparison between the incidence of cardiovascular diseases and myocardial infarction, it was found that the heterogeneity was too high. Through the sensitivity test, the source of heterogeneity was identified as the study by Zerah et al[32] and we excluded this paper. We found a reduced risk of myocardial infarction in the liberal transfusion groups, but there was no significant difference in congestive heart failure and arrhythmia between the restrictive and liberal transfusion strategy groups. Wang et al[40] and Docherty et al[16] argued it may not be safe to use a restrictive transfusion strategy in patients with ongoing acute coronary syndrome or chronic cardiovascular disease. Another meta-analysis showed there was no significant difference in the incidence of myocardial infarction in patients undergoing hip or knee surgery, but their study included patients who underwent both elective arthroplasty and hip fracture surgery.[33] Gu et al argued a restrictive transfusion strategy increases the risk of cardiovascular events in patients undergoing hip fracture surgery but not in those receiving elective arthroplasty.[41] These findings are consistent with ours. A meta-analysis by Brunskill et al also found very low-quality evidence of a lower risk of myocardial infarction in the liberal compared with the restrictive transfusion threshold group.[15] Compared with their study, our analysis added the latest literature and enhanced the credibility of the conclusion, but more studies will be needed to confirm it. Furthermore, we believe that the restrictive transfusion strategy increased the risk of heart attack rather than heart failure and arrhythmia in patients after hip fracture surgery.
This meta-analysis also showed that there were no significant differences in the rates of thromboembolic events (RR, 0.80; 95% CI, 0.38–1.67, P = .55) or length of hospitalization (mean difference = −0.44; 95% CI −1.09–0.20, P = .17) between the restrictive and liberal transfusion groups.
5. Limitations
Our review has several limitations. First, not all of the articles we included were RCTs. In particular, there was a lack of RCTs in this area in recent years. Second, definitions of specific complication varied between the included articles. For example, in some articles, cardiovascular disease referred to ischemic heart disease plus heart failure, but arrhythmia was also included in the scope of cardiovascular disease in other articles. These may also have resulted in bias. Third, in the included studies, thresholds for restrictive and liberal transfusion strategies varied. All of the above may have resulted in bias, although in most results, we found no evidence of statistically-significant heterogeneity.
6. Conclusion
This meta-analysis found no difference in mortality, length of hospitalization, and incidence rates of delirium, all infections, thromboembolic events, arrhythmia or congestive heart failure, between patients who underwent hip fracture surgery with restrictive versus liberal transfusion strategies. This review also found that the use of restrictive transfusion thresholds is associated with higher rates of acute coronary syndrome; however, the use of liberal transfusion thresholds increases the risk of cerebrovascular accidents (stroke). We, therefore, suggest that clinicians should evaluate a patient's condition in detail and adopt different transfusion strategies according to the patient's specific situation rather than merely using a certain transfusion strategy. Additional large-scale RCTs are needed to confirm these findings.
Author contributions
Data curation: Chao Zhu, Jian Yin, Bin Wang, Qingmei Xue, Shan Gao, Linyu Xing, Hua Wang, Wei Liu.
Formal analysis: Chao Zhu, Jian Yin, Bin Wang, Qingmei Xue.
Project administration: Xinhui Liu.
Writing – original draft: Chao Zhu, Jian Yin, Bin Wang.
Writing – review & editing: Xinhui Liu.
Footnotes
Abbreviations: RBC = red-blood-cell, RCS = retrospective cohort study, RCT = randomized controlled trial, RR = risk ratio.
CZ, JY, and BW contributed equally to this work.
All analyses were based on previously published studies, thus no ethical approval and patient consent are required.
The authors declare that they have no conflict of interest.
Funding: There is no funding source.
References
- [1].Xu Z, Zhang M, Yin J, et al. Redisplacement after reduction with intramedullary nails in surgery of intertrochanteric fracture: cause analysis and preventive measures. Arch Orthop Trauma Surg 2015;135:751–8. [DOI] [PubMed] [Google Scholar]
- [2].Eriksson BI, Bauer KA, Lassen MR, et al. Steering committee of the pentasaccharide in hip-fracture surgery s: fondaparinux compared with enoxaparin for the prevention of venous thromboembolism after hipfracture surgery. N Engl J Med 2001;345:1298–304. [DOI] [PubMed] [Google Scholar]
- [3].Pedersen AB, Cronin Fenton D, Nørgaard M, et al. Body mass index, risk of allogeneic red blood cell transfusion, and mortality in elderly patients undergoing hip fracture surgery. Osteoporos Int 2016;27:2765–75. [DOI] [PubMed] [Google Scholar]
- [4].Borghi B, Casati A. Incidence and risk factors for allogenic blood transfusion during major joint replacement using an integrated autotransfusion regimen. The Rizzoli Study Group on Orthopaedic Anaesthesia. Eur J Anaesthesiol 2000;17:411–7. [DOI] [PubMed] [Google Scholar]
- [5].Viber B, Gundtoft PH, Schønnemann J, et al. Introduction of national guidelines for restrictive blood transfusion threshold for hip fracture patients–a consecutive cohort study based on complete follow-up in national databases. J Orthop Surg Res 2018;13:116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Willett LR, Carson JL. Management of postoperative complications: anemia. Clin Geriatr Med 2014;30:279–84. [DOI] [PubMed] [Google Scholar]
- [7].Carson JL, Guyatt G, Heddle NM, et al. Clinical practice guidelines from the AABB red blood cell transfusion thresholds and storage. JAMA 2016;316:2025–35. [DOI] [PubMed] [Google Scholar]
- [8].Carson JL, Carless PA, Hebert PC. Transfusion thresholds and other strategies for guiding allogeneic red blood cell transfusion. Cochrane Database Syst Rev 2012;18:CD002042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Fontana S, Rigamonti V. Transfusion von Blutprodukten. Schweiz Med Forum 2013;13:89–93. [Google Scholar]
- [10].Hebert PC, Wells G, Blajchman MA, et al. A multicenter, randomized, controlled clinical trial of transfusion requirements in critical care. N Engl J Med 1999;340:409–17. [DOI] [PubMed] [Google Scholar]
- [11].Holst LB, Petersen MW, Haase N, et al. Restrictive versus liberal transfusion strategy for red blood cell transfusion: systematic review of randomised trials with meta-analysis and trial sequential analysis. BMJ 2015;350:h1354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Vuille-Lessard E, Boudreault D, Girard F, et al. Postoperative anemia does not impede functional outcome and quality of life early after hip and knee arthroplasties. Transfusion 2012;52:261–70. [DOI] [PubMed] [Google Scholar]
- [13].Hebert PC, Carson JL. Transfusion threshold of 7 g per decilitre: the new normal. N Engl J Med 2014;371:1459–61. [DOI] [PubMed] [Google Scholar]
- [14].Carson JL, Stanworth SJ, Roubinian N, et al. Transfusion thresholds and other strategies for guiding allogeneic red blood cell transfusion. Cochrane Database Syst Rev 2016;10:CD002042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Brunskill SJ, Millette SL, Shokoohi A, et al. Red blood cell transfusion for people undergoing hip fracture surgery. Cochrane Database Syst Rev 2015;4:CD009699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Docherty AB, O’Donnell R, Brunskill S, et al. Effect of restrictive versus liberal transfusion strategies on outcomes in patients with cardiovascular disease in a non-cardiac surgery setting: systematic review and meta-analysis. BMJ 2016;352:i1351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Hovaguimian F, Myles PS. Restrictive versus liberal transfusion strategy in the perioperative and acute care settings: a context-specific systematic review and meta-analysis of randomized controlled trials. Anesthesiology 2016;125:46–61. [DOI] [PubMed] [Google Scholar]
- [18].Simon GI, Craswell A, Thom O, et al. Outcomes of restrictive versus liberal transfusion strategies in older adults from nine randomised controlled trials: a systematic review and meta-analysis. Lancet Haematol 2017;4:e465–74. [DOI] [PubMed] [Google Scholar]
- [19].Cameron ID, Chen JS, March LM, et al. Hip fracture causes excess mortality owing to cardiovascular and infectious disease in institutionalized older people: a prospective 5-year study. J Bone Miner Res 2010;25:866–72. [DOI] [PubMed] [Google Scholar]
- [20].Higgins J, Green S, (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration 2011. www.cochrane-handbook.org. [Google Scholar]
- [21].Harris JD, Quatman CE, Manring MM, et al. How to write a systematic review. Am J Sports Med 2014;42:2761–8. [DOI] [PubMed] [Google Scholar]
- [22].Leuzinger E, Poblete B, Konrad CJ, et al. How current transfusion practices in geriatric patients with hip fracture still differ from current guidelines and the effects on outcome: a retrospective observational study. Eur J Anaesthesiol 2018;35:972–9. [DOI] [PubMed] [Google Scholar]
- [23].Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics 1994;50:1088–101. [PubMed] [Google Scholar]
- [24].Egger M, David SG, Schneider M, et al. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997;315:629–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Carson JL, Terrin ML, Barton FB, et al. A pilot randomized trial comparing symptomatic vs. hemoglobin-level-driven red blood cell transfusions following hip fracture. Transfusion 1998;38:522–9. [DOI] [PubMed] [Google Scholar]
- [26].Foss NB, Kristensen MT, Jensen PS, et al. The effects of liberal versus restrictive transfusion thresholds on ambulation after hip fracture surgery. Transfusion 2009;49:227–34. [DOI] [PubMed] [Google Scholar]
- [27].Gregersen M, Borris LC, Damsgaard EM. Postoperative blood transfusion strategy in frail, anemic elderly patients with hip fracture. Acta Orthop 2015;86:363–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Parker MJ. Randomised trial of blood transfusion versus a restrictive transfusion policy after hip fracture surgery. Injury 2013;44:1916–8. [DOI] [PubMed] [Google Scholar]
- [29].Carson JL, Terrin ML, Noveck H, et al. Liberal or restrictive transfusion in high-risk patients after hip surgery. N Engl J Med 2011;365:2453–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Gruber-Baldini AL, Marcantonio E, Orwig D, et al. Delirium outcomes in a randomized trial of blood transfusion thresholds in hospitalized older adults with hip fracture. J Am Geriatr Soc 2013;61:1286–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Blandfort S, Gregersen M, Borris LC, et al. Blood transfusion strategy and risk of postoperative delirium in nursing homes residents with hip fracture. A post hoc analysis based on the TRIFE randomized controlled trial. Aging Clin Exp Res 2017;29:459–66. [DOI] [PubMed] [Google Scholar]
- [32].Zerah L, Dourthe L, Cohen-Bittan J, et al. Retrospective evaluation of a restrictive transfusion strategy in older adults with hip fracture. J Am Geriatr Soc 2018;66:1151–7. [DOI] [PubMed] [Google Scholar]
- [33].Mao TM, Gao FQ, Han J, et al. Restrictive versus liberal transfusion strategies for red blood cell transfusion after hip or knee surgery a systematic review and meta-analysis. Medicine (Baltimore) 2017;96:e7326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Liumbruno GM, Biancofiore G, Marano G, et al. Liberal transfusion strategy improves survival in perioperative but not in critically ill patients A meta-analysis of randomised trials. Br J Anaesth 2015;115:511–9. [DOI] [PubMed] [Google Scholar]
- [35].Shokoohi A, Stanworth S, Mistry D, et al. The risks of red cell transfusion for hip fracture surgery in the elderly. Vox Sang 2015;103:223–30. [DOI] [PubMed] [Google Scholar]
- [36].Rohde JM, Dimcheff DE, Blumberg N, et al. Health care-associated infection after red blood cell transfusion: a systematic review and meta-analysis. JAMA 2014;311:1317–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Teng ZW, Zhu Y, Liu YG, et al. Restrictive blood transfusion strategies and associated infection in orthopedic patients: a meta-analysis of 8 randomized controlled trials. Sci Rep 2015;5:13421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Rubinstein C, Davenport DL, Dunnagan R, et al. Intraoperative blood transfusion of one or two units of packed red blood cells is associated with a fivefold risk of stroke in patients undergoing elective carotid endarterectomy. J Vasc Surg 2013;57suppl 2:53S–7S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Bucerius J, Gummert JF, Borger MA, et al. Stroke after cardiac surgery: a risk factor analysis of 16,184 consecutive adult patients. Ann Thorac Surg 2003;75:472–8. [DOI] [PubMed] [Google Scholar]
- [40].Wang Y, Shi X, Wen M, et al. Restrictive versus liberal blood transfusion in patients with coronary artery disease: a metaanalysis. Curr Med Res Opin 2017;33:761–8. [DOI] [PubMed] [Google Scholar]
- [41].Gu WJ, Gu XP, Wu XD, et al. Restrictive versus liberal strategy for red blood-cell transfusion. J Bone Joint Surg Am 2018;100:686–95. [DOI] [PubMed] [Google Scholar]


