Abstract
Rationale:
Although most complications of herpes zoster (HZ) are associated with the spread of varicella-zoster virus from the initially involved sensory ganglion, motor nerve impairment, such as limb weakness, is a rare but severe complication that is difficult to treat.
Patient concern:
A 73-year-old female presented with sudden left upper limb pain and weakness after HZ.
Diagnosis:
Brachial plexopathy following HZ (postherpetic brachial plexopathy).
Intervention:
Despite alleviation of the vesicles with antiviral treatments, the left upper limb weakness and neuropathic pain did not improve. After obtaining patient's consent, ultrasound-guided polydeoxyribonucleotide (PDRN) injection was performed around the left brachial plexus.
Outcomes:
The patient showed marked improvement in left arm pain from numerical rating scale (NRS) 9 to 4, 1 day after PDRN injection. Subsequently, the pain improved to NRS 3, and motor weakness improved to Medical Research Council grade 2 to 4.
Lessons:
PDRN can be considered a viable substitute for corticosteroid injection in treatment of motor weakness and neuropathic pain after HZ.
Keywords: brachial plexus, herpes zoster, polydeoxyribonucleotide, postherpetic neuralgia, ultrasonography
1. Introduction
Herpes zoster (HZ) usually results from reactivation of endogenous varicella-zoster virus (VZV) that persisted in latent form within the sensory ganglia.[1,2] Most complications of HZ are associated with the spread of VZV from the initially involved sensory ganglion.[1] However, motor nerve impairment after HZ, such as limb weakness, is a rare but burdensome complication that is difficult to treat. The corticosteroids have previously been reported to be effective in managing postherpetic motor and sensory neuropathies, owing to their anti-inflammatory effects.[3] However, it's use may be limited because of various side effects, such as adrenal suppression, glucocorticoid-induced osteoporosis, and cognitive and mood disorders.[4] Recently, polydeoxyribonucleotide (PDRN) has been reported as a viable substitute for corticosteroids in various musculoskeletal disorders.[4–8] Here, we reported a case of a patient with brachial plexopathy following HZ (postherpetic brachial plexopathy), who showed improvement after administration of ultrasound-guided PDRN injection around the brachial plexus. This case report was approved by the institutional review board of Daegu Fatima Hospital (DFH17ORIO343). Informed written consent was obtained from the patient for publication of this case report and accompanying images.
2. Case report
A 73-year-old Asian female with a history of well-controlled hypertension and hyperlipidemia presented with sudden left upper limb pain, graded numeric rating scale[9] (NRS) 9, and weakness. This was preceded by paresthesia for 3 days in the left posterior neck and left arm. Magnetic resonance imaging (MRI) of the spine did not show any evidence of spinal disease. However, characteristic grouped vesicles and surrounding erythema were developed on the dermatome of 5th and 6th cervical root, 3 days after development of the pain. There was a weakness in the left shoulder, which was rated Medical Research Council (MRC)[10] grade 2 in the manual muscle test (Fig. 1A). The remaining neurological examination was insignificant. With clinical identification of HZ, antiviral and pain control therapy was started with IV acyclovir (5 mg/kg/d), pregabalin (150 mg/d), and Helium-Neon laser (632.8 nm/8.5 mW, 10 min/d) for 8 days. Despite resolution of the vesicles and erythema, the weakness did not improve. In electrophysiological studies, performed 3 weeks after onset of symptoms, left brachial plexopathy was diagnosed. Brachial plexus MRI was acquired 21 days after the onset of symptoms. Coronal T2-weighted short tau inversion recovery images demonstrated mild swelling and increased signals in the left brachial plexus, especially in the C5 and C6 dorsal root ganglia and roots. With the result of studies and clinical history, postherpetic brachial plexopathy was diagnosed (Fig. 1B). Patient was initially treated with pregabalin (150 mg/d) and fentanyl patch (25 μg/h) for pain control, but these were discontinued due to the side effects, such as nausea and vomiting. The non-steroidal anti-inflammatory drugs were tried but also discontinued due to the side effect; heartburn. Next, the patient was recommended for corticosteroid injection around the brachial plexus, but she refused the injection due to concerns regarding the metabolic side effects of corticosteroids. Then, after she was adequately informed about the anti-inflammatory effects of PDRN, the patient agreed to receive a PDRN (Rejuvenex, Pharma Research, South Korea) injection. Ultrasound-guided injection was performed with PDRN (PDRN [5.625 mg/3 mL] + 1% lidocaine [7 mL], total: 10 mL) around the left brachial plexus (Fig. 1C). After single day, the patient showed marked alleviation of left arm pain from NRS 9 to 4. Three more PDRN injections were performed at a weekly interval. After the treatments, the left arm pain was maintained at NRS 3 for 6 months and motor weakness improved from MRC grade 2 to 4.
Figure 1.
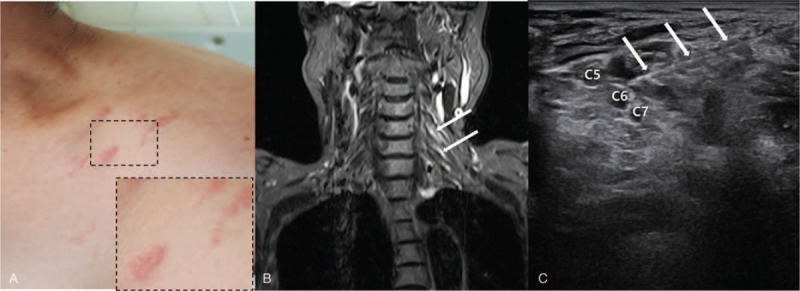
(A) The erythematous vesicular eruption is distributed around the left shoulder. (B) Brachial plexus MRI acquired 21 days after the onset of symptoms. Coronal T2-weighted short tau inversion recovery images demonstrate mild swelling and increased signals in the left brachial plexus especially in the C5 and C6 dorsal root ganglia and roots (white arrow) (C) Ultrasound-guided PDRN injection (white arrow) to the left C5 and C6 root. MRI = magnetic resonance images, PDRN = polydeoxyribonucleotide.
3. Discussion
The VZV usually invades sensory nerves; however, it can also invade motor nerves, especially the anterior spinal nerve root or anterior horn cell. Invasion of the brachial plexus is also uncommon.[3] In previous studies, the motor neuropathy caused by HZ was suggested to be associated with an inflammatory demyelinating process.
PDRN is obtained from the sperm of salmon and acts via stimulation of the A2A receptor.[11] Adenosine is a purine nucleoside that is released from variety of cells in response to several types of stress.[12] It has previously been suggested that adenosine regulates inflammation via interaction with 1 or more of 4 known receptors (A1, A2A, A2B, and A3).[12] Among the receptors, stimulation of A2A receptor is known to inhibit production of pro-inflammatory cytokines, such as tumor necrosis factor-α, in human peripheral blood mononuclear cells. Moreover, in a previous study, PDRN was shown to decrease the circulating levels and cartilage expression of the inflammatory cytokines in an animal model of rheumatoid arthritis.[13] These results suggested that PDRN may potentially be a viable therapeutic alternative to corticosteroids. In our case, a patient with postherpetic motor and sensory neuropathies exhibited amelioration of her symptoms after ultrasound-guided peri-brachial plexus PDRN injections. The neurological symptoms seem to have improved due to the anti-inflammatory effects of PDRN. Therefore, when the use of corticosteroids is restricted due to their side effects, PDRN can be considered.
Different studies have reported different prognosis of postherpetic brachial plexitis. Motor recovery varied from full recovery within a few days to partial recovery after 2 years.[1,3,14–16] Our patient did not gain full recovery, even after 6 months. This is thought to be due to the degree of motor nerve involvement. However, more studies are needed to reveal the exact prognosis of this disease.
In conclusion, PDRN injection can be considered a viable substitute of corticosteroid injection, when the use of corticosteroid is restricted due to side effects.
Author contributions
Supervision: Jong-Moon Hwang, Jin-Sung Park, Sungwon Park, Byung Joo Lee.
Writing – original draft: Jun Young Kim, Donghwi Park.
Writing – review and editing: Donghwi Park.
Footnotes
Abbreviations: HZ = herpes zoster, MRI = magnetic resonance imaging, NRS = numeric rating scale, PDRN = polydeoxyribonucleotide, VZV = varicella-zoster virus.
This research was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Science, ICT and Future Planning (NRF- 2017R1D1A1B03033127) (NRF- 2018R1C1B5085905).
No commercial party having a direct financial interest in the results of the research supporting this article has or will confer a benefit upon the authors or upon any organization with which the authors are associated.
The authors have no conflicts of interest to disclose.
References
- [1].Fabian VA, Wood B, Crowley P, et al. Herpes zoster brachial plexus neuritis. Clin Neuropathol 1997;16:61–4. [PubMed] [Google Scholar]
- [2].Kim JM, Lee Z, Han S, et al. Treatment of Ramsay-Hunt's syndrome with multiple cranial nerve involvement and severe dysphagia: a case report. Medicine 2018;97:e0591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Kim JG, Chung SG. Herpetic brachial plexopathy: application of brachial plexus magnetic resonance imaging and ultrasound-guided corticosteroid injection. Am J Phys Med Rehabil 2016;95:e67–71. [DOI] [PubMed] [Google Scholar]
- [4].Park D, Yu KJ, Cho JY, et al. The effectiveness of 2 consecutive intra-articular polydeoxyribonucleotide injections compared with intra-articular triamcinolone for hemiplegic shoulder pain: a STROBE-complaint retrospective study. Medicine 2017;96:e8741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Lee GJ, Park D. Usefulness of polydeoxyribonucleotide as an alternative to corticosteroids in patients with lateral epicondyitis: a case series. Medicine 2018;97:e10809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Park JS, Park D. Effect of polydeoxyribonucleotide injection in a patient with carpal tunnel syndrome. Am J Phys Med Rehabil 2018;97:e93–5. [DOI] [PubMed] [Google Scholar]
- [7].Park D. Application of ultrasound-guided C5 nerve root block using polydeoxyribonucleotide in traumatic C5 nerve root injury caused by fracture of the articular process of the cervical spine: a case report. Medicine 2017;96:e8728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Ryu K, Ko D, Lim G, et al. Ultrasound-guided prolotherapy with polydeoxyribonucleotide for painful rotator cuff tendinopathy. Pain Res Manag 2018;2018:8286190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Joos E, Peretz A, Beguin S, et al. Reliability and reproducibility of visual analogue scale and numeric rating scale for therapeutic evaluation of pain in rheumatic patients. J Rheumatol 1991;18:1269–70. [PubMed] [Google Scholar]
- [10].Park D, Lee SH, Shin JH, et al. Lower limb muscle magnetic resonance imaging in myotonic dystrophy type 1 correlates with the six-minute walk test and CTG repeats. Neuromuscul Disord 2018;28:29–37. [DOI] [PubMed] [Google Scholar]
- [11].Bianchini P, Tellini N, Morani AM, et al. Pharmacological data on polydeoxyribonucleotide of human placenta. Int J Tissue React 1981;3:151–4. [PubMed] [Google Scholar]
- [12].Jacobson KA, Gao ZG. Adenosine receptors as therapeutic targets. Nat Rev Drug Discov 2006;5:247–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Bitto A, Polito F, Irrera N, et al. Polydeoxyribonucleotide reduces cytokine production and the severity of collagen-induced arthritis by stimulation of adenosine A((2)A) receptor. Arthrit Rheumat 2011;63:3364–71. [DOI] [PubMed] [Google Scholar]
- [14].Teo HK, Chawla M, Kaushik M. A rare complication of herpes zoster: segmental zoster paresis. Case Rep Med 2016;2016:7827140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Choi JY, Kang CH, Kim BJ, et al. Brachial plexopathy following herpes zoster infection: two cases with MRI findings. J Neurol Sci 2009;285:224–6. [DOI] [PubMed] [Google Scholar]
- [16].Jones LK, Jr, Reda H, Watson JC. Clinical, electrophysiologic, and imaging features of zoster-associated limb paresis. Muscle Nerve 2014;50:177–85. [DOI] [PubMed] [Google Scholar]


