Abstract
Rationale:
Many studies have shown that cataract surgery can be performed safely and improve visual acuity, without increasing the risk of progression of existing age-related macular degeneration (AMD). Data are emerging for an intraocular lens (IOL) that utilizes an advanced optical design to optimize the image supplied to all areas of the macula and not just the foveal center, which may benefit patients with center-involving macular disorders.
Patient concerns:
An 83-year-old Caucasian female presented with poor contrast sensitivity and color perception with increasing glare over the preceding year.
Diagnosis:
She had a progressive cortical cataract and stable dry AMD in the left eye, and wet AMD in the right eye. In the left eye, preoperative best-corrected distance visual acuity (BCDVA) was 0.2 (decimal) and best-corrected near visual acuity (BCNVA) was 0.05 (decimal).
Interventions:
Standard small-incision phacoemulsification was performed in the left eye, with capsular bag implantation of EyeMax Mono (LEH Pharma, London, UK), a single-piece, soft, hydrophobic, acrylic IOL designed to optimize image quality across the macula, rather than a standard monofocal lens.
Outcomes:
At 6 months postoperation, visual acuity in the left eye had markedly improved, with a BCDVA of 0.5 (decimal) and a BCNVA of 0.2 (decimal).
Conclusion:
In this first case undertaken at our center (and the first in Austria), cataract extraction and EyeMax Mono implantation were performed safely, with good subjective and objective outcome measures consistent with the effects of image optimization across the macula. Further studies of this IOL in patients with center-involving macular disorders, such as AMD, are warranted.
Keywords: AMD, EyeMax Mono, IOL, phacoemulsification, visual acuity
1. Introduction
Cataract and age-related macular degeneration (AMD) are aging-related phenomena that often co-exist in elderly patients. In the past, there have been concerns that cataract extraction by phacoemulsification might be associated with an increased risk of AMD progression. However, many studies (including the age-related eye disease study 2 [AREDS2]) have since shown that cataract surgery may be performed safely and has the potential to improve visual acuity without increasing the risk of progression to exudative AMD.[1,2]
As a result of cataract surgery, pseudophakic patients with AMD may experience improvements in contrast sensitivity, color perception, and best-corrected distance visual acuity (BCDVA). In AREDS2, patients with advanced AMD who received cataract surgery reported modest improvements in visual acuity, with a mean improvement of 6.8 early treatment diabetic retinopathy study (ETDRS) letters.[2]
Currently, patients with AMD who undergo cataract surgery often receive standard monofocal intraocular lenses (IOLs), prism IOLs or telescopic IOLs.[3] However, standard monofocal IOLs are optically designed to benefit normal-sighted individuals – similar to the natural crystalline lens, they focus light onto the fovea at the center of the macula. In contrast, patients with dry AMD experience a loss of function in this region of the eye, and their preferred retinal locus (PRL) may shift to the peripheral macula.[4] A poorer-quality image is provided by standard monofocal IOLs to the macula outside of the central few degrees, and this has negative consequences on visual function in patients with AMD. In undertaking activities of daily living, such as reading, patients with AMD are highly dependent on maximizing contrast sensitivity and fixation stability.[5]
Data are now emerging for EyeMax Mono, a new single-piece, soft, hydrophobic, acrylic IOL that increases breadth of focus and reduces blur, thereby improving image quality across all areas of the macula and not just the foveal center.[6,7] The lens optics are wavefront-optimized to provide an enhanced quality of image to an area extending 10° from the foveal center, and laboratory simulations indicate that the lens delivers superior image quality compared with standard monofocal IOLs at 4° and 7.5° of retinal eccentricity.[6]
2. Case presentation
Herein we report the case of an 83-year-old Caucasian female, presenting with symptoms of poor contrast sensitivity and color perception with increasing glare over the course of the preceding year. Written informed consent was obtained from the patient for the interventions completed and for publication of this report. Although not a formal clinical trial, the principles detailed in the Declaration of Helsinki have been considered for production of this case report.
Cortical cataract (C5 based on the Lens Opacities Classification System III grading system) and stable dry AMD were noted in the left eye, with poor image on fundoscopy (Fig. 1). In the left eye, which was the current target, pre-operative BCDVA and best-corrected near visual acuity (BCNVA) were 0.2 (decimal) and 0.05 (decimal), respectively (Fig. 2). BCNVA in the right eye was hand movements only as a result of a traumatic corneal injury with scattering approximately 14 years earlier, and wet AMD diagnosed 11 years ago requiring 26 intravitreal injections. Cataract surgery in the right eye with implantation of a monofocal IOL was undertaken 4 years previously.
Figure 1.
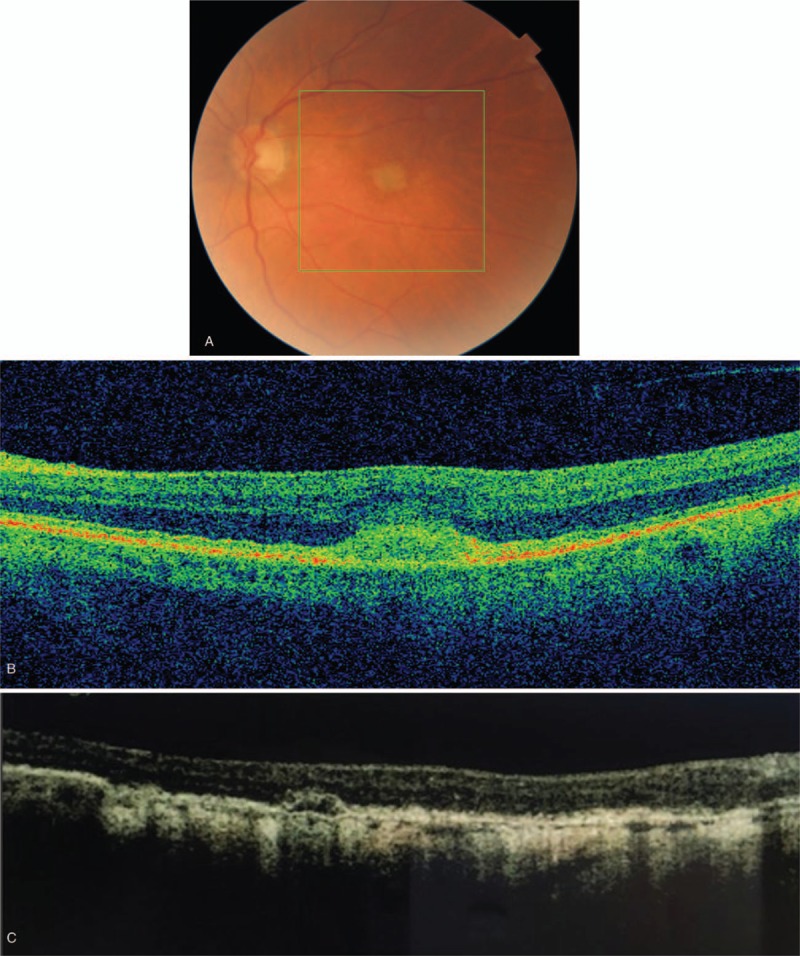
Preoperative imaging in the left eye, receiving an EyeMax Mono IOL. (A) Fundoscopy; (B) Optical coherence tomography; (C) Area of geographical atrophy: 0.91 mm2. IOL = intraocular lens.
Figure 2.
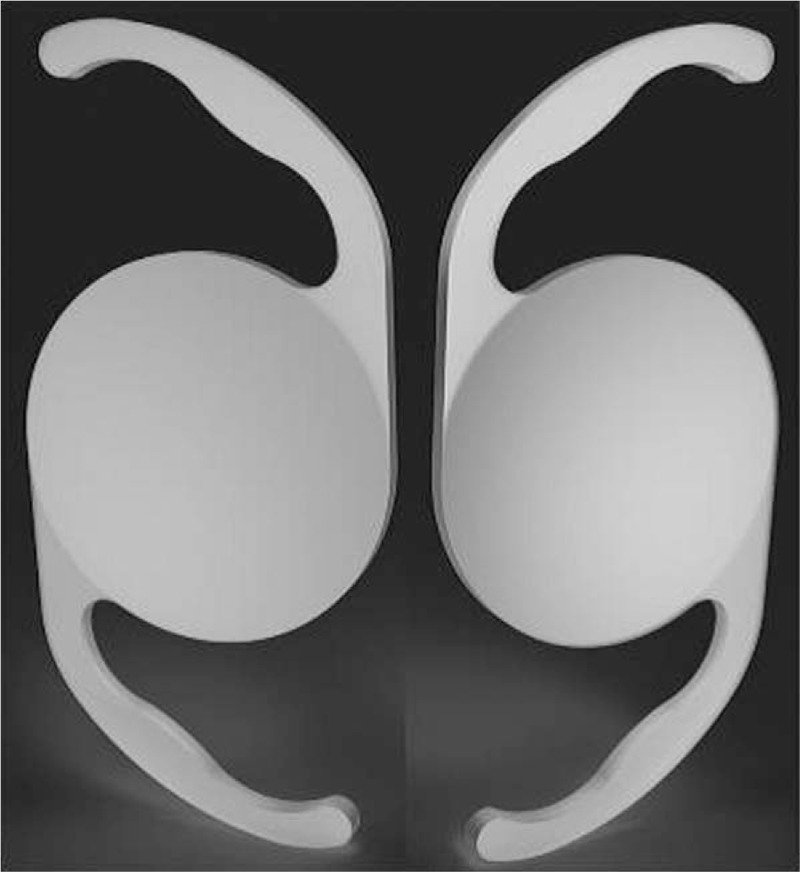
EyeMax Mono IOL (LEH Pharma, London, UK) showing the anterior view (left side) and posterior view (right side). IOL = intraocular lens.
Standard phacoemulsification cataract surgery with small incision, capsular bag implantation of the EyeMax Mono IOL (CE marked; LEH Pharma, London, UK; Fig. 3) was performed in the left eye in October 2017. The surgery was completed without complication and standard post-surgery/follow-up protocols were applied. Emmetropia was targeted and achieved. Visual acuity progressively improved following surgery and was stable by 6 months, with BCDVA and BCNVA improving to 0.5 (decimal) and 0.2 (decimal), respectively (X). The patient reported subjective improvement immediately after surgery for distance vision; with near vision, incremental improvements were reported over the first 3 months, which is consistent with a neuro-adaptive component that may occur with this type of IOL.[7] No vision rehabilitation training was required.
Figure 3.
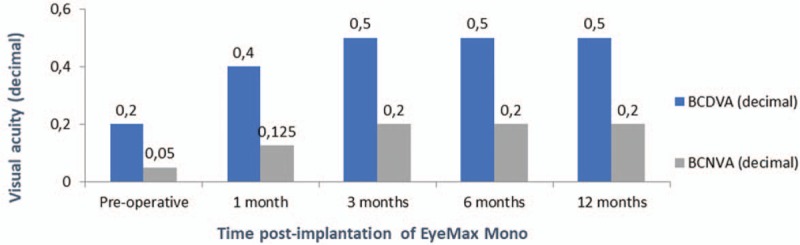
Visual acuity changes post-implantation of EyeMax Mono. BCDVA = best-corrected distance visual acuity, BCNVA = best-corrected near visual acuity.
No halos or glare were reported and no posterior capsular opacification was observed (evaluation period was 8 months). Intraocular pressures remained within the normal range and no other complications or side effects occurred.
3. Discussion
Few treatments are available for patients with AMD. For those with choroidal neovascularization (wet AMD), intravitreal antivascular endothelial growth factor therapy has the potential to stabilize or improve vision.[8] However, due to the progressive nature of the disease, even these patients ultimately lose vision over time.[8] For the remaining 90% of patients with dry AMD, only supportive measures are widely available and cataract surgery often constitutes the most promising opportunity to improve their vision.
Currently available surgically implanted IOLs used in patients with AMD include standard monofocal IOLs, prism IOLs, and telescopic IOLs.[3] The limitations of these lenses can include a restricted field of view, a range of potential complications, and endothelial cell loss; and some lenses can require a period of post-surgical visual rehabilitation to optimize outcomes.[3] Intraocular telescopes have been available for many years but their risk/benefit profile is generally poor, with application being limited to only 1 eye in patients with advanced AMD and severe visual impairment.[9,10] Intraocular telescopes can be large devices, requiring a longer incision (and a higher level of surgical skill) than foldable lenses,[3] and they generally require a period of post-operative visual rehabilitation.[3,11] Meanwhile, standard monofocal IOLs offer limited functional benefits to patients with dry AMD, as they are designed to focus light onto the fovea (the area of greatest functional loss in progressive disease).[12–14]
Until recently, there was no IOL specifically designed to optimize the image supplied to PRL (those areas of the peripheral macula that patients become increasingly dependent on as AMD progresses). The availability of the EyeMax Mono IOL offers a potential step-change in the management of patients with dry AMD who undergo cataract surgery. The EyeMax Mono is similar to a standard monofocal IOL, except that its optics are refined to generate transverse asphericity and maintain a breadth of focus across the macula (in much the same way that longitudinal asphericity is employed to generate depth of focus and reduce dependence on spectacles). The effect is to provide a high-quality image with reduced blur in areas of the macula extending up to 10° from the center of the fovea, where photoreceptor cell densities may still afford visual acuities of 6/30 Snellen or better. The lens is also designed to minimize chromatic aberration, further optimizing image quality delivered to the macula. As with a standard monofocal IOL, EyeMax Mono may be implanted in 1 or both eyes, and surgeons can select a hypermetropic refractive target in severe AMD cases to generate 10% to 20% magnification with the aid of spectacle correction. The goal of this IOL is to supply the highest quality image to the patient's PRL and other functioning areas of the retina that they depend on or may become dependent on as the macular disease progresses.[7]
In our case study, we report improvements in visual acuity consistent with previously published results with EyeMax Mono. After 3 months, our patient improved by 0.3 (decimal) in BCDVA in the left eye, equivalent to approximately 20 ETDRS letters.
In a prospective pilot study in 8 eyes of 7 patients with bilateral dry AMD and 1+ or lower cataract, with a preoperative CDVA of 0.60 LogMAR (logarithm of minimum angle of resolution) or worse, the mean ETDRS improvement 2 months after EyeMax Mono implantation was 18 letters.[7] In a case series of 244 eyes with dry AMD or stable, wet AMD with a pre-operative visual acuity of ≥0.3 LogMAR, the mean CDVA (LogMAR) improved by −0.35 (equating to a gain of 18 ETDRS letters) 3 months after EyeMax Mono implantation.[6] Microperimetric studies have suggested that improvements in visual function continue for a few months after EyeMax Mono implantation, as patients adjust fixation to take advantage of image optimization at the PRL with varying degrees of neuro-adaptation – an effect we observed in our patient at near vision.[7]
In conclusion, in this first case study undertaken at our center (first case in Austria), cataract extraction and implantation of the EyeMax Mono IOL was performed safely, with improved subjective and objective outcome measures consistent with the effects of image optimization across the macula. Our initial experience with the EyeMax Mono IOL is supported by published data indicating that an IOL designed to increase the breadth of focus is capable of delivering superior visual outcomes in patients with center-involving maculopathy safely and without the disadvantages associated with intraocular telescope implantation. Optimizing image quality across the macula should, in theory, result in improved functional outcomes, and results from future studies exploring this are eagerly awaited. The ultimate goal of IOL implantation is enhancing patient quality of life and self-autonomy. Overall, the results indicate that EyeMax Mono helps to address the unmet needs in selected cases of dry AMD. Implanted at the right time, and using the right procedures, it is a powerful tool in focussing the battle against dry AMD. The most important principle is to be completely honest, and to focus on mutual trust between patient and surgeon rather than promising miracles. When selected for the right cases, EyeMax Mono is extremely effective.
Author contributions
Conceptualization: Andreas F. Borkenstein.
Investigation: Andreas F. Borkenstein.
Methodology: Eva-Maria Borkenstein.
Supervision: Eva-Maria Borkenstein.
Writing – original draft: Andreas F. Borkenstein.
Andreas F. Borkenstein orcid: 0000-0001-6341-9069.
Footnotes
Abbreviations: AMD = age-related macular degeneration, AREDS2 = age-related eye disease study 2, BCDVA = best-corrected distance visual acuity, BCNVA = best-corrected near visual acuity, ETDRS = early treatment diabetic retinopathy study, IOL = intraocular lens, LogMAR = logarithm of minimum angle of resolution, PRL = preferred retinal locus.
Ethics approval was not applicable for this 1-patient case study. The patient provided consent for phacoemulsification and IOL implantation with EyeMax Mono IOL (CE-marked).
The authors have no funding and conflicts of interest to disclose.
References
- [1].Ehmann DS, Ho AC. Cataract surgery and age-related macular degeneration. Curr Opin Ophthalmol 2017;28:58–62. [DOI] [PubMed] [Google Scholar]
- [2].Huynh N, Nicholson BP, Agron E, et al. Visual acuity after cataract surgery in patients with age-related macular degeneration: age-related eye disease study 2 report number 5. Ophthalmology 2014;121:1229–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Grzybowski A, Wasinska-Borowiec W, Alio JL, et al. Intraocular lenses in age-related macular degeneration. Graefes Arch Clin Exp Ophthalmol 2017;255:1687–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Fletcher DC, Schuchard RA. Preferred retinal loci relationship to macular scotomas in a low-vision population. Ophthalmology 1997;104:632–8. [DOI] [PubMed] [Google Scholar]
- [5].Crossland MD, Culham LE, Kabanarou SA, et al. Preferred retinal locus development in patients with macular disease. Ophthalmology 2005;112:1579–85. [DOI] [PubMed] [Google Scholar]
- [6].Qureshi MA, Robbie SJ, Hengerer FH, et al. Consecutive case series of 244 age-related macular degeneration patients undergoing implantation with an extended macular vision IOL. Eur J Ophthalmol 2018;28:198–203. [DOI] [PubMed] [Google Scholar]
- [7].Robbie SJ, Tabernero J, Artal P, et al. Initial clinical results with a novel monofocal-type intraocular lens for extended macular vision in patients with macular degeneration. J Refract Surg 2018;34:718–25. [DOI] [PubMed] [Google Scholar]
- [8].Rofagha S, Bhisitkul RB, Boyer DS, et al. Seven-year outcomes in ranibizumab-treated patients in ANCHOR, MARINA, and HORIZON: a multicenter cohort study (SEVEN-UP). Ophthalmology 2013;120:2292–9. [DOI] [PubMed] [Google Scholar]
- [9].Orzalesi N, Pierrottet CO, Zenoni S, et al. The IOL-Vip System: a double intraocular lens implant for visual rehabilitation of patients with macular disease. Ophthalmology 2007;114:860–5. [DOI] [PubMed] [Google Scholar]
- [10].Hudson HL, Lane SS, Heier JS, et al. Implantable miniature telescope for the treatment of visual acuity loss resulting from end-stage age-related macular degeneration: 1-year results. Ophthalmology 2006;113:1987–2001. [DOI] [PubMed] [Google Scholar]
- [11].Dunbar HMP, Dhawahir-Scala FE. A discussion of commercially available intra-ocular telescopic implants for patients with age-related macular degeneration. Ophthalmol Ther 2018;7:33–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Kessel L, Erngaard D, Flesner P, et al. Cataract surgery and age-related macular degeneration. An evidence-based update. Acta Ophthalmol 2015;93:593–600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Casparis H, Lindsley K, Kuo IC, et al. Surgery for cataracts in people with age-related macular degeneration. Cochrane Database Syst Rev 2017;2:CD006757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Kessel L, Koefoed Theil P, Lykke Sorensen T, et al. Cataract surgery in patients with neovascular age-related macular degeneration. Acta Ophthalmol 2016;94:755–60. [DOI] [PubMed] [Google Scholar]


