Abstract
Background:
Postcholecystectomy syndrome (PCS) is a term used to describe the persistence of biliary colic or right upper quadrant abdominal pain with a variety of postoperative gastrointestinal symptoms. Acupuncture and related treatments have shown clinical effects for PCS in many studies. But the systematic reviews and meta-analyses for them are lacking. We aim to evaluate the efficacy and safety of acupuncture on the treatment of PCS.
Methods:
We will search 8 electronic databases, including the Web of Science, PubMed, Cochrane Library, Embase, and 4 Chinese databases (CBM, Wanfang, VIP, and CNKI databases), and additional sources (WHO ICTRP, ChiCTR, Clinical Trials, Grey Literature Database), for potentially eligible studies. Literature retrieval, screening, and data extraction will be conducted by 2 researchers independently. In case of disagreement, a 3rd party shall be consulted to assist judgment. We will use RevmanV.5.3 to perform a fixed effect meta-analysis on the data of clinical homogeneity studies, and evidence's level will be assessed through the method for GRADE.
Results:
This systematic review and meta-analysis will put a high-quality synthesis of the efficacy and safety of acupuncture treatment in PCS.
Conclusion:
The conclusion of this systematic review will provide evidence to assess acupuncture therapy is an efficacy and safe intervention to treat and control PCS.
Ethics and dissemination:
Since this article does not involve patients’ private data, no ethical approval is required. The agreement will be disseminated by peer-reviewed journals or conference reports.
Trial registration number:
PROSPERO CRD4201929287.
Keywords: acupuncture, postcholecystectomy syndrome, protocol, systematic review
1. Introduction
Cholecystectomy, approximately 700,000 cases performed each year,[1] is the most common gastrointestinal operation performed in the United States. Despite being the most commonly performed operations, sometimes cholecystectomy fails to relieve symptoms.[2] And 10% of patients may develop postcholecystectomy syndrome (PCS) weeks to month's later. PCS was 1st described in 1947 by Womack and Crider.[3] And it is defined as the recurrence of symptoms similar to those experienced before the cholecystectomy.[4] In 5% to 40% of patients with cholelithiasis, regardless of the type of surgery, the symptoms persist postoperatively.[5,6] And the incidence rate of the PCS in this study's population was 19.8%.[7] Approximately 5% to 40% of patients who have undergone cholecystectomy continue to have symptoms of abdominal pain, vomiting, gastrointestinal symptoms (dyspepsia, loose stool, and the like) and are thought to suffer from PCS.[7–11]
Causes of PCS are complicated and many can be attributed to extra-biliary causes.[7] So the treatments for PCS include physical therapy, medicine,[12–14] and surgical treatment.[15] In eastern, physical treatment such as acupuncture has a good effect for PCS.[16–19] Acupuncture has been widely used in treating the symptoms.[20] However, to our knowledge, the randomized controlled trials (RCTs) examining the effectiveness and safety of acupuncture for PCS have never been systematically evaluated. Therefore, we will carry out this study to evaluate the evidence of RCTs for acupuncture treatment of PCS.
2. Methods
2.1. Design and registration of the review
This SR has been registered on PROSPERO and registration number is CRD42019129287 and the protocol is based on the PRISMA-P guidelines.[21]
2.2. Inclusion criteria for study selection
2.2.1. Type of study
All the studies of acupuncture in the treatment of PCS and the included studies will be all RCTs without limitation on language or publication types restriction. Nonrandomized clinical studies, quasi-RCTs, cluster RCTs, and case reports will be excluded.
2.2.2. Types of participants
Trials involving patients who are diagnosed PCS will be included.
2.2.3. Types of interventions
Acupuncture and related treatments will be used in the intervention group. Studies using acupuncture in experimental group will be included regardless of the treatment length and frequency. And control group will consist of drugs, placebo, sham acupuncture, etc.
2.2.4. Types of outcome measures
2.2.4.1. Primary outcomes
Pain intensity (relevant confirmed pain measurement scales such as visual analog scale), the nausea incidence and the vomiting incidence will be analyzed.
2.2.4.2. Secondary outcomes
-
1.
The recovery of gastrointestinal function: first defecation time, 1st flatus time, 1st bowel sounds time, duration of abdominal distension, etc.
-
2.
Adverse effects (relevant symptoms caused by acupuncture).
2.3. Data sources
We will search 8 electronic databases and additional sources, including the Web of Science, PubMed, Cochrane Library, Embase, CBM, Wanfang, VIP, CNKI, and WHO ICTRP, ChiCTR, Clinical Trials, Grey Literature Database, for potentially eligible studies. RCTs on acupuncture treatment in patients with PCS will be searched for independently by 2 reviewers in those sources.
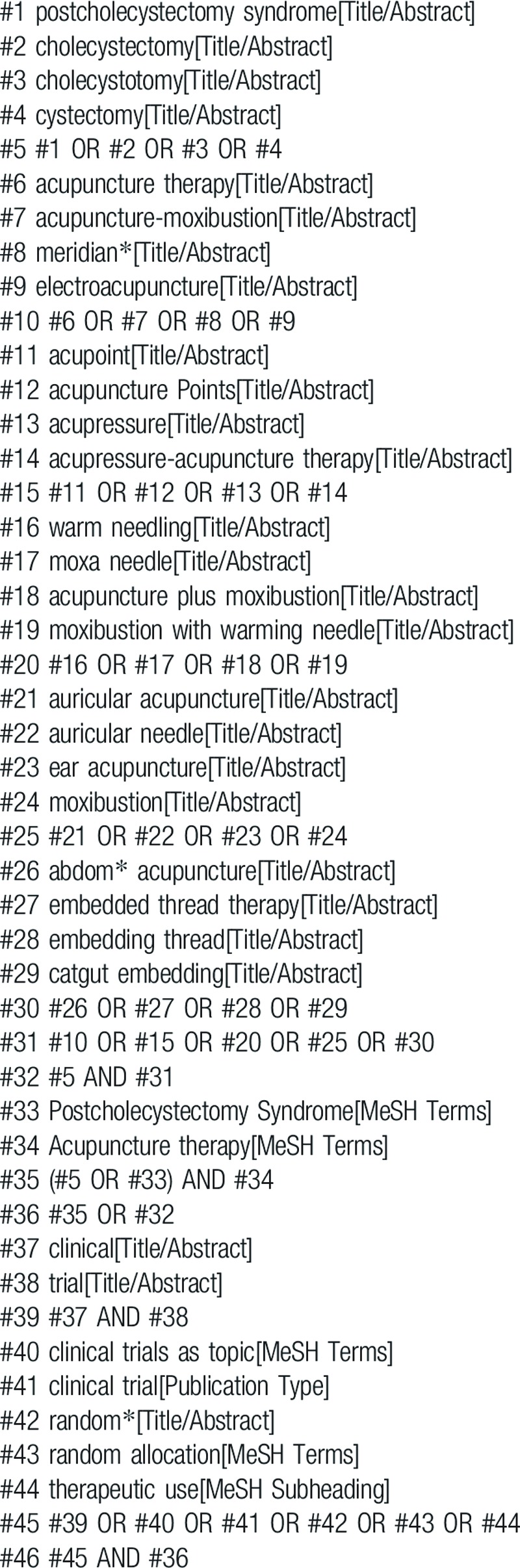
2.4. Search strategy
The details are adjusted according to the specific sources including CBM, CNKI, WF, VIP, Web of Science, Embase, PubMed, Cochrane Library, WHO ICTRP, ChiCTR, Clinical Trials, and Grey Literature Database. The search strategy for PubMed is shown in Table 1.
Table 1.
Search strategy for the PubMed database.
2.5. Data collection and analysis
2.5.1. Selection of studies
All reviewers will have a professional training about background, purpose, and process of the review. In the literature collection, the title and abstract of the literature will be 1st read to eliminate duplicate literature and the eligible studies searched will be uploaded to a database set up through NoteExpress. Two review authors will select and record independently through screening the titles, abstracts, and key words. Any disagreement about the inclusion of the studies will be resolved through discussion between the 2 review authors. If the discussion cannot reach an agreement, the arbiter will make a final decision of the study selection. If authors are similar or incidence data are extracted from the same database, the study period will be assessed. Details of the selection procedure for studies are shown in a PRISMA-P flow chart (Fig. 1)
Figure 1.
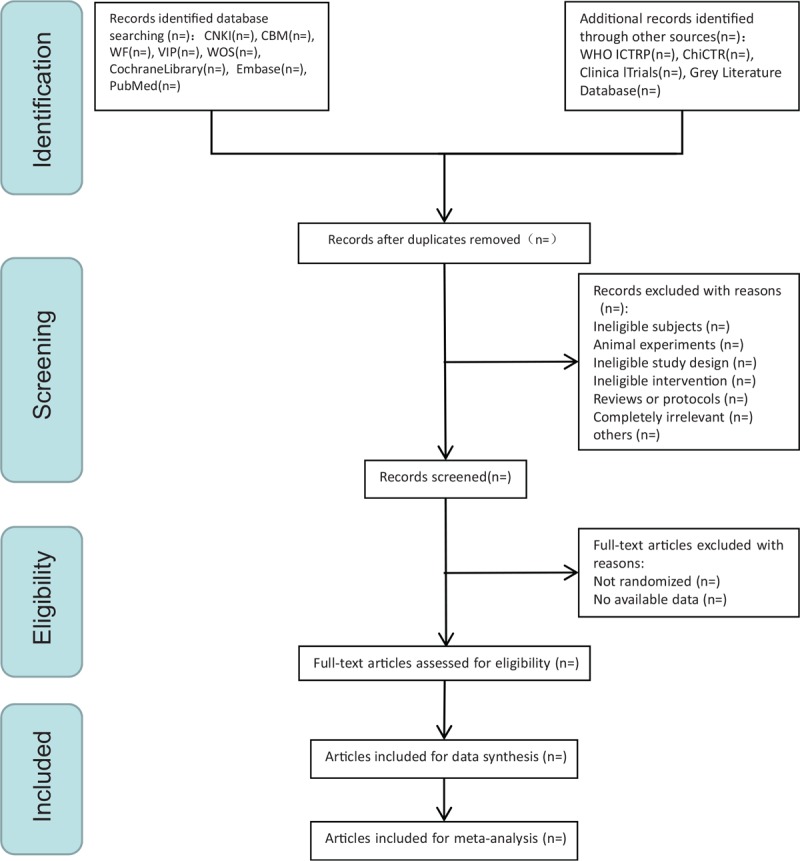
The Preferred Reporting Items for Systematic Reviews and Meta-analyses Protocols flow chart of selection process.
2.5.2. Data extraction and management
Data extraction will be also conducted by 2 researchers independently through a standardized eligibility form. In case of disagreement, a 3rd party (the arbiter) shall be consulted to assist judgment, and the missing information shall be supplemented by contacting the author. The general information of the selected articles will be extracted, including 1st author, year of publication, country, study design, sample size, detailed intervention, control treatment, duration of disease, duration of follow-up, and the like. When the data of articles are insufficient or ambiguous, one of the authors will in contact with the original author to request detailed about the research by e-mail or telephone or estimate the data.
2.5.3. Assessment of risk bias
Two review authors will measure the risk of bias of the included studies with Cochrane Handbook V.5.3.0 independently, which includes the following 7 items: sequence generation, blinding of participants, blinding of outcome assessors, allocation concealment, incomplete outcome data, selective outcome reporting, and other sources of bias. It will be ranked risk level within categorized as low risk of bias, unclear risk of bias, and high risk of bias. In case of disagreement, the arbiter shall be consulted to assist judgment.
2.5.4. Measures of treatment effect
The dichotomous data will be analyzed by relative risk (RR) ratio with 95% confidence intervals (CIs), and the mean difference (MD) or standard MD (SMD) with 95% CIs will be used to estimate the continuous data.
2.5.5. Management of missing data
Where possible, we will analyze the data according to the intention-to-treat. If there is missing or incomplete data, we will contact the original investigator to verify the study characteristics and obtain missing numerical result data. If the missing data are not available, then this analysis will depend on the data available.
2.5.6. Assessment of heterogeneity
According to the Cochrane Handbook, we will choose the I2 statistic to measure heterogeneity among the studies in every analysis. When P > .1, I2 < 50%, it is considered that there is no heterogeneity between the experiment, and the fixed effects model will be used for statistics, otherwise, the random effects model is adopted to analyze.
2.5.7. Assessment of reporting biases
If the number of included studies is >10, we will use funnel plots to measure publication bias. If funnel chart is evenly distributed, it indicates no reporting bias, and vice versa.
2.5.8. Data synthesis
The data will be analyzed and synthesized through Review Manager 5.3 software which from Cochrane Collaboration will be employed to compute the data synthesis. The fixed effects model (I2 < 50%) or random effects model (I2 ≥ 50%) will be selected. All data will be analyzed with 95% CIs. The dichotomous data will be analyzed by RR, and the continuous data will be analyzed by MD or SMD.
2.5.9. Subgroup analysis
If we find substantial heterogeneity, subgroup analysis will be implemented according to acupuncture types, outcome measures, and the like.
2.5.10. Sensitivity analysis
We will carry out sensitivity analysis to identify the quality and robustness of the results in the review. The principal criteria include methodological quality, sample size, and analysis issue (such as missing data's efficacy). The meta-analysis will be operated repeatedly.
2.5.11. Grading the quality of evidence
The reviewers will use the GRADE rating standards.[22] The GRADE system will be used to GRADE the obtained outcome indicators from 5 items of research limitations, inconsistency, indirectness, inaccuracy, and publication bias. In the case of the RCTs, the GRADE classifies the evidence of the outcome indicators evaluated by the system, and all the outcome indicators are graded by quality through the GRADE rating standards. Then, evidence quality will be rated “high,” “moderate,” “low,” or “very low” according to the GRADE rating standards. The quality of the evidence is high, indicating that future research is unlikely to change existing evidence; “moderate” indicates that future research may have an important impact on existing evidence, and may change the evaluation results; Being low-level indicates that future research is likely to have a significant impact on existing evidence and may change the evaluation results; “very low” indicating that all existing evidence is highly uncertain.
3. Publication plan
The systematic review will be published in peer-reviewed journals in both electronic and print versions.
4. Discussion
The PCS is used to describe a collection of symptoms experienced by patients following cholecystectomy, many of which may not be attributed to disorder of biliary system.[23]
In China, acupuncture is the most common therapeutic option for diseases with pain. It is proved by clinical systematic reviews[24–26] that acupuncture reduces the symptom of PCS. Acupuncture also has good effects on nausea, vomiting, and gastrointestinal function illustrated in many SRs.[27–30]
It's a 1st SR about acupuncture treatment for PCS, we expect that this systematic review will provide clinical evidence for the efficacy and safety of current acupuncture treatment of PCS, provide medical staffs with more useful information, and provide patients with better advises. There may be some limitations in this SR, including different types of acupuncture, language limitations, lack of research, and the like, which may lead to substantial heterogeneity.
Author contributions
Conceptualization: Zihan Yin, Ying Cheng, Fan-rong Liang.
Data curation: Qiwei Xiao, Han Yang, Yanan Fu.
Formal analysis: Qiwei Xiao, Guixing Xu, Han Yang.
Funding acquisition: Fan-rong Liang.
Methodology: Guixing Xu.
Project administration: Fan-rong Liang.
Supervision: Jun Zhou, Jiao Chen, Ling Zhao.
Writing – original draft: Zihan Yin, Ying Cheng.
Writing – review & editing: Zihan Yin, Ying Cheng.
Zihan Yin orcid: 0000-0001-8741-1205.
Footnotes
Abbreviations: CBM = Chinese Biomedical Literature Database, ChiCTR = Chinese Clinical Trial Register, CNKI = China National Knowledge Infrastructure, GRADE = Grading of Recommendations Assessment, Development, and Evaluation, MD = mean difference, PCS = postcholecystectomy syndrome, PRISMA-P = Preferred Reporting Items for Systematic Reviews and Meta-analyses Protocols, RCTs = randomized controlled trials, RR = relative risk, SMD = standard mean difference, VIP = China Science and Technology Journal Database, WF = WanFang database, WHO ICTRP = World Health Organization International Clinical Trials Registry Platform.
ZY and YC are the first co-authors to this study.
This study is funded by Major program of the National Natural Science Foundation of China (fund no: 81590951).
The authors have no conflicts of interest to disclose.
References
- [1].Ahrendt SA, Pitt HA. Townsend CM, Beauchamp RD, Evers BM, Mattox KL. Biliary tract. Sabiston Textbook of Surgery: The Biological Basis of Modern Surgical Practice 17th edPhiladelphia, PA: Elsevier; 2004. 1597–639. [Google Scholar]
- [2].Arora D, Kaushik R, Kaur R, et al. Post-cholecystectomy syndrome: a new look at an old problem. J Minim Access Surg 2018;14:202–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Womack NA, Crider RL. The persistence of symptoms following cholecystectomy. Ann Surg 1947;126:31–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Jaunoo SS, Mohandas S, Almond LM. Postcholecystectomy syndrome (PCS). Int J Surg 2010;8:15–7. [DOI] [PubMed] [Google Scholar]
- [5].Murshid K. The postcholecystectomy syndrome: a review. Saudi J Gastroentero 1996;2:124–37. [PubMed] [Google Scholar]
- [6].Kouloura A, Sgourakis G, Lanitis S, et al. Enriched view of postcholecystectomy syndrome: nowadays and in former times. Hellenic J Surg 2015;87:156–64. [Google Scholar]
- [7].Shirah BH, Shirah HA, Zafar SH, et al. Clinical patterns of postcholecystectomy syndrome. Ann Hepatobiliary Pancreat Surg 2018;22:52–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Schofer JM. Biliary causes of postcholecystectomy syndrome. J Emerg Med 2010;39:406–10. [DOI] [PubMed] [Google Scholar]
- [9].Moore T, Amin M. Post-cholecystectomy syndrome. Clin Pract Cases Emerg Med 2017;1:446–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Glasgow RE, Mulvihill SJ. Feldman M, Friedman LS, Brandt LJ. Treatment of gallstone disease. Sleisenger & Fordtran's Gastrointestinal and Liver Diseases 8th edPhiladelphia, PA: Saunders; 2006. 1419–37. [Google Scholar]
- [11].Lum YW, House MG, Hayanga AJ, et al. Postcholecystectomy syndrome in the laparoscopic era. J Laparoendosc Adv Surg Tech A 2006;16:482–5. [DOI] [PubMed] [Google Scholar]
- [12].Lipnitskiĭ EM, Isakova OV, Movchun VA, et al. Effectiveness of Duspatalin therapy in the treatment and prevention of post-cholecystectomy syndrome [in Russian]. Vestn Ross Akad Med Nauk 2011. 7–11. [PubMed] [Google Scholar]
- [13].Wang L, Dong Y, Zhang J, et al. The efficacy of gabapentin in reducing pain intensity and postoperative nausea and vomiting following laparoscopic cholecystectomy: a meta-analysis. Medicine 2017;96:e8007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Ye F, Wu Y, Zhou C. Effect of intravenous ketamine for postoperative analgesia in patients undergoing laparoscopic cholecystectomy: a meta-analysis. Medicine 2017;96:e9147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Phillips MR, Joseph M, Dellon ES, et al. Surgical and endoscopic management of remnant cystic duct lithiasis after cholecystectomy—a case series. J Gastrointest Surg 2014;18:1278–83. [DOI] [PubMed] [Google Scholar]
- [16].Tan Y, Zhao Y, He T, et al. Efficacy and safety of auricular point acupressure treatment for gastrointestinal dysfunction after laparoscopic cholecystectomy: study protocol for a randomized controlled trial. Trials 2016;17:280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Samad K, Afshan G, Kamal R. Effect of acupressure on postoperative nausea and vomiting in laparoscopic cholecystectomy. J Pak Med Assoc 2003;53:68–72. [PubMed] [Google Scholar]
- [18].Agarwal A, Bose N, Gaur A, et al. Acupressure and ondansetron for postoperative nausea and vomiting after laparoscopic cholecystectomy. Canadian Journal of Anesthesia 2002;49:554–60. [DOI] [PubMed] [Google Scholar]
- [19].Agarwal A, Bose N, Gaur A, et al. Acupressure and ondansetron for postoperative nausea and vomiting after laparoscopic cholecystectomy. Can J Anesth 2002;49:554–60. [DOI] [PubMed] [Google Scholar]
- [20].S Y, C M Therapeutic observation of acupuncture plus Chinese medication for postcholecystectomy syndrome. Shanghai J Acupunct Moxibust 2016;35:291–3. [Google Scholar]
- [21].Shamseer L, Moher D, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ 2015;349:g7647. [DOI] [PubMed] [Google Scholar]
- [22].Guyatt GH, Oxman AD, Schünemann HJ, et al. GRADE guidelines: a new series of articles in the Journal of Clinical Epidemiology. J Clin Epidemiol 2011;64:380–2. [DOI] [PubMed] [Google Scholar]
- [23].Isherwood J, Oakland K, Khanna A. A systematic review of the aetiology and management of post cholecystectomy syndrome. Surgeon 2019;17:33–42. [DOI] [PubMed] [Google Scholar]
- [24].Paley CA, Tashani OA, Bagnall A, et al. A Cochrane systematic review of acupuncture for cancer pain in adults. BMJ Support Palliat Care 2011;1:51. [DOI] [PubMed] [Google Scholar]
- [25].Manyanga T, Froese M, Zarychanski R, et al. Pain management with acupuncture in osteoarthritis: a systematic review and meta-analysis. Bmc Complem Altern Med 2014;14:312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Hu C, Zhang H, Wu W, et al. Acupuncture for pain management in cancer: a systematic review and meta-analysis. Evid Based Complement Alternat Med 2016;2016:1–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Cheong KB, Zhang J, Huang Y, et al. The effectiveness of acupuncture in prevention and treatment of postoperative nausea and vomiting - a systematic review and meta-analysis. PLoS One 2013;8:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Usichenko TI, Hesse T. Appropriate timing and intensity of Pc6 stimulation for the prevention of postoperative nausea and vomiting. Acupunct Med 2016;34:70–1. [DOI] [PubMed] [Google Scholar]
- [29].Bik CK, Jiping Z, Yong H. Effectiveness of acupuncture in postoperative ileus: a systematic review and meta-analysis. J Tradit Chin Med 2016;36:271–82. [DOI] [PubMed] [Google Scholar]
- [30].Cheong KB, Zhang JP, Huang Y. The effectiveness of acupuncture in postoperative gastroparesis syndrome--a systematic review and meta-analysis. Complement Ther Med 2014;22:767–86. [DOI] [PubMed] [Google Scholar]


