Abstract
Background:
Male infertility has become a worldwide public health problem. However, the effect of low body mass index (BMI) is still controversial.
Methods:
Relevant articles in Pubmed, Embase, Web of science, and Wanfang database published until September 2017 were searched without language restriction. We performed a meta-analysis about low BMI and semen parameters containing total sperm count, concentration, semen volume, and sperm motility (overall and progressive), including 709 men with low BMI and 14,622 men with normal BMI.
Results:
Thirteen studies were included in this meta-analysis and a total of 15,331 individuals were accumulated. We pooled data from these articles and found standardized weighted mean differences in semen parameters (total sperm count and semen volume) showed significant difference between low BMI and normal BMI.
Conclusions:
This systematic review with meta-analysis has confirmed that there was a relationship between low BMI and semen quality, which suggesting low BMI may be a harmful factor of male infertility. Yet lacking of the raw data may influence the accuracy of the results. Further researches are needed to identify the role of underweight in male sterility.
Keywords: low body mass index, meta-analysis, semen parameters, underweight
1. Introduction
As an important clinical characteristic, body mass index (BMI) indicates the state of body to some extent. Increasing evidence suggested that high BMI (overweight and obesity) is a risk factor for people, which contributes to the development of many diseases, such as diabetes, cardiovascular disease, cancers, as well as male infertility.[1–3] Male infertility is a multi-factorial diseases, which is affected by genetic factors, environmental exposure as endocrine disrupters,[4,5] lifestyle-related factors,[6] and obesity.[7,8] Currently, the effect of obesity on male fertility has attracted more attention since a large number of related studies have gradually emerged.[9] However, whether men with low BMI has normal fertility or not is still unknown. As a well-known health risk,[10,11] low BMI could increase the mortality risk in patients with schizophrenia,[3] as well as compromise live birth rate in fresh transfer in vitro fertilization cycles.[12] Thus, it is important to pay additional attention to the effect of low BMI on fertility body.
A meta-analysis[13] published in 2013 identified a J-shaped association between BMI categories and risk of oligozoospermia or azoospermia, which suggests that low BMI may impair semen quality. Some studies have also identified that low BMI was associated with reduced semen quality, even though the affected semen parameters were not precisely the same. Jensen et al[14] reported that low BMI could reduce total sperm count and sperm concentration, and Paasch and colleagues[15] found a similar result that sperm count was decreased in underweight group than normal-weight group. In additional to sperm count, Luque et al[16] also reported a lower motility of underweight men. The analogous result about semen volume was found by Qiu et al.[17]
However, many researches also reported that no relationship exists between low BMI and any semen parameters, such as studies conducted by Belloc et al,[9] Duits et al,[18] and Shayeb et al[19] with a large number of participants.
We summarized all these relevant studies and performed this meta-analysis to investigate the effect of low BMI on several semen parameters, so as to reveal the relationship between low BMI and semen quality.
2. Materials and methods
2.1. Ethics statement
This is a meta-analysis based on published studies only, ethical approval was not necessary.
2.2. Search strategy and selection criteria
Relevant studies about BMI and semen parameters published until September 2017 from PubMed, Web of Science, Embase, and Wanfang database were searched regardless of language used. We performed a basic screen of these studies by browsing titles from databases, and removed duplicates and irrelevances. Then, articles that are reviews, or without data about the relationship between BMI and semen parameters, or irrelevances through viewing the abstracts were also excluded. Afterwards, we also excluded articles with no available data, articles could not be included in the analysis, and articles without data about underweight group. The references of the pivotal studies screened out were also searched to find out other relevant articles. At last, regardless of the origin, age, size, or ethnicity of participants, the eligible ones were incorporated into our study. The information about study characteristics and semen parameters of underweight and normal weight of these articles were extracted. The above work was completed by 2 authors independently. After discussion, they reached agreement.
The search strategy is taken as follows: (overweight OR weight OR obesity OR BMI OR body fat OR body weight OR body mass index OR adiposity OR IBW OR ideal weight) AND (sperm OR semen OR spermatozoa OR sperm count OR sperm concentration OR semen quality OR semen parameters OR sperm quantity OR total sperm count OR oligozoospermia OR azoospermia OR semen volume OR sperm motility OR spermatids OR spermatocytes OR spermatogonia).
2.3. Data synthesis and analysis
We performed this meta-analysis using articles including data about any 1 of semen parameters (total sperm count, sperm concentration, semen volume, sperm motility, or sperm progressive motility) in underweight and normal weight. In order to facilitate the calculation, we converted all data extracted to the form of mean and standard deviation. BMI was divided into 2 levers by World Health Organization (WHO) criteria: under 18.5 (underweight) and 18.5 to 24.9 (normal weight) kg/m2, except in some ones classifying according to their own standard. Group with a BMI between 18.5 and 24.9 was defined as the reference group. SMD was used as the effect scale index that calculated by mean, standard deviation and sample size using Stata version 12.0.
In order to evaluate the possible heterogeneity between articles, we accessed the I2 statistic. The random-effect model was used to assess standardized weighted mean differences (SMD) under the condition that P value for heterogeneity was ≤.10 or I2 ≥50%, which indicates a lack of high heterogeneity.[20] Additionally, we conducted sensitive analyses and subgroup to evaluate the effect of single literature and the ethnicity of study participants on the overall outcome, respectively. Egger test and Begg funnel plot were further calculated to show a diagnosis of publication bias. All statistical were performed with Stata version 12.0. P < .05 was defined as statistically significant.
3. Results
3.1. Result of search
We found a total of 32,946 articles, including 10,306, 11,712, 9568, and 1360 articles from PubMed, Web of Science, Embase, and Wanfang, respectively. Then, we excluded 32,465 studies including 14,298 duplicates and other irrelevances. After review of 481 abstracts, 57 studies were selected for further screening, which were potentially appropriate to be included in this meta-analysis. Finally, after excluding 7 ones without available data, 12 could not be included in the calculation, and 25 without data about underweight group, 13 articles studying the effect of low BMI on semen parameters were incorporated into our meta-analysis (Fig. 1).
Figure 1.
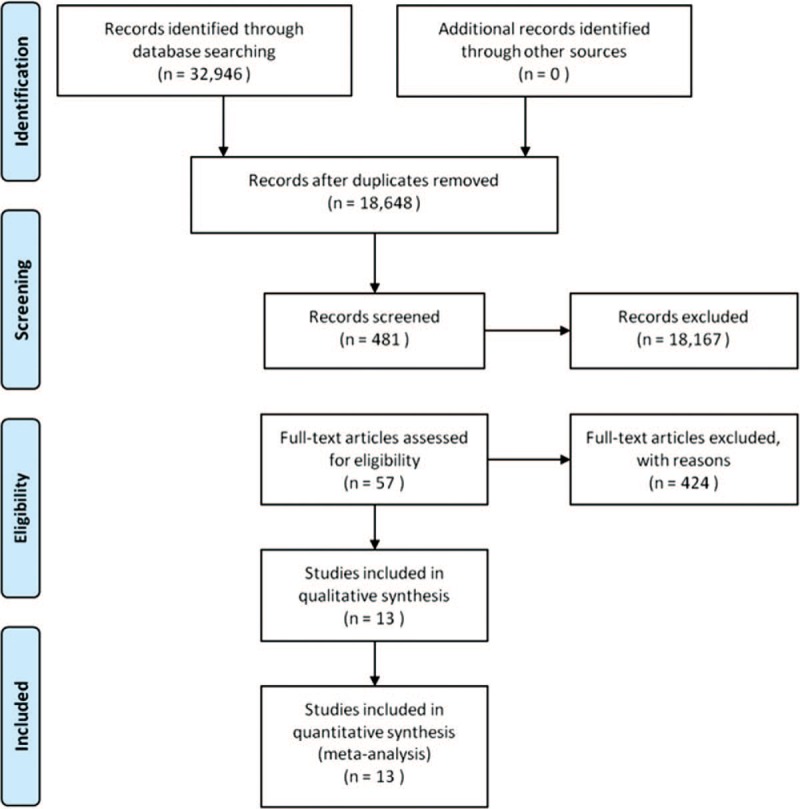
Flow chart of study selection.
3.2. Description of studies and participants
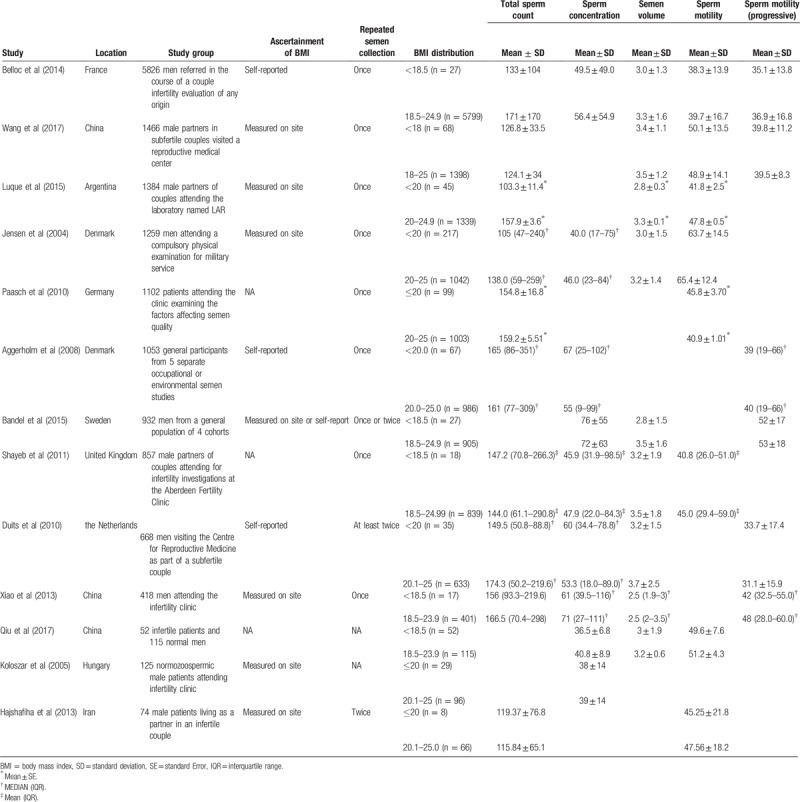
After a layer of screening, 13 articles (Table 1) with a total of 15,331 participants (709 belonging to underweight group, and 14,622 belonging to the reference group) were included in our meta-analysis. Six of these studies included more than 1000 participants, which constituted the main component of this meta-analysis. There are 3 articles that used 18.5 and 25.0 as the boundaries of BMI as prescribed by WHO, while 7 used 20.0 and 25.0, 1 used 18.5 and 24.0, and 1 used 18.0 and 25.0, respectively. All participants collected at least 1 semen sample for testing, who recruited from either a general population or subfertile couples, with 1 exception that from physical examination of conscription. Among these articles, researched outcomes including each semen parameters were as follows: total sperm count (10/13), concentration (10/13), volume (9/13), motility (8/13), and progressive motility (6/13). Data of height and weight used in these studies were all measured by professional researches except 4 self-reported and 3 without mention. Except for 2 case–control articles, a prospective cohort, and a retrospective study that reported cross-sectional data, all others were cross-sectional studies.
Table 1.
Summary of characteristics of observational studies included in this review.
3.3. Impact of BMI on semen parameters
Data from 13 articles were used to perform the meta-analysis in this review. After calculated the SMD of semen parameters in low BMI group compared with normal BMI group, the results showed that underweight decreased the level of total sperm count (P = .001) (Fig. 2) and semen volume (P = .001). At the same time, no significant statistical difference about changes of sperm concentration and sperm motility was observed. We only showed the result of total sperm count in this meta-analysis, while the results of other semen parameters did not show in any special figure.
Figure 2.
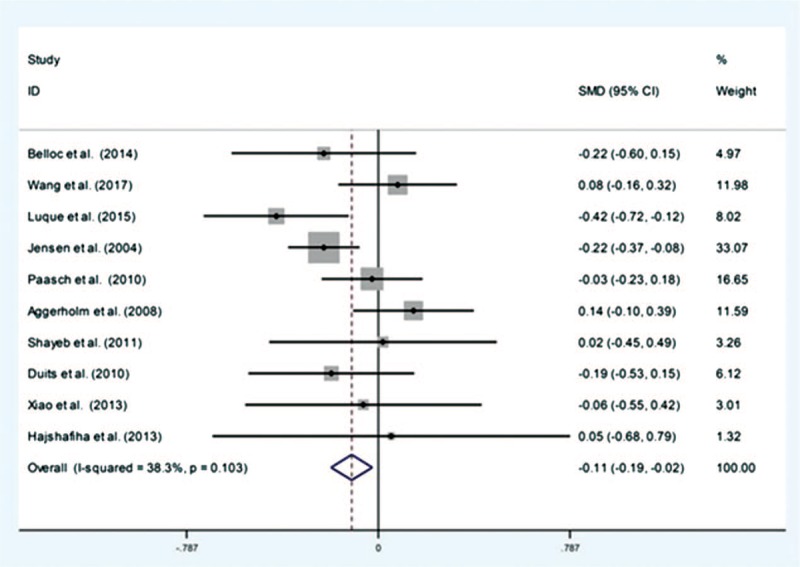
Forest plot of total sperm count of low body mass compared with normal body mass. Each point represents a separate study for the indicated association.
3.4. Sensitivity analyses
The sensitivity analyses were conducted to evaluate the effect of a special study on the whole outcome. The results showed that the SMD of total sperm count changed after removing data from Luque et al[16] or Jensen et al,[14] and the SMD of motility changed when excluding data from Wang et al[21] or Paasch et al,[15] while the results of others were not qualitatively altered with or without any article (Fig. 3).
Figure 3.
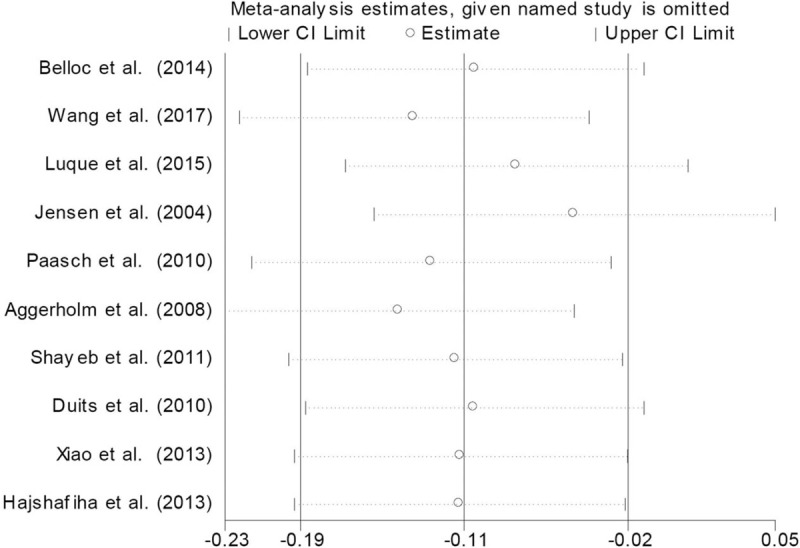
Sensitivity analysis about total sperm count.
3.5. Subgroup analyses
Given the effect of the ethnicity of population on the outcome, we conducted subgroup analyses. The results provided evidence that the total sperm count and semen volume were different in the Caucasian and Colored populations (Fig. 4).
Figure 4.
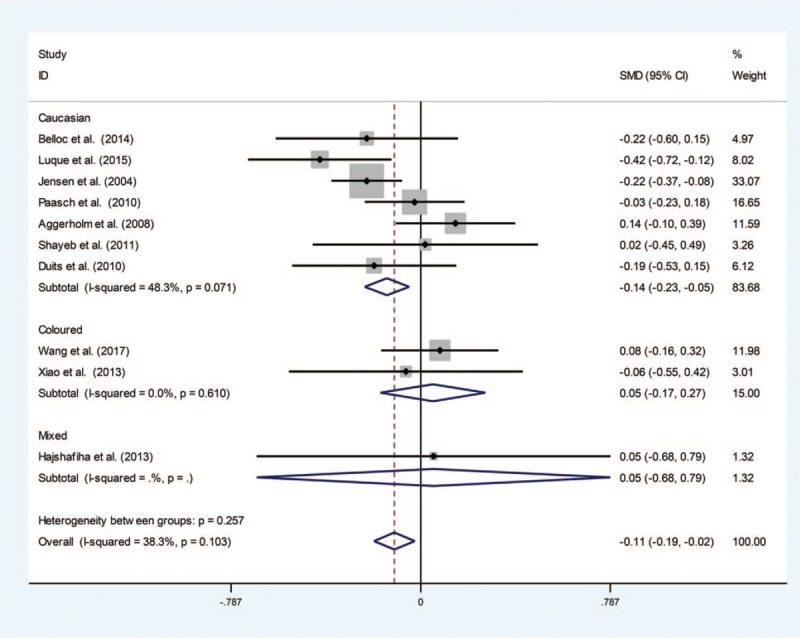
Subgroup analysis based on ethnicity about total sperm count.
3.6. Assessment of publication bias
We performed the Egger test and Begg funnel plot to assess the publication bias, and the results showed no evidence in each semen parameter (Fig. 5).
Figure 5.
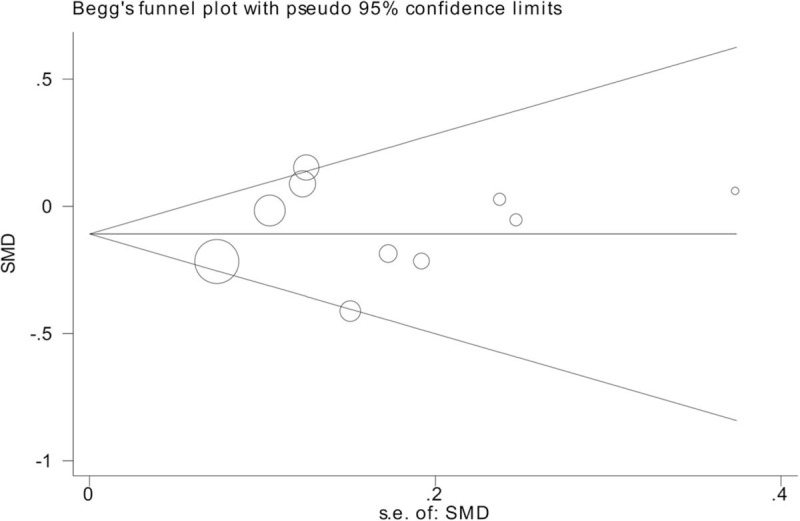
Funnel plot of observational studies about total sperm count.
4. Discussion
As a worldwide health problem, infertility has drawn widespread attention in recent decades. Many studies have investigated the effect of low BMI on female reproductive capacity. Veleva et al[22] established a positive relationship between low BMI and miscarriage. Cai et al[12] found low BMI compromised live birth rate in fresh transfer in vitro fertilization cycles. These results indicate that low BMI is a risk factor for female fertility. However, there is no relevant report about the effect of low BMI on male reproductive capacity. This meta-analysis showed that low BMI decreased semen parameters such as total sperm count, semen volume rather than sperm concentration and motility (overall or progressive motility), suggesting that low BMI is a risk for semen quality.
The result of this meta-analysis is consistent with several studies that recruited more than 1000 participants,[14,15] although they showed impact of low BMI on different semen parameter. While 2 meta-analysis[13,23] about the influence of BMI on total sperm count or sperm concentration showed no relationship between them published in 2010 and 2013, respectively. MacDonald et al[23] found no relationship between BMI and total sperm count or sperm concentration, and Sermondade et al[13] found that sperm concentration showed no difference across different BMI categories. But researchers of the latter[13] found a J-shaped association between BMI categories and risk of abnormal sperm count, which suggests that low BMI may be a risk factor for semen quality. Differences in literatures included, sample size, method of statistical analysis may lead to the different result of our study and meta-analysis published before. And we guess sample size is the dominant one, since we updated new studies published in recent years. However, as the number of participant in low BMI group in included studies are relatively small, more relevant researches with a large sample size are needed to reveal the correlation between low BMI and semen parameters.
There are several mechanistic studies on the effects of obesity on semen quality yet. In general, it can be summarized as the following points:
- (1)
-
(2)
Destruction of Sertoli and Leydig cells[27];
-
(3)
Insulin resistance and hyperinsu linemia[28];
-
(4)
Impairment of DNA integrity with increased level of oxidative stress[29];
-
(5)
Erectile dysfunction and sexuality in a reverse fashion in obese men.[30]
However, few studies evaluated the mechanism low body weight on male reproductive capacity Limited by the number of related studies, the corresponding mechanism remains unclear. Analogous to obese men, some researchers[14] speculated that hormonal imbalance may be involved in reduced semen quality in men with low BMI. Additionally, men with low BMI may have unhealthy lifestyles, as well as slight malnutrition or subclinical adverse conditions, which could affect their reproductive health.[6] However, there is still lack of sufficient evidence, and more deeper studies are needed to show the precise mechanism.
Given that obesity is a potentially harmful factor in male infertility, many researchers have begun to study the effect of weight loss on semen quality through exercise interventions, dietary, or bariatric surgery.[31–33] Some researchers suggest that weight loss should be implemented in obese men for seeking fertility treatment,[34,35] In particular, bariatric surgery may gradually become a way for infertile men induced by obesity to improve their fertility in the circumstance that relevant studies have been springing out recent decades.[36,37] Our results have confirmed that low BMI is a pernicious factor for male fertility, which forced us to ponder the question that whether excessive weight loss affects semen quality in the opposite direction, and whether weight loss treatment should be formulated a degree of restriction, especially about bariatric surgery. We expect more in-depth researches to answer these questions.
Because the original data could not be obtained from the corresponding authors, all information used in this meta-analysis was depended on published literatures only, which inescapably affected the authenticity and reliability of our results. We used SMD as the effect parameter, and converted data format through the acceptable formula to minimize effect as far as possible. Another problem is the inconsistent boundaries used to classify BMI in the included studies which could also influence the result, and we could not converted them into the standard criteria defined by WHO. Fortunately, the boundaries were only 4 types and were generally same that also explained the problem to a certain extent. Besides, taking the data processing into account, we kicked out some relevant articles that might provide useful information. And, the trial sequence analysis suggested that the number of participants included in our meta-analysis was small. Our study could serve as a reminder that calls for more attention to the content of this area.
According to this meta-analysis, men with low BMI have decreased parameters of semen, suggesting that underweight might be a risk factor of male infertility. We look forward to springing out large sample researches to identify the role of low BMI in male sterility.
Acknowledgment
The authors thank Na Qin for her support and guidance throughout the study.
Author contributions
Conceptualization: Dan Guo, Jiazhen Dai.
Data curation: Dan Guo, Min Xu, Rong Ju.
Formal analysis: Dan Guo, Qifan Zhou, Chunhua Wu.
Methodology: Min Xu, Qifan Zhou, Chunhua Wu, Rong Ju.
Supervision: Jiazhen Dai.
Writing – original draft: Min Xu, Rong Ju.
Writing – review and editing: Dan Guo, Jiazhen Dai.
Footnotes
Abbreviations: BMI = body mass index, SMD = standardized weighted mean differences, WHO = World Health Organization.
DG and MX contributed equally to the study and they should be regarded as joint first authors.
The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
The authors have no conflicts of interest to disclose.
References
- [1].Hafekost K, Lawrence D, Mitrou F, et al. Tackling overweight and obesity: does the public health message match the science? BMC Med 2013;11:41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Xu X, Zhou L, Miao R, et al. Association of cancer mortality with postdiagnosis overweight and obesity using body mass index. Oncotarget 2016;7:5023–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Sugai T, Suzuki Y, Yamazaki M, et al. High prevalence of underweight and undernutrition in Japanese inpatients with schizophrenia: a nationwide survey. BMJ Open 2015;5:e008720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Spano M, Toft G, Hagmar L, et al. Exposure to PCB and p, p’-DDE in European and Inuit populations: impact on human sperm chromatin integrity. Hum Reprod 2005;20:3488–99. [DOI] [PubMed] [Google Scholar]
- [5].Elzanaty S, Rignell-Hydbom A, Jonsson BA, et al. Association between exposure to persistent organohalogen pollutants and epididymal and accessory sex gland function: multicentre study in Inuit and European populations. Reprod Toxicol 2006;22:765–73. [DOI] [PubMed] [Google Scholar]
- [6].Sharpe RM. Environmental/lifestyle effects on spermatogenesis. Philos Trans R Soc Lond B Biol Sci 2010;365:1697–712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Fejes I, Koloszar S, Zavaczki Z, et al. Effect of body weight on testosterone/estradiol ratio in oligozoospermic patients. Arch Androl 2006;52:97–102. [DOI] [PubMed] [Google Scholar]
- [8].Sallmen M, Sandler DP, Hoppin JA, et al. Reduced fertility among overweight and obese men. Epidemiology 2006;17:520–3. [DOI] [PubMed] [Google Scholar]
- [9].Belloc S, Cohen-Bacrie M, Amar E, et al. High body mass index has a deleterious effect on semen parameters except morphology: results from a large cohort study. Fertil Steril 2014;102:1268–73. [DOI] [PubMed] [Google Scholar]
- [10].Flegal KM, Graubard BI, Williamson DF, et al. Reverse causation and illness-related weight loss in observational studies of body weight and mortality. Am J Epidemiol 2011;173:1–9. [DOI] [PubMed] [Google Scholar]
- [11].Wirth R, Streicher M, Smoliner C, et al. The impact of weight loss and low BMI on mortality of nursing home residents - results from the nutritionDay in nursing homes. Clin Nutr 2016;35:900–6. [DOI] [PubMed] [Google Scholar]
- [12].Cai J, Liu L, Zhang J, et al. Low body mass index compromises live birth rate in fresh transfer in vitro fertilization cycles: a retrospective study in a Chinese population. Fertil Steril 2017;107:422–9.e2. [DOI] [PubMed] [Google Scholar]
- [13].Sermondade N, Faure C, Fezeu L, et al. BMI in relation to sperm count: an updated systematic review and collaborative meta-analysis. Hum Reprod Update 2013;19:221–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Jensen TK, Andersson AM, Jorgensen N, et al. Body mass index in relation to semen quality and reproductive hormones among 1,558 Danish men. Fertil Steril 2004;82:863–70. [DOI] [PubMed] [Google Scholar]
- [15].Paasch U, Grunewald S, Kratzsch J, et al. Obesity and age affect male fertility potential. Fertil Steril 2010;94:2898–901. [DOI] [PubMed] [Google Scholar]
- [16].Luque EM, Tissera A, Gaggino MP, et al. Body mass index and human sperm quality: neither one extreme nor the other. Reprod Fertil Dev 2017;29:731–9. [DOI] [PubMed] [Google Scholar]
- [17].Qiu Fenglong, Ni Rong, Zhong Jixiang, et al. Relationship of different influencing factors and sperm quality parameters in infertile men. Chinese Journal of Human Sexuality. 2017; 26:112-5. [Google Scholar]
- [18].Duits FH, van Wely M, van der Veen F, et al. Healthy overweight male partners of subfertile couples should not worry about their semen quality. Fertil Steril 2010;94:1356–9. [DOI] [PubMed] [Google Scholar]
- [19].Shayeb AG, Harrild K, Mathers E, et al. An exploration of the association between male body mass index and semen quality. Reprod Biomed Online 2011;23:717–23. [DOI] [PubMed] [Google Scholar]
- [20].Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med 2002;21:1539–58. [DOI] [PubMed] [Google Scholar]
- [21].Wang EY, Huang Y, Du QY, et al. Body mass index effects sperm quality: a retrospective study in Northern China. Asian J Andrology 2017;19:234–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Veleva Z, Tiitinen A, Vilska S, et al. High and low BMI increase the risk of miscarriage after IVF/ICSI and FET. Hum Reprod 2008;23:878–84. [DOI] [PubMed] [Google Scholar]
- [23].MacDonald AA, Herbison GP, Showell M, et al. The impact of body mass index on semen parameters and reproductive hormones in human males: a systematic review with meta-analysis. Hum Reprod Update 2010;16:293–311. [DOI] [PubMed] [Google Scholar]
- [24].Davidson LM, Millar K, Jones C, et al. Deleterious effects of obesity upon the hormonal and molecular mechanisms controlling spermatogenesis and male fertility. Hum Fertil (Camb) 2015;18:184–93. [DOI] [PubMed] [Google Scholar]
- [25].Hammoud AO, Carrell DT, Gibson M, et al. Updates on the relation of weight excess and reproductive function in men: sleep apnea as a new area of interest. Asian J Androl 2012;14:77–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Katib A. Mechanisms linking obesity to male infertility. Cent European J Urol 2015;68:79–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Globerman H, Shen-Orr Z, Karnieli E, et al. Inhibin B in men with severe obesity and after weight reduction following gastroplasty. Endocr Res 2005;31:17–26. [DOI] [PubMed] [Google Scholar]
- [28].Bhasin S, Cunningham GR, Hayes FJ, et al. Testosterone therapy in men with androgen deficiency syndromes: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab 2010;95:2536–59. [DOI] [PubMed] [Google Scholar]
- [29].Zorn B, Vidmar G, Meden-Vrtovec H. Seminal reactive oxygen species as predictors of fertilization, embryo quality and pregnancy rates after conventional in vitro fertilization and intracytoplasmic sperm injection. Int J Androl 2003;26:279–85. [DOI] [PubMed] [Google Scholar]
- [30].Esposito K, Giugliano F, Di Palo C, et al. Effect of lifestyle changes on erectile dysfunction in obese men: a randomized controlled trial. JAMA 2004;291:2978–84. [DOI] [PubMed] [Google Scholar]
- [31].Niskanen L, Laaksonen DE, Punnonen K, et al. Changes in sex hormone-binding globulin and testosterone during weight loss and weight maintenance in abdominally obese men with the metabolic syndrome. Diabetes Obes Metab 2004;6:208–15. [DOI] [PubMed] [Google Scholar]
- [32].Kaukua J, Pekkarinen T, Sane T, et al. Sex hormones and sexual function in obese men losing weight. Obes Res 2003;11:689–94. [DOI] [PubMed] [Google Scholar]
- [33].Hakonsen LB, Thulstrup AM, Aggerholm AS, et al. Does weight loss improve semen quality and reproductive hormones? Results from a cohort of severely obese men. Reprod Health 2011;8:24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Du Plessis SS, Cabler S, McAlister DA, et al. The effect of obesity on sperm disorders and male infertility. Nat Rev Urol 2010;7:153–61. [DOI] [PubMed] [Google Scholar]
- [35].Abiad F, Awwad J, Abbas HA, et al. Management of weight loss in obesity-associated male infertility: a spotlight on bariatric surgery. Hum Fertil (Camb) 2017;20:227–35. [DOI] [PubMed] [Google Scholar]
- [36].Samavat J, Cantini G, Lotti F, et al. Massive weight loss obtained by bariatric surgery affects semen quality in morbid male obesity: a preliminary prospective double-armed study. Obes Surg 2018;28:69–76. [DOI] [PubMed] [Google Scholar]
- [37].El Bardisi H, Majzoub A, Arafa M, et al. Effect of bariatric surgery on semen parameters and sex hormone concentrations: a prospective study. Reprod Biomed Online 2016;33:606–11. [DOI] [PubMed] [Google Scholar]


