Supplemental Digital Content is available in the text
Keywords: healthcare utilization, inpatient, marriage, medicare, outpatient, skilled nursing facility
Abstract
To explain prior literature showing that married Medicare beneficiaries achieve better health outcomes at half the per person cost of single beneficiaries, we examined different patterns of healthcare utilization as a potential driver.
Using the Medicare Current Beneficiary Survey (MCBS) data, we sought to understand utilization patterns in married versus currently-not-married Medicare beneficiaries. We analyzed the relationship between marital status and healthcare utilization (classified based on setting of care utilization into outpatient, inpatient, and skilled nursing facility (SNF) use) using logistic regression modeling. We specified models to control for possible confounders based on the Andersen model of healthcare utilization.
Based on 13,942 respondents in the MCBS dataset, 12,929 had complete data, thus forming the analytic sample, of whom 6473 (50.3%) were married. Of these, 58% (vs. 36% of those currently-not-married) were male, 45% (vs. 47%) were age >75, 24% (vs. 70%) had a household income below $25,000, 18% (vs. 14%) had excellent self-reported general health, and 56% (vs. 36%) had private insurance. Compared to unmarried respondents, married respondents had a trend toward higher odds of having a recent outpatient visit (unadjusted odds ratio (OR) 1.11, 95% confidence interval (CI) 1.04–1.19, adjusted odds ratio (AOR) 1.10, (CI) 0.99–1.22), and lower odds in the year prior to have had an inpatient stay (AOR 0.84, CI 0.72–0.99) or a SNF stay (AOR 0.55, CI 0.40–0.75).
Based on MCBS data, odds of self-reported inpatient and SNF use were lower among married respondents, while unadjusted odds of outpatient use were higher, compared to currently-not-married beneficiaries.
1. Introduction
There are reasons to suspect that healthcare utilization patterns may differ according to marital status. First, healthcare costs among married Medicare beneficiaries are approximately half of those not married;[1] this difference in costs is observed among the nonelderly (age < 65) as well, but for the elderly, the difference is significantly greater.[2] Second, socio-demographic factors have been demonstrated to be important determinants of healthcare utilization.[3–5] Third, unmarried individuals have reduced access to resources that may affect utilization (e.g. health insurance and disposable income) than those who are married and may engage in riskier health-related behaviors,[6,7] possibly impacting utilization. Fourth, previous research suggests that being married is predictive of better health status,[8–10] perhaps attributable to more effective patterns of utilization. This study analyses health care utilization patterns based on marital status and aims to explore the importance of and mechanisms by which marital status may influence healthcare utilization, costs, and outcomes.
A substantial literature supports a positive effect of marriage on health. Married individuals, especially men, have a longer life expectancy than the unmarried,[10,11] better mental health,[12] and report greater satisfaction with overall quality of life.[13] The observed relationship between marriage and health was initially thought to be due to “marriage selection” (i.e., married individuals may be self-selected based on health-related characteristics, attitudes toward health, or behavioral factors).[14] However, there is a growing literature regarding the concept of “marriage protection.” This concept implies a protective role of a strong social relationship that may result in better health because spouses (especially women) function as care takers, providing physical and emotional support.[15–17] The idea that social circumstances impact the production of health is also supported by the Grossman model of health capital.[18] According to the Grossman model, individuals are not only mere consumers but also producers of healthcare, and that such production of healthcare is impacted by investments an individual makes to improve their health, one of which is leveraging personal social capital, such as marital status.[19]
However, because the literature does not corroborate the same extent of health benefits among unmarried cohabiting couples, marriage may influence health status in ways other than the “support function” of cohabitation.[6,13] Cohabiting couples are less likely to share resources (e.g. health insurance benefits or finances) than married ones. In an analysis of young married women (age 24–34), the positive health effects of marriage were found only among the unemployed, suggesting that the relationship between marriage and healthcare utilization may be modified by additional social circumstances.[20] In addition, risk-adjusted healthcare expenditures are lower among married couples despite better health outcomes (defined as the extent of change in or preservation of health status following an intervention). These findings raise the possibility that marital status may influence health outcomes through efficient (improved outcomes for a given cost or reduced costs without a decrement in health outcomes) utilization of health-related resources. The aforementioned disparate assertions and conclusions lead to two questions: First, do married couples differ in their patterns of healthcare utilization, and second, if such a difference truly exists, is it responsible for the previously observed differences in costs and health outcomes? In this analysis, we focus on answering the former question.
To our knowledge, the published literature does not include a rigorous analysis of the association between marital status and patterns of utilization across settings of healthcare provision. Most research on healthcare utilization is focused on specific disease conditions, a single setting of care, or among patients with a particular insurance status, much of which is not grounded in a robust theoretical framework.[21–25] Some studies have focused on costs instead of service utilization as the primary outcome measure.[1]
Understanding any difference in healthcare utilization associated with marital status is important, particularly as population demographics shift toward unmarried status and family structures change.[26–28] If there are indeed significant differences in patterns of healthcare utilization according to marital status, this insight may prove useful in the future to improve health outcomes and maximize the efficiency of healthcare provision. In conducting this study, we hypothesized that married Medicare beneficiaries would exhibit a more efficient pattern of healthcare utilization across settings of care.
2. Methods
2.1. Conceptual framework
We used the widely recognized Andersen model of healthcare utilization as the conceptual model to explore the relationship between marital status and healthcare utilization. The Andersen model is conceptually relevant for analyzing this relationship because characterizations of social structure are a central component of this model and therefore germane to our research question.[29] The model implies that healthcare utilization is determined by predisposing factors, enabling factors such as community resources, and need or demand-related factors.[3]
The original Andersen model was proposed in 1968 to study healthcare utilization by families, and its later modifications have been widely accepted and used as a conceptual model to understand individual healthcare utilization.[29–31] Based on this conceptual model, we extracted variables from our dataset potentially important in confounding the relationship between marital status and healthcare utilization to minimize any inaccuracy of the effect estimate. The potential confounding factors for which we controlled include demographic information (age, race, sex, education, and income), health status (self-rated general health, difficulty walking, and measures of functional limitations), insurance status (additional private insurance or dual Medicare and Medicaid coverage), and tendency to use healthcare, which we ascertained using receipt of an influenza vaccination as a proxy measure.[32]
2.2. Data and variables
We used the Medicare Current Beneficiary Survey (MCBS), a longitudinal in-person quarterly survey that follows a nationally representative sample of Medicare beneficiaries for a period of 3 years.[33,34] The MCBS is a complex random social survey designed to represent all current Medicare enrollees in the United States and Puerto Rico. We used the 2013 MCBS Access To Care Public Use File, a limited de-identified dataset of 13,924 survey participants that includes 459 variables obtained from the MCBS Round 67 as well as data from administrative sources.[35]
Our outcomes of interest were outpatient department (OPD) visits, inpatient hospitalization and skilled nursing facility (SNF) use. OPD use was measured over the recent past and was obtained through survey respondent report. The survey questionnaire ascertains information based on each respondent's most proximate OPD visitation prior to the current survey administration. Because the survey was conducted every 4 months, the OPD variable is likely to reflect OPD use in the few months prior to the interview. Inpatient and SNF use were derived from the administrative data linkage, measuring utilization over a 1-year period prior to the interview. Given the left-skewed distribution of the outcome variables, we dichotomized all three into zero or more than zero visits/admissions.
In our analysis, we coded marital status as a dichotomous variable between married and currently-not-married, the latter being an aggregate category including respondents who were widowed, divorced or never married. Our decision to specify this aggregate category was based on prior literature suggesting similar health risks (e.g., mortality rates) across types of currently unmarried individuals.[7,36]
The dataset included age brackets (<65, 65–75, >75) as categorical variables, which we used as such in the analysis. We categorized sex, race, and household size. We used self-rated health status as a representative predisposing factor. Additionally, we included difficulty walking and a variable representing degree of functional limitation (measured by the number of Activities of Daily Living (ADL) and Instrumental ADL limitations) as potential confounding variables, all of which we categorized. We measured access to care based on the presence of a dual Medicare and Medicaid insurance benefit or private insurance. We used influenza vaccination in the year prior to the survey as a proxy measure of health-related behavior and tendency to use healthcare. For all categorical variables, we used the first category as the reference category.
2.3. Analytic approach
We created multivariate logistic regression models based on the 2013 MCBS Public Use File cross-sectional data to estimate the relationship between marital status and each of the three outcome variables (OPD, inpatient, and SNF use). Given the skewed (toward zero) distribution of the outcome variables, we used logistic regression models rather than negative binomial or Poisson models for statistical efficiency and interpretability advantages. We controlled for potential confounding factors as was detailed above. For each outcome variable, the first model estimated the unadjusted relationship between marital status and that measure of utilization. The final multivariate-adjusted model included variables representing demographic factors, predisposing factors, insurance status, health behavior, and tendency to utilize healthcare. Model specification was based on the Andersen model in addition to the aforementioned statistical considerations.
We also tested additional models for each of the three outcome variables by including several additional variables measuring factors of potential importance like household structure (a categorical variable denoting household composition), and a limited set of self-reported comorbid conditions. The P-values were derived using Pearson's Chi-squared test on contingency tables of each variable versus dichotomized marital status. Statistical analyses were performed using R v. 3.3.2 (in addition to the base package, we used tidyverse, plyr, lmtest, sjPlot, stargazer). We did not seek Institutional Review Board approval in conducting this study because we used a publicly available de-identified dataset created based on the MCBS.
2.4. Subgroup analysis
In order to explore the association of nonspousal cohabitation (e.g., with siblings or children) and healthcare utilization, we further analyzed the currently-not-married subgroup. Within this subgroup, we compared utilization among those who were living alone to those who were living with other non-spousal household members. We created logistic regression models specifying household size (dichotomous variable with 1 or more than 1 members as categories) as the main predictor variables, the outcome variables remaining as previously described. We controlled for potential confounding factors identical to the way described above.
3. Results
Of our initial study sample of 13,924 respondents, 995 were excluded because of missing data, creating the final analytic sample of 12,929 observations. Table 1 exhibits the distribution of healthcare utilization across the three settings of care previously described, as well as the distribution of respondents’ marital status.
Table 1.
Frequency distribution of the study sample, according to marital status and measures of utilization across settings of care.
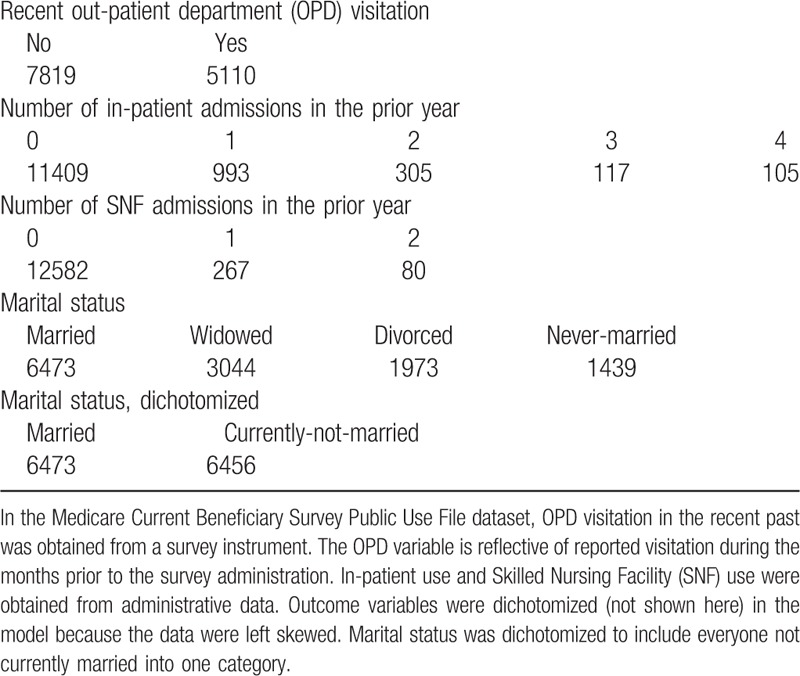
Table 2 demonstrates that, of the 12,929 respondents in the analytic sample, 6473 (50.3%) were currently married, the remaining 6456 (49.7%) having been currently-not-married at the time of survey administration. Married beneficiaries were more likely to be male, older, white and have higher income and education compared to those currently-not-married. They also had better self-rated health status, fewer functional limitations, and were more likely to have private insurance. Those currently-not-married tended to have lower income, belong to racial minorities, have worse self-reported health status, and were more likely to have dual Medicare and Medicaid coverage.
Table 2.
Medicare Current Beneficiary Survey (MCBS) 2013 respondent characteristics.
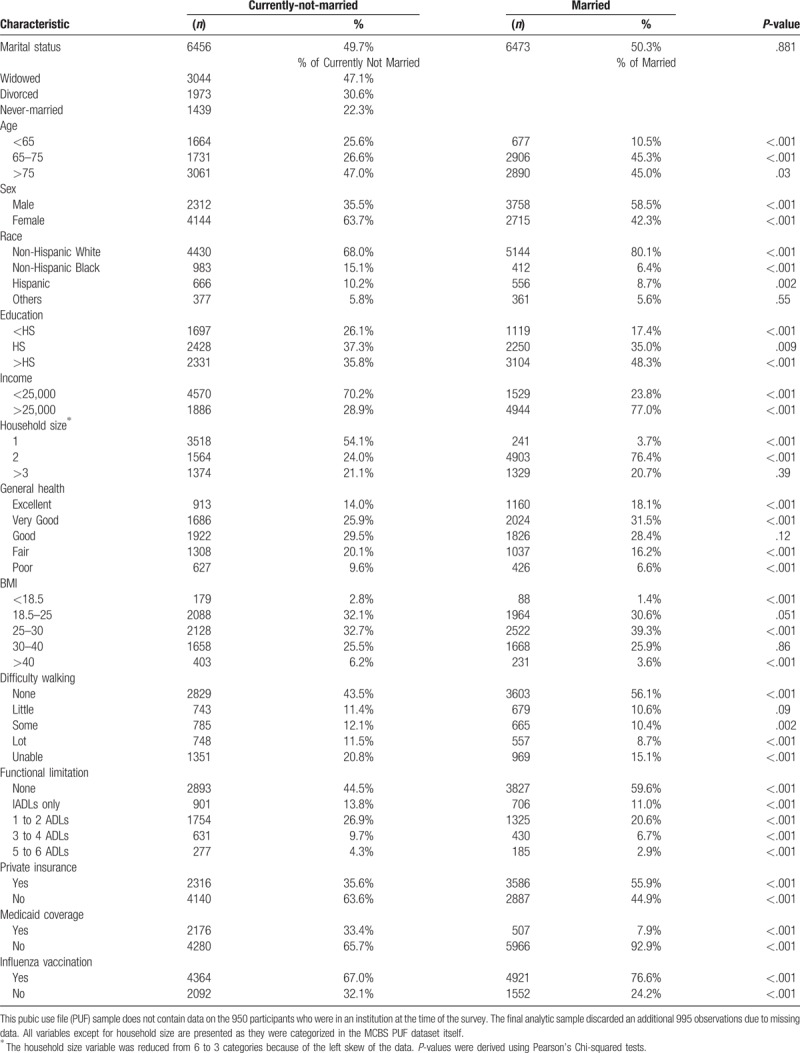
Table 3 demonstrates the adjusted odds ratios (AORs) measuring the association between marital status and each prespecified measure of utilization. We subdivide the following according to each measure of utilization.
Table 3.
Healthcare use in Medicare Beneficiaries - Logistic Regression Models.
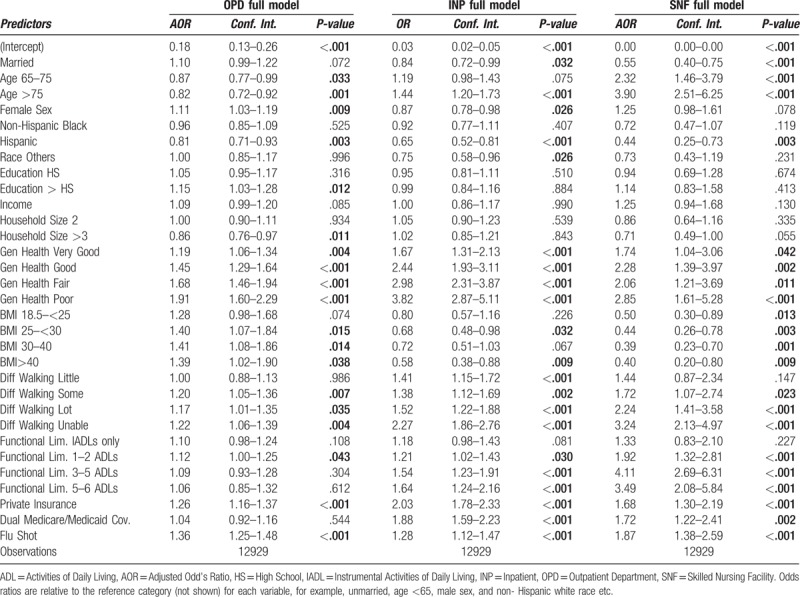
3.1. Outpatient utilization
Currently married respondents had higher unadjusted odds of having an outpatient visit in the recent past, although this relationship failed to maintain statistical significance in the adjusted model (unadjusted OR 1.11, 95% confidence interval CI 1.04–1.19, AOR 1.10, CI 0.99–1.22). In the OPD model, age >75 predicted reduced use of OPD (OR 0.82, [CI 0.72–0.92]. Similarly, Hispanics were less likely to have had an OPD visit compared to whites (AOR 0.71, CI 0.81–0.93). Each decrement in self-rated health status was associated with an increasingly greater likelihood of having had an OPD visit (e.g. poor health status, AOR 1.91, CI 1.60–2.29). Receipt of influenza vaccination and having supplemental private insurance were also associated with having had an outpatient visit in the recent past.
3.2. Inpatient utilization
Married respondents were less likely to have an inpatient stay in the year prior to the interview (unadjusted OR 0.77, CI 0.69–0.86, AOR 0.84, [CI 0.72–0.99]). Older age, male sex, difficulty walking, poor self-rated health, supplemental private insurance (AOR 2.03, CI 1.78–2.33), dual Medicare/Medicaid coverage (AOR 1.88, CI 1.59–2.23), were associated with a greater odds of hospitalization.
3.3. SNF utilization
Married status was associated with a markedly reduced odds of SNF use (unadjusted OR 0.46, CI 0.36–0.58, AOR 0.55, CI 0.40–0.75). Larger household size was associated with a trend suggesting a 29% reduction in SNF use, albeit not quite to statistical significance. Increasing age, low self-rated health status, and difficulty walking predicted a greater a greater use of SNF, as did the receipt of an influenza vaccination (OR 1.87, CI 1.38–2.59), private insurance (OR 1.68, CI 1.30–2.19), and dual Medicare/Medicaid coverage (OR 1.72, CI 1.22–2.41).
We performed additional analyses through inclusion of variables codifying comorbidities and household structure (to denote the nature of relationships in multi-member households). However, none of these characteristics were significant predictors of utilization and did not modify the relationship between marital status and the utilization measures (not reported).
3.4. Additional and subgroup analyses
In order to understand the relative effect of spousal cohabitation versus non-spousal cohabitation on utilization, we performed a subgroup analysis among respondents currently-not-married. In this analysis, we used a dichotomized household size variable as the primary predictor and the same outcome measures, controlling for the same set of potential confounders used in the main analysis. We did not find a consistent association between household size and utilization among respondents who were currently not married (Appendix 1).
4. Discussion
This analysis was aimed at elucidating the relationship between marital status and patterns of healthcare utilization among a sample of Medicare beneficiaries. Marital status was predictive of reduced use of inpatient and SNF services, with a trend toward greater use of outpatient services.
There are several important insights from our study that may have implications from clinical and policy perspectives. Reduced utilization of more costly inpatient and SNF care, with greater utilization of outpatient services, supports the assertion that the social components of marriage may result in a more efficient allocation of healthcare resources. Prior literature has identified a trend toward substitution of inpatient utilization with additional care received in the outpatient setting.[37,38] Outpatient visits enhance continuity of care, which has been associated with reduced hospitalization rates.[39,40] In particular, increased use of outpatient services reduces hospitalization rates among patients with Ambulatory Care Sensitive Conditions.[41–43] In fact, as many as 9%–22% of hospital admissions are thought to be avoidable with adequate provision of outpatient care.[44] Therefore, a greater reliance on readily available outpatient care may be one mechanism by which married people achieve better health outcomes. Additionally, outpatient visits are also much less costly than inpatient and SNF stays,[2,45] creating opportunities for efficient provision of care while preserving the continuity that is the cornerstone of longitudinal physician-patient relationships. The tendency to substitute costly inpatient and SNF services with less expensive outpatient services is likely an important reason why married Medicare beneficiaries have significantly lower healthcare costs than those currently-not-married. In addition to our primary findings regarding the relationship between marital status and healthcare utilization across multiple settings of care, our analysis reveals that older Medicare beneficiaries have lower outpatient utilization, but higher inpatient and SNF utilization. As expected, those with worse self-rated health status, a greater number of functional limitations, and additional insurance benefits have greater utilization across all domains of care. These findings are consistent with prior analyses.[46–48]
Our findings support the assertion that marital status is an important predictor of healthcare utilization. Although the observational nature of the data source limits our ability to draw true causal inferences, this analysis does exhibit a strong association, robust to multivariate modeling, between marital status and healthcare utilization in the three domains analyzed. This ‘‘spousal effect” is also corroborated by our finding that unmarried cohabitating individuals do not have the same pattern of reduced inpatient and SNF utilization with a trend toward greater outpatient utilization. These findings raise the possibility that marriage may influence health status not only through the support and protection that marriage offers, but also through a more efficient pattern of healthcare utilization.
In order to translate these findings into relevant policy, it is important to understand the causal mechanisms for this ‘‘spousal effect” in healthcare utilization. Our study does not allow us to unambiguously delineate these mechanisms. However, several mechanisms could explain the observed associations. First, spouses may function as in-home caretakers, thereby obviating the need for formal healthcare.[17] For example, spouses may assist with medication adherence, preparing and encouraging the consumption of healthy meals, or ensuring attendance at physician appointments.[49] Second, there may be psychological and physical health effects of spousal cohabitation, and that may consequently influence the volume and distribution of healthcare utilization.[5,15] Third, marriage has also been noted to create what has been referred to as “spare capacity” – the ability to dedicate one's time, effort, and available healthcare resources to improve health as a result of division of labor and shared responsibilities within the home.[50] Similarly, marriage also facilitates engagement in resource sharing and mutual investment. Fourth, there may be a self selection into marriage, often referred to as “marriage selection,” resulting from unobserved characteristics that influence both healthcare utilization and health.[14,51] We have tried to control for this potential selection as rigorously as our data would allow through regression controls. Consequently, we believe that our estimation reflects the effect of marriage mediated predominantly by the first three mechanisms.
We believe the trend toward greater OPD utilization observed among married respondents is mediated by a combination of factors: (a) greater access to resources, including higher total income and more private insurance enabling access to uninterrupted care; (b) greater health-enhancing home support and assistance improving compliance with outpatient appointments; (c) and higher levels of education contributing to intelligent and cost-effective decisions regarding the appropriate setting in which to pursue care. The validity of these assertions is supported by the fact that the relationship between marital status and OPD utilization is weakened when adjusted for these factors, suggesting that the observed relationship is in part mediated through these mechanisms.
Our study has important strengths. The MCBS is a nationally-representative survey administered to a large sample of Medicare beneficiaries across the United States. The depth of the dataset allowed us to adjust for a wide range of potential confounding factors. Our outcome measures also represent the broad domains of healthcare provision, conferring a more global perspective on the hypothesized findings. The models we constructed were based on a well-validated conceptual model, clinical considerations, and potential policy relevance. As we indicated above, for cases in which prior literature exists, our findings are consistent with those of other investigators using different data sources. Finally, our analysis produced robust estimates with potentially important implications. The positive association we observed between worse self-rated health status and receipt of an influenza vaccination (representative of propensity to seek medical attention) with utilization across all three settings of care supports the validity of the outcome measures we chose.
The major limitation of this study is that this is a cross-sectional analysis of secondary data that assessed an association but not a causal effect. Although we established a strong association between marital status and the utilization measures, it is possible that unobserved clinical characteristics or social differences that correlate with marriage actually mediate our findings. However, we believe that the depth of the data allowing us to perform a multivariate analysis among a nationally representative sample renders our findings valuable for plausible causal inference. Another limitation important to acknowledge is our inability to derive a relationship between marital status and health outcomes. We were also not able to delineate the diagnoses or clinical circumstances associated with inpatient and SNF use. If the reduced utilization among the married was for ambulatory care sensitive conditions, this would be of particular importance for health system structure and quality measurement. Incorporating such detailed clinical information would be an important direction for future research in this area. Although we have controlled for measures of perceived need for health care, we were not able to rigorously control for comorbid conditions using validated methods such as the Charlson or Elixhauser methods for risk adjustment.[52,53] However, as Andersen points out in the 1995 reassessment of his model, perceived needs (as may be reflected in self-rated health status) may be a better measure of care-seeking behavior compared to objective measures of health care need (e.g. comorbidity burden).[29] Since we did not have access to rigorous measures of respondents’ propensity to seek medical attention, we used the receipt of an influenza vaccination as a proxy measure. Despite its face validity as such, we cannot state with certainty the fidelity or robustness with which it ascertains an individual's tendency to pursue healthcare services.
Future research might examine whether increasing outpatient service consumption among unmarried individuals reduces their hospitalization rates and/or SNF use, and any quantifiable effect on their outcomes or the costs incurred. This would lend credence to the substitution effect described above. The ‘‘spousal effect” may be more than simply psychological, thus creating discernible patterns of behavior in which spouses engage in caregiving and healthcare system navigation, yielding measurable health benefits. Rigorous knowledge in this regard could facilitate the design of targeted healthcare interventions and home health services for unmarried people. Such interventions may realize benefits by simultaneously improving objective health outcomes and patient-centeredness, while reducing costs.
The impact of social circumstances on health care utilization patterns is not well understood, but we believe that our findings aid in elucidating the relationship between marital status and utilization of health care. This study provides important corroborative evidence to support such a relationship among Medicare beneficiaries. Therefore, we conclude that patterns of health care use may explain at least some of the variations in outcomes and costs observed across social groups. Longitudinal, prospectively specified studies might determine with greater confidence the extent to which a true causal effect underlies this relationship. Although we have explored the mechanisms that may underlie our findings, future investigations may be directed at more definitively elucidating the factors that mediate the observed relationships between marital status and utilization. A greater understanding of these factors may have important implications for clinical care, social policy, and improvements in health system design, which may hold the potential to optimize health and mitigate the economic challenges of healthcare provision.
Author contributions
Conceptualization: Kiran Raj Pandey, Gregory W. Ruhnke.
Data curation: Kiran Raj Pandey.
Formal analysis: Kiran Raj Pandey.
Methodology: Kiran Raj Pandey, Fan Yang, Kathleen A. Cagney, Fabrice Smieliauskas, David O. Meltzer, Gregory W. Ruhnke.
Software: Kiran Raj Pandey.
Supervision: Fan Yang, Kathleen A. Cagney, Fabrice Smieliauskas, David O. Meltzer, Gregory W. Ruhnke.
Writing – original draft: Kiran Raj Pandey.
Writing – review & editing: Kiran Raj Pandey, Fan Yang, Kathleen A. Cagney, Fabrice Smieliauskas, David O. Meltzer, Gregory W. Ruhnke.
Kiran Raj Pandey orcid: 0000-0002-8277-766X.
Supplementary Material
Footnotes
Abbreviations: ADL = activities of daily living, AOR = adjusted odds ratio, CI = confidence interval, IADL = instrumental activities of daily living, MCBS = Medicare Current Beneficiary Survey, OPD = out patient department, OR = odds ratio, SNF = skilled nursing facility.
None of the authors have any conflict of interest to declare.
Supplemental Digital Content is available for this article.
References
- [1].Banerjee S. Differences in Out-of-Pocket Health Care Expenses of Older Single and Couple Households. 2016. [Google Scholar]
- [2].Banerjee S. Utilization patterns and out-of-pocket expenses for different health care services among american retirees. EBRI Issue Brief 2015;411:1–20. [PubMed] [Google Scholar]
- [3].Andersen R, Newman JF. Societal and individual determinants of medical care utilization in the United States. Milbank Quarterly 2005;83: Online-only-Online-only. doi:10.1111/j.1468-0009.2005.00428.x. [PubMed] [Google Scholar]
- [4].Dunlop DD, Manheim LM, Song J, et al. Gender and ethnic/racial disparities in health care utilization among older adults. J Gerontol B Psychol Sci Soc Sci 2002;57:S221–33. [DOI] [PubMed] [Google Scholar]
- [5].de Boer AGE, Wijker W, de Haes HCJ. Predictors of health care utilization in the chronically ill: a review of the literature. Health Policy 1997;42:101–15. [DOI] [PubMed] [Google Scholar]
- [6].Waite LJ. Does marriage matter? Demography 1995;32:483–507. [PubMed] [Google Scholar]
- [7].Lillard LA, Waite LJ. Til death do us part: marital disruption and mortality. Am J Sociol 1995;100:1131–56. [Google Scholar]
- [8].Verbrugge LM. Marital status and health. J Marriage Fam 1979;41:267doi: 10.2307/351696. [Google Scholar]
- [9].Mendes de Leon CF, Appels AW, Otten FW, et al. Risk of mortality and coronary heart disease by marital status in middle-aged men in The Netherlands. Int J Epidemiol 1992;21:460–6. [DOI] [PubMed] [Google Scholar]
- [10].Coombs RH. Marital status and personal well-being: a literature review. Fam Relat 1991;40:97doi: 10.2307/585665. [Google Scholar]
- [11].Hu Y, Goldman N. Mortality differentials by marital status: an international comparison. Demography 1990;27:233–50. [PubMed] [Google Scholar]
- [12].Simon RW. Revisiting the relationships among gender, marital status, and mental health. Am J Sociol 2002;107:1065–96. [DOI] [PubMed] [Google Scholar]
- [13].Stack S, Eshleman JR. Marital status and happiness: a 17-Nation Study. J Marriage Fam 1998;60:527doi: 10.2307/353867. [Google Scholar]
- [14].Goldman N. Marriage selection and mortality patterns: inferences and fallacies. Demography 1993;30:189–208. [PubMed] [Google Scholar]
- [15].Cobb S. Social support as a moderator of life stress. Psychosom Med 1976;38:300–14. [DOI] [PubMed] [Google Scholar]
- [16].Espinosa J, Evans WN. Heightened mortality after the death of a spouse: marriage protection or marriage selection? J Health Econ 2008;27:1326–42. [DOI] [PubMed] [Google Scholar]
- [17].Arno PS, Levine C, Memmott MM. The economic value of informal caregiving. Health Aff (Millwood) 1999;18:182–8. [DOI] [PubMed] [Google Scholar]
- [18].Grossman M. On the concept of health capital and the demand for health. J Polit Econ 1972;80:223–55. [Google Scholar]
- [19].Grossman M. The Human Capital Model of the Demand for Health. Cambridge, MA: National Bureau of Economic Research; 1999. [Google Scholar]
- [20].Waldron I, Hughes ME, Brooks TL. Marriage protection and marriage selection--prospective evidence for reciprocal effects of marital status and health. Soc Sci Med 1996;43:113–23. [DOI] [PubMed] [Google Scholar]
- [21].Rizzo JA, Friedkin R, Williams CS, et al. Health care utilization and costs in a Medicare population by fall status. Med Care 1998;36:1174–88. [DOI] [PubMed] [Google Scholar]
- [22].Luber MP, Meyers BS, Williams-Russo PG, et al. Depression and service utilization in elderly primary care patients. Am J Geriatr Psychiatry 2001;9:169–76. [PubMed] [Google Scholar]
- [23].Henton FE, Hays BJ, Walker SN, et al. Determinants of Medicare home healthcare service use among Medicare recipients. Nurs Res 2002;51:355–62. [DOI] [PubMed] [Google Scholar]
- [24].Yang M, Barner JC. Use of the andersen health care services utilization behavioral model to understand the relationship between health insurance coverage and health care services utilization among the elderly. Value Health 2001;4:172doi: 10.1046/j.1524-4733.2001.40202-271.x. [Google Scholar]
- [25].Joung IM, van der Meer JB, Mackenbach JP. Marital status and health care utilization. Int J Epidemiol 1995;24:569–75. [DOI] [PubMed] [Google Scholar]
- [26].US Census Bureau. Historical Marital Status Tables. 2016. Available at: https://www.census.gov/data/tables/time-series/demo/families/marital.html [accessed date August 9, 2017]. [Google Scholar]
- [27].Pew Research Center. Record Share of Americans Have Never Married. Pew Research Center Social and Demographic Trends 2014. Available at: http://www.pewsocialtrends.org/2014/09/24/record-share-of-americans-have-never-married/ [accessed date May 8, 2017]. [Google Scholar]
- [28].US Census Bureau. The rise of living alone. 2016. Available at: https://www.census.gov/data/tables/time-series/demo/families/households.html [accessed date August 11, 2017]. [Google Scholar]
- [29].Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav 1995;36:1–0. [PubMed] [Google Scholar]
- [30].Andersen R, Newman JF. Societal and individual determinants of medical care utilization in the United States. Milbank Mem Fund Q Health Soc 1973;51:95–124. [PubMed] [Google Scholar]
- [31].Aday LA, Andersen R. A framework for the study of access to medical care. Health Serv Res 1974;9:208–20. [PMC free article] [PubMed] [Google Scholar]
- [32].Butz A, Hutton N, Joyner M, et al. HIV-infected women and infants: Social and health factors impeding utilization of health care. J Nurse Midwifery 1993;38:103–9. [DOI] [PubMed] [Google Scholar]
- [33].Adler GS. A profile of the Medicare Current Beneficiary Survey. Health Care Financ Rev 1994;15:153–63. [PMC free article] [PubMed] [Google Scholar]
- [34].Briesacher BA, Tjia J, Doubeni CA, et al. Methodological issues in using multiple years of the Medicare current beneficiary survey. Medicare Medicaid Res Rev 2012;2: doi: 10.5600/mmrr.002.01.a04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].CMS. Medicare Current Beneficiary Survey 2013 Access to Care, Public Use File User Guide. 2013. [Google Scholar]
- [36].Lund R, Holstein BE, Osler M. Marital history from age 15 to 40 years and subsequent 10-year mortality: a longitudinal study of Danish males born in 1953. Int J Epidemiol 2004;33:389–97. [DOI] [PubMed] [Google Scholar]
- [37].Goldsmith JC. The health care market: can hospitals survive? Harv Bus Rev 1980;58:100–12. [PubMed] [Google Scholar]
- [38].Stoeckle JD. The Citadel cannot hold: technologies go outside the hospital, patients and doctors too. Milbank Q 1995;73:3–17. [PubMed] [Google Scholar]
- [39].Gill JM, Mainous AG. The role of provider continuity in preventing hospitalizations. Arch Fam Med 1998;7:352–7. [DOI] [PubMed] [Google Scholar]
- [40].Mainous AG, Gill JM. The importance of continuity of care in the likelihood of future hospitalization: is site of care equivalent to a primary clinician? Am J Public Health 1998;88:1539–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Weissman JS. Rates of avoidable hospitalization by insurance status in massachusetts and maryland. JAMA 1992;268:2388doi: 10.1001/jama.1992.03490170060026. [PubMed] [Google Scholar]
- [42].Bindman AB, Grumbach K, Osmond D, et al. Preventable hospitalizations and access to health care. JAMA 1995;274:305–11. [PubMed] [Google Scholar]
- [43].Silver MP, Babitz ME, Magill MK. Ambulatory care sensitive hospitalization rates in the aged Medicare population in Utah, 1990∗ to 1994∗: a rural-urban comparison. J Rural Health 1997;13:285–94. [DOI] [PubMed] [Google Scholar]
- [44].Tian Y, Dixon A, Gao H. Emergency hospital admissions for ambulatory care-sensitive conditions: identifying the potential for reductions. The King's Fund Data Briefing 2014. [Google Scholar]
- [45].Galarraga JE, Mutter R, Pines JM. Costs associated with ambulatory care sensitive conditions across hospital-based settings. Acad Emerg Med 2015;22:172–81. [DOI] [PubMed] [Google Scholar]
- [46].Shah MN, Rathouz PJ, Chin MH. Emergency department utilization by noninstitutionalized elders. Acad Emerg Med 2001;8:267–73. [DOI] [PubMed] [Google Scholar]
- [47].Fried TR, Bradley EH, Williams CS, et al. Functional disability and health care expenditures for older persons. Arch Intern Med 2001;161:2602–7. [DOI] [PubMed] [Google Scholar]
- [48].Chin MH, Zhang JX, Merrell K. Diabetes in the African-American Medicare population. Morbidity, quality of care, and resource utilization. Diabetes Care 1998;21:1090–5. [DOI] [PubMed] [Google Scholar]
- [49].Simeonova E. Marriage, bereavement and mortality: the role of health care utilization. J Health Econ 2013;32:33–50. [DOI] [PubMed] [Google Scholar]
- [50].Castevens P. The impact of family structure on spare capacity and health care utilization. Health Watch 2014. 31–8. [Google Scholar]
- [51].Goldman N, Korenman S, Weinstein R. Marital status and health among the elderly. Soc Sci Med 1995;40:1717–30. [DOI] [PubMed] [Google Scholar]
- [52].Charlson M, Szatrowski TP, Peterson J, et al. Validation of a combined comorbidity index. J Clin Epidemiol 1994;47:1245–51. [DOI] [PubMed] [Google Scholar]
- [53].Elixhauser A, Steiner C, Harris DR, et al. Comorbidity measures for use with administrative data. Med Care 1998;36:8–27. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


