Abstract
Cases of foreign body ingestion are encountered relatively often in clinical settings; however, serious complications are rare. In such cases, mediastinal abscess due to esophageal perforation can become a life-threatening complication. Although highly invasive, surgery is often used as the first-line treatment. We herein report the case of a 65-year-old woman who presented with complaints of progressive odynophagia and dysphagia for 2 weeks following a fish meal. Enhanced cervicothoracic computed tomography demonstrated an enhanced round mass with peripheral contrasted margins. The mass was diagnosed as a mediastinal abscess resulting from esophageal perforation caused by a fish bone. Endoscopic ultrasound-guided abscess drainage (EUS-AD) was performed using a nasobiliary drainage tube (NDT). Two weeks later, the abscess had completely disappeared. EUS-AD was safe and effective in this case; furthermore, external drainage using NDT was suitable for this abscess located very close to the upper esophageal sphincter.
Keywords: mediastinal abscess, fish bone, endoscopic ultrasound-guided abscess drainage
Introduction
Ingestion of a foreign body is often encountered in daily practice. In many cases, foreign bodies are removed by endoscopy or pass spontaneously without complications (1). The most common foreign bodies are fish bones, which account for 37% of esophageal foreign bodies (2). The frequency of severe complications, such as an esophageal perforation or abscess due to an ingested fish bone, was reported to be 0.3% (3). A deep neck infection or abscess may spread to the pleural cavity or into a slit called the danger space (4) in the cervical fascia located in front of the vertebra.
In the absence of infection control, mediastinal abscess may become fatal (5,6). Surgery was previously used as the first-line treatment; however, several non-surgical treatments have recently been reported (7-11). Similar to previous articles, this report proposes a treatment method that is secure and less invasive than surgery.
Case Report
A 65-year-old woman without a significant medical history complained of progressive odynophagia and dysphagia. Two weeks before admission, she developed pharyngeal pain immediately after consuming fish. One week before admission, she developed a low-grade fever with pain, both of which gradually worsened.
On a physical examination, her vital signs were stable, but marked cervical tenderness was noted. Laboratory tests showed an elevated white blood cell count (10,100/μL) and C-reactive protein level (15.5 mg/dL). Laryngoscopy showed no significant findings. Axial contrast-enhanced computed tomography (CT) showed a round low-density lesion (22 mm×33 mm×60 mm) with rim enhancement at the back of the esophagus. The lesion was located in front of the thoracic vertebra (Fig. 1). We suspected the presence of a mediastinal abscess resulting from esophageal perforation caused by a fish bone, but no foreign body was detected. She was admitted on the day she visited the hospital, and we performed endoscopic drainage. Upper endoscopy showed a compressed esophageal lumen with a smooth mucosa (Fig. 2a). A convex echoendoscope (GF-UCT260; Olympus, Tokyo, Japan) and ultrasound processor (EU-ME2; Olympus) showed a mediastinal abscess as a clear marginal hypo- or mixed echoic collection with posterior enhancement (Fig. 2b). Transesophageal puncture of the mediastinal abscess was performed using a Sono TipⓇ 19 G (Mediglobe, Grassau, Germany) with a 0.025-inch guidewire (visiglide2™; Boston Scientific Japan, Tokyo, Japan) under a mobile C-arm fluoroscopic X-ray system (Clearscope SXT-9000A; Canon Medical Systems, Otawara, Japan) (Fig. 2c). After a small amount of contrast was injected into the abscess, a guidewire was introduced through the needle and coiled in it the abscess. A 4-mm biliary balloon catheter (ZARA; Kaneka Medix, Osaka, Japan) was then advanced through the esophageal wall over the guidewire in order to dilate the punctured route. A 6-Fr nasobiliary drainage tube (NDT; Flexima™ ENBD Catheter; Boston Scientific Japan) was deployed into the abscess and coiled in it. Dense and viscous pus was drained through the tube (Fig. 2d).
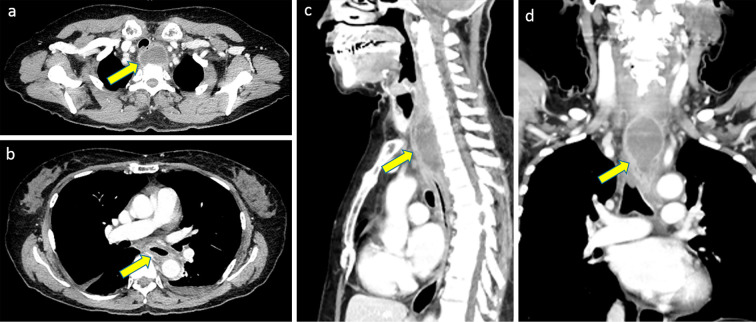
Figure 1.
Imaging findings. a: Axial image of contrast-enhanced computed tomography (CT) showing a round low-density lesion with rim enhancement on the back side of the esophagus. No foreign body was detected. The lesion was located in front of the thoracic vertebrae. b: The wall of the inferior esophagus was thick. c, d: Coronal and sagittal images of enhanced CT. The lesion was located in front of the thoracic vertebrae (C7-Th4). There were no significant findings in the thoracic vertebrae and no direct connection to the pleural cavity.
Figure 2.
The endoscopic examination and treatment. a: Upper endoscopy revealing that the esophageal lumen was severely compressed by the abscess. b: Convex endoscopic ultrasound images revealing an abscess with a clear marginal mixed echoic pattern with acoustic enhancement, implying floating abscess fluid. c: Mobile C-arm fluoroscopic X-ray system showing the nasogastric drainage tube advanced over the guidewire. d: High-viscosity pus aspirated from the abscess.
The patient's clinical course is shown in Fig. 3. Antibiotic therapy was started with ampicillin/sulbactam. Streptococcus intermedius was detected by a pus culture test, and antibiotic was de-escalated using ampicillin. According to the treatment period for deep neck infections, intravenous antibiotic therapy was continued for a total of three weeks.
Figure 3.
Patient’s clinical course after admission. Treatment details and transitive graphs of the WBC count and CRP level after admission. ABPC/SBT: ampicillin/sulbactam, ABPC: ampicillin, PPN: peripheral parenteral nutrition, OED: oral elemental diet, TPN: total parenteral nutrition, EUS-AD: endoscopic ultrasound-guided abscess drainage, NT: nasogastric tube, OI: oral intake, WBC: white blood cell, CRP: C-reactive protein
The abscess was irrigated with a saline solution through the tube with rotation of the patient's body direction. We confirmed the diminishing size of the abscess on fluoroscopic imaging and changed the tube location and shape accordingly (Fig. 4). Fifteen days after the procedure, the NDT was removed. We then deployed a nasogastric tube (NT) into the upper esophagus, with the side hole placed near the fistula, and applied intermittent suction (pressure, 10 cmH2O; aspiration for 10 seconds, stop aspiration for 20 seconds) to avoid salivary exposure and accelerate healing. After four days, we injected contrast through the NT under fluoroscopy. As there was no evidence of a residual fistula, the NT was removed. The patient started eating and was discharged after 26 days of hospitalization. She has since been asymptomatic without recurrence on contrast-enhanced CT.
Figure 4.
Imaging findings after the procedure. a, b: Contrast-enhanced computed tomography images (a, coronal; b, sagittal) seven days after admission. The size of the abscess decreased, but the pus persisted. A nasogastric drainage tube (NDT) was advanced through the esophageal wall at the upper esophageal sphincter (yellow arrow). c, d: Fluoroscopic guidance in the front and oblique directions. The NDT was coiled in the abscess (c, frontal presentation; d, oblique presentation). e, f: Contrast revealing shrinkage of the abscess. After shrinkage was confirmed, the NDT loop was decreased.
Discussion
Mediastinal abscess due to esophageal perforation is a rare condition, and a mediastinal abscess caused by an ingested fish bone is even rarer. The English-language literature was reviewed by searching the PubMed database using the terms “fish bone”, “esophageal perforation”, and “mediastinal abscess”. This review identified only five cases, which are summarized in Table. The median duration of the onset after ingestion of a fish bone was 10 days. Most of the abscesses were located on the exterior of the posterior wall of the upper cervical esophagus. Various treatments based on drainage of the abscess were selected. In most cases, the fish bone was able to be detected with imaging. Although a fish bone was not detected by imaging studies in the present patient, we diagnosed the cause of the abscess as a fish bone because the pain developed immediately after eating fish and continuously and gradually worsened. In addition, no primary infection source, such as discitis, vertebral osteomyelitis, or other deep neck space infections, was apparent in our patient.
Table.
Review of Literature on Mediastinal Abscess Caused by Ingested Fish Bones.
| Case | Sex | Age | Onset after ingestion of fish bone | The existence of fish bone | Location of abscess | Treatment | Outcome | Reference | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | M | 47 | 13 | Yes | Upper esophagus | Conservative treatment | Died | 5 | ||||||||
| 2 | M | 49 | 7 | No | Cervical esophagus | Drainage using direct laryngoscopy and esophagoscopy | Alive | 5 | ||||||||
| 3 | F | 68 | 4 | Yes | Middle esophagus | Removal* and drainage using esophagoscopy | Alive | 12 | ||||||||
| 4 | M | 50 | 1 | Yes | Cervical esophagus | Surgery | Alive | 10 | ||||||||
| 5 | M | 63 | 14 | Yes | Upper esophagus | Removal* and drainage using mediastinumscopy | Alive | 13 | ||||||||
| 6 | F | 65 | 14 | No | Upper esophagus | Endoscopic ultrasound-guided abscess drainage using a nasobiliary drainage tube | Alive | Ours |
Removal*: Removal of fish bone
Various treatment methods have been reported, including surgery, endoscopic methods using a rigid esophagoscope or EUS, and conservative antibiotic therapy (7-13). In the present case, contrast-enhanced CT showed that the abscess was located on the back side of the esophagus and in extensive contact with the cervical and thoracic vertebrae. A surgical approach has been reported to be unavoidable when complications are detected by CT on admission (10). However, EUS-guided abscess drainage (EUS-AD) was selected for the treatment based on the following three findings: first, the abscess was encapsulated and separated from the pleural cavity on CT; second, there was no fish bone within or around the abscess, which rendered surgical removal unnecessary; and third, EUS-AD is much less invasive than surgery.
External drainage was performed using an NDT in the present case. There are some advantages of external drainage compared to internal drainage. First, irrigation with saline and drainage can completely clean up the abscess cavity. Changing the tube's position and the patient's body direction can prevent drainage failure. Second, culture samples can be taken repeatedly. The most common causative organism is Viridans streptococci. Furthermore, deep neck space infections are typically polymicrobial and include anaerobes (14,15). The drained pus was repeatedly sent for culture, but no other organisms were detected in the present case. Third, pharyngeal discomfort is less likely to occur with external drainage than with internal drainage. If internal drainage is performed, the esophageal side of the stent may induce pharyngeal pain and discomfort. Fourth, it is easy to perform external drainage even without substantial technical skill in narrow working spaces, such as very close to the upper esophageal sphincter. In addition, an oral elemental diet (OED) can be ingested with monitoring of the NDT. We expected that an OED would accelerate healing and prevent the disturbance of the intestinal environment.
There have been two case reports of EUS-AD for mediastinal abscess, with internal drainage performed using a diabolo-shaped lumen-apposing metal stent in one case (6) and two double-pigtail catheters in the other (7). However, these devices might not have been suitable for the present case because the lesion was located from the cervical to the superior portion of the mediastinum; in addition, the puncture route was also quite limited at the upper esophageal sphincter. Another report described a case of EUS-AD and debridement of the abscess cavity using videoendoscopy, a treatment that achieved a technical and clinical success rate of 100% (11). However, this approach may also not have been suitable for the present case, given the abscess location. Furthermore, because of the need for a high degree of technical skill, the authors of that report suggested that this treatment should only be attempted in high-volume centers with extensive experience in EUS.
However, despite its advantages, external drainage using NDT was limited by the diameter of the drainage route. This diameter limitation can lead to treatment failure through disruption of necrotic tissue. In cases with easy access using endoscopy, additional intervention through the fistula is recommended. When additional intervention is difficult, as in the present case, large-diameter dilation during the initial procedure is a treatment option. Large-diameter dilation is safe (11) and can promote drainage. In the present case, we confirmed that contrast flowed to the esophageal lumen from the cavity through the side of the NDT on fluoroscopic imaging.
We had to select the most suitable treatment option depending on the abscess size and location, endoscopists' experience, and patient's pain. This case suggests that external drainage using an NDT may be the first choice in any given situation.
After NDT removal, an NT was inserted into the esophagus with intermittent aspiration on order to avoid salivary exposure. We were concerned about recurrence due to saliva because the abscess occurred despite the absence of a lodged fish bone. If saliva had flowed back into the cavity, a residual fistula might have developed. Furthermore, the fistula was located in the upper esophageal sphincter and could not be closed endoscopically. Instead of endoscopic closure, we used TPN and NT placement. With the use of transesophageal EUS-AD and large-diameter dilation, about half of the patients reportedly showed a tendency toward spontaneous closure of fistula (11). Another study reported that the median healing time after endoscopic clipping for esophageal perforation was 18 days when the perforation was caused by endoscopic submucosal dissection (16). Previous reports showed that fistulae heal with time, but the duration required is unknown. The immediate resumption of oral intake after NDT removal can lead to recurrence. Whether or not NT placement is useful or how long it should be left in place is unclear. We managed the present case conservatively in order to ensure safety, as a recurrent infection would require difficult reintervention. However, the patient reported feeling discomfort during the period of NT placement. In another report, the patient was instructed to avoid swallowing saliva after surgical treatment (10). Use of an NT and TPN varies according to individual circumstances.
Cases of a mediastinal abscess treated by EUS-AD are quite rare. The further accumulation and consideration of similar cases will be necessary. Although various treatment methods for mediastinal abscess have been reported to date, this case report revealed that EUS-AD was a safe and effective treatment. The advantages and disadvantages of each treatment method should be considered before selecting treatments for each patient.
The authors state that they have no Conflict of Interest (COI).
References
- 1. Eisen GM, Baron TH, Dominitz JA, et al. Guideline for the management of ingested foreign bodies. Gastrointest Endosc 55: 802-806, 2002. [DOI] [PubMed] [Google Scholar]
- 2. Sung SH, Jeon SW, Son HS, et al. Factors predictive of risk for complications in patients with esophageal foreign bodies. Dig Liver Dis 43: 632-635, 2011. [DOI] [PubMed] [Google Scholar]
- 3. Kim JP, Kwon OJ, Shim HS, et al. Analysis of clinical feature and management of fish bone ingestion of upper gastrointestinal tract. Clin Exp Otorhinolaryngol 8: 261-267, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Grodinsky M, Holyoke EA. The fasciae and fascial spaces of the head, neck and adjacent regions. Am J Anat 63: 367-408, 1938. [Google Scholar]
- 5. Ahmad R, Ishlah W, Shaharudin MH, et al. Posterior mediastinal abscess secondary to esophageal perforation following fish bone ingestion. Med J Malaysia 63: 162-163, 2008. [PubMed] [Google Scholar]
- 6. Peng A, Li Y, Xiao Z, et al. Study of clinical treatment of esophageal foreign body-induced esophageal perforation with lethal complications. Eur Arch Otorhinolaryngol 269: 2027-2036, 2012. [DOI] [PubMed] [Google Scholar]
- 7. Consiglieri CF, Escobar I, Gornals JB. EUS-guided transesophageal drainage of a mediastinal abscess using a diabolo-shaped lumen-apposing metal stent. Gastrointest Endosc 81: 221-222, 2015. [DOI] [PubMed] [Google Scholar]
- 8. Saxena P, Kumbhari V, Khashab MA. EUS-guided drainage of a mediastinal abscess. Gastrointest Endosc 79: 998-999, 2014. [DOI] [PubMed] [Google Scholar]
- 9. Kim H, Kim Y, Cho JH, et al. Internal drainage of an esophageal perforation in a patient with a high surgical risk. Korean J Thorac Cardiovasc Surg 50: 395-398, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Toma EA, Oun M, Enciu O, et al. The surgical management of acute esophageal perforation by accidentally ingested fish bone. Chirurgia (Bucur) 113: 156-161, 2018. [DOI] [PubMed] [Google Scholar]
- 11. Wehrmann T, Stergiou N, Vogel B, et al. Endoscopic debridement of paraesophageal, mediastinal abscesses: a prospective case series. Gastrointest Endosc 62: 344-349, 2005. [DOI] [PubMed] [Google Scholar]
- 12. Kimura T, Takemoto T, Fujiwara Y, et al. Esophageal perforation caused by a fish bone treated with surgically indwelling drainage and fibrin glue injection for fistula formation. Ann Thorac Cardiovasc Surg 19: 289-292, 2013. [DOI] [PubMed] [Google Scholar]
- 13. Wang J, Wu WB, Chen L, et al. Video-mediastinoscopy assisted fish bone extraction and superior Medistinal abscess debridement. J Cardiothorac Surg 13: 38, 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Rega AJ, Aziz SR, Ziccardi VB. Microbiology and antibiotic sensitivities of head and neck space infections of odontogenic origin. J Oral Maxillofac Surg 64: 1377-1380, 2006. [DOI] [PubMed] [Google Scholar]
- 15. Huang TT, Tseng FY, Yeh TH, et al. Factors affecting the bacteriology of deep neck infection: a retrospective study of 128 patients. Acta Otolaryngol 126: 396-401, 2006. [DOI] [PubMed] [Google Scholar]
- 16. Qadeer MA, Dumot JA, Vargo JJ, et al. Endoscopic clips for closing esophageal perforations: case report and pooled analysis. Gastrointest Endosc 66: 605-611, 2007. [DOI] [PubMed] [Google Scholar]