Abstract
Nowadays, infertility is one of the health issues in public health. Women with infertility suffer from a wide range of psychological problems. The goal of this study was to evaluate depression, sexual dysfunction and quality of life in Iranian women with infertility. In this study, 189 infertile women enrolled. All participants were asked to fill valid and reliable Persian versions of Beck Depression Inventory (BDI), Beck Anxiety Inventory (BAI), SF-36 and female sexual function index (FSFI). Mean age and mean duration of marriage were 28±5.9 and 5.9±0.3 years, respectively. One hundred and fifteen (60.8%) women had primary infertility and the remaining subjects (39.2%) secondary infertility. Mean BDI, BAI, FSFI and their domains as well as quality of life subscales were not significantly different between the two groups. There was a significant correlation between BDI, BAI, FSFI and subscales and domains of quality of life. Women with either primary or secondary infertility did not differ in terms of depression, anxiety, sexual function and quality of life domains.
Keywords:infertility, depression, anxiety, sexual function, quality of life.
INTRODUCTION
Inability to conceive after one year of unprotected sex is defined as infertility, which is a disabling condition for couples (1). Nearly 20% of couples face this problem, which has a global impact on their lives, leading to impaired quality of life (2, 3). Psychological problems such as depression, anxiety, stress, sexual dysfunction and suicidal attempt are among the most common difficulties experienced by these couples (4, 5). Previous studies showed that sexual dysfunction is higher among women affected by infertility than controls (5, 6). Different factors such as age, hormonal treatment and psychological well-being will influence sexual function in infertile women (5). Impairment of quality of life is an issue of concern in infertile women, and its level is lower than that of healthy controls (7). As there are few studies regarding this issue in Iran, we designed this study to evaluate depression, sexual dysfunction and quality of life in Iranian women with infertility.
METHODS
This cross sectional study was done in Zabol Clinic of Infertility between January 2017 and January 2018.
Inclusion criteria were: candidates for in vitro fertilization (IVF) and no underlying diseases such as kidney disease, coronary disease, PCO (polycystic ovarian syndrome).
All participants were asked to fill valid and reliable Persian versions of Beck Depression Inventory (BDI), Beck Anxiety Inventory (BAI), SF-36 and female sexual function index (FSFI) (8-10).
BDI consists of 21 questions rating from 0-3. Scores between 0 and 9 indicate no depression, scores between 10 and 18 show mild to moderate depression, scores between 19 and 29 indicate moderate to severe depression, and scores between 30 and 63 correspond to severe depression (8).
BAI includes 21 questions, each rating from 0 to 3. Scores between 0 and 7 are indicative of minimal anxiety, scores between 8 and 15 show mild anxiety, scores between 16 and 25 indicate moderate anxiety, and scores between 26 and 63 show severe anxiety (11). FSFI is a19-item self-report tool to measure female sexual function providing scores on six domains of sexual function, which include desire, arousal, lubrication, orgasm, satisfaction, and pain (9).
The SF-36 questionnaire consists of 36 questions in eight aspects. All questions are scored on a scale of 0 to 100, with 100 representing the highest level of functioning possible. Higher scores indicate less impairment in the quality of life (10)
All data were analyzed using SPSS software version 23 (Statistical Package for the Social Sciences, version 23, SPSS Inc., Chicago, IL, USA). Data were presented as Mean±SD for continuous or frequencies for categorical variables. Independent sample t test was used for comparison of continuous variables. Pearson Correlation coefficient calculated. P<0.05 was considered as significant.
RESULTS
In this study, 189 infertile women enrolled. Mean age and mean duration of marriage were 28±5.9 and 5.9±0.3 years, respectively.
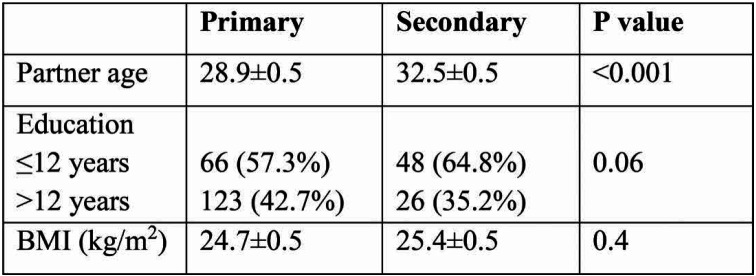
One hundred and fifteen (60.8%) had primary and remaining (39.2%) had secondary infertility. Partner age was significantly higher in secondary group (Table 1).
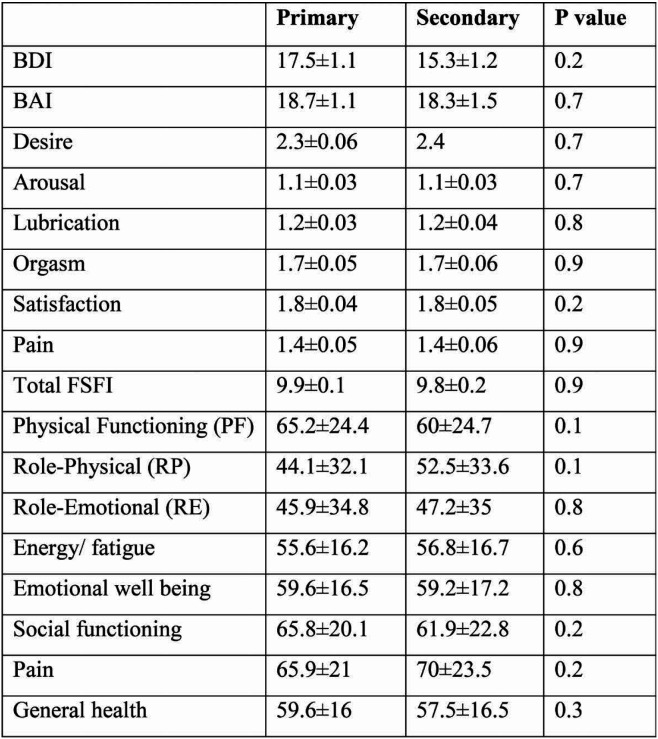
Mean BDI, BAI, FSFI and its domains as well as quality of life subscales were not significantly different between the two groups (Table2). There was a significant correlation regarding BDI, BAI, FSFI and its subscales and domains of quality of life (Table 3).
DISCUSSION
The result of this study showed that the mean scores of BDI, BAI, FSFI and SF-36 questionnaires were not significantly different between primary and secondary groups, while there were significant positive or negative correlations between most of these items. In our previous study, we found no significant difference regarding total FSFI score and its subscales in women with primary or secondary infertility (6), which confirms the current findings. In a previous study, Keshin et al. reported lower scores of orgasm, and satisfaction and total FSFI score in secondary group in comparison with primary one (12).
The results also showed that there was significant negative correlation regarding BDI/BAI and total FSFI score, which is indicative of negative effect of depression and anxiety on sexual function. This finding confirms findings of Lakatos et al (13). Depression is the most common psychological problem in women affected by infertility (5). This could be due to unsuccessful treatment of infertility and pressure on couples as the sense of powerlessness (13, 14).
Infertile couples experience a higher rate of anxiety, which could affect pregnancy outcome (15). In some previous studies, prevalence of anxiety was reported to vary between 9-28% in clinics for ART (16, 17), while the rate was higher for women than men (18). In a study in Taiwan, anxiety and depression was reported in 23% and 17% of infertile women under treatment (17), which is in accordance with the findings of Chi et al. (19). Dural et al. found higher quality of life scores in cases with lower anxiety and depression scores (20). BDI score had great correlation with emotional well-being, while anxiety had great correlation with pain domain of quality of life in our cases. In the study of Namdar et al., psychological dimension of QOL had greater correlation with the anxiety score (21).
We have also found that domains of quality of life were not significantly different between infertility groups, which is in agreement with the findings of Aduloju et al. (22). The results also show that, except RE, most domains of quality of life have a significant negative correlation with BDI and BAI. This finding is indicative of the negative effects of psychological problems on quality of life in infertile women. There is reciprocal relationship between depression and infertility treatment (23). Depressed cases do not seek treatment and couples seeking treatment become depressed after failure. It has been shown that infertility affects mental health, vitality, and emotional behavior domains od quality of life more than others (24). In many developing countries such as Iran, child bearing is very important and infertility can have a huge negative impact on social and marital life (21).
Women suffer from a wide range of psychological problems such as depression, anxiety, poorer marital adjustment, impaired quality of life, and less intercourse satisfaction (4, 21). It is unclear whether some special groups of women with infertility suffer more from psychological problems. The results of current study showed no significant difference regarding depression, anxiety, sexual function and quality of life between primary and secondary groups.
This study had some limitations. Firstly, it conducted in a clinic in Sistan and Baluchestan province. Secondly, the sample size in limited. Thirdly, there was no control group. Larger, multicentric studies with control groups are recommended.
CONCLUSION
Women with either primary or secondary infertility do not differ in terms of depression, anxiety, sexual function and quality of life domains.
Conflicts of interest: none declared.
Financial support: none declared.
TABLE 1.
Basic characteristics of two groups
TABLE 2.
Comparison of two groups regarding BDI, BAI, FSFI and its domains as well as quality of life subscales were not significantly different between the two groups
Contributor Information
Zahra SHAHRAKI, Zabol University of Medical Sciences, Zabol, Iran.
Mahsa GHAJARZADEH, Universal Council of Epidemiology (UCE), Universal Scientific Education and Research Network (USERN), Tehran, Iran.
Meysam GANJALI, Student Research Committee, Zabol University of Medical Sciences, Zabol, Iran.
References
- 1.Savitz-Smith J. Couples undergoing infertility treatment: implications for counselors. The Family Journal. 2003;4:383–387. [Google Scholar]
- 2.Baldur-Felskov B, Kjaer S, Albieri V, Steding-Jessen M, Kjaer T, Johansen C, et al. Psychiatric disorders in women with fertility problems: results from a large Danish register-based cohort study. Human reproduction. 2012;3:683–690. doi: 10.1093/humrep/des422. [DOI] [PubMed] [Google Scholar]
- 3.Kjaer TK, Jensen A, Dalton SO, Johansen C, Schmiedel S, Kjaer SK. Suicide in Danish women evaluated for fertility problems. Human reproduction. 2011;9:2401–2407. doi: 10.1093/humrep/der188. [DOI] [PubMed] [Google Scholar]
- 4.Monga M, Alexandrescu B, Katz SE, Stein M, Ganiats T. Impact of infertility on quality of life, marital adjustment, and sexual function. Urology. 2004;1:126–130. doi: 10.1016/j.urology.2003.09.015. [DOI] [PubMed] [Google Scholar]
- 5.Tanha FD, Mohseni M, Ghajarzadeh M. Sexual function in women with primary and secondary infertility in comparison with controls. International Journal of Impotence Research. 2014;4:132. doi: 10.1038/ijir.2013.51. [DOI] [PubMed] [Google Scholar]
- 6.Shahraki Z, Tanha FD, Ghajarzadeh M. Depression, sexual dysfunction and sexual quality of life in women with infertility. BMC Women’s Health. 2018;1:92. doi: 10.1186/s12905-018-0584-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rashidi B, Montazeri A, Ramezanzadeh F, Shariat M, Abedinia N, Ashrafi M . Health-related quality of life in infertile couples receiving IVF or ICSI treatment. BMC Health Services Research. 2008;1:186. doi: 10.1186/1472-6963-8-186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ghassemzadeh H, Mojtabai R, Karamghadiri N, Ebrahimkhani N. Psychometric properties of a Persian-language version of the Beck Depression Inventory-Second edition: BDI-II-PERSIAN. Depression and Anxiety. 2005;4:185–192. doi: 10.1002/da.20070. [DOI] [PubMed] [Google Scholar]
- 9.Fakhri A, Pakpour AH, Burri A, Morshedi H, Zeidi IM. The Female Sexual Function Index: translation and validation of an Iranian version. The Journal of Sexual Medicine. 2012;2:514–523. doi: 10.1111/j.1743-6109.2011.02553.x. [DOI] [PubMed] [Google Scholar]
- 10.Jafari H, Lahsaeizadeh S, Jafari P, Karimi M. Quality of life in thalassemia major: reliability and validity of the Persian version of the SF-36 questionnaire. Journal of Postgraduate Medicine. 2008;4:273. doi: 10.4103/0022-3859.41432. [DOI] [PubMed] [Google Scholar]
- 11.Kaviani H, Mousavi A. Psychometric properties of the Persian version of Beck Anxiety Inventory (BAI). Tehran University Medical Journal TUMS Publications. 2008;2:136–140. [Google Scholar]
- 12.Keskin U, Coksuer H, Gungor S, Ercan CM, Karasahin KE, Baser I. Differences in prevalence of sexual dysfunction between primary and secondary infertile women. Fertility and Sterility. 2011;5:1213–1217. doi: 10.1016/j.fertnstert.2011.08.007. [DOI] [PubMed] [Google Scholar]
- 13.Lakatos E, Szigeti JF, Ujma PP, Sexty R, Balog P. Anxiety and depression among infertile women: a cross-sectional survey from Hungary. BMC Women’s Health. 2017;1:48. doi: 10.1186/s12905-017-0410-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Reis S, Xavier MR, Coelho R, Montenegro N. Psychological impact of single and multiple courses of assisted reproductive treatments in couples: a comparative study. European Journal of Obstetrics & Gynecology and Reproductive Biology. 2013;1:61–66. doi: 10.1016/j.ejogrb.2013.07.034. [DOI] [PubMed] [Google Scholar]
- 15.Fassino S, Piero A, Boggio S, Piccioni V, Garzaro L. Anxiety, depression and anger suppression in infertile couples: a controlled study. Human Reproduction. 2002;11:2986–2994. doi: 10.1093/humrep/17.11.2986. [DOI] [PubMed] [Google Scholar]
- 16.Newton CR, Hearn MT, Yuzpe AA. Psychological assessment and follow-up after in vitro fertilization: assessing the impact of failure. Fertility and Sterility. 1990;5:879–886. doi: 10.1016/s0015-0282(16)53950-8. [DOI] [PubMed] [Google Scholar]
- 17.Chen T-H, Chang S-P, Tsai C-F, Juang K-D. Prevalence of depressive and anxiety disorders in an assisted reproductive technique clinic. Human Reproduction. 2004;10:2313–2318. doi: 10.1093/humrep/deh414. [DOI] [PubMed] [Google Scholar]
- 18.Volgsten H, Skoog Svanberg A, Ekselius L, Lundkvist Ö, Sundström Poromaa I. Prevalence of psychiatric disorders in infertile women and men undergoing in vitro fertilization treatment. Human Reproduction. 2008;9:2056–2063. doi: 10.1093/humrep/den154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chi H-J, Park I-H, Sun H-G, Kim J-W, Lee K-H. Psychological distress and fertility quality of life (FertiQoL) in infertile Korean women: The first validation study of Korean FertiQoL. Clinical and Experimental Reproductive Medicine. 2016;3:174–180. doi: 10.5653/cerm.2016.43.3.174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dural O, Yasa C, Keyif B, Celiksoy H, Demiral I, Yuksel Ozgor B, et al. Effect of infertility on quality of life of women: a validation study of the Turkish FertiQoL. Human Fertility. 2016;3:186–191. doi: 10.1080/14647273.2016.1214754. [DOI] [PubMed] [Google Scholar]
- 21.Namdar A, Naghizadeh MM, Zamani M, Yaghmaei F, Sameni MH. Quality of life and general health of infertile women. Health and Quality of Life Outcomes. 2017;1:139. doi: 10.1186/s12955-017-0712-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Aduloju OP, Olaogun OD, Aduloju T. Quality of life in women of reproductive age: a comparative study of infertile and fertile women in a Nigerian tertiary Centre. Journal of Obstetrics and Gynaecology. 2018;2:247–251. doi: 10.1080/01443615.2017.1347916. [DOI] [PubMed] [Google Scholar]
- 23.Namdar A, Naghizadeh MM, Zamani M, Yaghmaei F, Sameni MH. Quality of life and general health of infertile women. Health and Quality of life 0utcomes. 2017;1:139. doi: 10.1186/s12955-017-0712-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chachamovich J, Chachamovich E, Fleck M, Cordova FP, Knauth D, Passos E. Congruence of quality of life among infertile men and women: findings from a couple-based study. Human Reproduction. 2009;9:2151–2157. doi: 10.1093/humrep/dep177. [DOI] [PubMed] [Google Scholar]