Abstract
Background and objectives:Discoid lateral meniscus (DLM) is the most common congenital variant of a meniscus with a high prevalence meniscal tear due to abnormal shape and behavior. The proximal tibiofibular joint (PTFJ) has an important role during knee extension and ankle dorsiflexion. The aim of this research is to study the association between PTFJ morphology in MRI and DLM and its pathologies as compared with the normal lateral meniscus in Iranian population.
Materials and methods:Totally, 1729 MRI scans were reviewed, and 69 scans were selected based on inclusion/exclusion criteria. A group of aged-matched control patients without DLM were also included in this study. MRI scans were studied for DLM, meniscal tear and PTFJ inclination angle (horizontal or oblique). Findings were compared with those of patients without DLM.
Results:The frequency of horizontal-type PTFJ was significantly higher in the DLM group than in the control group. We also found a strong association (p value=0.018) between horizontal-type PTFJ and meniscal tear as compared with oblique-type in patients with DLM.
Conclusion:Horizontal-type PTFJ is more prevalent in patients with DLM. The meniscal tear is also more frequently seen in patients with DLM and horizontal-type PTFJ. Larger prospective studies are needed to confirm these results.
Keywords:Proximal tibiofibular joint, discoid lateral meniscus, meniscofibular ligament classification.
INTRODUCTION
Discoid lateral meniscus (DLM) is the most common congenital variant of the meniscus which was first reported by Young in 1889. Its prevalence ranges between 0.4% and 17% globally, and between 3% and 5% in the United States (1-3). The exact prevalence of DLM in the Iranian population is not well established in the literature. Disorganization of the circular collagen fiber system in DLM matrix makes the meniscus more prone to tearing up to twice as frequent than in normal lateral meniscus (20.4% vs. 9.9%) (2, 4-6). Magnetic resonance imaging (MRI) is usually useful and conclusive in the diagnosis of DLM (7, 8). However, the accuracy of detecting DLM can be decreased when some types of meniscal tear are present (6).
Proximal tibiofibular joint (PTFJ) has an important role in flexion and extension of the knee as well as in dorsiflexion of the ankle, which can be a possible source of pain in the lateral aspect of the knee joint (9-11). Considering pain symptoms in patients with DLM, investigating the morphology of PTFJ could help us better understand the biomechanics of the knee and may effect on pre- and post-operative plans in these patients.
Several anatomic studies have been done to describe the morphology of PTFJ, but the clinical application of these findings is limited (12-15). The more generally accepted classification of PTFJ morphology is based on the cadaveric studies by Ogden (16, 17). He divided PTFJ to horizontal- type (inclination of the joint<20°) and oblique-type (inclination>20°) by its different articular morphology. According to Barnett CH and Napier JR findings, horizontal-type PTFJ allows a wider range of motion during dorsiflexion of the ankle as compared with the oblique-type (18). The lateral meniscus is connected to the fibular head by the meniscofibular ligament (MFibL), an important stabilizer in the posterolateral corner of the knee joint (19-22). Bozkurt et al. confirmed the presence of this ligament in all subjects examined in their study and showed there was an increased tension of this ligament during dorsiflexion of the ankle (21). These authors also demonstrated that the NFL was thicker in subjects with a horizontal-type and rather slender in those with an oblique-type PTFJ.
Considering the connection of lateral meniscus to the fibular head by MFibL and thicker ligament in horizontal-type PTFJ, we can hypothesize that there are more loading and traction on this ligament in horizontal-type PTFJ, which can subsequently lead to different meniscal movements.
Suga N et al. have recently studied the morphology of PTFJ in patients with DLM as compared with normal lateral meniscus (23). Based on Ogden classification, these authors concluded that the horizontal-type PTFJ was significantly associated with DLM. To our knowledge, this was the only published study till the writing of this paper. Regarding all these findings, different PTFJ inclination and MFibL traction and subsequent meniscal movements could be an important explanation of the increased frequency of meniscal tear in patients with DLM. The aim of this study is to investigate the differences in the inclination of the PTFJ between patients with normal meniscus and DLM, with or without associated meniscal tear, using MRI. To the best of our knowledge, this is the first study on PTFJ morphology on the Iranian population with DLM.
MATERIAL AND METHODS
All patients who were referred for knee MRI to Shariati hospital academic center from October 2016 to March 2018 were assessed for their eligibility. Totally, 1729 MRI scans were reviewed. The scans had been performed using a Philips 1.5-T device with a knee surface coil. Standard protocols were used with a 4 mm section thickness. T2-weighted spin echo (SE), T1-weighted SE, proton density (PD) SE and fatsuppressed images in axial, coronal and sagittal sections were all reviewed for PTFJ inclination, meniscal or other possible bony or ligamentous pathologies. Images were reviewed and measured on MarcoPACS division software. Measurements were performed by an MSK radiologist with 10 years of experience and a junior radiology resident. Both readers were blinded to patient history.
Totally, 97 patients were diagnosed with DLM. They all received a phone call for gathering past medical and surgical history. Patients younger than 20 or older than 40 (due to the prevalence of osteoarthritis after the fifth decade) (24), those with comorbidities such as rheumatoid arthritis, osteoarthritis or any obvious bony and ligamentous abnormalities, and who had a history of knee joint surgery were excluded from this study. According to the mentioned criteria, 69 patients (38 females and 31 males) were selected for analysis. A group of aged-matched control patients without DLM were also included in this study (48 females and 21 males). As in the recently published study (23), sagittal images were used to assess the PTFJ inclination angle and classification based on the accepted Ogden method (16) (Figure 1).
Quantitative data are presented in mean ± standard deviation and qualitative as frequencies. We compared the distribution of characteristics between the groups using a non-parametric t-test (Mann-Whitney-U-Test) for numerical data and Fisher Exact or Chi-Square test in the event of categorical data. Statistical significance was assumed for a p value <0.05 and 95% confidence interval (CI). Inter-rater reliability was measured with Pearson correlation. The measurements reported in the document were performed by an experienced MSK radiologist. Statistical analysis was performed using SPSS software (Version 23.0; SPSS Inc.).
RESULTS
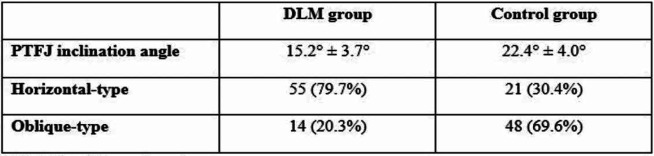
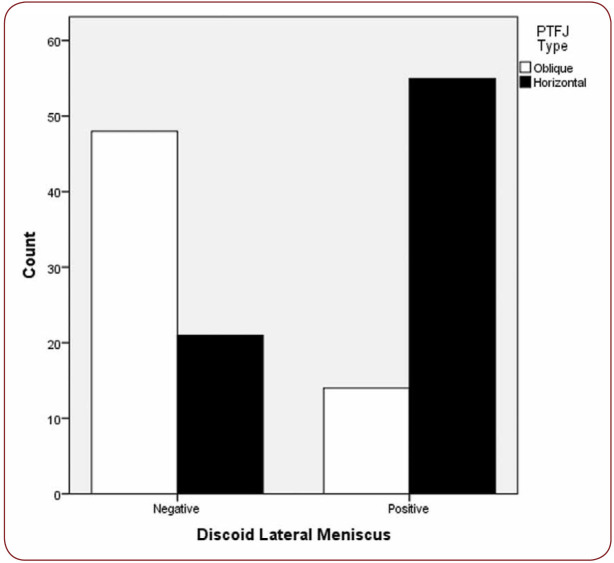
The prevalence of patients with DLM in Shariati hospital imaging center between October 2016 to March 2018 was about 5.6% (97 cases among 1729 reviewed MRI scans) which was narrowed to 69 cases based on inclusion/ exclusion criteria. The age of patients was 29.9±5.9 years in the DLM group and 29.1±6.1 years in and the control group, the minimum age being 20 and the maximum age 40. The inclination angle was 15.2°±3.7° for the DLM group and 22.4°±4.0° for the control group (p value< 0.001). PTFJ classification in the DLM and control groups are summarized in Table 1. The frequency of horizontal-type PTFJ was significantly higher in the DLM group than in the control group (p-value <0.001) (Figure 2).
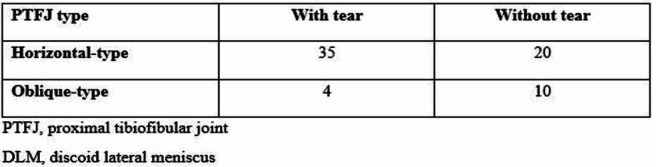
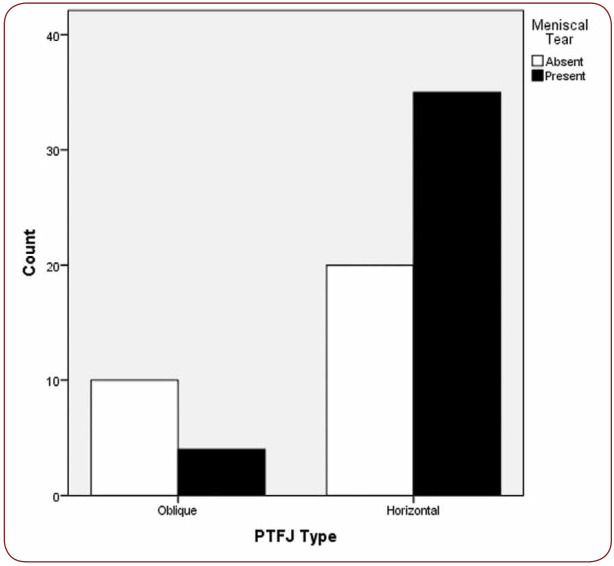
We have also analyzed the DLM group for a lateral meniscal tear. The meniscal tear was found in 39 (56.5%) patients with DLM. The inclination angle was 13.0°±3.1° for patients with DLM and meniscal tear and 18.1°±2.3° for those with DLM without a meniscal tear (p value< 0.001). In patients with DLM, we found a strong association (p value 0.018) between horizontal- type PTFJ and meniscal tear as compared with oblique-type (Table 2 and Figure 3). There was a strong inter-rater reliability for inclination measurements for the DLM group and the control group, with a Pearson correlation coefficient of 0.98 for both groups.
DISCUSSION
Suga N et al. have recently assessed the morphology of PTFJ in patients with DLM as compared with normal lateral meniscus (23) based on Ogden classification (16, 17). To our knowledge, there was no similar studies on Iranian population to the date this paper was written. Previous studies on discoid menisci have shown that this congenital variant was more susceptible to tear than normal ones (2, 4-6). Similarly to Suga N et al.’s report, we found that horizontaltype PTFJ had a strong association with DLM. However, in contrast to recent findings, we also concluded that there was a significant association between horizontal-type PTFJ and meniscal tear in patients with DLM. These latter findings are in contrast with Suga N et al.’s recent report. This discrepancy between findings may be explained by the use of different inclusion criteria, especially age groups, which are narrowed in our study. Larger studies are necessary to assess this disparity.
Horizontal-type PTFJ allows a wider range of motion during dorsiflexion of the ankle as compared with the oblique-type (18). The lateral meniscus is connected to the fibular head by MFibL (19-22). Increased tension of this ligament during dorsiflexion of the ankle along with thicker ligament in subjects with a horizontal-type PTFJ has been previously noted (21). Regarding these shreds of evidence, we can hypothesize that there are more loading and traction on this ligament in horizontal-type PTFJ, which can subsequently lead to different meniscal behavior and movement. These findings may be a preliminary explanation for a prevalent meniscal tear and lateral knee pain in patients with DLM.
The first limitation of this study was the sample size, which was due to the restricted database available in our imaging center. The more important limitation is detecting patients with DLM who have associated meniscal tears. As previously reported, MRI is usually useful in the diagnosis of DLM (7, 8). However, the accuracy of detecting DLM can be decreased when some types of meniscal tear are present (6). Considering this limitation of MRI, detailed surgical history and previous physical exam of patients could add more valuable information for analysis. Unfortunately, these data were not completely accessible due to limited hospital information system (HIS) and poor archives. Future prospective studies could help eliminate these limitations.
CONCLUSION
In comparison to the normal lateral meniscus, horizontal-type PTFJ is more prevalent in patients with DLM. Moreover, the meniscal tear is more frequently seen in patients with horizontaltype PTFJ and DLM. These findings may be related to the frequency of meniscal tear and lateral knee pain in these patients. Larger prospective studies are needed to confirm these results.
Conflicts of interest: none declared.
Financial support: none declared.
FIGURE 1.
Classification of PTFJ. The inclination angle is defined as the angle between PTFJ and the perpendicular line of the fibula axis. This sagittal PD image shows an oblique-type PTFJ.
TABLE 1.
PTFJ classification in the DLM and control groups
FIGURE 2.
Frequency of PTFJ types. The frequency of horizontal-type PTFJ is significantly higher in the DLM group than the control group
TABLE 2.
Lateral meniscal tear in DLM group
FIGURE 3.
The frequency of meniscal tear in patients with DLM. There is a strong association between horizontal-type PTFJ and meniscal tear as compared with oblique-type in patients with DLM
Contributor Information
Mostafa SHAHREZAEE, Department of Orthopedics, AJA University of Medical Sciences, Tehran, Iran.
Radin MAHERONNAGHSH, Department of Radiology, AJA University of Medical Sciences, Tehran, Iran.
Amirpejman HASHEMITAHERI, Tehran University of Medical Sciences, Tehran, Iran.
Mohammadreza CHAVOSHI, Department of Radiology, Shariati Hospital, Tehran, Iran.
References
- 1.Dai WL, Zhang H, Zhou AG, Zhang G, Zhang J. Discoid Lateral Meniscus. J Knee Surg. 2017;9:854–862. doi: 10.1055/s-0036-1598021. [DOI] [PubMed] [Google Scholar]
- 2.Kocher MS, Logan CA, Kramer DE. Discoid Lateral Meniscus in Children: Diagnosis, Management, and Outcomes. J Am Acad Orthop Surg. 2017;11:736–743. doi: 10.5435/JAAOS-D-15-00491. [DOI] [PubMed] [Google Scholar]
- 3.Jordan MR. Lateral Meniscal Variants: Evaluation and Treatment. J Am Acad Orthop Surg. 1996;4:191–200. doi: 10.5435/00124635-199607000-00003. [DOI] [PubMed] [Google Scholar]
- 4.Jung JY, Choi SH, Ahn JH, Lee SA. MRI findings with arthroscopic correlation for tear of discoid lateral meniscus: comparison between children and adults. Acta Radiol. 2013;4:442–447. doi: 10.1177/0284185113475442. [DOI] [PubMed] [Google Scholar]
- 5.Rohren EM, Kosarek FJ, Helms CA. Discoid lateral meniscus and the frequency of meniscal tears. Skeletal Radiol. 2001;6:316–320. doi: 10.1007/s002560100351. [DOI] [PubMed] [Google Scholar]
- 6.Sohn DW, Bin SI, Kim JM, Lee BS, Kim SJ. Discoid lateral meniscus can be overlooked by magnetic resonance imaging in patients with meniscal tears. K. nee Surg Sports Traumatol Arthrosc. 2018;8:2317–2323. doi: 10.1007/s00167-017-4704-6. [DOI] [PubMed] [Google Scholar]
- 7.Kramer DE, Micheli LJ. Meniscal tears and discoid meniscus in children: diagnosis and treatment. J Am Acad Orthop Surg. 2009;11:698–707. doi: 10.5435/00124635-200911000-00004. [DOI] [PubMed] [Google Scholar]
- 8.Ryu KN, Kim IS, Kim EJ, Ahn JW, Bae DK, Sartoris DJ, et al. MR imaging of tears of discoid lateral menisci. AJR Am J Roentgenol. 1998;4:963–967. doi: 10.2214/ajr.171.4.9762976. [DOI] [PubMed] [Google Scholar]
- 9.Kruckeberg BM, Cinque ME, Moatshe G, Marchetti D, DePhillipo NN, Chahla J, et al. Proximal Tibiofibular Joint Instability and Treatment Approaches: A Systematic Review of the Literature. Arthroscopy. 2017;9:1743–1751. doi: 10.1016/j.arthro.2017.03.027. [DOI] [PubMed] [Google Scholar]
- 10.Marchetti DC, Moatshe G, Phelps BM, Dahl KD, Ferrari MB, Chahla J, et al. The Proximal Tibiofibular Joint: A Biomechanical Analysis of the Anterior and Posterior Ligamentous Complexes. Am J Sports Med. 2017;8:1888–1892. doi: 10.1177/0363546517697288. [DOI] [PubMed] [Google Scholar]
- 11.Warner BT, Moulton SG, Cram TR, LaPrade RF. Anatomic Reconstruction of the Proximal Tibiofibular Joint. Arthrosc Tech. 2016;1:e207–e210. doi: 10.1016/j.eats.2015.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Barnett CH, Napier JR. The form and mobility of the fibula in metatherian mammals. J Anat. 1953;2:207–213. [PMC free article] [PubMed] [Google Scholar]
- 13.Bozkurt M, Yilmaz E, Atlihan D, Tekdemir I, Havitcioglu H, Gunal I. The proximal tibiofibular joint: an anatomic study. Clin Orthop Relat Res. 2003;406:136–140. doi: 10.1097/01.blo.0000030167.56585.2f. [DOI] [PubMed] [Google Scholar]
- 14.Lambert KL. The weight-bearing function of the fibula. A strain gauge study. J Bone Joint Surg Am. 1971;3:507–513. [PubMed] [Google Scholar]
- 15.Espregueira-Mendes JD, da Silva MV . Anatomy of the proximal tibiofibular joint. Knee Surg Sports Traumatol Arthrosc. 2006;3:241–249. doi: 10.1007/s00167-005-0684-z. [DOI] [PubMed] [Google Scholar]
- 16.Ogden JA. The anatomy and function of the proximal tibiofibular joint. Clin Orthop Relat Res. 1974;101:186–191. [PubMed] [Google Scholar]
- 17.Ogden JA. Subluxation of the proximal tibiofibular joint. Clin Orthop Relat Res. 1974;101:192–197. [PubMed] [Google Scholar]
- 18.Barnett CH, Napier JR. The axis of rotation at the ankle joint in man; its influence upon the form of the talus and the mobility of the fibula. J Anat. 1952;1:1–9. [PMC free article] [PubMed] [Google Scholar]
- 19.Obaid H, Gartner L, Haydar AA, Briggs TW, Saifuddin A. The meniscofibular ligament: an MRI study. Eur J Radiol. 2010;1:159–161. doi: 10.1016/j.ejrad.2008.09.026. [DOI] [PubMed] [Google Scholar]
- 20.Unay K, Ozkan K, Esenkaya I, Poyanli O, Akan K. Rupture of the meniscofibular ligament. J Orthop Surg Res. 2010;5:35. doi: 10.1186/1749-799X-5-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bozkurt M, Elhan A, Tekdemir I, Tonuk E. An anatomical study of the meniscofibular ligament. Knee Surg Sports Traumatol Arthrosc. 2004;5:429–433. doi: 10.1007/s00167-003-0450-z. [DOI] [PubMed] [Google Scholar]
- 22.Natsis K, Paraskevas G, Anastasopoulos N, Papamitsou T, Sioga A. Meniscofibular ligament: morphology and functional significance of a relatively unknown anatomical structure. Anat Res Int. 2012;2012:214784. doi: 10.1155/2012/214784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Suga N, Nakasa T, Ishikawa M, Nakamae A, Hayashi S, Yoshikawa M, et al. Characteristic morphology of the proximal tibiofibular joint in patients with discoid lateral meniscus. Knee. 2018;6:1027–1032. doi: 10.1016/j.knee.2018.07.019. [DOI] [PubMed] [Google Scholar]
- 24.Tahmasebi MN, Motaghi A, Shahrezaee M. Total knee arthroplasty in patients with osteoarthritis: Results of 34 operations. Tehran Univ Med J. 2009;2:146–150. [Google Scholar]