Abstract
Background:
Irreparable rotator cuff tears lead to superior translation of the humeral head. Numerous surgical management options are available to treat the condition.
Purpose:
To compare superior capsule stability among different types of patch grafting in irreparable rotator cuff tears.
Methods:
Six cadaveric shoulders were tested in a custom-designed shoulder testing system. Superior translation of the humerus and subacromial contact pressure were quantified in an intact condition (condition 1), after cutting the supraspinatus tendon (condition 2), and after additionally cutting the superior capsuloligamentous complex (condition 3). The results were compared among 3 types of patch grafting, in which capsule reconstruction was achieved by glenoidal 3-point (condition 4) or 2-point (condition 5) fixation or by affixing a graft below the acromion (condition 6).
Results:
No significant difference in subacromial pressure was measured by reconstruction with 2 or 3 anchors compared with conditions 1 and 2 (P > .05). However, with 3-point fixation, lower levels of pressure were measured than with 2-point fixation. Moreover, superior translation values were lower with 3-point fixation; the same applied for values of the preserved capsule as compared with the torn capsule. In condition 6, a significant increase in pressure in the neutral position was documented (P < .05).
Conclusion:
The superior capsuloligamentous complex plays an important role in stabilizing the glenohumeral joint. The results suggest that with additional medial anchoring at the coracoid base, the depressing and centering effect of the superior complex can probably be regained in a more physiological way compared with a reconstructed capsule with 2 glenoid attachments or with an interpositional graft below the acromion.
Keywords: superior glenohumeral stability, irreparable rotator cuff tears, capsule reconstruction, interposition, biomechanics
Irreparable rotator cuff tears lead to superior translation of the humeral head, which increases the risk of impingement between the greater tuberosity and the inferior surface of the acromion.1 Numerous surgical management options are available to treat this condition.1,5,14,19 Prominent in the most recent literature is reconstruction of the superior capsule by a graft that is attached medially to the superior glenoid and laterally to the greater tuberosity, as well as the use of an interpositional graft implanted between the inferior surface of the acromion and the humeral head, with the aim of improving glenohumeral translation to match physiological conditions. For both treatment options, promising short-term and midterm clinical results are reported.3,4,6,11,15,17,18,20
Nevertheless, some elementary questions regarding the biomechanical differences of these 2 surgical techniques remain unresolved to this date. First of all, there is debate about whether a subacromial spacer has the same biomechanical effects as reconstruction of the superior capsule, especially as the superior capsuloligamentous complex appears to be more efficient in adduction and acts as a secondary restraint in abduction.16 Second, as the anatomic attachment of the so-called superior coracohumeral-glenohumeral ligament complex is very broad and spans a significant portion of the glenoid and the coracoid,16 it remains unclear if an additional attachment at the coracoid base would have an overall beneficial effect on shoulder biomechanics after surgery.
To provide research data on these relevant issues, the objective of the present study was to compare superior capsule stability among different types of patch grafting in irreparable rotator cuff tears, in which superior capsule reconstruction was achieved by 2 or 3 attachments at the glenoid side or by positioning the graft below the acromion. We hypothesized that (1) a stabilizing effect of the superior capsule cannot solely be simulated by mere subacromial graft interposition and (2) with broad medial anchoring, the centering effect of the superior complex can probably be regained in a more physiological way.
Methods
Specimen Preparation
Six fresh-frozen, cadaveric unilateral shoulder specimens were used in the study. They were from 6 male donors with a mean age of 72 years (range, 51-92 years). The specimens were stored at –20°C and thawed at room temperature 24 hours before dissection.
The clavicle and humeral shaft were transected to a length of 10 cm. Thereafter, the same approach was undertaken in each specimen, which consisted of the dissection of skin and subcutaneous tissue while preserving the rotator cuff tendons, the capsule, the coracoacromial ligament, the pectoralis major, the latissimus dorsi, and the deltoid insertion. The tendons were augmented with 1.0 polydioxanone (PDS) fibers (Ethicon) in a Krackow locked running stitch.
The inferior angle of the scapula was positioned in rectangular preparation boxes made of hard plastic by using Technovit 4004 (Kulzer), a plastic embedding medium system based on methyl methacrylate. The scapula was placed in a way that allowed the glenoid to be positioned parallel to the top of the scapular box. Afterward, the specimens were mounted in a vertical position in a materials testing machine (Z010; Zwick). The scapular box was fixed to the custom-designed testing jig at 20° of anterior tilt in the sagittal plane. The humerus was aligned with the scapular plane.
Test Setup
With use of a fastening rope, the deltoid insertion was connected to the mobile traverse of the testing machine. The other muscle forces were simulated by directly attaching strings to the augmented tendons. After predefining 2 load cases, weight was put on the strings based on the established values of previous studies on cross-sectional force distribution of the relevant muscles (load case 1 [balanced loading, simulated resting position without superior force]: 40 N, deltoid; 20 N, pectoralis major; 20 N, latissimus dorsi; 10 N, supraspinatus; 10 N, infraspinatus/teres minor; 10 N, subscapularis; load case 2 [unbalanced loading, superior force on the humeral head]: 80 N, deltoid; 10 N, supraspinatus; 10 N, infraspinatus/teres minor; 10 N, subscapularis).10,12,13
The measurements were performed at 0°, 45°, and 90° of shoulder abduction in a neutral rotated position, which was achieved by 0° of scapular upward rotation and 0° of glenohumeral abduction, 15° of scapular upward rotation and 30° of glenohumeral abduction, and 30° of scapular upward rotation and 60° of glenohumeral abduction, respectively.
The 2 load cases were consecutively performed in each of the 6 following test conditions for each specimen. In condition 1, an intact rotator cuff tendon with an intact capsule complex was tested; in condition 2, the supraspinatus tendon was cut; in condition 3, the superior capsule additionally was dissected; and in conditions 4, 5, and 6, a graft was inserted.
The grafts were made by folding a human fascia lata, which was harvested through a longitudinal incision at the proximal femur of the specimen. The incision was carried down to the iliotibial band of the fascia lata. Carefully, the overlying fat was dissected, and the fascia was gently elevated off of the underlying muscle. After that, the grafts were folded twice to a thickness of 4 mm and sutured around the edge of the folds. The anterior-posterior width was matched between the posterior edge of the superior glenoid and the coracoid base and footprint at the greater tuberosity. The medial-lateral length of the grafts was matched in distance between the glenoid and the greater tuberosity in 30° of abduction.
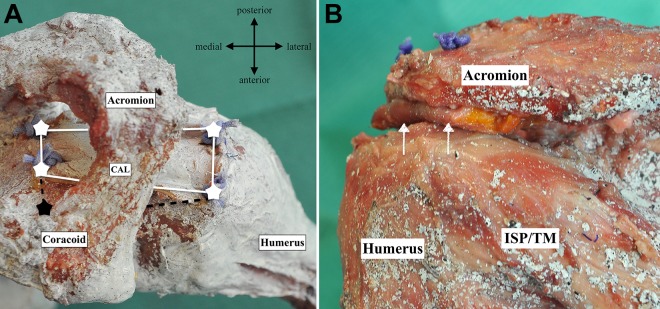
At the glenoid site, 3 bone tunnels were created, 2 with a distance of 5 mm from the superior glenoid rim and 1 additional tunnel at the base of the coracoid process. Consequently, 2 bone tunnels were drilled with a distance between them of 15 mm on the greater tuberosity at the footprint of the native capsule (Figure 1).
Figure 1.
(A) Superior view of a shoulder specimen (in a “speckle pattern” for the measurements). Attachments of the graft (white stars) after additional fixation at the coracoid base (black star), per condition 5. (B) Posterior view of a shoulder specimen. Attachments of the graft (white arrows) with transosseous suture repair inferior to the acromion, per condition 6. CAL, coracoacromoial ligament; ISP/TM, infraspinatus/teres minor.
In condition 4, the graft was attached at all 5 tunnels using transosseous suture repair (5 polyester sutures; 0 PDS fibers) at 30° of glenohumeral abduction in the scapular plane. The graft was attached with the infraspinatus by 2.0 PDS fibers. In condition 5, the attachment area at the coracoid base was dissected (Figure 1A). In condition 6, two drill holes were created through the acromion with a distance between them of 15 mm. Then, the fascia lata graft (4 mm) was attached with transosseous suture repair inferior to the acromion (Figure 1B).
Measurements
Superior translation of the humeral head relative to the acromion and subacromial pressure were measured for the abovementioned load cases. Superior translation was recorded for 3-dimensional displacement measurements with digital image correlation using a system with 2 monochrome digital cameras (Q-400-3D; Dantec Dynamics). Prior calibration of the image parameters as well as the exact placement of both cameras at a predefined distance and angle to each other made the 3-dimensional calculation of each point on the coordinate possible. Measurements of the positioning and geometry of each point for the entire duration of the testing period allowed for calculation according to the Gauss least squares method.
Calibration of the cameras was performed by a black-and-white checkerboard–patterned calibration plate, which was positioned typically 8 times at different angles in front of the specimen to allow for correct detection of the positioning of the cameras to the specimen and the correct physical size of the geometry in the picture frame. In total, 2 pairs of points from 2 predefined sets of points on the shoulder joint were chosen, which then were tracked by the cameras during translation measurements of the humerus . Point P1 served as a fix point at the lateral acromion, and point P2 was placed at the level of the insertion of the supraspinatus. The second pair of points, P3 and P4, was placed at a 25-mm medial distance to pair P1 and P2.
A stochastic “speckle pattern” was sprayed on the specimens (Figure 1), which was recorded during motion and automatically evaluated locally using subpixel-accurate digital image correlation algorithms with Istra 4D software (Dantec Dynamics).
To display the shift in translation in the different conditions and under different load cases (40 N and 80 N), a mean value of displacement was calculated independently of abduction. This was done by summarizing the local speckle pattern at points P1/P2 and P3/P4 in all degrees of abduction.
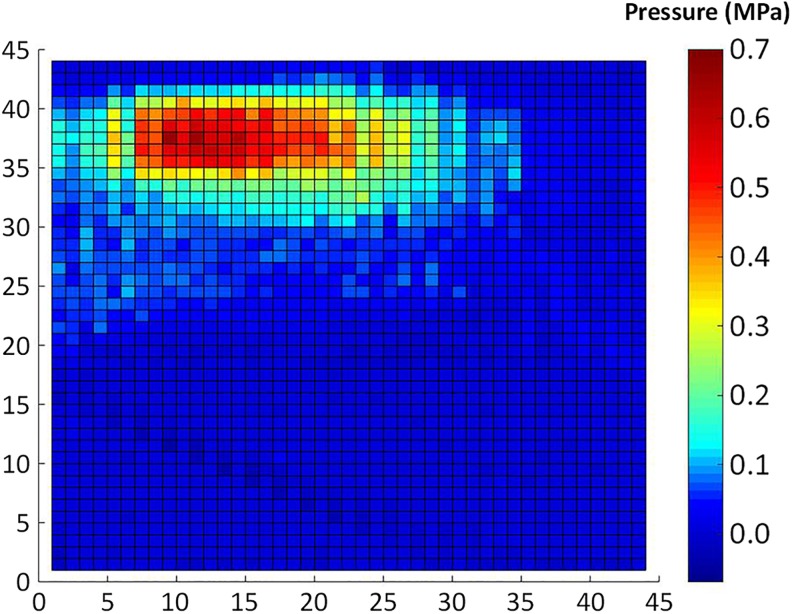
Subacromial contact pressure was recorded by means of Tekscan pressure sensors. A pressure sensor (Pressure Mapping Sensor 5076; Tekscan) with a total matrix height and width of 83.8 mm and a thickness of 0.102 mm was inserted inferior to the acromion. The sensors consisted of 44 rows and columns, comprising a total of 1.936 detection units (sensels) with a resolution of 27.6 sensels/cm2. When pressure was applied to the sensor, the pressure-dependent resistance of the sensels changed; this could be digitally analyzed to evaluate and visualize the contact area and pressure by means of color-coded mapping (Figure 2).
Figure 2.
Subacromial pressure distribution, which was digitally visualized by means of color-coded mapping.
Results
As shown in Table 1, there was a significant increase in pressure in condition 3 compared with the neutral position (0° of abduction) in the physiological situation/condition 1 (P < .05). Moreover, in 45° and 90° of abduction, a rise in subacromial pressure was observed compared with the physiological condition (P > .05). No significant difference in pressure was measured by reconstruction with 2 (condition 5) or 3 (condition 4) anchors compared with conditions 1 and 2 (P > .05). However, in condition 4, slightly lower levels of pressure were measured compared with condition 5 . In condition 6, a significant increase in pressure in the neutral position (P < .05) was documented. This effect did not occur in the setups with 45° and 90° of abduction (P > .05). The subacromial pressure values are presented in Table 1.
TABLE 1.
Subacromial Contact Pressurea
| Abduction | Condition 1 | Condition 2 | P | Condition 3 | P | Condition 4 | P | Condition 5 | P | Condition 6 | P |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 0° | 0.08 ± 0.07 | 0.10 ± 0.10 | .78 | 0.30 ± 0.17 | .001 | 0.09 ± 0.08 | .84 | 0.14 ± 0.07 | .33 | 0.24 ± 0.12 | .02 |
| 45° | 0.09 ± 0.09 | 0.21 ± 0.22 | .17 | 0.26 ± 0.15 | .05 | 0.06 ± 0.13 | .80 | 0.12 ± 0.20 | .72 | 0.15 ± 0.12 | .50 |
| 90° | 0.13 ± 0.09 | 0.15 ± 0.22 | .81 | 0.19 ± 0.16 | .45 | 0.04 ± 0.12 | .31 | 0.17 ± 0.09 | .56 | 0.17 ± 0.15 | .57 |
aData are presented as mean ± SD in MPa. Bolded P values indicate statistically significant difference compared with condition 1 (intact).
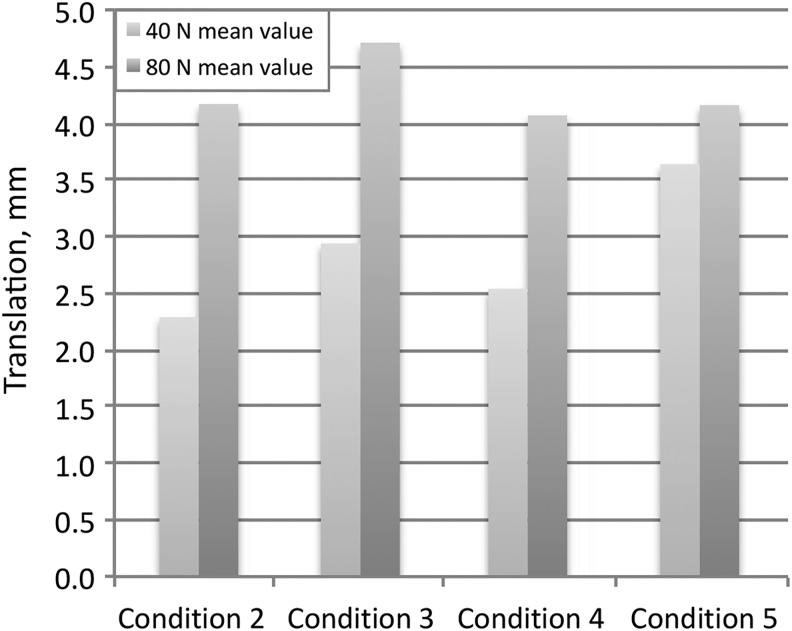
Table 2 and Figure 3 show the measurements of superior translation independently of abduction. The values were lower with 3-point fixation (condition 4) compared with measured displacement with 2-point fixation (condition 5); the same applied for displacement of the preserved capsule (condition 1) as compared with the torn capsule (condition 2).
TABLE 2.
Superior Translation of the Humeral Head
| Loading Trial | Humeral Head Translation, mm | |||
|---|---|---|---|---|
| 0° of Abduction | 45° of Abduction | 90° of Abduction | Mean Valuea | |
| Condition 2 | ||||
| 40 N | 2.61 | 1.15 | 3.11 | 2.29 |
| 80 N | 4.95 | 2.39 | 5.18 | 4.17 |
| Condition 3 | ||||
| 40 N | 4.04 | 2.11 | 2.67 | 2.94 |
| 80 N | 4.90 | 4.33 | 4.89 | 4.71 |
| Condition 4 | ||||
| 40 N | 3.24 | 1.28 | 3.12 | 2.54 |
| 80 N | 4.73 | 2.71 | 4.77 | 4.07 |
| Condition 5 | ||||
| 40 N | 4.76 | 2.98 | 3.18 | 3.64 |
| 80 N | 5.86 | 2.58 | 4.05 | 4.16 |
aThe mean value was calculated independently of abduction.
Figure 3.
Superior translation (mm) of the humeral head including a mean value, which was calculated independently of abduction.
Discussion
The present study measured and compared superior capsule shoulder stability after applying different superior capsule reconstruction techniques and subacromial graft interposition in a simulated condition of an irreparable rotator cuff tear. The findings of the 6 tested cadaveric shoulders support the results of previous biomechanical studies, which showed that the shoulder capsule plays an important role in stabilizing the glenohumeral joint.13 Any damage of its integrity simultaneously reduces the head-depressing and head-centering effect, which was presented by Mihata et al13 in previous biomechanical studies.7
Moreover, the results indicate a slight benefit of applying a reconstruction technique that matches natural conditions. Previous anatomic studies showed that the coracohumeral–superior glenohumeral ligament complex usually has a very broad attachment at the glenoid side and that it includes an essential anterior structure attaching at the coracoid process.2,16 As additional medial anchoring at the coracoid base better reconstructs such a physiological attachment, it can be assumed that the depressing and centering effect of the superior complex is also restored more fully. Even if we did not find statistically significant differences, this hypothesis is supported by the measured statistical tendencies in the reduction of the amount of misdirected superior translation and of subacromial pressure compared with that in graft fixation with only 2 attachment points at the glenoid. As this study only focused on the movement of abduction, future studies are needed to elaborate on any further beneficial effects of an additional attachment point, which may be especially relevant, as the coracohumeral ligamentous structure reaches its full capacity when the humerus is externally rotated, adducted, and retroflexed.2,8,9 Further studies should incorporate internal and external rotational movements of the humerus.
When considering the fact that the superior complex takes full effect in adduction and serves as a secondary restraint in abduction, it remains ever more debatable whether an interpositional graft can have the same biomechanical effects. Our results suggest that the reconstructed capsule shows a slight advantage on overall force distribution compared with the interpositional graft. A reconstructed capsule could be even more effective by fixation of the remaining rotator cuff at the graft. Hence, it can be concluded that the stabilizing effect of the superior capsule cannot solely be achieved or simulated by mere interposition. This becomes especially obvious when considering the differences in pressure to the neutral position, in which the reconstructed capsule shows a stabilizing effect in the superior direction. Again, this could be even more important in anterosuperior and inferior stability, as the superior capsule aids in protecting the humeral head from anterosuperior and inferior displacement.
All results have to be discussed and interpreted in light of the major limitations of this study. Despite the fact that the setup was arranged according to a pretesting power analysis based on existing biomechanical studies,10,12,13 most of our results showed only statistical tendencies and no statistically significant differences. Further studies with a greater number of specimens are needed to review these findings. Moreover, one has to bear in mind that the mechanical test setup with static muscle loading in cadaveric specimens does not fully match the biological muscle response. While bearing such limitations in mind, the chosen cadaveric study setup seems to offer one of the best available options to directly measure subacromial contact pressure as different interrelated muscle force responses are being taken into account.
Conclusion
The study results confirm previous biomechanical studies showing that the shoulder capsule plays an important role in stabilizing the glenohumeral joint. The comparison of the results of the different reconstruction techniques revealed statistical tendencies indicating that with additional medial anchoring at the coracoid base, the depressing and centering effect of the superior complex can probably be regained in a more physiological way compared with a reconstructed capsule with 2 glenoid attachments or with an interpositional graft below the acromion.
Footnotes
The authors declared that there are no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval was not sought for the present study.
References
- 1. Bedi A, Dines J, Warren RF, Dines DM. Massive tears of the rotator cuff. J Bone Joint Surg Am. 2010;92(9):1894–1908. [DOI] [PubMed] [Google Scholar]
- 2. Cooper DE, O’Brien SJ, Warren RF. Supporting layers of the glenohumeral joint: an anatomic study. Clin Orthop Relat Res. 1993;289:144–155. [PubMed] [Google Scholar]
- 3. Denard PJ, Brady PC, Adams CR, Tokish JM, Burkhart SS. Preliminary results of arthroscopic superior capsule reconstruction with dermal allograft. Arthroscopy. 2018;34(1):93–99. [DOI] [PubMed] [Google Scholar]
- 4. Deranlot J, Herisson O, Nourissat G. et al. Arthroscopic subacromial spacer implantation in patients with massive irreparable rotator cuff tears: clinical and radiographic results of 39 retrospectives cases. Arthroscopy. 2017;33(9):1639–1644. [DOI] [PubMed] [Google Scholar]
- 5. Henry P, Wasserstein D, Park S. et al. Arthroscopic repair for chronic massive rotator cuff tears: a systematic review. Arthroscopy. 2015;31(12):2472–2480. [DOI] [PubMed] [Google Scholar]
- 6. Holschen M, Brand F, Agneskirchner JD. Subacromial spacer implantation for massive rotator cuff tears: clinical outcome of arthroscopically treated patients. Obere Extrem. 2017;12(1):38–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Ishihara Y, Mihata T, Tamboli M. et al. Role of the superior shoulder capsule in passive stability of the glenohumeral joint. J Shoulder Elbow Surg. 2014;23(5):642–648. [DOI] [PubMed] [Google Scholar]
- 8. Kuhn JE, Bey MJ, Huston LJ, Blasier RB, Soslowsky LJ. Ligamentous restraints to external rotation of the humerus in the late-cocking phase of throwing: a cadaveric biomechanical investigation. Am J Sports Med. 2000;28(2):200–205. [DOI] [PubMed] [Google Scholar]
- 9. Lee TQ, Black AD, Tibone JE, McMahon PJ. Release of the coracoacromial ligament can lead to glenohumeral laxity: a biomechanical study. J Shoulder Elbow Surg. 2001;10(1):68–72. [DOI] [PubMed] [Google Scholar]
- 10. Mihata T, Bui CNH, Akeda M. et al. A biomechanical cadaveric study comparing superior capsule reconstruction using fascia lata allograft with human dermal allograft for irreparable rotator cuff tear. J Shoulder Elbow Surg. 2017;26(12):2158–2166. [DOI] [PubMed] [Google Scholar]
- 11. Mihata T, Lee TQ, Watanabe C. et al. Clinical results of arthroscopic superior capsule reconstruction for irreparable rotator cuff tears. Arthroscopy. 2013;29(3):459–470. [DOI] [PubMed] [Google Scholar]
- 12. Mihata T, McGarry MH, Kahn T, Goldberg I, Neo M, Lee TQ. Biomechanical role of capsular continuity in superior capsule reconstruction for irreparable tears of the supraspinatus tendon. Am J Sports Med. 2016;44(6):1423–1430. [DOI] [PubMed] [Google Scholar]
- 13. Mihata T, McGarry MH, Pirolo JM, Kinoshita M, Lee TQ. Superior capsule reconstruction to restore superior stability in irreparable rotator cuff tears: a biomechanical cadaveric study. Am J Sports Med. 2012;40(10):2248–2255. [DOI] [PubMed] [Google Scholar]
- 14. Ono Y, Davalos Herrera DA, Woodmass JM, Boorman RS, Thornton GM, Lo IK. Graft augmentation versus bridging for large to massive rotator cuff tears: a systematic review. Arthroscopy. 2017;33(3):673–680. [DOI] [PubMed] [Google Scholar]
- 15. Petri M, Greenspoon JA, Moulton SG, Millett PJ. Patch-augmented rotator cuff repair and superior capsule reconstruction. Open Orthop J. 2016;10:315–323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Pouliart N, Somers K, Eid S, Gagey O. Variations in the superior capsuloligamentous complex and description of a new ligament. J Shoulder Elbow Surg. 2007;16(6):821–836. [DOI] [PubMed] [Google Scholar]
- 17. Ricci M, Vecchini E, Bonfante E. et al. A clinical and radiological study of biodegradable subacromial spacer in the treatment of massive irreparable rotator cuff tears. Acta Biomed. 2017;88(suppl 4):75–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Senekovic V, Poberaj B, Kovacic L. et al. The biodegradable spacer as a novel treatment modality for massive rotator cuff tears: a prospective study with 5-year follow-up. Arch Orthop Trauma Surg. 2017;137(1):95–103. [DOI] [PubMed] [Google Scholar]
- 19. Sevivas N, Ferreira N, Andrade R. et al. Reverse shoulder arthroplasty for irreparable massive rotator cuff tears: a systematic review with meta-analysis and meta-regression. J Shoulder Elbow Surg. 2017;26(9):e265–e277. [DOI] [PubMed] [Google Scholar]
- 20. Tokish JM, Beicker C. Superior capsule reconstruction technique using an acellular dermal allograft. Arthrosc Tech. 2015;4(6):e833–e839. [DOI] [PMC free article] [PubMed] [Google Scholar]