Abstract
Aim
In-hospital cardiac arrest occurs in > 5,000 children each year in the US and almost half will not survive to discharge. Animal data demonstrate that an immediate post-resuscitation burst of hypertension is associated with improved survival. We aimed to determine if systolic and diastolic invasive arterial blood pressures immediately (0–20 min) after return of spontaneous circulation (ROSC) are associated with survival and neurologic outcomes at hospital discharge.
Methods:
This is a secondary analysis of the Pediatric Intensive Care Quality of CPR (PICqCPR) study of invasively measured blood pressures during intensive care unit CPR. Patients were eligible if they achieved ROSC and had at least one invasively measured blood pressure within the first 20 minutes following ROSC. Post-ROSC blood pressures were normalized for age, sex and height. “Immediate hypertension” was defined as at least one systolic or diastolic blood pressure > 90th percentile. The primary outcome was survival to hospital discharge.
Results:
Of 102 children, 70 (68.6%) had at least one episode of immediate post-CPR diastolic hypertension. After controlling for pre-existing hypotension, duration of CPR, calcium administration, and first documented rhythm, patients with immediate post-CPR diastolic hypertension were more likely to survive to hospital discharge (79.3% vs. 54.5%; adjusted OR=2.93; 95%CI, 1.16–7.69).
Conclusions:
In this post hoc secondary analysis of the PICqCPR study, 68.6% of subjects had diastolic hypertension within 20 minutes of ROSC. Immediate post-ROSC hypertension was associated with increased odds of survival to discharge, even after adjusting for covariates of interest.
Keywords: cardiac arrest, child, hypotension, hypertension, hemodynamics, post cardiac arrest care
Introduction
Among the 5–10,000 children in the US who require in-hospital cardiopulmonary resuscitation (CPR) annually, >95% occur in an intensive care unit (ICU).1, 2 While approximately three quarters of children who receive CPR will survive the initial event with return of spontaneous circulation (ROSC), almost half will die in the hospital during the post-cardiac arrest period.3–5
The post cardiac arrest period is a vulnerable time characterized by myocardial dysfunction, a systemic ischemic-reperfusion response, brain injury and multi-organ dysfunction.6–8 Hypotension during the first 12 hours following ROSC is common and is associated with lower rates of survival to discharge and worse neurologic outcomes.9, 10 As a result of these studies, the American Heart Association Guidelines for pediatric post-resuscitation care recommend the use of intravenous fluids and vasoactive agents to maintain a systolic blood pressure > 5th percentile for age.11 Animal data suggest that hypertension immediately post-cardiac arrest (1–5 minutes after reperfusion) is associated with improved outcomes, presumably by re-establishing microcirculatory cerebral blood flow.12 However, to date no pediatric cardiac arrest studies have evaluated the association of immediate post-cardiac arrest blood pressure with outcomes.
The Pediatric Intensive Care Quality of CPR (PICqCPR) study, a prospective multicenter cohort study of pediatric intensive care unit (ICU) CPR established that patients with an intra-arrest diastolic blood pressure (DBP) ≥ 25 mm Hg during CPR in infants or ≥ 30 mm Hg in children ≥1 year old were 70% more likely to survive to hospital discharge and 60% more likely to survive with a favorable neurologic outcome.13 In this post hoc secondary analysis of the PICqCPR data, we aimed to evaluate the association of immediate (0–20 min) post-ROSC systolic and diastolic invasive arterial blood pressures with survival and neurologic outcomes at hospital discharge. We hypothesized that patients who had immediate post-CPR diastolic hypertension would have higher rates of survival to discharge and that those with immediate post-CPR systolic or diastolic hypotension would have lower rates of survival to discharge.
Methods
This study is a secondary analysis of data from the PICqCPR Study.13
PICqCPR Study
The PICqCPR Study was a prospective multicenter cohort study of ICU CPR conducted by the Collaborative Pediatric Critical Care Research Network (CPCCRN) from eleven institutions between July 1, 2013 and June 30, 2016. Children ≥37 weeks gestation and <19 years old who received chest compressions for ≥1 minute and invasive arterial blood pressure monitoring prior to and during CPR in a CPCCRN Pediatric ICU or Pediatric Cardiac ICU were eligible.
Inclusion criteria were patients with: 1) invasive arterial BP monitoring prior to and during CPR; 2) first compression of CPR captured on transmitted arterial BP waveform data; 3) at least one minute of continuous arterial BP waveforms; and 4) central venous pressure, respiratory plethysmography or ECG artifact available on transmitted arterial BP waveform data to allow determination of CPR starts and stops. Exclusion criteria were: 1) unable to determine DBP (e.g., lack of arterial waveform due to line interruption for blood draw or truncation of BP waveform obscuring DBP) or 2) unable to determine when CPR started and stopped. Only the index (first of admission) CPR event was evaluated for patients with more than one CPR event because a patient can only survive once per hospitalization.14
The CPCCRN research coordinators obtained Utstein-style standardized cardiac arrest and CPR data,144 including: 1) patient factors such as demographics, preexisting conditions, and illness categories; 2) arrest characteristics such as interventions in place at time of arrest, first documented rhythm, immediate cause of arrest, duration of CPR, defibrillation shocks, and pharmacologic intervention; and 3) outcome data such as ROSC >20 minutes, survival to hospital discharge and survival to hospital discharge with a favorable neurologic outcome. The primary study did not evaluate post-cardiac arrest care and therefore information regarding post-ROSC clinical data, including vasopressor infusions, pH, lactate and other clinical interventions were not available.
The primary outcome was survival to hospital discharge and the secondary outcome was survival to hospital discharge with a favorable neurologic outcome. Pediatric Cerebral Performance Category (PCPC) scores pre-arrest and at hospital discharge were documented. Survival to hospital discharge with a favorable neurologic outcome was defined as PCPC 1–3 or no worse than pre-arrest PCPC.14, 15
Waveform Analysis
Analysis of waveform data has been previously described.13 DBP was sampled during mid-diastole for each compression. Central venous pressure, left atrial pressure, ECG artifact and/or respiratory plethysmography tracings were used to determine start, stop and interruptions of CPR. Mean DBP was determined for each minute of CPR, and mean DBP for each patient was the average DBP over the first 10 minutes of CPR. For patients with <10 minutes of CPR, the mean systolic and diastolic BPs were determined for the minutes of CPR provided.
Post-ROSC Blood Pressure Study
All patients included in the PICqCPR study were eligible for this secondary study. Patients were excluded if they received extracorporeal membrane oxygenation CPR (E-CPR) or did not survive the cardiac arrest event (did not achieve ROSC). This study was exempted by The Children’s Hospital of Philadelphia Institutional Review Board.
Based on the PICqCPR study, intra-arrest targets were defined as a DBP < or ≥ 25 mm Hg during CPR in infants < 1 year of age and DBP < or ≥ 30 mm Hg during CPR in children ≥1 year old.13
Post-ROSC blood pressures were obtained every 5 minutes for the first 20 minutes following cessation of CPR. Hypotension was defined as a systolic blood pressure (SBP) or DBP less than the fifth percentile derived from normative data for age, sex and height based on previous literature.16 Hypertension was defined as a SBP or DBP greater than the ninetieth percentile derived from normative data for age, sex and height.16
Our primary exposures of interest were any documented immediate post-ROSC diastolic hypotension (DBP < 5th percentile), systolic hypotension (SBP < 5th percentile), diastolic hypertension (DBP> 90th percentile), and systolic hypertension (SBP > 90th percentile). Secondary exposures were 1) a four-level variable including intra-arrest DBP targets and immediate post-CPR diastolic hypertension (above DBP target and hypertension, above DBP target and no hypertension, below DBP target and hypertension, below DBP target and no hypertension) and 2) a four-level variable including intra-arrest DBP target and immediate post-CPR systolic hypertension (above DBP target and hypertension, above DBP target and no hypertension, below DBP target and hypertension, below DBP target and no hypertension). The primary outcome for this study was survival to hospital discharge and the secondary outcome was survival to hospital discharge with a favorable neurologic outcome.
Statistical Analysis
Patient and event characteristics were summarized using frequencies and percentages or median and quartiles. Differences in these characteristics between patients who did and did not survive to hospital discharge were examined using Fisher’s exact test for categorical variables, the Cochran-Armitage trend test for ordinal variables and the Wilcoxon rank-sum test for continuous variables. Bivariate associations of post-cardiac arrest hypertension, hypotension, and the four level interaction variables of intra-arrest DBP with the survival outcomes were examined using Fisher’s exact test. These relationships were further evaluated using multiple logistic regression adjusted for pre-existing hypotension, duration of CPR, calcium administration, and first documented rhythm. Covariates for multiple regression were selected a priori. P-values are reported based on a 2-sided alternative and considered statistically significant when <0.05. All analyses were completed using SAS software v9.4 (Cary, NC).
Results
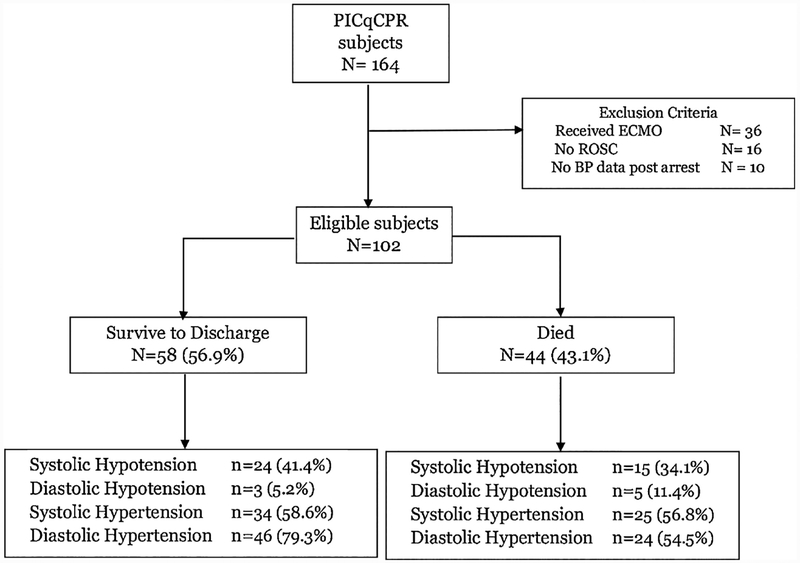
One hundred sixty four patients from PICqCPR were eligible. One hundred thirty five patients survived the event and had blood pressures recorded after ROSC; 33 patients were excluded because they received E-CPR. One hundred two patients were evaluable (Figure 1). Thirty nine (38.2%) had immediate post-CPR systolic hypotension; 59 (57.8%) had immediate post-CPR systolic hypertension; 8 (7.8%) had immediate post-CPR diastolic hypotension; and 70 (68.6%) had immediate post-CPR diastolic hypertension.
Figure 1:
CONSORT Diagram. This describes the percent of survivors and non-survivors of those were eligible for this study. Blood pressure groups by survival are described. ECMO: extracorporeal Membrane Oxygenation, PICqCPR: Pediatric Intensive Care Quality of CPR
Pre-arrest and arrest characteristics for the entire cohort are summarized by outcomes in Table 1. Patients who had a pre-existing condition of hypotension were less likely to survive to discharge (p=0.006) and less likely to have a favorable neurologic outcome (p=0.003) (Table 1). More patients with preexisting congenital heart disease survived to discharge with a favorable neurologic outcome (p=0.04). Non-survivors were more likely to receive intra-arrest calcium (p=0.025); however, no other intra-arrest factor was associated with outcome. There were no other differences between survival groups or neurologic outcome groups.
Table 1:
Demographic, event and post-CPR Characteristics by Survival to hospital discharge and survival to hospital discharge with favorable neurological outcome. BP: blood pressure, CPR: cardiopulmonary resuscitation, DBP: diastolic blood pressure
| Survival to Hospital Discharge | Survival to Hospital Discharge with Favorable Neurological Outcome | ||||||
|---|---|---|---|---|---|---|---|
| Overall (N = 102) | Yes (N = 58) | No (N = 44) | P-value | Yes (N = 53) | No (N = 49) | P-value | |
| Intra-arrest DBP | |||||||
| DBP above target (25 mmHg for infants, 30 mmHg for children) | 69 (67.6%) | 42 (72.4%) | 27 (61.4%) | 0.2871 | 37 (69.8%) | 32 (65.3%) | 0.6751 |
| Post-arrest Hypotension Indicators | |||||||
| Any systolic BP < 5th percentile | 39 (38.2%) | 24 (41.4%) | 15 (34.1%) | 0.5391 | 22 (41.5%) | 17 (34.7%) | 0.5431 |
| Any diastolic BP < 5th percentile | 8 (7.8%) | 3 (5.2%) | 5 (11.4%) | 0.2861 | 3 (5.7%) | 5 (10.2%) | 0.4761 |
| Post-arrest Hypertension Indicators | |||||||
| Any systolic BP > 90th percentile | 59 (57.8%) | 34 (58.6%) | 25 (56.8%) | 1.0001 | 32 (60.4%) | 27 (55.1%) | 0.6891 |
| Any diastolic BP > 90th percentile | 70 (68.6%) | 46 (79.3%) | 24 (54.5%) | 0.0101 | 41 (77.4%) | 29 (59.2%) | 0.0571 |
| Age (Months) | 9.0 [2.5, 43.5] | 8.0 [1.5, 33.5] | 12.0 [3.5, 50.0] | 0.2462 | 7.5 [1.5, 33.5] | 11.5 [3.5, 48.5] | 0.2182 |
| Age | 0.2241 | 0.2291 | |||||
| < 1 year | 59 (57.8%) | 37 (63.8%) | 22 (50.0%) | 34 (64.2%) | 25 (51.0%) | ||
| >= 1 year | 43 (42.2%) | 21 (36.2%) | 22 (50.0%) | 19 (35.8%) | 24 (49.0%) | ||
| Male | 59 (57.8%) | 35 (60.3%) | 24 (54.5%) | 0.6861 | 32 (60.4%) | 27 (55.1%) | 0.6891 |
| Ethnicity | 0.8211 | 0.9071 | |||||
| Hispanic or Latino | 14 (13.7%) | 8 (13.8%) | 6 (13.6%) | 8 (15.1%) | 6 (12.2%) | ||
| Not Hispanic or Latino | 72 (70.6%) | 42 (72.4%) | 30 (68.2%) | 37 (69.8%) | 35 (71.4%) | ||
| Unknown or Not Reported | 16 (15.7%) | 8 (13.8%) | 8 (18.2%) | 8 (15.1%) | 8 (16.3%) | ||
| Race | 0.3991 | 0.3001 | |||||
| White | 50 (49.0%) | 27 (46.6%) | 23 (52.3%) | 25 (47.2%) | 25 (51.0%) | ||
| Black or African American | 19 (18.6%) | 8 (13.8%) | 11 (25.0%) | 7 (13.2%) | 12 (24.5%) | ||
| Other | 7 (6.9%) | 5 (8.6%) | 2 (4.5%) | 5 (9.4%) | 2 (4.1%) | ||
| Unknown or Not Reported | 26 (25.5%) | 18 (31.0%) | 8 (18.2%) | 16 (30.2%) | 10 (20.4%) | ||
| Pre-existing conditions | |||||||
| Respiratory insufficiency | 84 (82.4%) | 46 (79.3%) | 38 (86.4%) | 0.4371 | 43 (81.1%) | 41 (83.7%) | 0.7991 |
| Hypotension | 76 (74.5%) | 37 (63.8%) | 39 (88.6%) | 0.0061 | 33 (62.3%) | 43 (87.8%) | 0.0031 |
| Congestive heart failure | 11 (10.8%) | 4 (6.9%) | 7 (15.9%) | 0.2001 | 4 (7.5%) | 7 (14.3%) | 0.3461 |
| Pneumonia | 12 (11.8%) | 7 (12.1%) | 5 (11.4%) | 1.0001 | 7 (13.2%) | 5 (10.2%) | 0.7621 |
| Sepsis | 24 (23.5%) | 14 (24.1%) | 10 (22.7%) | 1.0001 | 13 (24.5%) | 11 (22.4%) | 0.8201 |
| Trauma | 6 (5.9%) | 1 (1.7%) | 5 (11.4%) | 0.0821 | 1 (1.9%) | 5 (10.2%) | 0.1021 |
| Renal insufficiency | 11 (10.8%) | 6 (10.3%) | 5 (11.4%) | 1.0001 | 5 (9.4%) | 6 (12.2%) | 0.7541 |
| Malignancy | 3 (2.9%) | 1 (1.7%) | 2 (4.5%) | 0.5761 | 1 (1.9%) | 2 (4.1%) | 0.6071 |
| Congenital heart disease | 65 (63.7%) | 41 (70.7%) | 24 (54.5%) | 0.1021 | 39 (73.6%) | 26 (53.1%) | 0.0401 |
| Illness Category | 0.7751 | 0.6601 | |||||
| Surgical cardiac | 54 (52.9%) | 33 (56.9%) | 21 (47.7%) | 31 (58.5%) | 23 (46.9%) | ||
| Medical cardiac | 13 (12.7%) | 7 (12.1%) | 6 (13.6%) | 7 (13.2%) | 6 (12.2%) | ||
| Surgical non-cardiac | 8 (7.8%) | 4 (6.9%) | 4 (9.1%) | 3 (5.7%) | 5 (10.2%) | ||
| Medical non-cardiac | 26 (25.5%) | 13 (22.4%) | 13 (29.5%) | 12 (22.6%) | 14 (28.6%) | ||
| Unknown | 1 (1.0%) | 1 (1.7%) | 0 (0.0%) | 0 (0.0%) | 1 (2.0%) | ||
| Baseline Pediatric Cerebral Performance Category | 0.0983 | 0.0903 | |||||
| 1 - Normal | 44 (43.1%) | 26 (44.8%) | 18 (40.9%) | 25 (47.2%) | 19 (38.8%) | ||
| 2 - Mild disability | 32 (31.4%) | 20 (34.5%) | 12 (27.3%) | 17 (32.1%) | 15 (30.6%) | ||
| 3 - Moderate disability | 16 (15.7%) | 10 (17.2%) | 6 (13.6%) | 9 (17.0%) | 7 (14.3%) | ||
| 4 - Severe disability | 8 (7.8%) | 2 (3.4%) | 6 (13.6%) | 2 (3.8%) | 6 (12.2%) | ||
| 5 - Coma/vegetative state | 2 (2.0%) | 0 (0.0%) | 2 (4.5%) | 0 (0.0%) | 2 (4.1%) | ||
| Baseline functional status scale | 8.0 [6.0, 11.0] | 8.0 [6.0, 10.0] | 7.5 [6.0, 11.5] | 0.9312 | 8.0 [6.0, 10.0] | 8.0 [6.0, 11.0] | 0.6572 |
| Immediate Cause | |||||||
| Hypotension | 67 (65.7%) | 35 (60.3%) | 32 (72.7%) | 0.2131 | 33 (62.3%) | 34 (69.4%) | 0.5331 |
| Arrhythmia | 16 (15.7%) | 11 (19.0%) | 5 (11.4%) | 0.4121 | 10 (18.9%) | 6 (12.2%) | 0.4221 |
| Respiratory decompensation | 46 (45.1%) | 26 (44.8%) | 20 (45.5%) | 1.0001 | 23 (43.4%) | 23 (46.9%) | 0.8421 |
| Cyanosis without respiratory decompensation | 1 (1.0%) | 1 (1.7%) | 0 (0.0%) | 1.0001 | 1 (1.9%) | 0 (0.0%) | 1.0001 |
| First documented rhythm at time CPR initiated (Collapsed) | 0.1261 | 0.2731 | |||||
| Asystole/PEA | 32 (31.4%) | 14 (24.1%) | 18 (40.9%) | 13 (24.5%) | 19 (38.8%) | ||
| VF/VT | 7 (6.9%) | 3 (5.2%) | 4 (9.1%) | 3 (5.7%) | 4 (8.2%) | ||
| Bradycardia with poor perfusion | 59 (57.8%) | 38 (65.5%) | 21 (47.7%) | 34 (64.2%) | 25 (51.0%) | ||
| Unknown | 4 (3.9%) | 3 (5.2%) | 1 (2.3%) | 3 (5.7%) | 1 (2.0%) | ||
| Location of CPR Event | 0.1541 | 0.1571 | |||||
| PICU | 40 (39.2%) | 19 (32.8%) | 21 (47.7%) | 17 (32.1%) | 23 (46.9%) | ||
| CICU | 62 (60.8%) | 39 (67.2%) | 23 (52.3%) | 36 (67.9%) | 26 (53.1%) | ||
| Duration of CPR (minutes) | 5.0 [2.0, 11.0] | 4.0 [2.0, 10.0] | 7.0 [3.0, 14.5] | 0.0942 | 4.0 [2.0, 10.0] | 6.0 [3.0, 13.0] | 0.2572 |
| Duration of CPR (minutes) | 0.1481 | 0.4361 | |||||
| 1–5 | 57 (55.9%) | 37 (63.8%) | 20 (45.5%) | 33 (62.3%) | 24 (49.0%) | ||
| 6–15 | 30 (29.4%) | 16 (27.6%) | 14 (31.8%) | 15 (28.3%) | 15 (30.6%) | ||
| 16–35 | 12 (11.8%) | 4 (6.9%) | 8 (18.2%) | 4 (7.5%) | 8 (16.3%) | ||
| >35 | 3 (2.9%) | 1 (1.7%) | 2 (4.5%) | 1 (1.9%) | 2 (4.1%) | ||
| Interventions in place | |||||||
| Vascular access | 94 (92.2%) | 53 (91.4%) | 41 (93.2%) | 1.0001 | 48 (90.6%) | 46 (93.9%) | 0.7171 |
| Arterial catheter | 101 (99.0%) | 57 (98.3%) | 44 (100.0%) | 1.0001 | 52 (98.1%) | 49 (100.0%) | 1.0001 |
| Central venous catheter | 90 (88.2%) | 51 (87.9%) | 39 (88.6%) | 1.0001 | 46 (86.8%) | 44 (89.8%) | 0.7621 |
| Vasoactive infusion | 77 (75.5%) | 40 (69.0%) | 37 (84.1%) | 0.1041 | 37 (69.8%) | 40 (81.6%) | 0.1771 |
| Invasive mechanical ventilation | 86 (84.3%) | 46 (79.3%) | 40 (90.9%) | 0.1691 | 42 (79.2%) | 44 (89.8%) | 0.1781 |
| ETCO2 monitoring | 53 (52.0%) | 31 (53.4%) | 22 (50.0%) | 0.8421 | 30 (56.6%) | 23 (46.9%) | 0.4281 |
| Non-invasive ventilation | 11 (10.8%) | 8 (13.8%) | 3 (6.8%) | 0.3431 | 7 (13.2%) | 4 (8.2%) | 0.5291 |
| Pharmacologic interventions | |||||||
| Epinephrine | 86 (84.3%) | 49 (84.5%) | 37 (84.1%) | 1.0001 | 44 (83.0%) | 42 (85.7%) | 0.7891 |
| # of doses (when used) | 2.0 [1.0, 3.0] | 1.0 [1.0, 3.0] | 2.0 [1.0, 4.0] | 0.0612 | 1.0 [1.0, 3.0] | 2.0 [1.0, 4.0] | 0.0422 |
| Calcium | 42 (41.2%) | 18 (31.0%) | 24 (54.5%) | 0.0251 | 17 (32.1%) | 25 (51.0%) | 0.0701 |
| Sodium bicarbonate | 47 (46.1%) | 24 (41.4%) | 23 (52.3%) | 0.3191 | 22 (41.5%) | 25 (51.0%) | 0.4271 |
| Vasopressin | 5 (4.9%) | 3 (5.2%) | 2 (4.5%) | 1.0001 | 2 (3.8%) | 3 (6.1%) | 0.6691 |
Fisher’s exact test.
Wilcoxon rank-sum test.
Cochran-Armitage trend test.
More patients who survived to discharge had immediate post-CPR diastolic hypertension compared to non-survivors (46/58 [79.3%] vs 24/44 [54.45%]; p=0.01), as noted in Table 1. Immediate post-ROSC systolic hypotension, diastolic hypotension, and systolic hypertension were not associated with survival to discharge. Patients who survived to discharge were more likely to have met their intra-arrest DBP target and have post-ROSC diastolic hypertension than non-survivors (63.8% vs 31.8%; p =0.006), as noted in Table 2. None of the immediate post-ROSC blood pressure groups were associated with survival to discharge with a favorable neurologic outcome. There was no association between intra-arrest DBP category and post-CPR SBP or DBP category.
Table 2:
Intra-arrest Diastolic Blood Pressure and Post-CPR BP indicators by Survival and Neurologic Outcomes. DBP: diastolic blood pressure
| Survival to Hospital Discharge | Survival to Hospital Discharge with Favorable Neurological Outcome | |||||
|---|---|---|---|---|---|---|
| Yes (N = 58) | No (N = 44) | P-value | Yes (N = 53) | No (N = 49) | P-value | |
| Intra-arrest DBP Target and Post-arrest Systolic Hypertension | 0.0651 | 0.0511 | ||||
| Above DBP target and hypertension | 28 (48.3%) | 13 (29.5%) | 26 (49.1%) | 15 (30.6%) | ||
| Above DBP target and no hypertension | 14 (24.1%) | 14 (31.8%) | 11 (20.8%) | 17 (34.7%) | ||
| Below DBP target and hypertension | 6 (10.3%) | 12 (27.3%) | 6 (11.3%) | 12 (24.5%) | ||
| Below DBP target and no hypertension | 10 (17.2%) | 5 (11.4%) | 10 (18.9%) | 5 (10.2%) | ||
| Intra-arrest DBP Target and Post-arrest Diastolic Hypertension | 0.0061 | 0.0791 | ||||
| Above DBP target and hypertension | 37 (63.8%) | 14 (31.8%) | 32 (60.4%) | 19 (38.8%) | ||
| Above DBP target and no hypertension | 5 (8.6%) | 13 (29.5%) | 5 (9.4%) | 13 (26.5%) | ||
| Below DBP target and hypertension | 9 (15.5%) | 10 (22.7%) | 9 (17.0%) | 10 (20.4%) | ||
| Below DBP target and no hypertension | 7 (12.1%) | 7 (15.9%) | 7 (13.2%) | 7 (14.3%) | ||
After adjusting for pre-arrest hypotension, duration of CPR (minutes), intra-arrest calcium administration, and first documented rhythm, patients with immediate post-CPR diastolic hypertension had a 2.93 (95% CI [confidence interval]: 1.16, 7.69) higher odds of survival to discharge than those without diastolic hypertension (Table 3). After adjusting for the same covariates, patients with intra-arrest DBP above target and post-ROSC diastolic hypertension had a higher odds of survival to discharge than the other intra-arrest and immediate post-ROSC blood pressure groups (p=0.013), as noted in Table 3. Patients who survived to discharge with favorable neurologic outcome were more likely have intra-arrest DBP above target and immediate post-ROSC systolic hypertension than those who did not (49.1% vs 30.6%; p =0.051), as noted in Table 2, although this association was not demonstrable by multivariable analysis. (Table 3)
Table 3:
Multivariable models of Survival and Neurologic Outcomes. CI: confidence interval, CPR: cardiopulmonary resuscitation, DBP: diastolic blood pressure
| Survival to hospital discharge | Survival to Hospital Discharge with favorable neurologic outcome | |||
|---|---|---|---|---|
| Adjusted Odds ratio (95% CI) | P-value | Adjusted Odds ratio (95% CI) | P-value | |
| Immediate post-CPR DBP > 90th percentile | 0.023 | 0.119 | ||
| No | Reference | Reference | ||
| Yes | 2.93 (1.16, 7.69) | 2.06 (0.83, 5.26) | ||
| Intra-arrest DBP Target and Post-CPR Systolic Hypertension | 0.135 | 0.110 | ||
| Above DBP target and hypertension | Reference | Reference | ||
| Above DBP target and no hypertension | 0.64 (0.21, 1.89) | 0.50 (0.17, 1.44) | ||
| Below DBP target and hypertension | 0.30 (0.08, 1.05) | 0.42 (0.11, 1.45) | ||
| Below DBP target and no hypertension | 1.56 (0.40, 6.55) | 1.98 (0.53, 8.15) | ||
| Intra-arrest DBP Target and Post-CPR Diastolic Hypertension | 0.013 | 0.104 | ||
| Above DBP target and hypertension | Reference | Reference | ||
| Above DBP target and no hypertension | 0.12 (0.03, 0.45) | 0.21 (0.05, 0.74) | ||
| Below DBP target and hypertension | 0.41 (0.12, 1.34) | 0.73 (0.23, 2.29) | ||
| Below DBP target and no hypertension | 0.53 (0.14, 1.92) | 0.92 (0.26, 3.28) | ||
Results are based on multivariable model(s) adjusting for Hypotension, Duration of CPR (minutes), Calcium, and First documented rhythm.
Discussion
These PICqCPR data demonstrate that immediate post-ROSC diastolic hypertension (>90th percentile) is associated with increased survival to hospital discharge following pediatric in-hospital ICU cardiac arrest. These findings are consistent with large animal laboratory experimental data.12 Furthermore, patients with intra-arrest DBP above target and immediate post-ROSC diastolic hypertension were more likely to survive to discharge compared to patients without intra-arrest DBP above target or without post-ROSC diastolic hypertension. Immediate post-ROSC systolic hypotension and diastolic hypotension occurred only in 38% and 8% of these patients, respectively, and neither was associated with poor outcomes.
Hemodynamics during the first 20 minutes after cessation of CPR have not been well described in clinical pediatric cardiac arrest studies. In this PICqCPR cohort, diastolic hypertension following CPR occurred in 69% of patients, and was independently associated with survival to discharge. Abundant animal data have established that survival from cardiac arrest is dependent on adequate myocardial blood flow during CPR, and the primary determinant of myocardial blood flow during CPR is arterial diastolic pressure because myocardial blood flow occurs during the relaxation phase of CPR.17, 18 An experimental study of ventricular fibrillation cardiac arrest with controlled reperfusion demonstrated that dogs treated with norepinephrine to induce hypertension in the first 5 minutes following reperfusion had improved histopathologic and functional outcomes compared to those treated with normotension.12 The investigators’ premise was that immediate post-ROSC hypertension would more effectively re-establish microcirculatory cerebral blood flow. The driving force for post-ROSC cerebral blood flow is the cerebral perfusion pressure, or mean arterial pressure minus central venous pressure (or minus intracranial pressure if that is higher than central venous pressure). Because arterial diastolic pressure is a greater contributor to mean arterial pressure than the systolic pressure, it is not surprising that immediate post-ROSC diastolic pressure was associated with improved outcomes in our cohort rather than systolic hypertension.
In this small cohort of patients we did not see an association between intra-arrest DBP targets and post-arrest blood pressure categories. It is well known that prolonged CPR duration, more doses of epinephrine, unwitnessed events and lack of bystander CPR are associated with worse post-ROSC hemodynamics, although such studies have not evaluated immediate post-ROSC hemodynamics.9, 10 Associations with these intra-arrest factors are presumed to be due to severe tissue hypoxia and hypoperfusion. The lack of association between the intra-arrest DBP targets and post-ROSC blood pressure may be due to small sample size, the categorical approach to blood pressure groups used because of this small sample size or perhaps the immediate post resuscitation time period being too early to have unveiled the severity of injury’s impact on hemodynamics.
Immediate post-ROSC systolic hypotension occurred in 38% of patients consistent with previous studies evaluating early post-ROSC hypotension. For example, in one study of pediatric in-hospital and out-of-hospital cardiac arrests more than 50% of patients had an SBP less than the 5th percentile during the first 6 hours following ROSC.9 Similarly, a secondary study of the Therapeutic Hypothermia After Pediatric Cardiac Arrest trial of targeted temperature management for out-of-hospital cardiac arrests demonstrated the more than 25% of patients had systolic hypotension <5th percentile during the 6–12 hours following CPR.10 The lack of association of immediate post-ROSC systolic or diastolic hypotension in this study as compared to early hypotension in other studies, may be due to the differences in physiology immediately post-ROSC, including the effects of residual intravenous epinephrine administered during the resuscitation, or being too early to have reached the full effect of post-cardiac arrest myocardial dysfunction that impacts blood pressure most prominently at 4–24 hour following ROSC.19, 20 Most pediatric in-hospital cardiac arrests are now occurring within pediatric intensive care units, and 40% of these patient have arterial lines during CPR.2 Previous investigations provide data to support the use of continuous intra-arterial pressure monitoring for: 1) titration of CPR performance to hemodynamic effect (e.g., targeting to a diastolic pressure response13, 21 and 2) titration of hemodynamic supportive care to avoid post-resuscitation hypotension.11 The data from this PICqCPR study suggest that the immediate post-ROSC diastolic pressure may be an additional target to consider in our quest to improve outcomes following in-hospital cardiac arrests. However, it is unclear whether spontaneous hypertension after cardiac arrest might have a different effect on outcomes than hypertension induced by vasopressors.
This study had several limitations. First, the observational nature of the study design precludes determination of causality. Perhaps the immediate post-ROSC diastolic hypertension was associated with other factors that were in the causal pathway to better outcomes. Therefore, it is premature to conclude that intensivists should target high diastolic blood pressures immediately following ROSC. Nevertheless, these data suggest that immediate post-ROSC hemodynamics is a rich area for further investigation. Second, the power of these statistical analyses were limited by the small sample size. Some of the adjusted odds ratios suggested impressive associations of other post-ROSC hemodynamic groupings with survival outcomes, yet the 95% confidence intervals crossed 1.0 perhaps in part due to the small sample size. Third, there was limited information available regarding post-ROSC clinical data, including vasopressor infusions, pH, lactate and other clinical interventions. We excluded E-CPR patients since we were evaluating SBP and DBP, and most if not all of these patients would have non-pulsatile flow. Therefore, these findings are not generalizable to E-CPR patients. Finally, the CPCCRN sites are all large academic pediatric ICUs, and the quality of care provided before and after cardiac arrests may have differed from other institutions.
Conclusions:
These PICqCPR data demonstrate that diastolic hypertension (>90th percentile) within the first 20 minutes following ROSC is associated with increased survival to hospital discharge following pediatric in-hospital ICU cardiac arrests. Further study is necessary to confirm these findings, elucidate the potential physiologic mechanisms underlying these findings, and evaluate potential clinical interventions that may improve outcomes.
Acknowledgements
This study was supported, in part, by the following cooperative agreements from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, NIH, Department of Health and Human Services: UG1HD050096, UG1HD049981, UG1HD049983, UG1HD063108, UG1HD083171, UG1HD083166, UG1HD083170, U10HD050012, U10HD063106, U10HD063114 and U01HD049934.
Appendix A
The Eunice Kennedy Shriver National Institute of Child Health and Human Development Collaborative Pediatric Critical Care Research Network (CPCCRN) Investigators comprise:
Athena F. Zuppaa, Katherine Grahama, Carolann Twelvesa, Mary Ann Dilibertoa, William P. Landisa, Elyse Tomaniob, Jeni Kwokc, Michael J. Bellb,d, Alan Abrahamc, Anil Sapruc,e, Mustafa F. Alkhoulie, Sabrina Heidemannf, Ann Pawluszkaf, Mark W. Hallg, Lisa Steeleg, Thomas P. Shanleyh,i, Monica Weberh, Heidi J. Daltonj, Aimee La Bellj, Peter M. Mouranik, Kathryn Malonek, Christopher Locandrol, Whitney Colemanl, Alecia Petersonl, Julie Thelenl, Allan Doctorm
a Department of Anesthesiology and Critical Care Medicine, The Children’s Hospital of Philadelphia, University of Pennsylvania, Philadelphia, PA, United States
b Department of Pediatrics, Children’s National Medical Center, Washington D.C., United States
c Department of Anesthesiology and Critical Care Medicine, Children’s Hospital Los Angeles, University of Southern California Keck School of Medicine, Los Angeles, CA, United States
d Department of Critical Care Medicine, Children’s Hospital of Pittsburgh, University of Pittsburgh, Pittsburgh, PA, United States
e Department of Pediatrics, Benioff Children’s Hospital, University of California San Francisco, San Francisco, CA, United States
f Department of Pediatrics, Children’s Hospital of Michigan, Wayne State University, Detroit, MI, United States
g Department of Pediatrics, Nationwide Children’s Hospital, The Ohio State University, Columbus, OH, United States
h Department of Pediatrics, C.S. Mott Children’s Hospital, University of Michigan, MI, United States
i Department of Pediatrics, Lurie Children’s Hospital, Northwestern University, Chicago, IL, United States
j Department of Pediatrics, Phoenix Children’s Hospital, Phoenix, AZ, United States
k Department of Pediatrics, Denver Children’s Hospital, University of Colorado, Denver, CO, United States
l Department of Pediatrics, University of Utah, Salt Lake City, Utah, United States
m Department of Pediatrics, Washington University School of Medicine, St. Louis, MO, United States
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of Interest: The authors have no conflicts on interest.
References
- 1.Topjian AA, Berg RA and Nadkarni VM. Pediatric cardiopulmonary resuscitation: advances in science, techniques, and outcomes. Pediatrics 2008;122:1086–98 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Berg RA, Sutton RM, Holubkov R, et al. Ratio of PICU versus ward cardiopulmonary resuscitation events is increasing. Crit Care Med 2013;41:2292–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Moler FW, Silverstein FS, Holubkov R, et al. Therapeutic Hypothermia after In-Hospital Cardiac Arrest in Children. N Engl J Med 2017;376:318–329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Meert KL, Donaldson A, Nadkarni V, et al. Multicenter cohort study of in-hospital pediatric cardiac arrest. Pediatr Crit Care Med 2009;10:544–53 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Berg RA, Nadkarni VM, Clark AE, et al. Incidence and Outcomes of Cardiopulmonary Resuscitation in PICUs. Crit Care Med 2016;44:798–808 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Neumar RW, Nolan JP, Adrie C, et al. Post-cardiac arrest syndrome: epidemiology, pathophysiology, treatment, and prognostication. A consensus statement from the International Liaison Committee on Resuscitation (American Heart Association, Australian and New Zealand Council on Resuscitation, European Resuscitation Council, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Council of Asia, and the Resuscitation Council of Southern Africa); the American Heart Association Emergency Cardiovascular Care Committee; the Council on Cardiovascular Surgery and Anesthesia; the Council on Cardiopulmonary, Perioperative, and Critical Care; the Council on Clinical Cardiology; and the Stroke Council. Circulation 2008;118:2452–83 [DOI] [PubMed] [Google Scholar]
- 7.Kern KB, Hilwig RW, Berg RA, et al. Postresuscitation left ventricular systolic and diastolic dysfunction. Treatment with dobutamine. Circulation 1997;95:2610–3 [DOI] [PubMed] [Google Scholar]
- 8.Kern KB, Hilwig RW, Rhee KH and Berg RA. Myocardial dysfunction after resuscitation from cardiac arrest: an example of global myocardial stunning. J Am Coll Cardiol 1996;28:232–40 [DOI] [PubMed] [Google Scholar]
- 9.Topjian AA, French B, Sutton RM, et al. Early postresuscitation hypotension is associated with increased mortality following pediatric cardiac arrest. Crit Care Med 2014;42:1518–23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Topjian AA, Telford R, Holubkov R, et al. Association of Early Postresuscitation Hypotension With Survival to Discharge After Targeted Temperature Management for Pediatric Out-of-Hospital Cardiac Arrest: Secondary Analysis of a Randomized Clinical Trial. JAMA Pediatr 2018;172:143–153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.de Caen AR, Berg MD, Chameides L, et al. Part 12: Pediatric Advanced Life Support: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2015;132:S526–42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sterz F, Leonov Y, Safar P, Radovsky A, Tisherman SA and Oku K Hypertension with or without hemodilution after cardiac arrest in dogs. Stroke 1990;21:1178–1184 [DOI] [PubMed] [Google Scholar]
- 13.Berg RA, Sutton RM, Reeder RW, et al. Association Between Diastolic Blood Pressure During Pediatric In-Hospital Cardiopulmonary Resuscitation and Survival. Circulation 2018;137:1784–1795 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jacobs I, Nadkarni V, Bahr J, et al. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update and simplification of the Utstein templates for resuscitation registries: a statement for healthcare professionals from a task force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian Resuscitation Council, New Zealand Resuscitation Council, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Councils of Southern Africa). Circulation 2004;110:3385–97 [DOI] [PubMed] [Google Scholar]
- 15.Becker LB, Aufderheide TP, Geocadin RG, et al. Primary outcomes for resuscitation science studies: a consensus statement from the American Heart Association. Circulation 2011;124:2158–77 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rosner B, Cook N, Portman R, Daniels S and Falkner B Determination of blood pressure percentiles in normal-weight children: some methodological issues. Am J Epidemiol 2008;167:653–66 [DOI] [PubMed] [Google Scholar]
- 17.Kern KB, Ewy GA, Voorhees WD, Babbs CF and Tacker WA. Myocardial perfusion pressure: a predictor of 24-hour survival during prolonged cardiac arrest in dogs. Resuscitation 1988;16:241–50 [DOI] [PubMed] [Google Scholar]
- 18.Paradis NA, Martin GB, Rivers EP, et al. Coronary perfusion pressure and the return of spontaneous circulation in human cardiopulmonary resuscitation. JAMA 1990;263:1106–1113 [PubMed] [Google Scholar]
- 19.Adrie C, Adib-Conquy M, Laurent I, et al. Successful cardiopulmonary resuscitation after cardiac arrest as a “sepsis-like” syndrome. Circulation 2002;106:562–8 [DOI] [PubMed] [Google Scholar]
- 20.Laurent I, Monchi M, Chiche JD, et al. Reversible myocardial dysfunction in survivors of out-of-hospital cardiac arrest. J Am Coll Cardiol 2002;40:2110–2116 [DOI] [PubMed] [Google Scholar]
- 21.Meaney PA, Bobrow BJ, Mancini ME, et al. Cardiopulmonary resuscitation quality: [corrected] improving cardiac resuscitation outcomes both inside and outside the hospital: a consensus statement from the American Heart Association. Circulation 2013;128:417–35 [DOI] [PubMed] [Google Scholar]