Abstract
Background:
Anxiety, which is very prevalent in multiple sclerosis (MS) but understudied, has been shown to negatively affect cognition in many different populations. Slowed information processing speed underlies most cognitive impairments in MS, including verbal learning. The aim of this study was to look at how anxiety influences cognition—specifically processing speed and verbal learning—in MS.
Methods:
Eligibility criteria were adults (≥18 years) who had a diagnosis of clinically definite MS and had participated in neuropsychological research projects. A retrospective medical record review was conducted on the neuropsychological testing data. Two hierarchical multiple regressions were conducted to determine the unique contributions of processing speed and anxiety on verbal learning in MS, after adjusting for demographic and disability variables. Two separate mediation analyses were conducted to determine the relationship between processing speed, verbal learning, and anxiety.
Results:
Participants (N = 141) ranged in age from 18–91 years. Based on the multiple regression analyses, processing speed (β = 0.55, ΔR2 = 0.27, P < .001) and anxiety (β = −0.34, ΔR2 = 0.11, P < .001) were uniquely significant predictors of verbal learning. Based on the mediation analyses, there was a significant indirect effect of anxiety on verbal learning through processing speed (ab = −0.31, 95% CI = −0.60 to −0.09). There was also a significant indirect effect of processing speed on verbal learning through anxiety (ab = −0.05, 95% CI = 0.01 to 0.12).
Conclusions:
Results suggest a bidirectional relationship of anxiety and processing speed on verbal learning in MS. Anxiety has a significant effect on cognition and should not be overlooked. Interventions targeting anxiety may improve cognition in MS.
Keywords: Anxiety, Cognition, Multiple sclerosis (MS), Processing speed, Verbal learning
Multiple sclerosis (MS) is a neurodegenerative and inflammatory chronic disease of unknown etiology that affects the central nervous system and is characterized by substantial effects on physical, cognitive, and psychological functioning.1,2 Anxiety, a form of emotional distress that can have a negative effect on cognition,3,4 is prevalent in MS, yet it is understudied.5,6 The point prevalence rates of clinically significant anxiety in MS usually range from 30% to 50%, whereas the lifetime prevalence rates of anxiety disorders in MS have usually ranged from 14% to 41%, well above the rates of the general population as well as those of many other medical populations.7–10 According to attentional control theory, anxiety negatively affects cognition by increasing the influence of less-efficient, stimulus-driven, bottom-up processes over more-efficient, goal-oriented, top-down processes.11 Bottom-up processes are less efficient because they are controlled by basic sensory systems, and time is needed for the brain to piece together the various sensory stimuli. Bottom-up processes are also highly influenced by distractors in the environment, which interrupts goal-oriented cognitive processing. Top-down processes are more efficient because they are controlled by previous knowledge, mental heuristics, and context and, thus, require less effortful neural processing. Top-down processing is also more goal-oriented and less susceptible to distractors. Anxiety increases awareness of task-irrelevant stimuli that is usually threat-related, which thus interferes with the task at hand and negatively influences cognition.12 Several studies have demonstrated the negative impact of anxiety on cognition in MS.13–15 Specifically, anxiety may interfere with certain areas of executive functioning,13 visual memory,14 and information processing speed.16,17
Information processing speed is one of the primary cognitive deficits in MS and likely underlies deficits in other cognitive domains.18,19 For example, processing speed likely underlies working memory impairments in the disease because slower speed interferes with the acquisition of new information.18 Processing speed impairments also seem to be independent of motor issues.20,21
Verbal learning and memory are additional cognitive domains commonly impaired in MS22 that are often predictive of disease status.23 Several studies suggest that information processing speed is related to verbal memory impairments in MS by interfering with the encoding of verbal information, which is related to verbal learning.24–26 Demyelination in certain white matter tracts interferes with processing speed as well as encoding efficiency. New verbal information is often not processed quickly enough to adequately encode and learn the information. Verbal learning impairments are usually more pronounced in progressive stages of MS, where demyelination is more severe, which provides further support for the hypothesis that demyelination affects processing speed, which then negatively affects encoding of verbal information.25 Anxiety may also be playing a significant role in this relationship between processing speed and verbal learning.
Only a few studies have examined the relationship between verbal learning and memory and anxiety in MS populations, and they have yielded mixed results. Specifically, two studies found no correlations between measures of anxiety and verbal learning and memory,13,14 and another study found a significant negative relationship between state anxiety and delayed recall of a story learning task.27 Several studies conducted in non-MS populations have found significant negative relationships between anxiety and verbal learning and memory.3,28–30 Previous studies examining the relationships between anxiety and verbal learning and memory in MS have yielded mixed results, likely because they have not adjusted for disease or demographic variables in their analyses, which may be confounding these results. However, the relationship between anxiety and processing speed in MS seems to be more clear; several studies have found anxiety to be correlated with processing speed impairments in MS.16,17
To our knowledge, the present study is the first to look at the relationships between processing speed, verbal learning, and anxiety in MS. The aim of this study was to determine the role that anxiety plays in cognition in MS by separately examining the relationships between a measure of processing speed and verbal learning and between a measure of anxiety and verbal learning. Finally, a mediation analysis looking at the relationship between processing speed and verbal learning via anxiety in MS was conducted. Contrary to most previous studies looking at the relationships between these variables, this study adjusted for demographic and disease factors in the analyses. Based on previous research, we predicted that there would be a linear positive relationship between processing speed and verbal learning in MS. Because there has been a well-established relationship between anxiety and verbal learning and memory in non-MS populations,3,28–30 as well as between anxiety and other cognitive domains in MS,13,14 we predicted that after adjusting for demographic and disease variables there would be a linear negative relationship between anxiety and verbal learning in MS. Consistent with attentional control theory, we also predicted that anxiety would affect processing speed, which would, in turn, affect verbal learning.
Methods
Participants
Eligible participants were aged 18 years or older, had a diagnosis of clinically definite MS, were patients at Holy Name Medical Center in Teaneck, New Jersey, and were recruited for neuropsychological research projects. No patients were experiencing clinical exacerbations or were taking high-dose corticosteroids, that is, corticosteroids administered intravenously, such as methylprednisolone, at the time of testing.
Procedures
All the participants signed an informed consent form to participate in the research. The institutional review board at Albert Einstein College of Medicine (Bronx, NY) approved this study. Participants were administered neuropsychological tests using standard administration protocols. Participants also completed self-report measures and a disease-specific measure of disability.
Measures
California Verbal Learning Test, Second Edition
The California Verbal Learning Test, Second Edition (CVLT-II)31 is a test of verbal learning and memory. A list of 16 words is read to the participant at a rate of one word per second. The CVLT-II has been shown to be a reliable and valid measure of verbal learning and memory in MS.32 For the purposes of this study, only the total immediate recall score, which is the sum of the number of words correctly recalled on trials 1 through 5, was used in the analyses. Total immediate recall on the CVLT-II is related to initial learning and encoding of verbal information and has been found to be the critical aspect of verbal memory problems in MS.24
Symbol Digit Modalities Test–Oral Form
The standard and most widely used version of the Symbol Digit Modalities Test (SDMT) was used. The oral version of the SDMT has been found to be a sensitive measure of processing speed in MS.33,34 The score is the total number of accurate symbol-digit pairings completed in the allotted 90 seconds.
Hospital Anxiety and Depression Scale
The Hospital Anxiety and Depression Scale (HADS)35 is a 14-item measure designed for use in medically ill patients that alternates questions about anxiety and depression. The HADS items are multiple choice (0–3 Likert scale). A validation study of the HADS for use with patients with MS determined that cutoff scores of 8 or greater yielded the appropriate sensitivity and specificity for determining clinically significant anxiety and depression symptoms in MS.36 For the purposes of this study, only the anxiety subscale was used in the analyses.
Timed 25-Foot Walk Test
During the Timed 25-Foot Walk test,37 the participant is asked to walk a clearly marked 25-foot course as quickly and as safely as possible. Assistive walking devices may be used. Two trials of this task are administered. In this study, the average of these two trials was used in the analyses. This task has been shown to be an effective way to measure walking disability in MS.38
Data Analysis
A retrospective medical record review was conducted on the neuropsychological assessment data. All the data analyses were run using IBM SPSS Statistics for Windows, version 22.0 (IBM Corp, Armonk, NY). Hierarchical multiple regressions were conducted to examine the ability of a measure of processing speed to predict scores on a measure of verbal learning, and how self-reported anxiety predicts verbal learning after adjusting for demographic and MS-specific disability factors. The Process Macro39 was used to first conduct a mediation analysis looking at the mediational role of processing speed on the relationship between anxiety and verbal learning in MS. A second mediation analysis was then performed looking at the meditational role of anxiety on the relationship between processing speed and verbal learning in MS. Demographic and disease factors were also adjusted for in these analyses. Because T scores were used in place of raw scores, age did not need to be separately adjusted for in the analyses.
Results
Study Participants
The participants were 141 adult patients who met the eligibility criteria. See Table 1 for more information about demographic variables.
Table 1.
Demographic characteristics of the 141 study participants
| Variable | Value |
|---|---|
| Sex | |
| Female | 109 (77.3) |
| Male | 32 (22.7) |
| Marital statusa | |
| Married | 85 (60.3) |
| Unmarriedb | 53 (37.7) |
| Race/ethnicitya | |
| White | 96 (68.1) |
| Black | 14 (9.9) |
| Hispanic | 18 (12.8) |
| Other/not reported | 10 (7.1) |
| Age (n = 140), y | 48.7 ± 11.9 (18–81) |
| Education (n = 141), y | 14.7 ± 3.1 (9–41) |
Note: Values are given as number (percentage) or mean ± SD (range).
aMarital status and race/ethnicity data were missing for 3 participants.
bDivorced, 13.5%; never married (single or engaged), 19.9%; widowed, 4.3%.
Preliminary and Mediation Analyses
Preliminary analyses were conducted to ensure that there were no violations of the assumptions of normality, linearity, multicollinearity, and homoscedasticity. The first regression determined the effect of processing speed on verbal learning. Years of education and sex were entered in the first step. Walking speed, as a measure of disability, was entered in step 2. The SDMT total score was entered in step 3 as a measure of processing speed. The CVLT-II total score (trials 1-5) was the measure of verbal learning and served as the primary outcome. Processing speed was a uniquely significant predictor of verbal learning (β = 0.55, ΔR2 = 0.27, P < .001) (Table 2). A second regression retained the first two steps from the previous analysis but inserted the anxiety subscale of the HADS in the third step in place of the SDMT. Anxiety was a uniquely significant predictor of verbal learning (β = −0.34, ΔR2 = 0.11, P < .001) (Table 3).
Table 2.
Summary of hierarchical linear regression analysis for predicting effect of processing speed on verbal learning (N = 141)
| Variable | Model 1 | Model 2 | Model 3 | ||||||
|---|---|---|---|---|---|---|---|---|---|
| B | SE B | β | B | SE B | β | B | SE B | β | |
| Years of education | 0.202 | 0.352 | 0.049 | 0.222 | 0.350 | 0.054 | 0.161 | 0.299 | 0.039 |
| Sex | 0.763 | 2.582 | 0.025 | 0.789 | 2.565 | 0.026 | 0.112 | 2.194 | 0.004 |
| Motor disability, average 25-ft walk, s | −0.594 | 0.356 | −0.141 | 0.145 | 0.321 | 0.035 | |||
| SDMT total score | 0.547 | 0.076 | 0.548a | ||||||
| R2 block 1 = 0.003 | R2 Δ = 0.003 | F Δ = 0.219 | |||||||
| R2 block 2 = 0.023 | R2 Δ = 0.020 | F Δ = 2.783 | |||||||
| R2 block 3 = 0.292 | R2 Δ = 0.269 | F Δ = 51.693 | |||||||
Abbreviations: β, standardized beta coefficient; B, unstandardized beta coefficient; SDMT, Symbol Digit Modalities Test; SE B, standard error on beta.
aP < .001.
Table 3.
Summary of hierarchical linear regression analysis for predicting effect of anxiety on verbal learning (N = 141)
| Variable | Model 1 | Model 2 | Model 3 | ||||||
|---|---|---|---|---|---|---|---|---|---|
| B | SE B | β | B | SE B | β | B | SE B | β | |
| Years of education |
0.202 | 0.352 | 0.049 | 0.222 | 0.350 | 0.054 | 0.238 | 0.330 | 0.058 |
| Sex | 0.763 | 2.582 | 0.025 | 0.789 | 2.565 | 0.026 | 2.228 | 2.444 | 0.074 |
| Motor disability, average 25-ft walk, s | −0.594 | 0.356 | −0.141 | −0.535 | 0.336 | −0.127 | |||
| HADS anxiety subscale score | −1.004 | 0.238 | −0.341a | ||||||
| R2 block 1 = 0.003 | R2 Δ = 0.003 | F Δ = 0.219 | |||||||
| R2 block 2 = 0.023 | R2 Δ = 0.020 | F Δ = 2.783 | |||||||
| R2 block 3 = 0.136 | R2 Δ = 0.113 | F Δ = 17.869 | |||||||
Abbreviations: β, standardized beta coefficient; B, unstandardized beta coefficient; HADS, Hospital Anxiety and Depression Scale; SE B, standard error on beta.
aP < .001.
A mediation analysis was first performed to determine the relationship between anxiety and verbal learning through processing speed to test the primary hypothesis. There was a significant indirect effect of anxiety on verbal learning through processing speed (ab = −0.31, 95% CI = −0.60 to −0.09). The mediator accounted for approximately 32% of the total effect (PM = 0.32) (Figure 1). Given the significant inter-relatedness of the variables and to determine the unique role of anxiety as a mediator, a second mediation analysis was conducted to determine the relationship between processing speed and verbal learning through anxiety. There was a significant indirect effect of processing speed on verbal learning through anxiety (ab = −0.05, 95% CI = 0.01 to 0.12). The mediator accounted for approximately 9% of the total effect (PM = 0.09) (Figure 2).
Figure 1.
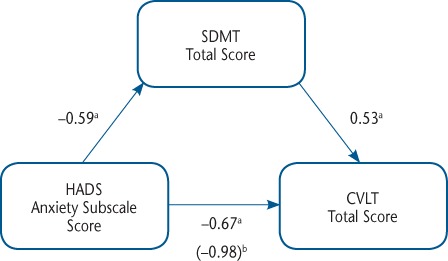
Mediation analysis of relationship between anxiety and verbal learning through processing speed
CVLT, California Verbal Learning Test, Second Edition; HADS, Hospital Anxiety and Depression Scale; SDMT, Symbol Digit Modalities Test. aP < .05. bP < .01.
Figure 2.
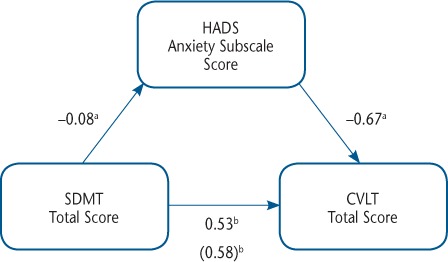
Mediation analysis of relationship between processing speed and verbal learning through anxiety
CVLT, California Verbal Learning Test, Second Edition; HADS, Hospital Anxiety and Depression Scale; SDMT, Symbol Digit Modalities Test. aP < .05. bP < .01.
Discussion
The results of this study suggest that a bidirectional relationship likely exists between anxiety and processing speed when influencing verbal learning in MS. The results of the first mediation analysis indicate that anxiety may be affecting verbal learning, in part by working through processing speed. This is consistent with attentional control theory, which proposes that anxiety may negatively affect cognition by influencing attention, which in turn slows processing speed; anxiety enhances attention for both internal and external distractors, thus disrupting effortful, goal-oriented cognitive processes. Attentional control theory states that anxiety increases attention to task-irrelevant stimuli, thus decreasing performance on cognitive tasks.11 Therefore, people with MS who have anxiety may be even slower at performing tasks than those without anxiety because their anxiety is distracting them from the task at hand. This also means that people with MS who receive treatment for anxiety may become less distracted by task-irrelevant internal stimuli, which may then improve their speed of information processing and, therefore, other aspects of cognition as well, such as verbal learning and memory.
The results of this study may also suggest that processing speed can affect verbal learning, in part by working through anxiety. Specifically, slowed processing speed is associated with higher levels of anxiety, which in turn is associated with lower levels of verbal learning. Slowed processing speed may enhance anxiety on tasks that require rapid processing of large chunks of information such as a list-learning task. However, more research is needed to confirm this hypothesized mechanism. Thus, this study provides empirical support for a bidirectional relationship of anxiety and processing speed affecting cognition in MS; anxiety may negatively affect attention, which slows down the speed of mental processing and, in turn, disrupts cognition, and slowed speed of mental processing may create symptoms of anxiety during tasks that place heavy demands on information processing, which then negatively affects cognition.
This study demonstrates the importance of screening for and treating anxiety in MS. More than 58% of the sample met the criteria for clinically significant anxiety. This study also showed that two frequently compromised areas of cognition in MS—processing speed and verbal learning—may be affected by anxiety. Slowed speed of information processing in MS likely negatively affects other aspects of cognition, as has been previously reported.18–20
Because anxiety and depression are often highly comorbid, the role of depression was also explored after the main analyses were run. Approximately 60% of the participants who met the criteria for clinically significant anxiety also met the criteria for clinically significant depression on a self-report depression measure. However, this depression measure was not significantly correlated with either processing speed or verbal learning after adjusting for demographic and disease factors. This depression measure was also added as an additional step to the two main regression equations, and it did not account for any significant unique variance in the regression equations. Thus, it was not added to the main mediation analyses.
This study has several limitations. This was a clinical sample, with people being referred for testing by their neurologist due to concerns about their cognition. A sample that was not cognitively compromised before testing may have yielded different results. Moreover, the level of clinically significant anxiety in this sample was 58%, which was higher than that in many of the other study samples.7–10 This finding likely increased the influence of anxiety in the analyses. The study also relied on self-reported anxiety, which may be susceptible to personal biases. Because the oral version of the SDMT was used, it may have been preferable to using a rudimentary oral motor speed measure as a control rather than the Timed 25-Foot Walk test because an oral motor speed measure21 would have adjusted for the oral motor demands involved in this version of the SDMT task. In addition, MS subtype diagnosed and time since diagnosis were not controlled for in the study.
To our knowledge, this is the first study to look at the connection between processing speed, anxiety, and verbal learning in MS. The results of this study support the idea that anxiety has a significant effect on cognition in MS and, thus, should be an important target for clinical interventions. Future clinical intervention studies for patients with MS and comorbid anxiety and cognitive deficits should be conducted to confirm this finding. These treatment studies should target symptoms of anxiety while measuring cognition before and after treatment to determine the impact of reducing anxiety on cognitive functioning in MS.
PRACTICE POINTS
Anxiety is very prevalent in MS but often goes unnoticed and untreated. In the present study, 58% of participants had clinically significant levels of anxiety.
Anxiety has a detrimental effect on cognitive functioning in people with MS, likely by interfering with attention. Anxiety seems to have a synergistic negative effect on cognition when combined with other underlying cognitive deficits, such as impaired processing speed.
Treating symptoms of anxiety in patients with MS can, in turn, improve their cognitive functioning.
Financial Disclosures
The authors declare no conflicts of interest.
Funding/Support
None.
References
- 1.Thornton AE, DeFreitas VG. The neuropsychology of multiple sclerosis. In: Grant I, Adams KM, editors. Neuropsychological Assessment of Neuropsychiatric and Neuromedical Disorders. 3rd ed. Oxford, UK: Oxford University Press; 2009. [Google Scholar]
- 2.Tullman MJ. Overview of the epidemiology, diagnosis, and disease progression associated with multiple sclerosis. Am J Manag Care. 2013;19(suppl):S15–S20. [PubMed] [Google Scholar]
- 3.Vytal KE, Cornwell BR, Letkiewicz AM, Arkin NE, Grillon C. The complex interaction between anxiety and cognition: insight from spatial and verbal working memory. Front Hum Neurosci. 2013;7:93. doi: 10.3389/fnhum.2013.00093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Basso MR, Lowery N, Ghormley C et al. Comorbid anxiety corresponds with neuropsychological dysfunction in unipolar depression. Cogn Neuropsychiatry. 2007;12:437–456. doi: 10.1080/13546800701446517. [DOI] [PubMed] [Google Scholar]
- 5.Janssens AC, Buljevac D, van Doorn PA et al. Prediction of anxiety and distress following diagnosis of multiple sclerosis: a two-year longitudinal study. Mult Scler. 2006;12:794–801. doi: 10.1177/1352458506070935. [DOI] [PubMed] [Google Scholar]
- 6.Feinstein A, O'Connor P, Gray T, Feinstein K. The effects of anxiety on psychiatric morbidity in patients with multiple sclerosis. Mult Scler. 1999;5:323–326. doi: 10.1177/135245859900500504. [DOI] [PubMed] [Google Scholar]
- 7.Beiske AG, Svensson E, Sandanger I et al. Depression and anxiety amongst multiple sclerosis patients. Eur J Neurol. 2008;15:239–245. doi: 10.1111/j.1468-1331.2007.02041.x. [DOI] [PubMed] [Google Scholar]
- 8.Bruce AS, Arnett PA. Longitudinal study of the symptom checklist 90-revised in multiple sclerosis patients. Clin Neuropsychologist. 2008;22:46–59. doi: 10.1080/13854040601064518. [DOI] [PubMed] [Google Scholar]
- 9.Feinstein A. Neuropsychiatric syndromes associated with multiple sclerosis. J Neurol. 2007;254(suppl 2):II73–II76. doi: 10.1007/s00415-007-2017-2. [DOI] [PubMed] [Google Scholar]
- 10.Korostil M, Feinstein A. Anxiety disorders and their clinical correlates in multiple sclerosis patients. Mult Scler. 2007;13:67–72. doi: 10.1177/1352458506071161. [DOI] [PubMed] [Google Scholar]
- 11.Eysenck MW, Derakshan N, Santos R, Calvo MG. Anxiety and cognitive performance: attentional control theory. Emotion (Washington, DC) 2007;7:336–353. doi: 10.1037/1528-3542.7.2.336. [DOI] [PubMed] [Google Scholar]
- 12.Derakshan N, Eysenck MW. Anxiety, processing efficiency, and cognitive performance. European Psychologist. 2009;14:168–176. [Google Scholar]
- 13.Stenager E, Knudsen L, Jensen K. Multiple sclerosis: correlation of anxiety, physical impairment and cognitive dysfunction. Ital J Neurol Sci. 1994;15:97–101. doi: 10.1007/BF02340120. [DOI] [PubMed] [Google Scholar]
- 14.Morrow SA, Rosehart H, Pantazopoulos K. Anxiety and depressive symptoms are associated with worse performance on objective cognitive tests in MS. J Neuropsychiatry Clin Neurosci. 2016;28:118–123. doi: 10.1176/appi.neuropsych.15070167. [DOI] [PubMed] [Google Scholar]
- 15.Julian LJ, Arnett PA. Relationships among anxiety, depression, and executive functioning in multiple sclerosis. Clin Neuropsychologist. 2009;23:794–804. doi: 10.1080/13854040802665808. [DOI] [PubMed] [Google Scholar]
- 16.Goretti B, Viterbo RG, Portaccio E et al. Anxiety state affects information processing speed in patients with multiple sclerosis. Neurol Sci. 2014;35:559–563. doi: 10.1007/s10072-013-1544-0. [DOI] [PubMed] [Google Scholar]
- 17.Roberg BL, Bruce JM, Lovelace CT, Lynch S. How patients with multiple sclerosis perceive cognitive slowing. Clin Neuropsychol. 2012;26:1278–1295. doi: 10.1080/13854046.2012.733413. [DOI] [PubMed] [Google Scholar]
- 18.DeLuca J, Chelune GJ, Tulsky DS, Lengenfelder J, Chiaravalloti ND. Is speed of processing or working memory the primary information processing deficit in multiple sclerosis? J Clin Exp Neuropsychol. 2004;26:550–562. doi: 10.1080/13803390490496641. [DOI] [PubMed] [Google Scholar]
- 19.Lengenfelder J, Bryant D, Diamond BJ, Kalmar JH, Moore NB, DeLuca J. Processing speed interacts with working memory efficiency in multiple sclerosis. Arch Clin Neuropsychol. 2006;21:229–238. doi: 10.1016/j.acn.2005.12.001. [DOI] [PubMed] [Google Scholar]
- 20.Rao SM, Aubin-Faubert PS, Leo GJ. Information processing speed in patients with multiple sclerosis. J Clin Exp Neuropsychol. 1989;11:471–477. doi: 10.1080/01688638908400907. [DOI] [PubMed] [Google Scholar]
- 21.Arnett PA, Smith MM, H Barwick FH, Benedict RH, Ahlstrom BP. Oralmotor slowing in multiple sclerosis: relationship to neuropsychological tasks requiring an oral response. J Int Neuropsychol Soc. 2008;14:454–462. doi: 10.1017/S1355617708080508. [DOI] [PubMed] [Google Scholar]
- 22.Benedict RH, Wahlig E, Bakshi R et al. Predicting quality of life in multiple sclerosis: accounting for physical disability, fatigue, cognition, mood disorder, personality, and behavior change. J Neurol Sci. 2005;231:29–34. doi: 10.1016/j.jns.2004.12.009. [DOI] [PubMed] [Google Scholar]
- 23.Strober L, Englert J, Munschauer F, Weinstock-Guttman B, Rao S, Benedict RH. Sensitivity of conventional memory tests in multiple sclerosis: comparing the Rao Brief Repeatable Neuropsychological Battery and the Minimal Assessment of Cognitive Function in MS. Mult Scler. 2009;15:1077–1084. doi: 10.1177/1352458509106615. [DOI] [PubMed] [Google Scholar]
- 24.DeLuca J, Barbieri-Berger S, Johnson SK. The nature of memory impairments in multiple sclerosis: acquisition versus retrieval. J Clin Exp Neuropsychol. 1994;16:183–189. doi: 10.1080/01688639408402629. [DOI] [PubMed] [Google Scholar]
- 25.Lafosse JM, Mitchell SM, Corboy JR, Filley CM. The nature of verbal memory impairment in multiple sclerosis: a list-learning and meta-analytic study. J Int Neuropsychol Soc. 2013;19:995–1008. doi: 10.1017/S1355617713000957. [DOI] [PubMed] [Google Scholar]
- 26.Brissart H, Morele E, Baumann C, Debouverie M. Verbal episodic memory in 426 multiple sclerosis patients: impairment in encoding, retrieval or both? Neurol Sci. 2012;33:1117–1123. doi: 10.1007/s10072-011-0915-7. [DOI] [PubMed] [Google Scholar]
- 27.Christodoulou C, Melville P, Scherl WF et al. Negative affect predicts subsequent cognitive change in multiple sclerosis. J Int Neuropsychol Society. 2009;15:53–61. doi: 10.1017/S135561770809005X. [DOI] [PubMed] [Google Scholar]
- 28.Mantella RC, Butters MA, Dew MA et al. Cognitive impairment in late-life generalized anxiety disorder. Am J Geriatr Psychiatry. 2007;15:673–679. doi: 10.1097/JGP.0b013e31803111f2. [DOI] [PubMed] [Google Scholar]
- 29.Bierman EJ, Comijs HC, Jonker C, Beekman AT. Effects of anxiety versus depression on cognition in later life. Am J Geriatr Psychiatry. 2005;13:686–693. doi: 10.1176/appi.ajgp.13.8.686. [DOI] [PubMed] [Google Scholar]
- 30.Leininger S, Skeel R. Cortisol and self-report measures of anxiety as predictors of neuropsychological performance. Arch Clin Neuropsychol. 2012;27:318–328. doi: 10.1093/arclin/acs035. [DOI] [PubMed] [Google Scholar]
- 31.Delis DC, Kramer JH, Kaplan E, Ober BA. California Verbal Learning Test, Second Edition (CVLT-II) San Antonio, TX: Psychological Corporation; 2000. [Google Scholar]
- 32.Stegen S, Stepanov I, Cookfair D et al. Validity of the California Verbal Learning Test–II in multiple sclerosis. Clin Neuropsychologist. 2010;24:189–202. doi: 10.1080/13854040903266910. [DOI] [PubMed] [Google Scholar]
- 33.Smith A. Symbol Digit Modalities Test (SDMT) Manual (Revised) Los Angeles, CA: Western Psychological Services; 1982. [Google Scholar]
- 34.Benedict RH, Cookfair D, Gavett R et al. Validity of the minimal assessment of cognitive function in multiple sclerosis (MACFIMS) J Int Neuropsychol Soc. 2006;12:549–558. doi: 10.1017/s1355617706060723. [DOI] [PubMed] [Google Scholar]
- 35.Zigmond AS, Snaith RP. The Hospital Anxiety and Depression Scale. Acta Psychiatr Scand. 1983;67:361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 36.Honarmand K, Feinstein A. Validation of the Hospital Anxiety and Depression Scale for use with multiple sclerosis patients. Mult Scler. 2009;15:1518–1524. doi: 10.1177/1352458509347150. [DOI] [PubMed] [Google Scholar]
- 37.Fischer JS, Rudick RA, Cutter GR, Reingold SC, National MS Society Clinical Outcomes Assessment Task Force The Multiple Sclerosis Functional Composite Measure (MSFC): an integrated approach to MS clinical outcome assessment. Mult Scler. 1999;5:244–250. doi: 10.1177/135245859900500409. [DOI] [PubMed] [Google Scholar]
- 38.Kieseier BC, Pozzilli C. Assessing walking disability in multiple sclerosis. Mult Scler. 2012;18:914–924. doi: 10.1177/1352458512444498. [DOI] [PubMed] [Google Scholar]
- 39.Hayes A. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach. New York, NY: The Guilford Press; 2013. [Google Scholar]


