Abstract
Objectives
This study aims to investigate the effect of physical therapy modalities on pain and functional status in patients with non-specific low back pain.
Patients and methods
Between February 2011 and August 2013, a total of 104 patients (38 males, 66 females; mean age 49.3±12.5 years; range 34 to 62 years) with non-specific chronic low back pain for more than 12 weeks without any neurological deficit were included in this randomized-controlled study. The patients were divided into two groups: physical therapy group (n=52) and control group (n=52). Both groups were given exercise and medical treatment; physiotherapy modalities were also applied in the physical therapy group. The patients were assessed using the Visual Analog Scale (VAS), Oswestry Disability Index (ODI), and Istanbul Low Back Pain Disability Index (ILBP) before treatment and at two weeks, three months, and one year after treatment.
Results
A total of 100 patients completed one-year follow-up. In both groups, the VAS, ODI, and ILBP significantly improved after treatment (p<0.01), compared to before treatment values. There were statistically significant differences in the VAS, ODI, and ILBP scores at three months and one year after treatment between the physical therapy group and control group (p<0.05).
Conclusion
Multidisciplinary approaches including physical therapy should be implemented to provide long-term improvement in pain and functional status in the treatment of non-specific chronic low back pain.
Keywords: Exercise, non-specific chronic low back pain, physical therapy methods
Introduction
Low back pain is one of the major health problems during life time with a prevalence of 80%, which causes functional loss and reduced productivity.[1,2] In 85% of patients with low back pain, the symptoms and signs are non-specific without a clear diagnosis, prognosis, or treatment protocol.[3,4] Chronic low back pain (CLBP) is back pain lasting longer than 12 weeks. It has a negative impact on functional, socioeconomic, and occupational activities and on the psychological status.[5-7] Due to the multiple negative effects associated with CLBP, it has been argued that a single technique for low back pain treatment would be ineffective and treatment should include a multidisciplinary approach.[8] A variety of conservative treatment modalities, such as exercise, physical therapy, and medication are applied in the treatment of CLBP. These techniques are intended to increase mobilization, decrease pain, and improve functional and psychological status.[9,10] Exercising is one of the main treatments used for CLBP and has been shown to reduce the duration and frequency of back pain.[11-13] Previous studies have demonstrated that physiotherapy modalities such as hot packs, ice massages, diathermy, ultrasound therapy, and transcutaneous electrical nerve stimulation (TENS) reduce inf lammation, relieve musculoskeletal symptoms and joint stiffness, thereby, providing symptomatic relief.[14-18] Additionally, medical treatment has been shown to be an effective method for symptomatic improvement of CLBP.[19-21] However, the efficacy of a combined approach with physical therapy and medical treatment for CLBP has not yet been sufficiently demonstrated. In the present study, we aimed to evaluate the effectiveness of physical treatment modalities for pain relief and functional status improvement in patients with CLBP.
Patients and Methods
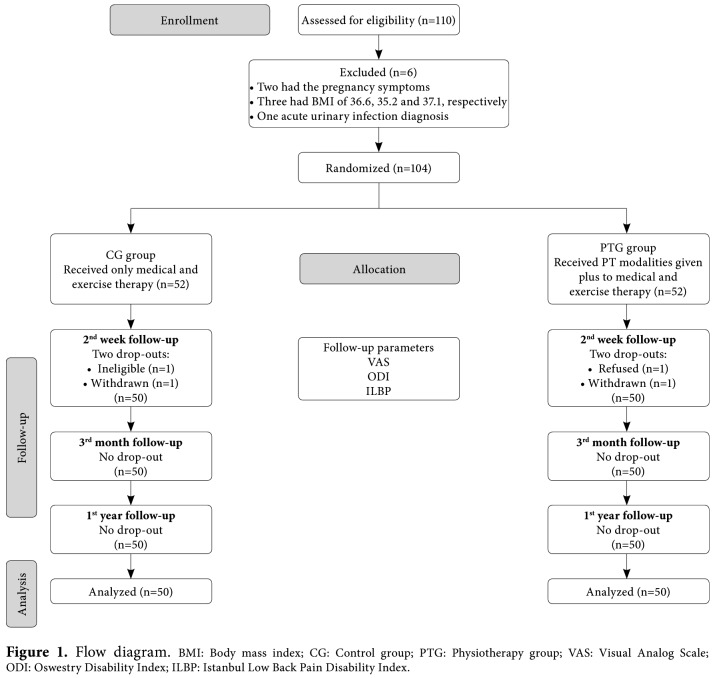
A total of 110 patients with CLBP were identified from the hospital records of the physical medicine and rehabilitation clinic between February 2011 and August 2013. The patients with CLBP of longer than 12 weeks without any neurological deficit were included in the study. Exclusion criteria were as follows: pain severity of ≥8 according to the Visual Analog Scale (VAS), age ≤18 years, pregnancy, previous surgery, structural abnormalities, spinal cord compression, serious instability, osteoporosis, body mass index (BMI) higher than 30 kg/m2, severe cardiovascular or metabolic disease, and acute infection. Accordingly, a total of 104 patients (38 males, 66 females; mean age 49.3±12.5 years; range 34 to 62 years) who met the inclusion criteria were included in this randomized- controlled study (Figure 1).
Figure 1. Flow diagram. BMI: Body mass index; CG: Control group; PTG: Physiotherapy group; VAS: Visual Analog Scale; ODI: Oswestry Disability Index; ILBP: Istanbul Low Back Pain Disability Index.
A detailed history of each patient was obtained and clinical examination was performed including neurological and physical examination of the lumbar region with inspection and palpation, lumbar mobility measurements, and lumbar range of motion measurements. All patients were evaluated by a single physician. The study protocol was approved by the local Ethics Committee. A written informed consent was obtained from each patient. The study was conducted in accordance with the principles of the Declaration of Helsinki.
Interventions
All patients were divided into two groups: physical therapy group (n=52) and control group (n=52). Physical therapy group (PTG) received physical therapy modalities in addition to medical and exercise therapy, while the control group (CG) was treated with medical and exercise therapy alone.
Medical treatment
If necessary, 1.5 g/day of paracetamol was prescribed.
Exercise program
Active isotonic and isometric strengthening exercises were prescribed to strengthen the frontal abdominal muscles (musculus obliquus externus abdominis, musculus obliquus internus abdominis, musculus rectus abdominis), deep abdominal muscles (musculus psoas major, musculus psoas minor, musculus iliacus, musculus quadratum lumbarum), and back muscles (musculi dorsi, musculus erector spinae, musculi transverso-spinales, musculi inter-spinales, musculi intertransversarii). For the hamstrings, lumbar extensors, and hip f lexors, a set of stretching exercises was prescribed. A home-based exercise program was instructed by the physiotherapist to each patient. In addition, a written exercise program was given to the patients. The exercise program lasted for three months and was performed at least five days per week, two exercises per day, with each exercise repeated at least 10 times.
Physical therapy
The physical therapy was administered to the waist region by the physiotherapist, for a total of 10 sessions, five days per week, with a single session per day. The sessions included a hot pack, ultrasound, and TENS treatment. Hot pack therapy was applied for 20 min and ultrasonic therapy for five min in continuous form at a frequency of 1 MHz and a density of 1.5 W/cm2.[16,17] In addition, TENS treatment was given in the following form: continuous, with strength of 100 Hz, 40 μSN for 30 min.
Evaluation criteria
All patients were assessed prior to treatment and at two weeks, three months, and one year after treatment. Pain severity was evaluated using the VAS according to a 10-point scale, where 0 points indicate no pain and 10 points indicate severe pain.[22] The functional status was evaluated using the Oswestry Disability Index (ODI).[23-28] and Istanbul Low Back Pain Disability Index (ILBP).[26] The ODI consists of 10 questions which assess the degree of pain, personal care, lifting, walking, sitting, standing, sleeping, social life, travel, and pain alteration, each scoring between 0 and 5. Maximum score is 50 and the total score is multiplied by two: the result is presented in percentage. The evaluation formula is as follows: points/total score (50) x 100= %, where 0% indicates the absence of pain and functional disability and 100% indicates severe pain and functional limitation. Its validity and reliability studies were conducted in patients with low back pain in the Turkish society.[25] In addition, ILBP is a scale with a total score of 0-90, including 18 items evaluating the functional status of patients with low back pain, with scores ranging from 0 to 5 for each question. Its validity and reliability studies were carried out.[26]
Sample size calculation
The number of the patients included in this study was determined based on VAS data. According to the results of Sahin et al.,[27] the mean score of the VAS in PTG was 7.16 with a standard deviation (SD) of 2.54 and the mean score of the VAS in CG was 5.72.[27] The sample size was based on a power of 80% (beta: 0.2). A p value of 0.05 was considered statistically significant. Accordingly, 48 patients were required in each group. We estimated a dropout rate of 10% and, thus, aimed to allocate 52 patients for each group.
Randomization
After the patients' medical histories were collected, the data relating to each patient were filled out by two investigators and placed in envelopes. Then, using a random number table obtained from the computer, the closed envelopes of the patients were randomly distributed into two groups in a 1:1 ratio (PTG, CG). During the study, 50 patients in each group completed at two weeks, three months, and one year follow-up (Figure 1).
Statistical analysis
Statistical analysis was performed using the PASW for Windows version 18.0 software (SPSS Inc., Chicago, IL, USA). The conformity of continuous variables with normal distribution was evaluated using the Shapiro- Wilk test. To evaluate the differences among the categorical variables (i.e., sex, education status, and profession) between the groups, the chi-square test was performed. The Mann-Whitney U test was used to compare significant differences among the abnormally distributed variables. Differences in continuous data between the groups were analyzed using the Student t-test for normally distributed variables. The repeated measures analysis of variance (ANOVA) was performed to compare the data from the parameters repeatedly measured in the intra-group analysis. The Bonferroni correction was carried out to make an inter-group analysis, and a post-hoc test was performed, if the variance analysis test result was significant. To detect the sub-group differences, the Bonferroni Student t-test was used. A p value of <0.05 was considered statistically significant.
Results
A total of 100 patients completed one-year follow-up. The mean age of PTG was 50.4±11.4 years and the mean age of CG was 46.2±12.3 years. There was no statistically significant difference in the age, sex, education, occupation, and BMI between the groups (p>0.05). Sixty-three percent of the groups were females, and 13% were university graduates. Demographic characteristics of both groups are shown in Table 1.
Table 1. Patient demographics.
| Physiotherapy group (n=50) | Control group (n=50) | ||||||
| n | % | Mean±SD | n | % | Mean±SD | p | |
| Age (year) | 50.4±11.4 | 46.2±12.3 | 0,08 | ||||
| Sex | 0,83 | ||||||
| Male | 18 | 36 | 19 | 38 | |||
| Female | 32 | 64 | 31 | 62 | |||
| Level of education | 0,46 | ||||||
| Primary school | 39 | 78 | 36 | 72 | |||
| Secondary school | 4 | 8 | 8 | 16 | |||
| Higher education | 7 | 14 | 6 | 12 | |||
| Profession | 0,09 | ||||||
| Housewife | 37 | 74 | 31 | 62 | |||
| Office worker | 9 | 18 | 7 | 14 | |||
| Working class | 4 | 8 | 12 | 24 | |||
| Body mass index | 29.4±5.0 | 28.6±5.2 | 0,44 | ||||
| SD: Standard deviation. | |||||||
In both groups, the VAS scores after the therapy were significantly lower compared to pre-therapy scores and the differences between pre-therapy and at three months post-therapy were found to be significant (p<0.05). ODI, and ILBP scores showed a significant improvement at two weeks and three months of follow-up compared to baseline values (p<0.05) (Table 2). There was a statistically significant difference in the VAS, ODI, and ILBP scores at two week, three months, and one year of follow-up, compared to the baseline values between the groups, in favor of PTG (Table 2).
Table 2. Intra- and inter-group comparisons of results before, at two weeks, three months, and one year after treatment.
| Physiotherapy group (n=50) | Control group (n=50) | Inter-group | ||
| Mean±SD | Mean±SD | p | F | |
| VAS baseline | 6.1±0.2 | 5.2±0.2 | 7,071 | |
| VAS 2nd week | 4.3±0.2* | 4.0±0.2* | 0,032 | |
| VAS 3rd month | 4.4±0.2* | 4.2±0.2* | 0,012 | |
| VAS 1st year | 4.7±0.3 | 5.0±0.2 | 0,007 | |
| ODI baseline | 50.6±1.0 | 45.2±1.3 | 6,690 | |
| ODI 2nd week | 43.6±1.6* | 33.3±2.3* | 0,021 | |
| ODI 3rd month | 43.7±1.7* | 33.8±2.1* | 0,011 | |
| ODI 1st year | 46.6±2.1 | 45.3±1.5 | 0,011 | |
| ILBP baseline | 30.7±1.8 | 24.0±2.0 | 9,615 | |
| ILBP 2nd week | 21.7±1.5* | 14.9±1.8* | 0,037 | |
| ILBP 3rd month | 22.6±1.7* | 16.8±1.6* | 0,019 | |
| ILBP 1st year | 25.3±2.0 | 22.0±1.9 | 0,002 | |
| SD: Standard deviation; VAS: Visual Analog Scale; ODI: Oswestry Disability Index; ILBP: Istanbul Low Back Pain Disability Index; F: Test statistics (analysis of variance with repeated measurements); * p<0.05 according to baseline values in intra-group comparison. | ||||
Discussion
In this randomized-controlled trial, we found that the combination of physical therapy methods, exercise, and medical treatment for non-specific CLBP improved pain and functional status than exercise and medical treatment without physical therapy. This improvement sustained for three months after the treatment. These results show that physiotherapy combined with medical therapy and exercise leads to better improvements in pain and functional status at three months after the initiation of the treatment. The main goals of CLBP treatment are to reduce pain, to improve soft tissue flexibility due to spasm and tension, to increase strength and endurance of the trunk stabilizers, and to improve mobility and posture, thereby, leading to improved functional capacity, better ability to perform activities of daily life, and prevention of work loss.[28,29] Many methods such as resting, medical treatment, back school, exercise programs, physical therapy modalities, and manipulation are used in the treatment of CLBP. It has been shown that a multidisciplinary approach is more effective than a single treatment modality.[30-32] Therefore, a multidisciplinary approach including physical therapy, exercise, and medical treatment was applied in our study. Decreased paraspinal muscle strength and endurance is an important risk factor for the development of low back pain. In addition, the body muscle strength is lower in patients with low back pain than in healthy people.[33] In patients with reduced muscle strength, the risk of lumbar pain is three times higher. Therefore, exercise is one of the primary treatment modalities for non-specific CLBP.[33] It aims to improve posture, to strengthen the trunk muscles, and to increase aerobic capacity, leading to reduced pain and improved functional status.[13,34] In a study, Van Tulder et al.[35] reported that exercise for the treatment of low back pain was effective in accelerating improvements in daily life activities and return to work. In a meta-analysis, the patients with CLBP treated with exercise therapy showed a significant improvement in terms of pain and functional status, compared to the patients who received no treatment or other conservative treatments.[36] It has also been shown that inactivity leads to undesirable behaviors such as kinesophobia, anxiety, and difficulty in coping with pain, and exercise therapy reduces these behaviors.[37,38] However, there is no precise information concerning the effect of exercise types (i.e., flexion, stretching, or strengthening) on the patient outcomes.[34,37] In several studies, it has been shown that the pain relief due to exercise therapy in CLBP is limited to six-months duration.[39] In our study, lumbar isometric, lumbar flexion, and lumbar and hamstring stretching exercises were applied. Pain and functional status both improved with physiotherapy, exercise therapy, and medical treatment prescribed in this study. We also observed that this improvement lasted for one year. During the study of CLBP patients, we concluded that pain and functional status were negatively affected; therefore, the treatment was demonstrated to be effective in improving the severity of the pain and the function status.[40] In the present study, the VAS was used to assess the pain severity and the ODI and ILBP were used to evaluate the functional status. We found significantly higher improvements in the VAS, ODI, and ILBP scores with the addition of physiotherapy at three month and one year of follow-up, compared to medical and exercise therapy alone. Another method used in the treatment of patients with non-specific CLBP, which we also included in this study, is physical therapy modalities. These modalities allow for short-term treatment, including cold application, hot pack, ultrasound, diathermy, and TENS.[2,16,18] These treatments are non-invasive, safe, easy to administer, and rarely cause significant side effects, except mild skin irritation.[41,42] In several studies, it has been shown that physical therapy is more effective than placebo.[34,42,43] One of the most commonly used physical therapy methods is TENS. In one study, TENS was found to be more effective in reducing pain and increasing the range of motion of the joint, compared to placebo.[34] Marchand et al.[44] divided 48 patients with low back pain into three groups as the control, placebo, and TENS. A 43% reduction in the pain severity was found in the TENS group.[44] In another study evaluating hot and cold applications, it was shown that warm application was more successful than placebo in reducing pain in patients with acute and subacute lumbar pain, and cold application provided pain control in the acute phase and reduced the muscle tension.[16] In our study, there was no placebo group. We found that when added to medical treatment and exercise, physical therapy was associated with a higher improvement in pain and functional status. Although the efficacy of these treatment modalities was not evaluated separately in our study, the positive effect of the addition of physical therapy to the other treatment modalities was demonstrated. In many studies, CLBP treatment groups are heterogeneous, no control group is included, and treatment efficacy is only evaluated for a short time.[45] In our study, the treatment groups were homogeneous and a control group was included. Follow-up was continued for one year. It is critical that the treatment effect for CLBP is long-term; therefore, retention of pain control and functional improvements must be maintained. Isokinetic measurements are the gold standard to demonstrate the efficacy of exercises, but are very subjective. In our study, we did not perform isokinetic muscle strength measurements; this may represent a limitation. Another limitation is the unknown contribution of medical and exercises therapies to patients’ improvement. The ideal control group for this study would be a group of patients who are followed without any treatment. As this would be unethical, however, we provided medical and exercise therapy to our control group patients. In conclusion, treatment approaches for chronic conditions should have long-term effects and should ideally provide permanent improvement. Our study results showed that improvements were able to be sustained for one year after the treatment. Therefore, combined treatment with exercise, medical therapy, and physiotherapy was found to be more effective for non-specific CLBP than exercise and medical therapy alone. These results suggest that treatment of CLBP should ideally include a multidisciplinary approach with physiotherapy to provide long-term improvement.
Footnotes
Conflict of Interest: The authors declared no conflicts of interest with respect to the authorship and/or publication of this article.
Financial Disclosure: The authors received no financial support for the research and/or authorship of this article.
References
- 1.Burdorf A. Reducing random measurement error in assessing postural load on the back in epidemiologic surveys. Scand J Work Environ Health. 1995;21:15–23. doi: 10.5271/sjweh.3. [DOI] [PubMed] [Google Scholar]
- 2.Isaac Z, Katz JN, Borenstein DG. Regional and widespread pain: lumbar spine disorders. In: Hochberg MC, Silman AJ, Smolen JS, Weinblatt MH, editors. Rheumatology. Oxford: Elsevier; 2008. pp. 593–618. [Google Scholar]
- 3.Kääpä EH, Frantsi K, Sarna S, Malmivaara A. Multidisciplinary group rehabilitation versus individual physiotherapy for chronic nonspecific low back pain: a randomized trial. Spine (Phila Pa 1976) 2006;31:371–376. doi: 10.1097/01.brs.0000200104.90759.8c. [DOI] [PubMed] [Google Scholar]
- 4.Moffett J, McLean S. The role of physiotherapy in the management of non-specific back pain and neck pain. Rheumatology (Oxford) 2006;45:371–378. doi: 10.1093/rheumatology/kei242. [DOI] [PubMed] [Google Scholar]
- 5.Hildebrandt J, Ursin H, Mannion AF, Airaksinen O, Brox JI, Cedraschi C, et al. European guidelines for the management of chronic non specific low back pain. Eur Spine J. 2006;15(Suppl 2):192–300. doi: 10.1007/s00586-006-1072-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Maher CG. Effective physical treatment for chronic low back pain. Orthop Clin North Am. 2004;35:57–64. doi: 10.1016/S0030-5898(03)00088-9. [DOI] [PubMed] [Google Scholar]
- 7.Becker A, Held H, Redaelli M, Chenot JF, Leonhardt C, Keller S, et al. Implementation of a guideline for low back pain management in primary care: a cost-effectiveness analysis. Spine (Phila Pa 1976) 2012;37:701–710. doi: 10.1097/BRS.0b013e31822b01bd. [DOI] [PubMed] [Google Scholar]
- 8.van Tulder MW, Koes BW, Assendelft WJ, Bouter LM, Maljers LD, Driessen AP. Chronic low back pain: exercise therapy, multidisciplinary programs, NSAID's, back schools and behavioral therapy effective; traction not effective; results of systematic reviews. Ned Tijdschr Geneeskd. 2000;144:1489–1494. [PubMed] [Google Scholar]
- 9.Berker E, Dinçer N. Chronic pain and rehabilitation. [Article in Turkish] Agri. 2005;17:10–16. [PubMed] [Google Scholar]
- 10.Waddell G, Burton AK. Concepts of rehabilitation for the management of low back pain. Best Pract Res Clin Rheumatol. 2005;19:655–670. doi: 10.1016/j.berh.2005.03.008. [DOI] [PubMed] [Google Scholar]
- 11.Liddle SD, Gracey JH, Baxter GD. Advice for the management of low back pain: a systematic review of randomised controlled trials. Man Ther. 2007;12:310–327. doi: 10.1016/j.math.2006.12.009. [DOI] [PubMed] [Google Scholar]
- 12.van der Roer N, van Tulder M, Barendse J, Knol D, van Mechelen W, de Vet H. Intensive group training protocol versus guideline physiotherapy for patients with chronic low back pain: a randomised controlled trial. Eur Spine J. 2008;17:1193–1200. doi: 10.1007/s00586-008-0718-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.van Middelkoop M, Rubinstein SM, Kuijpers T, Verhagen AP, Ostelo R, Koes BW, et al. A systematic review on the effectiveness of physical and rehabilitation interventions for chronic non-specific low back pain. Eur Spine J. 2011;20:19–39. doi: 10.1007/s00586-010-1518-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nordin M, Campello M. Physical therapy: exercises and the modalities: when, what, and Why? Neurol Clin. 1999;17:75–89. doi: 10.1016/s0733-8619(05)70115-8. [DOI] [PubMed] [Google Scholar]
- 15.Choi BK, Verbeek JH, Tam WW, Jiang JY. Exercises for prevention of recurrences of low-back pain. Cochrane Database Syst Rev. 2010;1:6555–6555. doi: 10.1002/14651858.CD006555.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shahbandar L, Press J. Diagnosis and Nonoperative Management of Lumbar Disk Herniation. Oper Tech Sports Med. 2005;13:114–121. [Google Scholar]
- 17.Jordan J, Konstantinou K, Morgan TS, Weinstein J. Herniated lumbar disc. Clin Evid. 2005;14:1–4. [PubMed] [Google Scholar]
- 18.Simpson AK, Cholewicki J, Grauer J. Chronic low back pain. Curr Pain Headache Rep. 2006;10:431–436. doi: 10.1007/s11916-006-0074-3. [DOI] [PubMed] [Google Scholar]
- 19.Turner JA, Denny MC. Do antidepressant medications relieve chronic low back pain. J Fam Pract. 1993;37:545–553. [PubMed] [Google Scholar]
- 20.Chou R, Huffman LH. Medications for acute and chronic low back pain: a review of the evidence for an American Pain Society/American College of Physicians clinical practice guideline. Ann Intern Med. 2007;147:505–514. doi: 10.7326/0003-4819-147-7-200710020-00008. [DOI] [PubMed] [Google Scholar]
- 21.Özcan E. Bel ağrılarında ilaç tedavisi. Türkiye Klinikleri Fiz Tıp ve Reh Derg. 2000;1:10–14. [Google Scholar]
- 22.Strong J, Ashton R, Chant D. Pain intensity measurement in chronic low back pain. Clin J Pain. 1991;7:209–218. doi: 10.1097/00002508-199109000-00007. [DOI] [PubMed] [Google Scholar]
- 23.Fairbank JC, Couper J, Davies JB, O'Brien JP. The Oswestry low back pain disability questionnaire. Physiotherapy. 1980;66:271–273. [PubMed] [Google Scholar]
- 24.Fritz JM, Irrgang JJ. A comparison of a modified Oswestry Low Back Pain Disability Questionnaire and the Quebec Back Pain Disability Scale. Phys Ther. 2001;81:776–788. doi: 10.1093/ptj/81.2.776. [DOI] [PubMed] [Google Scholar]
- 25.Duruöz MT, Özcan E, Ketenci A, Karan A, Kiralp MZ. Cross cultural validation of the revised Oswestry pain questionnaire in a Turkish population. Arthritis δ Rheumatism. 1999;42 (Suppl):1200–1200. [Google Scholar]
- 26.Duruoz T, Cerrahoglu L, Tıkız C, Turan Y. İstanbul bel ağrısı fonksiyonel skalasının klinik değişime duyarlılığı. Lokomotor Dergisi. 2008;45:839–842. [Google Scholar]
- 27.Sahin N, Albayrak I, Durmus B, Ugurlu H. Effectiveness of back school for treatment of pain and functional disability in patients with chronic low back pain: a randomized controlled trial. J Rehabil Med. 2011;43:224–229. doi: 10.2340/16501977-0650. [DOI] [PubMed] [Google Scholar]
- 28.McGill SM. Low back exercises: evidence for improving exercise regimens. Phys Ther. 1998;78:754–765. doi: 10.1093/ptj/78.7.754. [DOI] [PubMed] [Google Scholar]
- 29.Simmonds M, Olson SL, Jones S, Hussein T, Lee CE, Novy D, et al. Psychometric characteristics and clinical usefulness of physical performance tests in patients with low back pain. Spine (Phila Pa 1976) 1998;23:2412–2421. doi: 10.1097/00007632-199811150-00011. [DOI] [PubMed] [Google Scholar]
- 30.Chou R, Qaseem A, Snow V, Casey D, Cross JT Jr, Shekelle P, et al. Diagnosis and treatment of low back pain: a joint clinical practice guideline from the American College of Physicians and the American Pain Society. Ann Intern Med. 2007;147:478–491. doi: 10.7326/0003-4819-147-7-200710020-00006. [DOI] [PubMed] [Google Scholar]
- 31.Negrini S, Giovannoni S, Minozzi S, Barneschi G, Bonaiuti D, Bussotti A, et al. Diagnostic therapeutic flow-charts for low back pain patients: the Italian clinical guidelines. Eura Medicophys. 2006;42:151–170. [PubMed] [Google Scholar]
- 32.Poitras S, Rossignol M, Dionne C, Tousignant M, Truchon M, Arsenault B, et al. An interdisciplinary clinical practice model for the management of low-back pain in primary care: the CLIP project. BMC Musculoskelet Disord. 2008;9:54–54. doi: 10.1186/1471-2474-9-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Airaksinen O, Brox JI, Cedraschi C, Hildebrandt J, Klaber-Moffett J, Kovacs F, et al. Chapter 4. European guidelines for the management of chronic nonspecific low back pain. Eur Spine J. 2006;15:192–300. doi: 10.1007/s00586-006-1072-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Quittan M. Management of back pain. Disabil Rehabil. 2002;24:423–434. doi: 10.1080/09638280110108850. [DOI] [PubMed] [Google Scholar]
- 35.van Tulder M, Malmivaara A, Esmail R, Koes B. Exercise therapy for low back pain: a systematic review within the framework of the cochrane collaboration back review group. Spine (Phila Pa 1976) 2000;25:2784–2796. doi: 10.1097/00007632-200011010-00011. [DOI] [PubMed] [Google Scholar]
- 36.Hayden JA, van Tulder MW, Malmivaara AV, Koes BW. Meta-analysis: exercise therapy for nonspecific low back pain. Ann Intern Med. 2005;142:765–775. doi: 10.7326/0003-4819-142-9-200505030-00013. [DOI] [PubMed] [Google Scholar]
- 37.Klaber Moffett JA, Carr J, Howarth E. High fear-avoiders of physical activity benefit from an exercise program for patients with back pain. Spine (Phila Pa 1976) 2004;29:1167–1172. doi: 10.1097/00007632-200406010-00002. [DOI] [PubMed] [Google Scholar]
- 38.Norris C, Matthews M. The role of an integrated back stability program in patients with chronic low back pain. Complement Ther Clin Pract. 2008;14:255–263. doi: 10.1016/j.ctcp.2008.06.001. [DOI] [PubMed] [Google Scholar]
- 39.Smith C, Grimmer-Somers K. The treatment effect of exercise programmes for chronic low back pain. J Eval Clin Pract. 2010;16:484–491. doi: 10.1111/j.1365-2753.2009.01174.x. [DOI] [PubMed] [Google Scholar]
- 40.Maughan EF, Lewis JS. Outcome measures in chronic low back pain. Eur Spine J. 2010;19:1484–1494. doi: 10.1007/s00586-010-1353-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Moyá F, Grau M, Riesco N, Núñez M, Brancós MA, Valdés M, et al. Chronic low back pain: multispecialty assessment of 100 patients. Aten Primaria. 2010;26:239–244. doi: 10.1016/S0212-6567(00)78653-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Li LC, Bombardier C. Physical therapy management of low back pain: an exploratory survey of therapist approaches. Phys Ther. 2001;81:1018–1028. [PubMed] [Google Scholar]
- 43.Şimşek Ş, Yağcı N, Gedik E. The effect of back school program on fear avoidance behavior, disability and pain in chronic mechanic low back pain. J Clin Anal Med. 2015;6(Suppl 3):389–393. [Google Scholar]
- 44.Marchand S, Charest J, Li J, Chenard JR, Lavignolle B, Laurencelle L. Is TENS purely a placebo effect? A controlled study on chronic low back pain. Pain. 1993;54:99–106. doi: 10.1016/0304-3959(93)90104-W. [DOI] [PubMed] [Google Scholar]
- 45.Karahan AY, Sahin N, Baskent A. Comparison of effectiveness of different exercise programs in treatment of failed back surgery syndrome: A randomized controlled trial. J Back Musculoskelet Rehabil. doi: 10.3233/BMR-160722. 2016 Jun 17. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]