Abstract
Purpose.
In this pilot study, we evaluated changes in toothbrushing behaviors associated with a mobile game.
Methods.
Children ages 5–6 years were taught to use the Brush Up game and played it once/day at home for seven days (N=34). The primary outcome was toothbrushing quality measured as duration and distribution. The paired t-test was used to assess pre/post changes and Holm’s method adjusted for multiple testing (α=0.05).
Results.
The mean age was 73.7±6.6 months, 29.4% were female, and 47.1% were White. After seven days, toothbrushing duration increased significantly (P<0.001). Toothbrushing distribution improved with increased brushing of the lingual, maxillary occlusal, and posterior buccal surfaces. For children who played the game for 14 days (n=15), even greater improvements in quality and distribution were observed. Improvements in toothbrushing did not persist one year later without further app use but there were noted changes that could be clinically meaningful.
Conclusions.
Mobile health games can potentially improve toothbrushing quality in children. Additional trials are needed to assess mobile toothbrushing games.
Keywords: health app, children, toothbrushing behaviors, dental hygiene, technology, behavior change, mobile game, game application
Introduction
Tooth decay is a multifactorial disease that is preventable through regular toothbrushing.1 Studies report 80% of children brush twice daily, but actual rates may be lower because of overreporting.2–4 Many caregivers experience difficulties enforcing toothbrushing habits and an older study demonstrated children commonly miss tooth surfaces during toothbrushing.5–7 These factors highlight the importance of developing strategies to improve toothbrushing in childhood.
Efforts to improve toothbrushing in children have focused on health education based on the premise that inadequate knowledge is the main barrier. However, findings from a recent systematic review indicate that health education alone does not significantly improve toothbrushing attitudes or behaviors.8 Most caregivers know toothbrushing is important, but lack self-efficacy and other skills to enforce toothbrushing habits.9
Most families own devices that give them access to mobile health games.10 Two systematic reviews reported limited support for mobile games,11–12 but the original interventions were found to be passive (e.g., text reminders, monitoring), making it likely that the problem was with weak intervention design. In terms of toothbrushing games, a U.K. study surveyed 189 toothbrushing mobile game users ages 7–75 years (e.g., how clean did your teeth feel after using the game).13 Most users were adults, the game was not tailored to children, and the study focused on perceptions rather than behaviors. A second study described a proposed intervention for a toothbrushing game for Dutch teens.14 Dental researchers have explored online coaching, text messages, and “selfie” photographs as ways to improve toothbrushing, but none have been scaled commercially.15–17
Mobile toothbrushing games for children have become ubiquitous despite the lack of evidence demonstrating effectiveness. The goal of this pilot study was to evaluate a commercially-available mobile children’s toothbrushing game called Brush Up and assess whether the game could potentially help improve toothbrushing behaviors. We tested the hypothesis that game play would be associated with improvements in toothbrushing quality.
Methods
Game Development.
Brush Up is a theory-based mobile game that helps children develop toothbrushing skills through modeling, instructional song, and immediate performance feedback. The game teaches children the Modified Bass Stillman Technique. The game was originally developed using data from a series of formative evaluations with children ages 5–6 years at a Boys and Girls Club in Atlanta, GA. We focused on children ages 5–6 years because this is the developmental period in which many children begin to show signs of independence for health behaviors like toothbrushing and the minimal requisite motor skills, even though it is important to underscore the importance of adult supervision during brushing for young children. The game design includes an instructional song to guide brushing. Children helped refine the song’s words, voted on their favorite tune, and selected a cartoon exemplar. Subsequent formative tests showed that the initial exemplar selected by children (a dog) was difficult for children to emulate during toothbrushing. Instead, a “monster” with a child-like dentition and special jaw geometry was designed that would allow children to visualize the inside of the mouth while playing the game. The exemplar is gender, race, and ethnicity neutral to ensure appropriateness for children of all backgrounds (Figure 1).
Figure 1.
Images of BrushUp cartoon exemplar and sample intraoral view of the cartoon’s mouth that child sees while using BrushUp app
Game Features.
Brush Up teaches the child to brush along with a song that lasts three minutes. The tempo sets the pace of sulcus strokes and sweeps. The rhythm counts off twelve miniscule strokes and three broad sweeps for each tooth surface before advancing to the next. The song and accompanying video progress through the mouth sequentially from tooth to tooth. An instrumented toothbrush monitors the child’s performance while he or she brushes in tandem with a cartoon exemplar. The toothbrush incorporates an Inertial Measurement Unit (IMU), a package of gyroscopes and accelerometers. Data from sensors allow the software to continuously calculate the orientation of the toothbrush and infer its position in the mouth. The software directly reads the torque applied by sweeping motions, and can calculate brushing force as the child accelerates the brush back and forth. These data are reported in real time to the app using a Bluetooth Low Energy interface. The player is rewarded for accurate conformance with the demonstration. Performance errors are detected by the game system and immediately highlighted by verbal, visual, and sound effect cues in addition to a scoreboard penalty. The player is congratulated when these errors are later corrected.
Study Population.
Children ages 5–6 years were recruited from mixed-income neighborhoods in Atlanta, Georgia through posters placed in local stores, schools, and libraries in June and July 2012. There was also in-person recruitment of participants by a Research Assistant at local grocery store parking lots. The goal was to recruit a convenience sample of 34 children, which is what the limited study budget permitted. There were no a priori sample size calculations. Exclusion criteria were intellectual, developmental, or physical disabilities that might interfere with toothbrushing or gameplay. At the end of the study, each participating family received $200 as a thank you gift. The study was approved by the Morehouse School of Medicine IRB.
Study Procedures.
We obtained written consent from the child’s primary caregiver and verbal assent from each child. Caregivers completed a survey on demographics (e.g., child’s age in months, sex, race, ethnicity, grade, handedness). At baseline, all children brushed their teeth with a manual toothbrush in a GamesThatWork laboratory decorated as a bathroom with a sink and mirror. The child received no brushing guidance from any adult, peer, video, game, music, or clock. All toothbrushing visits were videotaped. Caregivers could observe through a small one-way window. Identical procedures took place during subsequent study visits.
After the baseline assessment, children were taught to use Brush Up by a Research Assistant. Each child was sent home with a sensor-enabled toothbrush and a laptop computer with Brush Up installed. The computer had Bluetooth connectivity to the toothbrush and Internet connectivity to the research servers, which enabled the team to record and monitor toothbrushing remotely. Caregivers were given instructions on how to set up the game at home, and were asked to have the child play each evening for seven consecutive nights (once/night). Caregivers were specifically asked not to provide any toothbrushing instruction during the study.
Outcome Measures.
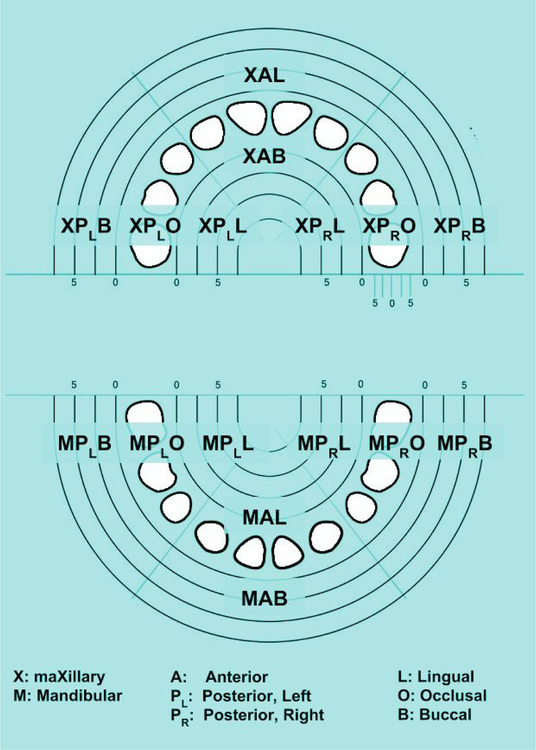
The study was a pre-post intervention with a single arm. The primary outcome was toothbrushing quality measured as total time (in seconds) the child brushed and distribution of brushing, measured at baseline and at seven days after app use. Outcomes were based on video analysis performed retrospectively by a Research Assistant blinded to when the video was recorded. The video recordings measured total toothbrushing time. In addition, using electronic timers and video scoring software, a researcher assessed toothbrushing time on specific tooth surfaces to measure distribution of toothbrushing. The maxillary and mandibular arches were divided into an anterior zone with lingual and buccal brushing surfaces, and left and right posterior zones were divided into lingual, buccal and occlusal brushing surfaces (16 surfaces total) (Figure 2).
Figure 2.
Diagram indicating 16 segments of the mouth to assess distribution of toothbrushing
Data Management and Analyses.
Survey data were entered into a spreadsheet and verified for accuracy. Toothbrushing data were captured remotely and stored on secure servers. We generated descriptive statistics on the study population. Our main hypothesis was that toothbrushing quality would improve after seven days.
While developing the original study protocol, we wanted to evaluate outcomes again at 14 days for all children, but limited study resources permitted only a subset of families to participate beyond seven days. Accordingly, we conducted exploratory analyses to evaluate outcomes after seven additional days of app use (total of 14 days of app use) for first 15 children that enrolled in the study to test the exploratory hypothesis of whether there would be a dose response associated with additional game play. As part of a follow-up grant, we had the opportunity to compare outcomes at one-year post-baseline to assess if skills were sustained even though we acknowledge the high likelihood of insufficient statistical power. One-year comparisons were run separately for children who played the game for seven days (n=14) and 14 days (n=10). We used a 95% confidence interval and the paired t-test to evaluate pre/post changes (α=0.05). Holm’s method was used to adjust for multiple testing. All analyses were conducted using SAS Version 9.4 (SAS Institute Inc., Cary, NC, USA).
Results
Descriptive Statistics.
For the 34 children who were assessed after seven days of game play, the mean age was 73.7 months (standard deviation: 6.6 months), 29.4% were female, 47.1% were White, 5.9% were Hispanic, and 85.3% were right-handed. Demographics were similar for children assessed at 14 days and one year.
Main Hypotheses.
After seven days, there were significant improvements in the main outcome measure in which the mean total toothbrushing time increased by 23.1±31.5 seconds (95% confidence interval [CI]: 12.2, 34.1; P<0.001) (Table 1). Toothbrushing distribution improved, with significant increases on lingual, maxillary occlusal, and posterior buccal surfaces. The largest increase was observed for lingual surfaces from a baseline mean of 0.9 seconds to a mean of 13.2 seconds (average increase=12.3 seconds; 95% CI: 7.4, 17.3). At baseline only 14.7% (5/34) of the children had any brushing of the lingual surfaces as compared to 76.5% (26/34) of the children who brushed lingual surfaces after seven days (McNemar’s test; P<0.001).
Table 1.
Toothbrushing Time (in Seconds) and Pre/Post Differences after Seven and Fourteen Days Post-Baseline
| Tooth Surfaces | Baseline n=34 Mean (SD) |
After 7 Days n=34 Mean (SD) |
Pre/Post Difference Mean (SD) |
95% CI* | P-value** |
|---|---|---|---|---|---|
| All surfaces | 46.2 (31.3) | 69.4 (30.4) | 23.1 (31.5) | 12.2, 34.1 | 0.0002† |
| Lingual surfaces | 0.9 (2.3) | 13.2 (14.1) | 12.3 (14.2) | 7.4, 17.3 | <.0001† |
| Buccal surfaces | 30.1 (28.6) | 38.0 (21.7) | 7.8 (21.9) | 0.2, 15.4 | 0.045 |
| Occlusal surfaces | 15.2 (10) | 18.2 (10.5) | 3.0 (11.0) | −0.8, 6.8 | 0.12 |
| Maxillary occlusal surfaces | 5.9 (6.1) | 9.2 (6.3) | 3.3 (5.9) | 1.2, 5.4 | 0.0028† |
| Mandibular occlusal surfaces | 9.3 (6.7) | 9.0 (5.6) | −0.3 (7.9) | −3.1, 2.5 | 0.83 |
| Posterior buccal surfaces | 15.7 (17.7) | 22.8 (14.9) | 7.1 (12.8) | 2.6, 11.6 | 0.0027† |
| Anterior buccal surfaces | 14.5 (14.3) | 15.2 (10.2) | 0.7 (12.5) | −3.7, 5.1 | 0.74 |
| Tooth Surfaces | Baseline n=15 Mean (SD) |
After 14 Days n=15 Mean (SD) |
Pre/Post Difference Mean (SD) |
95% CI* | P-value** |
| All surfaces | 39.9 (21.0) | 108.9 (47.6) | 69.0 (51.2) | 40.7, 97.3 | 0.0001† |
| Lingual surfaces | 0.9 (1.6) | 36.0 (22.3) | 35.1 (22.1) | 22.8, 47.3 | <.0001† |
| Buccal surfaces | 24.5 (18.3) | 45.4 (18.0) | 20.9 (18.0) | 10.9, 30.8 | 0.0005† |
| Occlusal surfaces | 14.4 (10.8) | 27.5 (17.0) | 13.1 (18.6) | 2.7, 23.4 | 0.017† |
| Maxillary occlusal surfaces | 6.5 (7.3) | 13.1 (9.8) | 6.7 (10.5) | 0.8, 12.5 | 0.028 |
| Mandibular occlusal surfaces | 7.9 (5.6) | 14.3 (7.9) | 6.4 (10.0) | 0.9, 11.9 | 0.026 |
| Posterior buccal surfaces | 13.5 (11.5) | 28.4 (11.4) | 14.9 (11.9) | 8.3, 21.5 | 0.0003† |
| Anterior buccal surfaces | 11.1 (9.2) | 17.0 (7.6) | 5.9 (7.6) | 1.7, 10.1 | 0.0089† |
95% confidence interval for the average change between time points
Paired t-test, p-value
Statistically significant after adjustment for multiple testing, Holm’s method (p-value < 0.05)
Exploratory Hypotheses.
For the subset of children who played the game for an additional seven days (n=15 children), the mean total toothbrushing time increased by 69.0±51.2 seconds (95% CI: 40.7, 97.3; P<0.001) (Table 1). Toothbrushing time increased significantly on all surface types after 14 days. Similar to the seven-day results, the largest increase was observed for the lingual surfaces (average increase=35.1 seconds; 95% CI: 22.8, 47.3). At baseline only 26.7% (4/15) of the children had any brushing of the lingual surfaces as compared to 93.3% (14/15) after 14 days (McNemar’s test; P=0.006).
The increases in time and changes in distribution observed after seven days and 14 days were not statistically significant after one year without game play(Table 2). However, there were improvements that failed to reach statistical significance but could be clinically meaningful. For example, in the group of children with 14 days of game play, as compared to baseline, the mean total time increased by 15.1 seconds (P=0.41) and the mean time for lingual surfaces increased by 9.5 seconds (P=0.18). At baseline only 20.0% (2/10) brushed the lingual surfaces compared to 60% (6/10) of the children after one year (McNemar’s test; P=0.13).
Table 2.
Toothbrushing Time (in Seconds) and Pre/Post Differences One-Year after Baseline
| Tooth Surfaces N=14 children who used app for 7 days |
Baseline Mean (SD) |
After 7 Days Mean (SD) |
After One Year Mean (SD) |
Pre/Post Difference Mean (SD) |
95% CI* | P-value** |
|---|---|---|---|---|---|---|
| All surfaces | 40.6 (23.8) | 68.3 (34.9) | 53.9 (47.4) | 13.3 (54.2) | −18.0, 44.6 | 0.38 |
| Lingual surfaces | 0.4 (1.3) | 13.5 (14.9) | 0.9 (3.3) | 0.5 (3.7) | −1.6, 2.7 | 0.60 |
| Buccal surfaces | 26.2 (27.4) | 36.6 (24.3) | 35.5 (34.8) | 9.3 (45.6) | −17.0, 35.6 | 0.46 |
| Occlusal surfaces | 14.0 (8.9) | 18.1 (11.7) | 17.5 (15.5) | 3.5 (12.8) | −3.9, 10.8 | 0.33 |
| Maxillary occlusal surfaces | 4.6 (5.0) | 8.9 (6.6) | 5.0 (5.8) | 0.3 (5.2) | −2.7, 3.3 | 0.82 |
| Mandibular occlusal surfaces | 9.4 (7.6) | 9.2 (7.2) | 12.5 (13) | 3.1 (13.7) | −4.8, 11.1 | 0.41 |
| Posterior buccal surfaces | 12.7 (18.8) | 20.7 (17.5) | 21.5 (24.8) | 8.8 (28.2) | −7.5, 25.1 | 0.26 |
| Anterior buccal surfaces | 13.5 (14.0) | 15.9 (12.0) | 14 (18.6) | 0.5 (26.9) | −15.0, 16.0 | 0.95 |
| Tooth Surfaces N=10 children who used app for 14 days |
Baseline Mean (SD) |
After 14 Days Mean (SD) |
After One Year Mean (SD) |
Pre/Post Difference Mean (SD) |
95% CI* | P-value** |
| All surfaces | 45.7 (23.6) | 119.1 (49.7) | 60.8 (58.1) | 15.1 (55.1) | −24.3, 54.6 | 0.41 |
| Lingual surfaces | 0.8 (1.7) | 38.8 (23.8) | 10.3 (20.2) | 9.5 (20.5) | −5.2, 24.2 | 0.18 |
| Buccal surfaces | 28.8 (21.4) | 49.8 (18.4) | 37.7 (37.4) | 8.9 (35.7) | −16.7, 34.4 | 0.45 |
| Occlusal surfaces | 16.1 (12.5) | 30.5 (19.7) | 12.9 (8.0) | -3.2 (16.8) | −15.2, 8.8 | 0.56 |
| Maxillary occlusal surfaces | 7.8 (8.6) | 14.9 (11.1) | 5.7 (5.1) | -2.1 (10.0) | −9.3, 5.0 | 0.52 |
| Mandibular occlusal surfaces | 8.3 (4.6) | 15.6 (9.4) | 7.2 (4.1) | -1.1 (7.7) | −6.6, 4.4 | 0.66 |
| Posterior buccal surfaces | 14.9 (13.9) | 30.2 (12.1) | 22.7 (20.5) | 7.8 (18.5) | −5.5, 21.0 | 0.22 |
| Anterior buccal surfaces | 13.9 (10.2) | 19.6 (7.5) | 15.0 (21.6) | 1.1 (22.1) | −14.7, 16.9 | 0.88 |
95% confidence interval for the average change between pre-play and one year. See footnote A for exception.
Paired t-test, p-value
Statistically significant after adjustment for multiple testing, Holm’s method (p-value < 0.05)
Discussion
We assessed whether a toothbrushing app could improve toothbrushing quality in children ages 5–6 years. Our data show significant improvements in toothbrushing time and distribution for children who used Brush Up for seven days. Further improvements were observed for a subset of children who used Brush Up for 14 days. In the absence of continued app use, few improvements noted after seven and 14 days appeared to persist after one year. Collectively, these findings suggest that health apps are a promising strategy to improve toothbrushing behaviors in children, but that continual use may be needed to optimize improvements.
There are no published studies to which we can directly compare our findings. However, numerous studies from outside of dentistry have shown improvements in health behaviors associated with apps.18–19 Total toothbrushing time increased by over 50% after seven days and nearly doubled after 14 days of app use (Table 1). These increases are clinically significant given that baseline toothbrushing time was high (46.2 and 39.9 seconds, respectively). Furthermore, there were significant improvements in toothbrushing of previously neglected tooth surfaces, including the lingual and maxillary occlusal surfaces, which are difficult areas to brush for young children.
Mechanism information on how apps like Brush Up improve toothbrushing behaviors is important knowledge that could be used for future app-based interventions. For instance, improvements in toothbrushing were greater for children who used the app for 14 days compared to seven days. This suggests that longer app use may be associated with greater improvements, but the optimal intervention dose is unknown. A related issue is the length of the toothbrushing session. At the time of the study, the Brush Up song lasted three minutes. It may have been possible to achieve similar results with a two-minute song, a refinement that would reduce participant burden. In addition, the repetitiveness of health apps may lead to app fatigue over time. However, this is a positive feature for population subgroups for whom routines are important, including individuals with autism spectrum disorders.6,20 Post-intervention interviews with families and child end-users could help to elucidate ways to optimize, refine, and tailor app-based interventions.
There were three main study limitations: 1) small sample size; 2) study was not a randomized clinical trial; and 3) no assessment of health outcomes. The small sample may explain why we failed to see statistically significant differences at one-year. Our study results are expected to inform sample size calculations for future interventions to ensure an adequately powered randomized clinical trial. Such a study would need to put in place strategies that would allow sufficient follow-up of participants to assess the extent to which longer-term behavior change is possible though app-based interventions. Participant incentives as well as e-incentives built into the app would help maintain participant engagement and follow-up. The third limitation could be overcome by including short- and long-term oral health outcomes assessments to assess whether toothbrushing with mobile games can prevent disease and improve oral health. It important to acknowledge the importance of adult supervision during toothbrushing, to ensure that an appropriate amount of fluoridated toothpaste is being used and to monitor appropriate brushing. We also recognize that caries is a multifactorial disease in which factors beyond toothbrushing such as minimizing added sugar intake and utilizing dental care are important in disease prevention.
In conclusion,
Toothbrushing games can potentially improve toothbrushing quality in children in terms of total brushing time and distribution.
Interventions need to be designed to achieve long-term, sustained improvements in toothbrushing and oral health.
Future research should continue to evaluate mobile games as part of intervention approaches to improve oral health behaviors and outcomes in vulnerable pediatric populations.
Acknowledgments
We would like to thank Brian Daviadoff and Leontyne Robinson for research assistance and formative game development; Stephanie Chergi and Jenna DiLorenzo for game art and animation; Vernon Simms for music production; and Hilario Gonzalez and Adam Gensler for software engineering. The study was funded by the U.S. National Institute for Dental and Craniofacial Research grant nos. R43DE21334 and K08DE020856.
Footnotes
Author Disclosure Statement
GamesThatWork developed the Brush Up game and has an ongoing interest in its success. Two authors (JJ, DJ) are principals of GamesThatWork.
References
- 1.Kumar S, Tadakamadla J, Johnson NW. Effect of toothbrushing frequency on incidence and increment of dental caries: A systematic review and meta-analysis. J Dent Res 2016;95(11):1230–1236. [DOI] [PubMed] [Google Scholar]
- 2.Polk DE, Geng M, Levy S, Koerber A, Flay BR. Frequency of daily tooth brushing: predictors of change in 9- to 11-year old US children. Community Dent Health 2014;31(3):136–140. [PMC free article] [PubMed] [Google Scholar]
- 3.Martins CC, Oliveira MJ, Pordeus IA, Paiva SM. Comparison between observed children’s tooth brushing habits and those reported by mothers. BMC Oral Health 2011;September 3:11:22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sanzone LA, Lee JY, Divaris K, DeWalt DA, Baker AD, Vann WF Jr. A cross sectional study examining social desirability bias in caregiver reporting of children’s oral health behaviors. BMC Oral Health 2013;June 1:13:24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Trubey RJ, Moore SC, Chestnutt IG. Children’s toothbrushing frequency: the influence of parents’ rationale for brushing, habits and family routines. Caries Res 2015;49(2):157–164. [DOI] [PubMed] [Google Scholar]
- 6.Capozza LE, Bimstein E. Preferences of parents of children with autism spectrum disorders concerning oral health and dental treatment. Pediatr Dent 2012;34(7):480–484. [PubMed] [Google Scholar]
- 7.Macgregor ID, Rugg-Gunn AJ. A survey of toothbrushing sequence in children and young adults. J Periodontal Res 1979. May;14(3):225–30. [DOI] [PubMed] [Google Scholar]
- 8.Werner H, Hakeberg M, Dahlström L, Eriksson M, Sjögren P, Strandell A, Svanberg T, Svensson L, Wide Boman U. Psychological interventions for poor oral health: A systematic review. J Dent Res 2016;95(5):506–514. [DOI] [PubMed] [Google Scholar]
- 9.Huebner CE, Riedy CA. Behavioral determinants of brushing young children’s teeth: implications for anticipatory guidance. Pediatr Dent 2010;32(1):48–55. [PMC free article] [PubMed] [Google Scholar]
- 10.Pew Research Center. U.S. smartphone use in 2015 2015. Available at: http://www.pewinternet.org/2015/04/01/us-smartphone-use-in-2015/. Accessed on September 2, 2016.
- 11.Sheehy S, Cohen G, Owen KR. Self-management of diabetes in children and young adults using technology and smartphone applications. Curr Diabetes Rev 2014;10(5):298–301. [DOI] [PubMed] [Google Scholar]
- 12.Quelly SB, Norris AE, DiPietro JL. Impact of mobile apps to combat obesity in children and adolescents: A systematic literature review. J Spec Pediatr Nurs 2016;21(1):5–17. [DOI] [PubMed] [Google Scholar]
- 13.Underwood B, Birdsall J, Kay E. The use of a mobile app to motivate evidence-based oral hygiene behaviour. Br Dent J 2015;219(4):E2. [DOI] [PubMed] [Google Scholar]
- 14.Scheerman JFM, van Meijel B, van Empelen P, Kramer GJC, Verrips GHW, Pakpour AH, Van den Braak MCT, van Loveren C. Study protocol of a randomized controlled trial to test the effect of a smartphone application on oral-health behavior and oral hygiene in adolescents with fixed orthodontic appliances. BMC Oral Health 2018. February 7;18(1):19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hurling R, Claessen JP, Nicholson J, Schäfer F, Tomlin CC, Lowe CF. Automated coaching to help parents increase their children’s brushing frequency: an exploratory trial. Community Dent Health 2013;30(2):88–93. [PubMed] [Google Scholar]
- 16.Schluter P, Lee M, Hamilton G, Coe G, Messer-Perkins H, Smith B. Keep on brushing: a longitudinal study of motivational text messaging in young adults aged 18–24 years receiving Work and Income Support. J Public Health Dent 2015;75(2):118–125. [DOI] [PubMed] [Google Scholar]
- 17.Madan Kumar PD, Mohandoss AA, Walls T, Rooban T, Vernon LT. Using smartphone video “selfies” to monitor change in toothbrushing behavior after a brief intervention: A pilot study. Indian J Dent Res 2016;27(3):268–277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schoeppe S, Alley S, Van Lippevelde W, Bray NA, Williams SL, Duncan MJ, Vandelanotte C. Efficacy of interventions that use apps to improve diet, physical activity and sedentary behaviour: a systematic review. Int J Behav Nutr Phys Act 2016. December 7;13(1):127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fedele DA, Cushing CC, Fritz A, Amaro CM, Ortega A. Mobile Health Interventions for Improving Health Outcomes in Youth: A Meta-analysis. JAMA Pediatr 2017. May 1;171(5):461–469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Epstein A, Whitehouse A, Williams K, Murphy N, Leonard H, Davis E, Reddihough D, Downs J. Parent-observed thematic data on quality of life in children with autism spectrum disorder. Autism 2017. October 1:1362361317722764. [DOI] [PubMed] [Google Scholar]