Abstract
Introduction:
Because of financial pressures, low-income individuals sometimes run out of cellphone service towards the end of the month.
Aims:
To determine if the time of month affects ability to reach low-income smokers by telephone.
Methods:
We reviewed data from a completed trial in the United States of emergency department (ED)-initiated tobacco dependence treatment for low-income smokers at a busy, academic ED in an urban community. We recorded the date of each one-month follow-up call, and divided each month into four time blocks: Week 1, Week 2, Week 3, and Week 4.
Results:
A total of 2,049 phone calls were made to reach 769 participants. Of these calls, 677 (33%) resulted in contact; 88% of all participants were contacted. Using generalised estimating equations with Week 4 as reference, the odds of a successful contact at Weeks 1, 2, and 3 were, respectively, 1.52 (95% CI 1.18, 1.96), 1.30 (95% CI 1.01, 1.66), and 1.37 (95% CI 1.07, 1.76).
Conclusions:
Study participants became progressively difficult to reach. This result may reflect low-income smokers’ decreased rates of active telephone service later in the month and suggests a mechanism to improve follow-up rates in future studies of low-income populations.
Introduction
A common challenge in clinical research is the inability to achieve adequate follow-up of all participants. Inadequate follow-up threatens external validity and the generalizability of study results and conclusions (Leon, Demirtas, & Hedeker, 2007; Woolard, 2004) Studies that focus on low-income or marginalised populations often face additional challenges to achieving adequate follow-up rates, such as increased rates of substance abuse, mental illness, unstable housing, unreliable telephone service, incarceration, and limited or adverse prior experiences with research, although the impact of these challenges on follow-up rates is sometimes unclear (Blumenthal, Sung, Coates, Williams, & Liff, 1995; Cunningham et al., 2008; Ramos-Gomez et al., 2008). Multiple studies report good follow-up rates using strategies such as using multiple modes of contact, including reminder mailings about upcoming follow-up dates, frequent participant contact and incentives for updating contact information, although there is a paucity of information focused on maximising follow-up rates specifically in low-income populations (Cunningham et al., 2008; Twitchell, Hertzof, Klein, & Schuckit, 1992; Walton, Ramanathan, & Reischl, 1998; Warner et al., 2013).
Though little has been reported on how to maximise the yield of each contact attempt, several studies highlight the success and importance of repeated follow-up attempts. One study of 608 located repeat driving under the influence (DUI) offenders reported 70% follow-up completion of participants at 19 calls, 79.6% completion at 40 calls, and 80.3% at 70 calls (Kleschinsky, Bosworth, Nelson, Walsh, & Shaffer, 2009). The importance of increased follow-up rates is augmented by research that highlight important differences between easier and harder-to-reach populations. A longitudinal study investigating Attention Deficit Hyperactivity Disorder, Conduct Disorder (CD), and Oppositional Defiant Disorder (ODD) found that participants requiring more than 20 contact attempts to complete follow-up were significantly more likely to have CD and ODD (Cotter, Burke, Stouthamer-Loeber, & Loeber, 2005). An Emergency Department (ED) based study of predominantly low income cocaine users reported differences in age, substance abuse diagnosis and concurrent mental health treatment in study enrollees that were more difficult to reach, which highlights the importance of high follow-up rates for study validity (Cunningham et al., 2008).
In a recently reported clinical trial of an ED-initiated intervention for low-income smokers (Bernstein et al., 2015), our research staff observed that it seemed more difficult to contact subjects by telephone later in the month. We suspected that this might result from a higher likelihood of phone service disconnection later in the month, due to the exhaustion of public assistance resources that are distributed at the beginning of the month. We reviewed PubMed and Scopus for English-language articles published between 1994 and 2014 using the keywords “low-income”, “follow-up”, “weekly variability,” “end of the month,” and “contact attempt(s)” and did not identify any studies evaluating variation in ability to reach low-income populations by time of month, or in relation to “payday” or receipt of public assistance.
Our hypothesis was that the odds of successfully reaching a subject by phone would be higher in the first week of the month, and decrease with each subsequent week. If true, this finding would have implications for planning follow-up in clinical trials and clinical care focusing on low-income populations.
Methods
Study Design
This study is a secondary analysis of the one month follow-up calls in a single-hospital two-arm randomised trial of a multicomponent intervention for adult smokers presenting to the ED (Bernstein et al., 2015). The details of study enrolment, including the CONSORT diagram, have been previously reported (Bernstein et al., 2015). The primary study intervention consisted of a brief motivational interview, initiation of nicotine replacement therapy in the ED, provision of six weeks of nicotine replacement therapy, and referral to the state smokers’ quitline. Provision of one telephone number was required for entry into the study, although additional contact numbers were recorded if available. Study personnel did not ask participants whether the telephones were cell phones or land lines. Our institution’s Human Investigation Committee approved this study. All participants participated in informed consent, including an in-person explanation of the potential risks and benefits of participating in the study.
Setting
A level I trauma academic medical centre ED that treats 90,000 adults per year in a medically underserved urban community. Study participants were enrolled from October 2010 to December 2012.
Inclusion criteria
Patients were eligible if they were at least 18 years of age, spoke English, had Medicaid or no insurance, were able to give written informed consent, smoked at least 100 cigarettes lifetime and were currently every- or some-day smokers.
Exclusion Criteria
Patients were excluded if they lived out of state, were too ill to give consent, presented primarily with a psychiatric problem, were pregnant or nursing, in police custody, had a history of allergy to nicotine replacement products, were currently in treatment for tobacco dependence, or were leaving the ED against medical advice.
Incentives
At enrolment, all participants were given $10 gift cards for a local retailer, with additional payments of $25 at each telephone follow-up. The consent document informed subjects of the amount and timing of payments.
Follow-Up Protocol
Follow-up calls were placed to all subjects at one, three, and twelve months after enrolment. Follow-up calls were placed on the day follow-up was due based on the enrolment date and were repeated over a two-week period, including nights and weekends, until either the follow-up was completed or the two-week eligibility period was closed.
Whether research assistants were able to reach each of the 769 participants during each of the 2,049 phone calls was logged in an Excel (Microsoft, Redmond, WA) spreadsheet. Within a two-week period after one-month follow-up, an unlimited number of phone calls were made. No additional calls were logged after the participant was reached. A telephone conversation of any kind counted as being able to “reach” the participant, even if the follow-up questionnaire was not completed. Calls were made by research assistants blinded to group assignment, between the hours of 8 am and 9 pm, seven days per week, except for major holidays. Study participants were called at varying times of day and week to maximise the likelihood of contact.
In addition to participants who we were never able to reach by telephone, study participants who were deceased, incarcerated, or residing in an inpatient psychiatric, drug or alcohol treatment facility were considered unreachable and not included in the analysis. Patients who had their one-month follow-up completed while hospitalised at the study hospital during their follow-up period were considered reachable.
Methods of Measurement
Of the 778 participants enrolled in the primary study, detailed call logs for one-month follow-up calls were available for 769 participants. Only calls made for one-month follow-up were included based on maximal contact rates. We recorded the date of each call, and divided each month into four time blocks: Week 1, Week 2, Week 3, and Week 4 (days 22–31). Data were analysed with descriptive statistics and generalised estimating equations (GEE) using SAS (SAS Institute, Cary, NC) to account for clustering of calls within subjects. Covariates included in the model were subject sex, age, race, ethnicity, educational attainment, insurance status, and disposition from the ED (admitted or discharged.) Alpha for significance was set at 0.05. Univariate and bivariate data were analysed with parametric and categorical methods, as appropriate.
Results
The study participants’ mean age was 40.5 years; 47.7% were male; 39.2% were white, 39.6% African-American, 20.3% Hispanic, and 0.9% Asian or other. Of all subjects, 15.7% were uninsured, and the remainder had Medicaid. There were no differences between groups in baseline characteristics, as noted in Table 1.
Table 1.
Description of subjects
| Variable | Reached by Phone N = 663 | Not Reached by Phone N = 106 | P Value |
|---|---|---|---|
| Age, years, mean (SD) | 40.5(11.6) | 39.6(11.3) | 0.44 |
| Male sex, N (%) | 313(47.2) | 52 (49.1) | 0.72 |
| Race/Ethnicity, N (%) | |||
| White | 256 (38.6) | 46 (43.4) | 0.79 |
| Black/African-American | 268 (40.4) | 38 (35.8) | |
| Hispanic | 133 (20.1) | 21 (19.8) | |
| Other | 6 (0.9) | 1 (0.9) | |
| Education level, N (%) | |||
| Grades 1–8 (elementary) | 26 (3.9) | 4 (3.8) | 0.32 |
| Grades 9–11 (some high school) | 184 (27.8) | 25 (23.6) | |
| Grade 12 or GED (high school graduate) | 303 (45.7) | 43 (40.6) | |
| College 1–3 years (some college or technical school) | 135 (20.4) | 30 (28.3) | |
| College 4 years or more (4-year college graduate) | 15(2.3) | 4 (3.8) | |
| Insurance, N (%) | |||
| Self-pay/None | 107 (16.1) | 13(12.3) | 0.74 |
| Medicaid | 516(77.8) | 87 (82.1) | |
| Other (Medicaid/Medicare, other state insurance) | 40(6.1) | 6 (5.7) | |
| Disposition from ED, N (%) | 0.50 | ||
| Discharged | 462 (69.7) | 79 (74.5) | |
| Admitted | 198(29.9) | 27 (25.5) | |
| Walked out/Left against medical advice | 3 (0.5) | 0(0) |
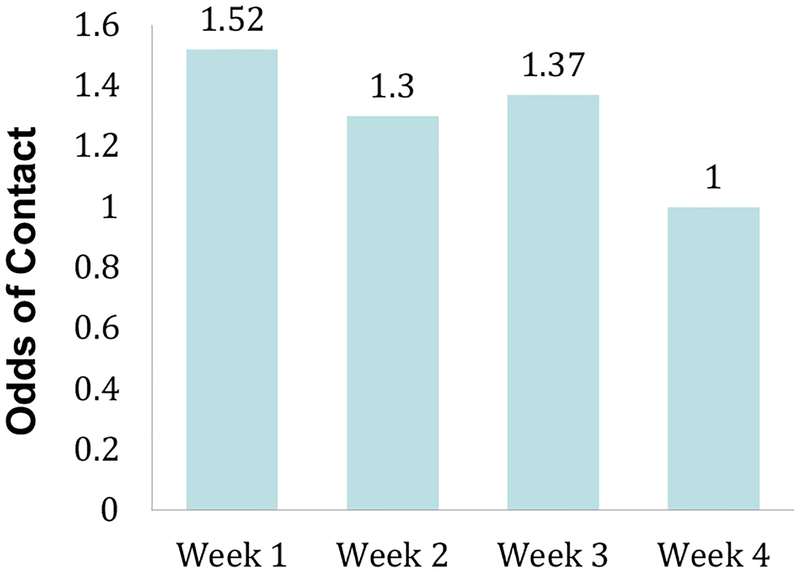
A total of 2,049 phone calls were made to reach 769 participants. Of these calls, 677 (33%) resulted in participant contact. The proportion of successful calls made at Weeks 1, 2, 3, and 4 were, respectively, 34.4%, 30.8 %, 32.1%, and 34.4%. Using GEE modelling to account for clustering with Week 4 as reference, the odds of a successful contact at Weeks 1, 2, and 3 were, respectively, 1.52 (95% CI = [1.18, 1.96]), 1.30 (95% CI = [1.01, 1.66]), and 1.37 (95% CI = [1.07, 1.76]). Data are summarised in Figure 1. Subject age, gender, race, education level, insurance status and ethnicity were not associated with odds of successful contact.
Figure 1.
Odds of participant contact by telephone at one month. Using generalised estimating equations (GEE) modelling with Week 4 as reference, the odds of a successful contact at Weeks 1, 2, and 3 were, respectively, 1.52 (95% CI = [1.18,1.96]), 1.30 (95% CI = [1.01, 1.66]), and 1.37 (95% CI = [1.07, 1.76]).
Discussion
In a study of 769 low-income adult smokers visiting a single ED in the north-eastern US, subjects were easiest to reach by phone in the first week of the month, with decreased odds of contact in subsequent weeks, and lowest in the final week. The association between timing of call and odds of contact, to our knowledge has not been previously reported and suggests a potential method to reduce attrition in a broad range of research involving low-income populations.
Although likely multifactorial, one plausible hypothesis for our decreased ability to reach participants during the last week of the month may be related to decreased access to active telephone service. Based on spending patterns observed in low-income households (Stephens, 2003) and literature describing increased food scarcity at the end of the month, we suspect that the variation in ability to reach low-income patients is most likely related to greater availability of active telephone service, particularly cell phones, early in the month.
In the United States, virtually all public assistance including supplemental security income (SSI), SSI with disability insurance, Temporary Assistance for Needy Families, and Supplemental Nutrition Assistance Program are distributed in the first few days of the month (“DSS: How to Access Cash and Supplemental Nutrition Assistance Program (SNAP) Benefits,” n.d.; Security Administration & of Communications, 2012). As the month progresses, available resources decrease and food insecurity increases in low-income populations (Tarasuk, McIntyre, & Li, 2007). We suspect, therefore, that more participants are able to pay for their phone service early in the month, although we acknowledge the existence of other possibilities such as increased time away from home at work or procuring food or decreased time available to answer the phone.
Prior studies demonstrated the improved financial position of low-income households early in the month. These households demonstrate increased spending early in the month, after monthly paycheck or public assistance disbursement, and increased food insecurity towards the end the month (Hamelin, Beaudry, & Habicht, 2002; Hastings & Washington, 2010; Seligman, Bolger, Guzman, López, & Bibbins-Domingo, 2014; Stephens, 2003; Tarasuk et al., 2007; Thompson et al., 1988). An analysis published in 2003 describes a 7–20% increase above mean expenditures in the week following receipt of Social Security benefits by families whose benefits constitute more than 70% of their income, with an 80% increase in spending on the day of benefit receipt (Stephens, 2003). Correspondingly, multiple studies report increased food insecurity in low-income populations with declining food expenditures, decreased consumption of vegetables and milk products, decreased overall calorie consumption, and increased use of soup kitchens at the end of the month, all of which were attributed to exhaustion of monetary resources (Hamelin et al., 2002; Hastings & Washington, 2010; Tarasuk et al., 2007; Thompson et al., 1988). Thompson et al. (1988) reported a 43% increase in the number of meals served by an Upstate New York soup kitchen in the last compared to the first week of the month (Thompson et al., 1988).
This phenomenon is consistent with California hospital admission data from 2000 to 2008. A study evaluating hospital admissions found a 27% increase in admissions for hypoglycaemia for low-income diabetics in the last calendar week of the month compared to the first week (Seligman et al., 2014). A more recent study, found increased odds of ED visit or hospital admission for hypoglycaemia in patients with household incomes less than the national median during Week 4 compared to earlier weeks (Basu, Berkowitz, & Seligman, 2017). Overall, studies show that low-income households struggle with paying for basic needs towards the end of the month, including food, which would be a heavily competing priority for households who purchase cell phone minutes only when they can afford them.
Limited telephone service at the end of the month due to competition for finite resources would be much more likely in households with predominantly cellular phone service plans, in which one buys minutes as needed rather than a monthly bill for a land line. Data from the National Health Interview Survey (NHIS) from 2010 to 2012 showed that the proportion of wireless-only phone services in households below the poverty line, at 100–200% of the poverty line, and >200% of the poverty line, increased, respectively, from 42.8–54.3%, 35.2–45.9%, and 21.7–33.2% (Blumberg & Luke, 2013) 20. Another recent study reported cell phone ownership of 74% among 1,898 individuals with annual incomes less than $20,000 (Purnell, Griffith, Eddens, & Kreuter, 2014).
Disconnection of phone service occurs for many low-income patients. In a 2012 survey of predominantly low-income (70% with annual income < $35,000) participants, 27.3% reported disconnection of phone service in the previous 24 months (Warner et al., 2013). Another study of repeat offenders for DUI reported disconnected telephone service in one-third of participants. Over time, investigators were able to complete follow-up in 93 of the 243 (39.7%) participants that had disconnected phone service (Kleschinsky et al., 2009). This suggests that telephone disconnection is frequently a transient phenomenon, although the study did not examine the association between the timing of calls and the likelihood of contact. It is also possible that the variation is not entirely due to disconnected phone service, as cell phone users may engage in more aggressive screening of phone calls later in the month to “save” minutes for emergencies. Although they did not evaluate whether time of month was related, study participant concern over the personal cost of using cell phone minutes to participate in research follow-up has been previously described as a reason for refusing to participate in follow-up phone calls (Kleschin-sky et al., 2009)9. As supported by NHIS data (Blumberg & Luke, 2013) that suggest increase rates of wireless-only households in low-income populations, we suspect that most of our participants were cell phone users, although unstable housing likely played some role in our contact patterns.
Though disconnection or non-use of telephone services as economic resource scarcity increases during at the end of the month is our leading hypothesis, other factors are plausible. Participants may have been more difficult to reach at the end of the month if they provided a land line phone for contact, if they were more frequently eating outside of the house in the homes of friends or family with less food insecurity, or if they were more frequently eating out of the house at soup kitchens, which have been shown to be busier at the end of the month (Thompson et al., 1988). Another possibility is that individuals with tip-based or cash-based employment may be working more, or have “picked up extra shifts” at the end of the month in an attempt to offset the monthly fluctuation of resources and are therefore less available to participate in study follow-up.
Regardless of the aetiology of our findings, this work may have implications both for clinical care and research. Lessons learned from this study include (1) the importance of persistence – more follow-up calls continue to increase the likelihood of reaching an individual, (2) variation in time of day, day of week, and time of month may increase likelihood of reaching a patient for follow-up, (3) texting was an effective method for reaching participants in some cases (although we did not consistently collect text data, we were able to establish contact and arrange a convenient time for telephone follow-up in some cases).
The study has several limitations. We did not ask subjects what kind of phone service they have, or whether they “conserve” minutes as the month progresses, so we cannot make inferences about our inability to reach specific subjects. We also do not have information about the billing cycle for participants’ telephone service plans, although anecdotal evidence from our subjects indicates that many are on “pay as you go” plans and purchase additional cell phone minutes when needed, and when they have funds to do so. As a proxy for low-income, we used insurance status. Most subjects on Medicaid or who are uninsured are low income, but we did not explicitly ask about household income. Finally, we did not ask our subjects whether they receive public assistance (other than Medicaid), or the relationship between receipt of public assistance and their household income spending habits.
Conclusion
Low-income smokers showed a near-monotonic decrease throughout the month in the ability to be reached by phone. Our findings suggest that follow-up may be maximised by “front-loading” phone calls earlier in the month. This is a testable hypothesis that can be assessed in future trials.
Funding
R01CA141479, K12DA033312.
Footnotes
Conflicts of Interest
The authors have no conflicts of interest to report.
References
- Basu S, Berkowitz SA, & Seligman H (2017). The monthly cycle of hypoglycemia. Medical Care, 55(7), 639–645. Retrieved from 10.1097/MLR.0000000000000728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernstein SL, D’Onofrio G, Rosner J, O’Malley S, Makuch R, Busch S et al. (2015). Successful tobacco dependence treatment in low-income emergency department patients: A randomized trial. Annals of Emergency Medicine,66(2), 140–147. Retrieved from 10.1016/j.annemergmed.2015.03.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blumberg SJ, & Luke JV (2013). Wireless substitution: Early release of estimates from the national health interview survey, January–June 2013. Retrieved from https://www.cdc.gov/nchs/data/nhis/earlyrelease/wireless201312.pdf.
- Blumenthal DS, Sung J, Coates R, Williams J, & Liff J (1995). Recruitment and retention of subjects for a longitudinal cancer prevention study in an inner-city black community. Health Services Research, 30(1 Pt 2), 197–205. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/7721592. [PMC free article] [PubMed] [Google Scholar]
- Cotter RB, Burke JD, Stouthamer-Loeber M, & Loeber R (2005). Contacting participants for follow-up: How much effort is required to retain participants in longitudinal studies? Evaluation and Program Planning, 28, 15–21. Retrieved from 10.1016/j.evalprogplan.2004.10.002. [DOI] [Google Scholar]
- Cunningham R, Walton MA, Tripathi SP, Outman R, Murray R, & Booth BM (2008). Tracking inner city substance users from the emergency department: How many contacts does it take? Academic Emergency Medicine: Official Journal of the Society for Academic Emergency Medicine, 15(2), 136–143. Retrieved from 10.1111/j.1553-2712.2008.00033.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DSS: How to Access Cash and Supplemental Nutrition Assistance Program (SNAP) Benefits. (n.d.). Retrieved September 7, 2017 https://www.ct.gov/dss/cwp/view.asp?a=2349&q=304628.
- Hamelin A-M, Beaudry M, & Habicht J-P (2002). Characterization of household food insecurity in Québec: Food and feelings. Social Science & Medicine (1982), 54(1), 119–132. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/11820676. [DOI] [PubMed] [Google Scholar]
- Hastings J, & Washington E (2010). The first of the month effect: Consumer behavior and store responses. American Economic Journal: Economic Policy, 2(2), 142–162. Retrieved from 10.1257/pol.2.2.142. [DOI] [Google Scholar]
- Kleschinsky JH, Bosworth LB, Nelson SE, Walsh EK, & Shaffer HJ (2009). Persistence pays off: Follow-up methods for difficult-to-track longitudinal samples. Journal of Studies on Alcohol and Drugs, 70(5), 751–761. Retrieved from 10.15288/jsad.2009.70.751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leon AC, Demirtas H, & Hedeker D (2007). Bias reduction with an adjustment for participants’ intent to dropout of a randomized controlled clinical trial. Clinical Trials (London, England), 4(5), 540–547. Retrieved from 10.1177/1740774507083871. [DOI] [PubMed] [Google Scholar]
- Purnell JQ, Griffith J, Eddens KS, & Kreuter MW (2014). Mobile technology, cancer prevention, and health status among diverse, low-income adults. American Journal of Health Promotion: AJHP, 28(6), 397–402. Retrieved from 10.4278/ajhp.120816-ARB-396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramos-Gomez F, Chung LH, Gonzalez Beristain R, Santo W, Jue B, Weintraub J et al. (2008). Recruiting and retaining pregnant women from a community health center at the US-Mexico border for the mothers and youth access clinical trial. Clinical Trials (London, England), 5(4), 336–346. Retrieved from 10.1177/1740774508093980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Security Administration S., & of Communications O. (2012). Schedule of social security benefit payments 2012. Retrieved September 7, 2017 https://www.ssa.gov/pubs/calendar2012.pdf.
- Seligman HK, Bolger AF, Guzman D, López A, & Bibbins-Domingo K (2014). Exhaustion of food budgets at month’s end and hospital admissions for hypoglycemia. Health Affairs (Project Hope), 33(1), 116–123. Retrieved from 10.1377/hlthaff.2013.0096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stephens MJ (2003). “3rd of the Month”: Do social security recipients smooth consumption between checks? The American Economic Review. American Economic Association; Retrieved from 10.2307/3132184. [DOI] [Google Scholar]
- Tarasuk V, McIntyre L, & Li J (2007). Low-income women’s dietary intakes are sensitive to the depletion of household resources in one month. The Journal of Nutrition, 137(8), 1980–1987. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/17634274. [DOI] [PubMed] [Google Scholar]
- Thompson FE, Taren DL, Andersen E, Casella G, Lambert JK, Campbell CC et al. (1988). Within month variability in use of soup kitchens in New York State. American Journal of Public Health, 78(10), 1298–1301. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/3421384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Twitchell GR, Hertzof CA, Klein JL, & Schuckit MA (1992). The anatomy of a follow-up. Addiction, 87(9), 1327–1333. Retrieved from 10.1111/j.1360-0443.1992.tb02741.x. [DOI] [PubMed] [Google Scholar]
- Walton MA, Ramanathan CS, & Reischl TM (1998). Tracking substance abusers in longitudinal research: Understanding follow-up contact difficulty. American Journal of Community Psychology, 26(2), 233–253. Retrieved from 10.1023/A:1022128519196. [DOI] [PubMed] [Google Scholar]
- Warner ET, Glasgow RE, Emmons KM, Bennett GG, Askew S, Rosner B et al. (2013). Recruitment and retention of participants in a pragmatic randomized intervention trial at three community health clinics: Results and lessons learned. BMC Public Health, 13(1), 192 Retrieved from 10.1186/1471-2458-13-192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woolard RH (2004). Research fundamentals: Follow-up of subjects in clinical trials: Addressing subject attrition. Academic Emergency Medicine, 11(8), 859–866. Retrieved from 10.1197/j.aem.2003.09.021. [DOI] [PubMed] [Google Scholar]