Abstract
Objective: Opioid pain medications are commonly prescribed postsurgically for pain. Few studies have investigated the effects of Battlefield Acupuncture (BFA) on postsurgical pain and pain-medication use. To date, no studies have investigated BFA's effectiveness for reducing postoperative shoulder pain and pain-medication use post surgery. The objective of this study was to determine if adding BFA to a rehabilitation protocol was effective for reducing pain and use of prescribed pain medications, compared to that protocol alone after shoulder surgery.
Materials and Methods: Forty Department of Defense beneficiaries (ages 17–55) were randomized to either a standard-of-care group or a standard-of-care + BFA group prior to shoulder surgery. The standard BFA protocol was administered with semipermanent acupuncture needles emplaced on the subjects' ears for 3–5 days within 24 hours after shoulder surgery in an outpatient physical therapy setting. BFA was reapplied, as needed, up to 6 weeks postsurgically for pain management in the intervention group. The primary outcomes were visual analogue scale (VAS) pain rating and daily pain medication use by each subject. Secondary outcome measures were the Global Rating of Change and Patient Specific Functional scale. Outcome measures were obtained at 24 hours, 72 hours, 1 week, 2 weeks, and 6 weeks post surgery.
Results: Significant differences in average and worst VAS pain change scores were noted between baseline and 7 days (P < 0.05). The main effect for time was significant (average and worst VAS pain) at all timepoints (P < 0.05), without time–group interactions seen. No significant differences between the groups in pain-medication use were observed (P > 0.05)
Conclusions: BFA reduced postsurgical shoulder pain significantly between the groups' average and worst pain change scores between baseline and 7 days despite similar opioid and nonsteroidal anti-inflammatory drug use between the groups.
Keywords: Battlefield Acupuncture, opioids, pain medication, postsurgical medications, shoulder surgery
Introduction
Opioids were involved in more than 60% of drug-related overdose deaths in 2016, increasing 3% from 2015.1 Prescription opioid use and abuse is at an epidemic level in the United States.2 The Centers for Disease Control and Prevention estimates more than 260 million opioid prescriptions are written annually.1 The Veterans Health Administration (VHA) observed the average length of postoperative opioid use in postsurgical patients to be 15 days.3 Due to the nature of the military's work in austere environments and the need for constant deployment readiness, prolonged use of prescribed pain medications (opioids specifically) limits readiness drastically. Side-effects from narcotic pain medications increase duty limitations directly.
Battlefield Acupuncture (BFA) is an integrative pain-treatment option for sailors, airmen, marines and soldiers to decrease prescription medication usage4–7 that does not replace Western medical evidence-based practice.
BFA, a specific auricular-acupuncture technique developed in 2001 by Richard C. Niemtzow, MD, PhD, MPH, is used widely among civilian and military medical providers to treat pain.4 This protocol has been taught in all branches of the Department of Defense (DoD) in efforts to provide alternatives to side-effect–laden prescription and over-the-counter (OTC) pain medications.4 BFA and other integrative medicine topics have been taught at the Uniformed Services University of Health Sciences since 2006.4 Suggested chemical mechanisms for BFA's effectiveness are inhibition of neurotransmitters and inflammatory markers, such as substance P and interleukins, along with endogenous opioid release.8,9 Research using functional magnetic resonance imaging (fMRI) and positive electron tomography have shown that auricular acupuncture attenuates pain sensation within the sensory cortex.10
Dr. Niemtzow named this protocol, Battlefield Acupuncture due to its effect on in pain control in austere environments.5 Although this treatment has been taught widely to medical providers, there is minimal scientific evidence on how it reduces the perception of pain and there is inconsistent evidence on BFA's impact on postoperative pain medication use. Studies have shown inconsistent outcomes with respect to reported pain in patients who received BFA over 24–72-hour durations post knee and hip surgery,.11,12 The outcomes in BFA research show trends for decreased nonsteroidal anti-inflammatory drug (NSAID) use (amount and length of usage) in the short-term (within 72 hours), but these observations have only been clinically significant.11,12 There is a growing body of evidence supporting the use of BFA for treating acute and chronic pain.11,13–18 To date, no studies have investigated the use of BFA for patients after shoulder surgery, and BFA's impact on pain and prescription pain-medication use.
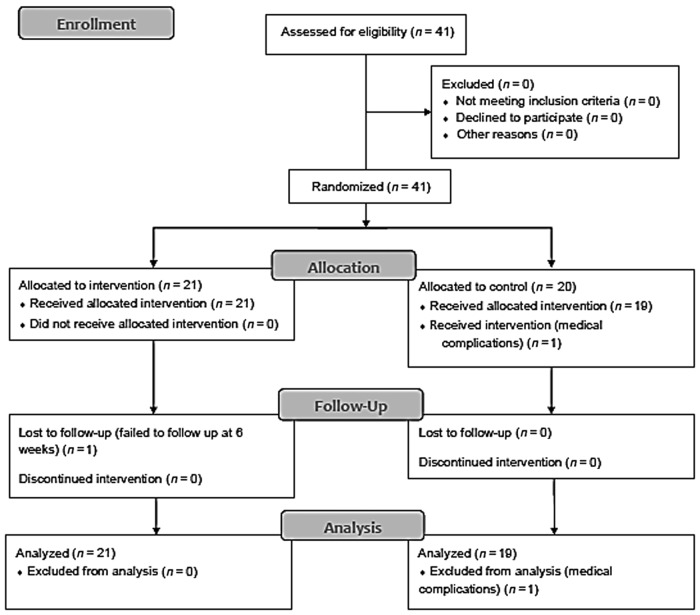
The purpose of this randomized clinical trial was to investigate the effectiveness of BFA for reducing postsurgical pain-medication use and pain when added to usual postsurgical care, compared to usual postsurgical care alone. Secondary outcome measures included the Patient Specific Functional Scale (PSFS)19 and Global Rating of Change (GROC).20 This study met Consolidated Standards Of Reporting Trials (CONSORT; Fig. 1) and Standards for Reporting Interventions in Clinical Trials of Acupuncture (STRICTA) guidelines for randomized clinical trials, with added BFA as the intervention. The authors' hypothesis was that pain-medication use and pain would be reduced significantly in the intervention group, compared to the standard-of-care–alone group in the first 2 weeks post surgery.
FIG. 1.
Study Consolidated Standards Of Reporting Trials (CONSORT; 2010) diagram of subject allocation. Recruitment was goal N = 40; some subjects were withdrawn from the study (1 for medical complications).
Materials and Methods
A convenience sample of 41 DoD beneficiaries, enrolled at the Keller Army Community Hospital at West Point, NY and the U.S. Military Academy (USMA), also at West Point, was recruited after scheduling shoulder surgery. The inclusion criteria were DoD beneficiaries, ages 17–55, and status post shoulder surgery, as well as consent to participate in this study. The exclusion criteria were self-reported pregnancy, history of bloodborne pathogens/infectious diseases/active infections/metal allergy, bleeding disorders, and participants who were not fluent in English.
Subject randomization and group assignment were performed by a noninterested third party using an electronic random-number generator. Group assignment was performed prior to the study commencing in an opaque envelope and attached to the respective subject's folder. After subject consent was obtained, the group assignment envelope was opened by the primary investigator. Subjects were not blinded to group assignment, because, for BFA. the needles (Sedatelec Aiguille Semipermanente®; ASP® gold needles) are worn for 3–5 days, semipermanently in the patient's ears.5,7
The sample size was calculated a priori with G Power 3.1.2 software and determined that 17 subjects per group would provide adequate power to detect any differences in the primary outcomes. It was assumed that for 4 visits in the first 2 weeks and an estimated η2 effect size of 0.4 (a very large effect size)21,22 between groups for pain and opioid-pill count reduction between groups, a sample size of 34 would be needed with α = 0.05 and ß = 0.8. The recruitment goal was 40 subjects to account for potential attrition.
Standard treatment (which was given to the control group) is defined as usual postsurgical care to include surgery-specific protocols, therapeutic modalities, and prescribed/over-the-counter pain medications. The intervention group received BFA in addition to standard postsurgical treatment.
The primary and associate investigators were certified in BFA by Dr. Niemtzow prior to the start of this study. All investigators were experienced active-duty physical therapists (U.S. Army, Navy, Air Force), board-certified in orthopedic and/or sports physical therapy, and credentialed in dry needling.
The aforementioned Sedatelec ASP gold needles were used in the intervention group. These semipermanent, gold-plated acupuncture needles are sterile and for single use in BFA (Figs. 2 and 3). Subjects in the BFA group were given acupuncture treatment by the primary or associate investigators who were certified in BFA according to their group. The subjects' ears were cleaned with alcohol swabs prior to receiving BFA.5 The subjects had the semipermanent needles inserted into some or all the following BFA points on one or both ears, depending on the patients' clinical responses: Cingulate Gyrus; Thalamus; Omega 2; Point Zero; and Shen Men (in that order; Fig. 2).5,7 BFA treatment consists of using up to 5 ASP needles in each ear, but, if a patient reported pain reduction to 0–1 of 10 (on a numeric pain-rating scale), the acupuncture procedure was stopped at that insertion point.5,7 No additional needle stimulation (manual, electrical) was provided through the inserted semipermanent ASP® needles during the intervention timeframe (6 weeks post surgery). The number of BFA treatments was dictated by each subject's response (i.e., current pain level) and desire for further BFA treatments. ASP needles, being semi-permanent, are designed to stay in the ear for 3–5 days. Subjects were instructed to allow the needles to fall out on their own, per Dr. Niemtzow's protocol.5,7 Subjects were also instructed on the removal of the ASP needles (if they became irritants or a nuisance) and about ear hygiene during participation in the study.
FIG. 2.
Battlefield Acupuncture points in order (from bottom to top): Cingulate Gyrus; Thalamus; Omega 2; Point Zero; And Shen Men.
FIG. 3.

Sedatelec Aiguille Semipermanente® gold stainless-steel needles and applicator. Source for image from http://www.fiveelementtcm.com
Concurrent to the BFA treatment, the intervention group also received standard postsurgical care for their respective shoulder surgeries with an approved protocol. The supervising medical provider (physical therapist, athletic trainer) managed outpatient rehabilitation treatment frequency, intensity, and progression.
The control group received standard postsurgical care for their respective shoulder surgeries (e.g., Bankart repair, etc.). The supervising provider (physical therapist, athletic trainer, etc.) governed outpatient rehabilitation treatment frequency, intensity, and progression. Both groups received appropriate home exercise programs per their respective shoulder surgeries.
Outcome assessment was performed at 24 hours, 72 hours, 7 days, 14 days, and 6 weeks after surgery. An intention-to-treat analysis was planned with the last observation carried forward for any missing data.
Data were analyzed using the IBM Statistical Package for the Social Sciences, version 25 (SPSS version 25) and R software version 3.4.4. A 2 × 5 mixed-model analysis of variance (ANOVA) with Sidak's post hoc testing was used with time as the within-subjects factor, and group (control or BFA) as the between-subjects factor.
This study's independent variables (Table 1) were group assignment (intervention and control) and time (baseline at 24 hours, 72 hours, 1 week, 2 weeks, and 6 weeks). The dependent variables were the daily pill log (pain-medication use), visual analogue scale (VAS)23 for pain, GROC scores,19,20 and PSFS scores.19 The VAS for pain, commonly used to assess pain perception clinically, has good reliability and validity.23–25 The GROC quantifies perceived improvement or decline relative to an intervention.20 The clinimetric properties of the GROC (high face validity, good reliability, and sensitivity to change) allow patients to account for changes in pain, function, and ability while judging patients' physical improvements or regressions.20,26 The PSFS has demonstrated good reliability and validity among patients with upper-extremity and shoulder pathology.19,27–29
Table 1.
Independent Variables & Dependent Variables in the Study
| Independent variables | Dependent variables |
|---|---|
| Group assignment: | |
| Control/Interventiona | Daily pill log |
| Time: | VAS for pain24 |
| 24hours | |
| 72 hours | |
| 1 week | GROC19,20 |
| 2 weeks | PSFS19 |
| 6 weeks |
Intervention = Battlefield Acupuncture and standard postsurgical care/Control = standard postsurgical care.
VAS, visual analogue scale; GROC, Global Rating of Change; PSFS, Patient Specific Functional Scale.
Results
A total of 41 subjects gave consents and were enrolled into the study, of which 1 subject was withdrawn from the study after randomization (due to a medical complication). The intervention and control groups consisted of 21 and 19 subjects, respectively. Figure 1 shows a flow diagram of recruitment and retention for this trial. Subject descriptive statistics are shown in Tables 2, 3, and 4.) The CONSORT diagram in Figure 1 depicts preliminary subject allocations, follow-ups, and analyses during the study.
Table 2.
Battlefield Acupuncture Subjects' (N = 40) Baseline Descriptive Statistics
| Demographics | Mean (95% CI) | SD | SEM | Skewness | Kurtosis |
|---|---|---|---|---|---|
| Age (yr) | 20.27 (20.26–20.28) | 1.39 | 0.22 | 0.16 | −0.29 |
| College (yr) | 2.54 (2.53–2.55) | 1.07 | 0.17 | 0.03 | −1.22* |
| Gender | 31M/9Fa | 0.42 | 0.067 | 1.37* | −0.14 |
| Height (cm) | 179.13 (176.51–181.75) | 8.19 | 1.29 | −0.12 | −0.75 |
| Mass (kg) | 79.68 (75.97–83.39) | 11.59 | 1.83 | 0.25 | −0.13 |
Nonnormal data distribution.
Females accounted for 29% of the study population, exceeding the male and female census at the U.S. Military Academy.30
CI, confidence interval; SD, standard deviation; SEM, standard error of the mean; yr, years, M, male; F, female.
Table 3.
Battlefield Acupuncture Control Cohort's (N = 19) Baseline Descriptive Statistics
| Demographics | Mean (95% CI) | SD | SEM | Skewness | Kurtosis |
|---|---|---|---|---|---|
| Age (yr) | 20.5 (20.48–20.52) | 1.23 | 0.28 | 0.15 | −0.95* |
| College (yr) | 3.5 (3.49–3.51) | 0.98 | 0.23 | −0.17 | −0.8* |
| Gender | 14M/5Fa | 0.45 | 0.1 | 1.17* | −0.72* |
| Height (cm) | 176.46 (172.92–180.01) | 7.35 | 1.68 | −0.13 | −0.65 |
| Mass (kg) | 78.16 (73.48–82.84) | 9.72 | 2.23 | −0.482 | 0.633 |
Nonnormal data distribution.
Females accounted for 35% of the control cohort, exceeding the current gender census at the U.S. Military Academy.30
CI, confidence interval, SD, standard deviation; SEM, standard error of the mean; yr, years; m, male; F, female.
Table 4.
Battlefield Acupuncture Intervention Cohort's (N = 21) Baseline Descriptive Statistics
| Demographics | Mean (95% CI) | SD | SEM | Skewness | Kurtosis |
|---|---|---|---|---|---|
| Age (yr) | 20.33 (20.31–20.35) | 1.56 | 0.34 | −0.36 | −0.05 |
| College (yr) | 2.52 (2.51–2.54) | 1.17 | 5.79 | 0.53 | −1.46 |
| Gender | 17M/4Fa | 0.4 | 0.087 | 1.7* | 0.97* |
| Height (cm) | 181.55 (177.76–185.34) | 8.33 | 1.82 | −0.36 | −0.7 |
| Mass (kg) | 81.06 (75.07–87.05) | 13.15 | 2.87 | 0.37 | −0.77 |
Nonnormal data distribution.
Females accounted for 24% of the intervention cohort, exceeding the current gender census at the U.S. Military Academy.30
CI, confidence interval, SD, standard deviation; SEM, standard error of the mean; yr, years; M, male; F, female
The study sample's mean age was 20.27 (95% confidence interval [CI]: 20.26, 20.28) with males accounting for the majority (71%) of participants. Overall female gender distribution exceeded the current USMA gender census.30 All sample demographic characteristics were normally distributed with homoscedasticity observed (except gender) and were similar between the groups (P > 0.05; Table 5).
Table 5.
Battlefield Acupuncture Between-Groups Opioid Use (t-Test for Equality of Means)
| 95% CI of the difference | |||||||
|---|---|---|---|---|---|---|---|
| Timepoints | t | df | Sig. (2-tailed) | Mean difference | SE difference | Lower | Upper |
| 24 hr | 0.318 | 32 | 0.752 | 0.294 | 0.924 | −1.588 | 2.176 |
| 72 hr | 0.763 | 33 | 0.451 | 1.716 | 2.248 | −2.858 | 6.290 |
| 7 d | 0.883 | 33 | 0.384 | 2.876 | 3.257 | −3.751 | 9.503 |
| 14 d | 1.076 | 33 | 0.290 | 3.745 | 3.480 | −3.335 | 10.825 |
| 42 d | 1.076 | 33 | 0.290 | 3.745 | 3.480 | −3.335 | 10.825 |
Note: There was no significant difference in opioid use between the groups (intervention and control) at all timepoints (P > 0.05).
t, time; df, difference; Sig., significance; SE, standard error; CI, confidence interval, hr, hours, d, days.
Arthroscopic Bankart repair was the most common shoulder surgery performed on the subjects (n = 34, 85%), followed by the Laterjet procedure (n = 2, 5%). Laterality of surgical procedures within the sample was reported as 23 left- (57.5%) and 16 right-shoulder surgeries (40%). Female subjects within the sample predominantly reported right-shoulder surgeries (n = 8 of 9, 88.9%), with 77.8% having arthroscopic Bankart repairs. Male subjects reported surgical laterality as: 22 left- (73.3%) and 9 right-shoulder (30%) surgeries. Repeat ipsilateral shoulder surgery was performed on 4 subjects (10.3%), and prior contralateral shoulder surgery was reported by 3 subjects (7.7%).
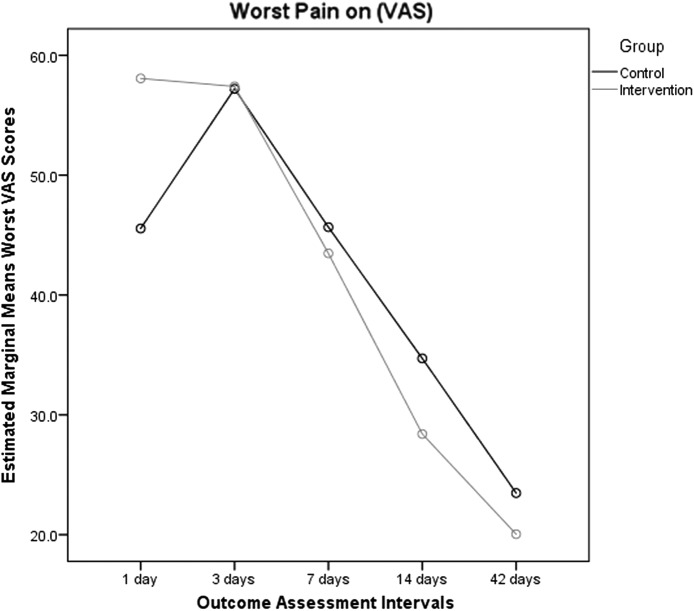
A main effect for time was observed for each subject's average and worst pain (VAS) using the Greenhouse–Geisser correction (both P < 0.001) for the mixed-model ANOVA Significant main effects for time (Table 6), were noted between all timepoints for average and worst VAS pain (P < 0.05). There was no significant time–group interactions (P > 0.05) (Figs. 4 and 5).
Table 6.
Between-Group Demographic Independent Samples t-Test
| Demographics | Levene's test for equality of variances | t-Test for equality of means | |||||||
|---|---|---|---|---|---|---|---|---|---|
| F | Sig. | t | df | Sig. (2-tailed) | Mean difference | SE difference | 95% CI of the difference | ||
| Lower | Upper | ||||||||
| Age | 0.856 | 0.361 | −0.275 | 38 | 0.785 | −0.123 | 0.447 | −1.028 | 0.783 |
| Height (cm) | 0.350 | 0.558 | −1.918 | 37 | 0.063 | −4.89 | 2.55 | −10.06 | 0.27 |
| Mass (kg) | 3.112 | 0.086 | −0.730 | 37 | 0.470 | −2.76 | 3.78 | −10.42 | 4.9 |
| College (yr) | 1.914 | 0.175 | 0.094 | 37 | 0.925 | 0.040 | 0.421 | −0.812 | 0.892 |
Notes: No significant difference was observed between the groups (P > 0.05); equality of variance was observed with Levene's test (P > 0.05).
t, time; Sig., significance; df, degrees of freedom; SE, standard error; CI confidence interval; yr, years.
FIG. 4.
Main effect for time with Greenhouse Geisser correction significant (P < 0.001) for the mixed-model analysis of variance for the average pain score (visual analogue scale [VAS]).
FIG. 5.
Main effect for time observed between all timepoints for worst pain (visual analogue scale; P < 0.001).
Planned post hoc testing revealed a significant difference between the intervention and control group's baseline worst VAS pain scores (Table 7; P = 0.041). Pain-change scores for average and worst VAS pain were significantly different between baseline and 7 days (P = 0.026, 95% CI: −22.25, −1.46; P = 0.041; 95% CI −28.76, −0.65, respectively). The GROC change scores showed no significant difference between the groups.
Table 7.
Changes in Average & Worst Pain Between Groups
| Outcome measures | Control (n = 19; 95% CI)b | Intervention (n = 21; 95%CI)b | Between-group differences (95% CI)c |
|---|---|---|---|
| VAS average (0–100 mm)a | |||
| Baseline to 72 hr | (−3.61) (−2.56, 9.78) | 5.71 (−3.94, 15.36) | |−9.32| (−20.68, 2.04) |
| 72 hr to 7 d | 8.11 (3.01, 13.21) | 10.64 (4.91, 16.37) | |−2.53| (−10.03, 4.95) |
| Baseline to 7 d | 4.5 (−2.05, 11.05) | 16.36 (8.05, 24.67) | |−11.86| (−22.25, −1.46)* |
| 7 d to 14 d | 6.37 (1.68, 11.06) | 6.74 (2.22, 11.25) | |−0.37| (−6.67, 5.93) |
| 14 d to 42 d | 9.76 (3.15, 16.37) | 1.91 (−1.43, 5.25) | 7.85 (0.61, 15.1) |
| VAS worst (0–100 mm)a | |||
| Baseline to 72 hr | (−11.66) (−23.57, 0.25) | 0.67 (−6.58, 7.92) | |−12.33| (−25.51, 0.85) |
| 72 hr to 7 days | 11.55 (4.34, 18.76) | 13.93 (6.47, 21.38) | |−2.37| (−12.46, 7.71) |
| Baseline to 7 d | (−0.11) (−10.92, 10.7) | 14.6 (4.82, 24.38) | |−14.71| (−28.81, −.061)* |
| 7 d to 14 d | 10.95 (2.83, 19.1) | 15.07 (7.91, 22.22) | |−4.12| (−14.59, 6.3) |
| 14 d to 42 d | 11.24 (1.05, 21.43) | 8.36 (2.19, 16.18) | 2.87 (−9.09, 14.85) |
Adapted from Cleland et al.45
Higher scores on VAS indicate greater pain; negative changes in scores indicate increased pain and positive changes in scores indicate decreased pain.
Values are within-group mean (95% confidence interval) differences over time.
Values are mean (95% confidence interval) differences in within-group changes between groups at each outcome measurement.
P < 0.05.
VAS, visual analogue scale; CI, confidence interval; hr, hours, d, days
The GROC is a 15-point (−7 to +7, with −7 = a very great deal worse, 0 = no change or improvement, and +7 = a very great deal better) self-report Likert scale of patient-perceived progress or regression since the onset of medical treatment.20 The minimal clinically important difference (MCID) for the GROC is 2 points and the minimal detectable change (MCD) is 0.45 points on the condensed 11-point scale.20 The GROC scale has high face validity and reliability, with numerous studies defining major improvement as 5 or more (deterioration is −5 or less).20 The intervention group reported greater GROC scores than controls, meeting the MCID in 45% of the cohort and the major improvement (MI) in 40% of the group (GROC scores between 24 hours and 7 days). Nearly 39% of the control group reported meeting the GROC's MCID and MI between 24 hours and 7 days. See Table 8.
Table 8.
VAS for Comparison of Pain Groups
| Group | Average VAS pain | Worst VAS pain | |
|---|---|---|---|
| 24 hr to 7 d | 24 hr to 7 d | ||
| Controla | MCID | 0 | 2 |
| MI | 1 | 1 | |
| Intervention (BFA)b | MCID | 2 | 2 |
| MI | 4 | 6 |
The control group (n = 18) reported 5.6% MI in average and worst VAS pain between baseline and 7 d
The intervention (BFA) group (n = 20) reported 10% MCID in average and worst VAS pain between baseline and 7 d, and 20% and 30% MI in average and worst VAS pain (respectively) at baseline and 7 d.
VAS: visual analogue scale; hr, hours; d, days; BFA, Battlefield Acupuncture; MCID, minimal clinically important difference; MI, major improvement.
There was no difference in opioid use between the groups at any timepoint (P > 0.05, Table 5). Use of NSAIDs (OTC or prescribed ibuprofen or naproxen sodium) and acetaminophen (a total of 85 tablets ingested over the entirety of the study) was not significantly different between the groups (P > 0.05) over the same time periods.
No adverse events related to the BFA or standard postsurgical rehabilitation were reported during this study.
Discussion
The purpose of this randomized clinical trial was to evaluate the effectiveness of BFA in patients after shoulder surgery. While both treatment groups experienced significant reductions in pain over time, the addition of BFA to a standard rehabilitation protocol resulted in a significantly greater reduction in average and worst pain-change scores between baseline and 7 days. Average and worst pain-change scores (VAS) 95% confidence intervals (CI) between groups, from 1 to 7 days, included the MCID for VAS and provided evidence of clinically important differences in favor of BFA.31,32 Prior research investigating BFA's effect on musculoskeletal pain has produced positive results with clinically meaningful pain reduction without statistical significance.11,33,34 The majority of randomized controlled trials (RCTs) performed using BFA and auricular acupuncture have been deemed “less than rigorous” due to small sample sizes, lack of blinding (therapists and subjects), and lack of sham acupuncture.35
Prior research has shown the MCID for the VAS of pain ranging from 13 to 19 mm.23–26,36 The VAS is widely used in clinical research to measure pain, but can have minimal clinical meaning despite statistical significance.24 The VAS MCID correlates to “a little less pain” and has been scientifically questioned with respect to clinical improvement. Lee and colleagues recommended using a greater VAS MCID threshold for “major” clinical improvement (a VAS change >30 mm), indicating adequate pain control.24 In the control group, 5.6% of the patients had major reductions in average and worst pain from baseline to 7 days. In the intervention group, patients reported major reductions in average pain and worst pain of 20% and 30%, respectively, between baseline and 7 days.
As noted in other studies, opioid, NSAID, and acetaminophen use was similar between the groups (P > 0.05).11,13,33 In contrast to Usichenko, et al.'s 2007 research on auricular acupuncture after ambulatory knee surgery11 that showed significant reductions in ibuprofen use at 24 hours (P < 0.05), this study noted similar NSAID (ibuprofen or naproxen sodium) uses between the groups. Larger RCTs to evaluate auricular and BFA's (protocol and modified protocols) effect on musculoskeletal pain did not show significant differences in opioid use.11,13,33
The PSFS has demonstrated high reliability, validity, and responsiveness to change in patients with shoulder pain.29 Koehorst and colleagues reported the MDC and MCID of the PSFS in patients with shoulder pain as 0.97 and 1.29, respectively.29
This study's short time line for outcomes assessment (6 weeks), postoperative protection within an abduction sling and unrealistic functional activity selection by this study's subjects resulted in subject PSFS data that was noncontributive. Generalizability of the PSFS on primary shoulder pain warrants caution due to researchers providing example activities to assist subjects in choosing activities limited by their shoulder pain.29
Postsurgical pain-medication prescription protocols due to surgeon preference and/or formulary restrictions could have influenced this study's outcomes. Within the health system in which this study was accomplished, all orthopedic surgeons solely prescribed Percocet,® Colace,® and antinausea medications postsurgically (1 exception was made for a patient who had an opioid-medication allergy). A 2017 study by Chang et al., investigated extremity pain in an emergency department and refuted the effectiveness of opioids for reducing acute, moderate limb pain.37 Multiple studies have produced similar outcomes comparing the effectiveness of paracetamol (acetaminophen) and opioids for decreasing moderate acute musculoskeletal pain.37–40 McNicol and colleagues investigated single-dose intravenous (IV) paracetamol (acetaminophen) for acute postsurgical pain in a 2018 systematic review and meta-analysis, noting that 1 g of paracetamol reduced pain up to 50% in 1 of 4 patients.40 However, given that oral bioavailability of paracetamol (acetaminophen) postsurgically is slow and that swallowing the tablets might not be feasible immediately after surgery, IV administration is preferred.40 McNicol et al.'s meta-analysis reported no differences among paracetamol (acetaminophen), NSAIDs, and opioids for pain outcomes. Caution is warranted, as multiple researchers cite inconsistent sample sizes in comparator and placebo-control samples, as well as varied drug dosages within prescribed pain medications and outcome assessment intervals.37–40 Furthermore, research has shown that acetaminophen (i.e., paracetamol and its hydrolyzed derivative propacetamol) administered IV has a superior safety profile with significantly fewer adverse events, compared to opioids.37,38,40
Limitations
The results of this study, due to numerous factors, might not be readily applicable to the general population. The mean age of the study sample (N = 40) was ∼20 years, and the subjects were predominantly male (71%). Homogeneity in surgical procedures performed (Bankart repair, n = 34, 85%) limits the prediction of this study's outcomes (time effects and pain-change scores) to other sample populations and procedures typically performed on older populations. The acute mechanism of injury reported in this study sample might not reflect mechanisms of injury reported in older populations. The study sample used opioid pain medication for fewer than 13 days (within-subjects and between-subjects) (Fig. 6), which is fewer than overall opioid use reported by the DoD Veterans Health Administration, but might not reflect the general populations' typical postsurgical opioid use.41,42
FIG. 6.
Subjects' (both groups) average daily opioid intakes, postsurgical days 1–14. No opioid use after day 14 was reported. Mean days of opioid use = 5.82 (± 2.72) postsurgery (error bars = standard deviations).
Access to health care for this study's sample does not reflect usual access to care in the civilian population, which is greatly limited by insurance coverage, work-schedule conflicts, and attendance feasibility. The study sample had daily, open-door access to physical therapy/athletic training (sports medicine) care, 5–6 days per week, without fiscal or work limitations.
A recent study investigating modified BFA, sham BFA, and standard care alone reported no significant differences in opioid use, postsurgical knee pain, and increased quality of life.33 This variance from the original BFA protocol, applying the ASP needles in all 10 BFA points without walking in-between needle placements, compared to sham BFA (ASP needles placed within the homunculus within the ear) has been confounded by recent literature. Dr. Niemtzow's 2009 BFA literature suggested that the five BFA points are “areas” or “fields.7” ASP needle placement will vary by mm, within and between BFA practitioners, for pain attenuation to occur.7 Crawford et al. used electrically inactive auricular acupuncture areas that have been correlated to the upper extremity for the sham treatment (5 ASP needles were placed in the upper extremity region).12 Caution is warranted due to a differing methodology for ASP needle placement by Crawford et al.12 Huang et al.'s, 2016 study investigating expanded auricular homunculus zones in veterans, identified acupuncture points by pressure sensitivity, compared to Crawford's approach.43 In a 2017 systematic review and meta-analysis, sham acupuncture in the ear was deemed “difficult” due to more than 93 auricular acupoints with neighboring zones.14 Therapeutic effects of acupuncture (body or auricular), in well-documented acupoints or pseudo-acupoints, have been noted in multiple sham-controlled studies and correlated with fMRI observations, nullifying the assumptions of true sham acupuncture.14,17,43,44
Future Research
Additional research should investigate patient satisfaction with BFA, compared to controls; and psychometric responses to treatment; as well as incorporating blinding of the assessors. Further investigation into the VAS pain-change score with a more-robust sample size is indicated. Variations within the BFA protocol (i.e., sequencing of the acupoints) is an additional area to be investigated, compared to standardized BFA and controls.
Conclusions
This is the first randomized clinical trial to investigate the effect of BFA on postsurgical shoulder pain and opioid use. BFA positively reduced postsurgical pain, as shown by the significant differences between the BFA group's average and worst pain-change scores, compared to the control group. While pain-medication use was similar between the groups, BFA may be an effective adjunct to Western medicine for pain control and reducing opioid utilization.
Acknowledgments
This study was approved by the Regional Health Command Atlantic Institutional Review Board and is registered at clinicaltrials.gov (Identifier: NCT03525275).
This article was part of the first author's doctoral thesis research and defense. The research defense committee members were: Donald L. Goss, PT, PhD; Matthew Posner, MD; Michael Crowell, PT, DSc; John Mason, PT, DSc; and Denny Kramer PhD.
This research would not have been possible without the support and guidance of numerous individuals. First, Dr. Collinsworth thanks his wife, whose patience, support, and encouragement are without limits. Second, he thanks his family, who have, without hesitation, supported his efforts in completing this educational goal.
Dr. Collinsworth also offers gratitude and thanks to the Baylor—KACH Division 1 Sport Physical Therapy staff members for their advice and mentorship during this extensive process.
Author Disclosure Statement
No financial conflicts exist. Any reference to a specific commercial product, process, or service by trade name, trademark, manufacturer, or otherwise, does not constitute or imply its endorsement, recommendation, or favoring by the United States Government.
Funding Information
No funding was received for this research.
References
- 1. Rudd RA, Seth P, David F, Scholl L. Increases in drug and opioid-involved overdose deaths—United States, 2010–2015. MMWR Morb Mortal Wkly Rep. 2016;65(5051):1445–1452 [DOI] [PubMed] [Google Scholar]
- 2. Volkow ND, McLellan AT. Opioid abuse in chronic pain—misconceptions and mitigation strategies. New Engl J Med. 2016;374(13):1253–1263 [DOI] [PubMed] [Google Scholar]
- 3. Mudumbai SC, Oliva EM, Lewis ET, et al. Time-to-cessation of postoperative opioids: A population-level analysis of the Veterans Affairs health care system. Pain Med. 2016;17(9):1732–1743 [DOI] [PubMed] [Google Scholar]
- 4. Walker PH, Pock A, Ling CG, Kwon KN, Vaughan M. Battlefield Acupuncture: Opening the door for acupuncture in Department of Defense/Veteran's [sic] Administration health care. Nurs Outlook. 2016;64(5):491–498 [DOI] [PubMed] [Google Scholar]
- 5. Niemtzow RC. Battlefield Acupuncture. 2007;19(4):225–228 [Google Scholar]
- 6. Niemtzow RC, Belard JL, Nogier R. Battlefield Acupuncture in the U.S. military: A pain-reduction model for NATO. Med Acupunct. 2015;27(5):344–348 [Google Scholar]
- 7. Niemtzow RC, Litscher G, Burns SM, Helms JM. Battlefield Acupuncture: Update. Med Acupunct. 2009;21(1):43–46 [Google Scholar]
- 8. Clement-Jones V, McLoughlin L, Tomlin S, Besser GM, Rees LH, Wen HL. Increased beta-endorphin but not met-enkephalin levels in human cerebrospinal fluid after acupuncture for recurrent pain. Lancet. 1980;ii(8201):946–949 [DOI] [PubMed] [Google Scholar]
- 9. Soliman N, Frank BL. Auricular acupuncture and auricular medicine. Phys Med Rehabil Clin N Am. 1999;10:547–554,viii [PubMed] [Google Scholar]
- 10. Cho ZH, Oleson TD, Alimi D, Niemtzow RC. Acupuncture: The search for biologic evidence with functional magnetic resonance imaging and positron emission tomography techniques. J Altern Complement Med. 2002;8(4):399–401 [DOI] [PubMed] [Google Scholar]
- 11. Usichenko TI, Kuchling S, Witstruck T, et al. Auricular acupuncture for pain relief after ambulatory knee surgery: A randomized trial. CMAJ. 2007;176(2):179–183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Crawford P, Penzien DB, Coeytaux R. Reduction in pain medication prescriptions and self-reported outcomes associated with acupuncture in a military patient population. Med Acupunct. 2017;29(4):229–231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Usichenko TI, Hermsen M, Witstruck T, Hofer A, Pavlovic D, Lehmann C, Feyerherd F. Auricular acupuncture for pain relief after ambulatory knee arthroscopy—a pilot study. Evid Based Complement Alternat Med. 2005;2(2):185–189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Jan AL, Aldridge ES, Rogers IR, Visser EJ, Bulsara MK, Niemtzow RC. Does ear acupuncture have a role for pain relief in the emergency setting? A systematic review and meta-analysis. Med Acupunct. 2017;29(5):276–289 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Romoli M, Greco F, Giommi A. Auricular acupuncture diagnosis in patients with lumbar hernia. Complement Ther Med. 2016;26:61–65 [DOI] [PubMed] [Google Scholar]
- 16. Goertz CM, Niemtzow R, Burns SM, Fritts MJ, Crawford CC, Jonas WB. Auricular acupuncture in the treatment of acute pain syndromes: A pilot study. Mil Med. 2006;171(10):1010–1014 [DOI] [PubMed] [Google Scholar]
- 17. Zhang CS, Yang AW, Zhang AL, May BH, Xue CC. Sham control methods used in ear-acupuncture/ear-acupressure randomized controlled trials: A systematic review. J Altern Complement Med. 2014;20(3):147–161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Moss DA, Crawford P. Ear acupuncture for acute sore throat: A randomized controlled trial. J Am Board Fam Med. 2015;28(6):697–705 [DOI] [PubMed] [Google Scholar]
- 19. Abbott JH, Schmitt J. Minimum important differences for the patient-specific functional scale, 4 region-specific outcome measures, and the numeric pain rating scale. J Orthop Sports Phys Ther. 2014;44(8):560–564 [DOI] [PubMed] [Google Scholar]
- 20. Kamper SJ, Maher CG, Mackay Global rating of change scales: A review of strengths and weaknesses and considerations for design. J Man Manip Ther. 2009:17(3):163–170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Coe R. Its the effect size, stupid: What effect size is and why it is important [presentation]. Annual Conference of the British Educational Research Association Annual Conference Exeter, England September 12–14, 2002:22 [Google Scholar]
- 22. Sullivan GM, Feinn R. Using effect size-or why the P value is not enough. J Grad Med Educ. 2012;4(3):279–282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Briggs M, Closs JS. A descriptive study of the use of visual analogue scales and verbal rating scales for the assessment of postoperative pain in orthopedic patients. J Pain Symptom Manage. 1999;18(6):438–446 [DOI] [PubMed] [Google Scholar]
- 24. Lee JS, Hobden E, Stiell IG, Wells GA. Clinically important change in the visual analog scale after adequate pain control. Acad Emerg Med. 2003;10(10):1128–1130 [DOI] [PubMed] [Google Scholar]
- 25. Price DD, McGrath PA, Rafii A, Buckingham B. The validation of visual analogue scales as ratio scale measures for chronic and experimental pain. Pain. 1983;17(1):45–56 [DOI] [PubMed] [Google Scholar]
- 26. Wright A, Hannon J, Hegedus EJ, Kavchak AE. Clinimetrics corner: A closer look at the minimal clinically important difference (MCID). J Man Manip Ther. 2012;20(3):160–166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Hefford C, Abbott JH, Arnold R, Baxter GD. The patient-specific functional scale: Validity, reliability, and responsiveness in patients with upper extremity musculoskeletal problems. J Orthop Sports Phys Ther. 2012;42(2):56–65 [DOI] [PubMed] [Google Scholar]
- 28. Horn KK, Jennings S, Richardson G, Vliet DV, Hefford C, Abbott JH. The patient-specific functional scale: Psychometrics, clinimetrics, and application as a clinical outcome measure. J Orthop Sports Phys Ther. 2012;42(1):30–42 [DOI] [PubMed] [Google Scholar]
- 29. Koehorst ML, van Trijffel E, Lindeboom R. Evaluative measurement properties of the patient-specific functional scale for primary shoulder complaints in physical therapy practice. J Orthop Sports Phys Ther. 2014;44(8):595–603 [DOI] [PubMed] [Google Scholar]
- 30. United States Military Academy. [scroll down to Student Life for gender distribution]. U.S. News & World Report Best Colleges. Online document at: www.usnews.com/best-colleges/west-point-2893 Accessed July29, 2019
- 31. Stratford PW. The added value of confidence intervals. Phys Ther. 2010;90(3):333–335 [DOI] [PubMed] [Google Scholar]
- 32. Sim J, Reid N. Statistical inference by confidence intervals: Issues of interpretation and utilization. Phys Ther. 1999;79(2):186–195 [PubMed] [Google Scholar]
- 33. Crawford P, Moss DA, Crawford AJ, Sharon DJ. Modified Battlefield Acupuncture does not reduce pain or improve quality of life in patients with lower extremity surgery. Mil Med. 2019;184(suppl1):545–549 [DOI] [PubMed] [Google Scholar]
- 34. Abdelfatah MM, Beacham MC, Freedman M, Tillmann HL. Can Battlefield Acupuncture improve colonoscopy experience? Med Acupunct. 2018;30(5):279–281 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Usichenko TI, Lehmann C, Ernst E. Auricular acupuncture for postoperative pain control: A systematic review of randomised clinical trials. Anaesthesia. 2008;63(12):1343–1348 [DOI] [PubMed] [Google Scholar]
- 36. Hawker GA, Mian S, Kendzerska T, French M. Measures of adult pain: Visual analog scale for pain (VAS Pain), numeric rating scale for pain (NRS Pain), McGill Pain Questionnaire (MPQ), Short-Form McGill Pain Questionnaire (SF-MPQ), Chronic Pain Grade Scale (CPGS), Short Form-36 Bodily Pain Scale (SF-36 BPS), and measure of Intermittent and Constant Osteoarthritis Pain (ICOAP). Arthritis Care Res (Hoboken). 2011;63(suppl11):S240–S252 [DOI] [PubMed] [Google Scholar]
- 37. Chang AK, Bijur PE, Esses D, Barnaby DP, Baer J. Effect of a single dose of oral opioid and nonopioid analgesics on acute extremity pain in the emergency department: A randomized clinical trial. JAMA. 2017;318(17):1661–1667 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Graudins A, Meek R, Parkinson J, Egerton-Warburton D, Meyer A. A randomised controlled trial of paracetamol and ibuprofen with or without codeine or oxycodone as initial analgesia for adults with moderate pain from limb injury. Emerg Med Australas. 2016;28(6):666–672 [DOI] [PubMed] [Google Scholar]
- 39. Krebs EE, Gravely A, Nugent S, et al. Effect of opioid vs nonopioid medications on pain-related function in patients with chronic back pain or hip or knee osteoarthritis pain: The SPACE randomized clinical trial. JAMA. 2018;319(9):872–882 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. McNicol ED, Tzortzopoulou A, Cepeda MS, Francia MB, Farhat T, Schumann R. Single-dose intravenous paracetamol or propacetamol for prevention or treatment of postoperative pain: A systematic review and meta-analysis. Br J Anaesth. 2011;106(6):764–775 [DOI] [PubMed] [Google Scholar]
- 41. VA/DoD Clinical Practice Guideline for Opioid Therapy for Chronic Pain. Veterans Administration/Department of Defense; 2017. Online document at: www.healthquality.va.gov/guidelines/Pain/cot/VADoDOTCPG022717.pdf Accessed July29, 2019
- 42. VA/DoD Clinical Practice Guideline for the Management of Substance Use Disorders. Veterans Administration/Department of Defense; 2015. Online document at: www.healthquality.va.gov/guidelines/MH/sud/VADoDSUDCPGRevised22216.pdf Accessed July29, 2019
- 43. Huang W, Halpin SN, Perkins MM. A case series of auricular acupuncture in a veteran's population using a revised auricular mapping–diagnostic paradigm (RAMP-uP). Complement Ther Med. 2016;27:130–136 [DOI] [PubMed] [Google Scholar]
- 44. Huang W, Pach D, Napadow V, et al. Characterizing acupuncture stimuli using brain imaging with FMRI—a systematic review and meta-analysis of the literature. PLoS One. 2012;7(4):e32960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Cleland JA, Mintken PE, McDevitt A, Bieniek ML, Carpenter KJ, Kulp K, Whitman JM. Manual physical therapy and exercise versus supervised home exercise in the management of patients with inversion ankle sprain: A multicenter randomized clinical trial. J Orthop Sports Phys Ther 2013;43(7):443–455 [DOI] [PubMed] [Google Scholar]