Abstract
Chronic kidney disease (CKD) has become a major public health problem in the USA and worldwide. A large majority of patients with CKD have mild to moderate disease and microalbuminuria. It has increasingly been noted that patients with CKD have a significantly higher risk of cardiovascular outcomes compared to patients with normal kidney function. Many studies have shown increased risk beginning at stage 3 CKD but risk has been elevated in patients with milder degrees of kidney dysfunction in some studies. This risk may be better predicted by the degree of albuminuria in the earlier stages of CKD. Data addressing interventions to improve outcomes in patients with mild to moderate CKD are scarce. In this paper, we examined data and post hoc analyses from the ORIGIN and ACCORD trials. Data indicate that intensive treatment of diabetes in patients with CKD actually may result in adverse outcomes. The mechanism by which CKD results in increased cardiovascular risk is not clear. Patients with CKD frequently have the traditional risk factors that cause cardiovascular disease and there are mechanisms that are unique to CKD that promote the development of cardiovascular disease. In this article, we describe in some detail traditional, newer and novel risk factors that play a role in the development of CKD and heart disease.
Keywords: CKD, CAD, cardiovascular mortality, diabetes mellitus
Introduction
Over 20 million people in the USA have been diagnosed with diabetes mellitus (DM).1 DM is a recognized risk factor for cardiovascular disease and is the leading cause of chronic kidney disease (CKD) in the USA. United States Renal Data System (USRDS) data have shown an overall prevalence of CKD (Stages 1–5) in the US adult general population of 14.8% over the period 2013–2016 whereas the prevalence of CKD among patients with DM was more than double this figure at 36% in this same time period.2 Patients with DM usually have other risk factors for cardiovascular disease, such as hypertension and hyperlipidemia. However, the higher rates of cardiovascular morbidity and mortality that are seen in patients with diabetic nephropathy cannot be explained by the presence of these traditional risk factors, and CKD has been shown to be an independent risk factor for cardiovascular disease.3 The impact of CKD on increased cardiovascular risk has been demonstrated and it is felt that CKD should be regarded as a coronary disease equivalent.4
United States Renal Data System
The 2018 USRDS data also reported that a prevalence of cardiovascular disease among patients 66 and older with CKD is approximately twice that of patients without CKD (64.5% vs 32.4%).2 In addition, a large burden of mortality in CKD patients is as a result of cardiovascular disease. In fact, patients with CKD die of cardiovascular disease more often than they progress to end-stage renal disease (ESRD).5 Although there are plenty of data documenting increased cardiovascular risk in patients with CKD, data in patients with type 2 diabetes mellitus (T2DM) and CKD are scarce.
Furthermore, the effect of treatment in patients with early diabetes or prediabetes is not known. In this article, therefore, we addressed primarily this patient population, examined data from the ORIGIN study and we reviewed the relevant literature.
The ORIGIN trial was a randomized control trial (RCT) of 12,537 patients with pre-DM or early T2DM which was designed to evaluate the effect of basal insulin on outcomes.6 In a post hoc analysis, cardiovascular outcomes in patients with normal kidney function were compared to patients with stage 1–3 CKD. Persons with mild to moderate CKD were found to have an 87% higher risk of the composite end point of nonfatal myocardial infarction (MI), nonfatal stroke or death from cardiovascular causes.
These patients had significantly higher risks of nonfatal MI and stroke and a greater than twofold higher risk for both cardiovascular and all-cause mortality. Results of this trial showed no difference in cardiovascular outcomes between patients treated with insulin or those in the placebo arm. There was no difference in outcomes after treatment with insulin in either patients with CKD or patients with normal kidney function. In the post hoc analysis, CKD stages 1, 2 and 3 remained an independent predictor when proteinuria was excluded. When proteinuria was included, CKD was not a significant contributor. This suggested that proteinuria is a stronger predictor of risk for these outcomes than the presence of mild to moderate CKD.7
CKD, proteinuria and risk of cardiovascular disease
It has been demonstrated that reduction in estimated glomerular filtration rate (eGFR) is associated with increased risk of cardiovascular events. In a study of over 1 million patients in an integrated health-care system, with a median follow up of 2.84 years, the rate of cardiovascular events, death and hospitalization increased steeply as eGFR declined. The HR of any cardiovascular events doubled when eGFR fell to 30–44 mL/min/1.73 m2 compared with the reference group with eGFR ≥60 mL/min/1.73 m2. The HR further increased to 3.4 when eGFR fell below 15 mL/min/1.73 m2. The risk of death from any cause also increased by almost 600% when eGFR fell below 15 mL/min/1.73 m2.8
The risk of MI due to CKD seems to be even higher than the risk conferred by DM. This was demonstrated in a population-based study of over 1 million patients in Canada. They found that in people without established CAD, the rate of MI was lower in patients with DM without CKD compared to patients with CKD at 5.4 per 1,000 person-years vs 6.9 per 1,000 person-years. This risk also increased with decreasing eGFR and increasing albuminuria. The rate of incident myocardial infarction in people with diabetes was about half that of people with eGFR <45 mL/min per 1.73 m2 and severely increased proteinuria.9
Increased urinary albumin excretion has also been shown to be a strong predictor of cardiovascular disease in patients with DM that is independent of both GFR and the presence of diabetes.10 The progression of microalbuminuria in subjects with T2DM is independently associated with a further increased risk for cardiovascular disease.11,12,13
The increased risk has been shown to be proportional to the level of albuminuria, and in some studies the cardiovascular risk is increased even at levels that are not considered to be abnormal.
A study of over 200,000 patients in Ontario 66 years and older from 2002 to 2015 showed that increased urinary albumin excretion was associated with a higher risk of both non-ST-elevation myocardial infarction (NSTEMI) and ST-elevation myocardial infarction (STEMI) at any level of kidney function. ACR >30 mg/mmol was associated with a twofold higher adjusted risk of both STEMI and NSTEMI among patients with eGFR ≥60 mL/min/1.73 m2 compared to ACR <3 mg/mmol.14
In a post hoc analysis of the Heart Outcomes Prevention Evaluation (HOPE) study in patients with and without diabetes, microalbuminuria increased the risk of major cardiovascular events (RR 1.83), all-cause death (2.09) and hospitalization for congestive heart failure (3.23). The risk of events increased proportionally with increasing ACR, and the risk of cardiovascular events was elevated at levels that are even below the cutoff for microalbuminuria.15
This finding of increased cardiovascular risk at levels of albuminuria <30 mg/g was also noted in a meta-analysis of over 1 million participants across 14 countries in general population cohorts. With respect to eGFR, the increase in mortality risk became statistically significant at eGFR 60 mL/min/1.73 m2 and increased twofold at eGFR 30–45 mL/min/1.73 m2 independently of albuminuria. Across all eGFR categories but <30 mL/min/1.73 m2, higher ACR was associated with greater than twofold higher mortality risk. Compared to the ACR level 5 mg/g, an ACR within the microalbuminuria range increased the risk twofold. The increased risk became statistically significant at an ACR of 10 mg/g compared to 5 mg/g.16 Similar results were noted in a meta-analysis of cardiovascular mortality in patients with high risk for CKD.17
It is also important for treating physicians to be aware of the significant risk conferred by decreased eGFR, and that in the presence of mild CKD, any degree of proteinuria is also associated with adverse outcomes. The Losartan Intervention For Endpoint reduction in hypertension (LIFE) study suggested that during treatment, any reduction in the risk for the primary outcome (myocardial infarction, stroke, and cardiovascular mortality) was linked to a proportional reduction of urinary albumin excretion.18
Pathophysiological mechanisms
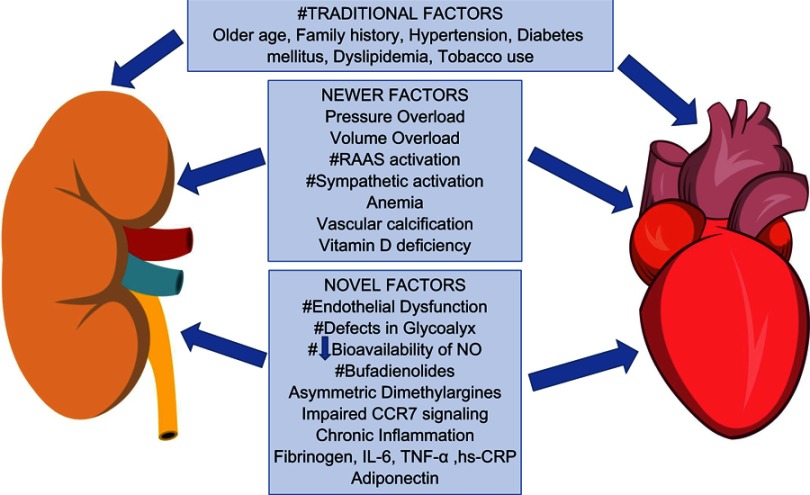
The pathophysiological mechanisms that define the link between renal and cardiovascular disease are not fully understood. Patients with CKD often have traditional risk factors for cardiovascular disease, namely older age, hypertension, DM, dyslipidemia, tobacco use, family history, and male gender. However, the presence of these risk factors cannot account for the increased cardiovascular morbidity and mortality that has been demonstrated in CKD. The discovery of novel risk factors and biomarkers that are unique to CKD help to better understand the complex relationship between the kidney and the heart and how CKD promotes cardiovascular disease.
The bi-directional relationship between the heart and kidney is called the cardiorenal syndrome. Type IV describes CKD that contributes to decreased cardiac function, cardiac hypertrophy and/or increased risk of adverse cardiovascular events and is called chronic renocardiac syndrome.19 CKD causes pressure overload secondary to hypertension and vascular stiffness and volume overload that increases left ventricular wall stress. These factors can result in the development of cardiomyopathy and left ventricular failure.20
Novel risk factors and biomarkers
Bufadienolides are compounds that belong to the cardiac glycoside class (like digoxin) and have been proposed to have a causative role in the development of cardiac disease in CKD. These compounds inhibit the adenosine triphosphatase sodium-potassium pump (Na-K-ATPase), thus inducing natriuresis, vasoconstriction and subsequently increasing blood pressure, as well as cardiac inotropy.21,22 They are synthesized in the adrenal cortex and placenta and levels are elevated as a result in chronic volume overload, as can occur in CKD. Marinobufagenin is the most studied member of this class. It has been implicated in the development of fibrosis in uremic cardiomyopathy by showing that in animal models, immunization against marinobufagenin improved cardiac hypertrophy, fibrosis, and oxidative stress. It has also been shown to play a role in promoting fibrosis of the kidney.23
It has been postulated that common processes may underlie the association between renal and cardiovascular disease.24 Published in 1989, the Steno hypothesis proposed that albuminuria was a result of global dysfunction of the vascular endothelium.25 However, the causal relationship still needs to be clarified, as it remains unclear whether microalbuminuria causes endothelial dysfunction or vice versa. Recent findings suggest that vascular endothelium has a crucial role in determining the permeability of albumin, through a molecule called glycocalix. Glycocalix fills the endothelial fenestrae and plays a role in permeability, specifically glomerular size and charge selectivity.25–27 Defects in endothelial glycocalyx have been implicated not only in microalbuminuria but also to the pathogenesis of atherosclerosis. It is speculated that the penetrance of albumin through the glomerulus reflects a generalized transvascular leakage of albumin and possibly other lipoprotein particles into the arterial wall, thus contributing to atherosclerosis.25,28
More recent studies have demonstrated the role of decreased bioavailability of nitric oxide in the development of endothelial dysfunction.29 Nitric oxide has potent vasodilation, antiplatelet, antiproliferative, anti-adhesive, permeability-decreasing, and anti-inflammatory properties and decreased bioavailability of NO has been implicated in the development both proteinuria and cardiovascular disease.
Other biochemical molecules, known as dimethylarginines, are implicated in the pathogenesis of cardiovascular disease in CKD.30 They are usually excreted into the urine as products of protein degradation, and subsequently their urinary levels are raised in clinical conditions associated with increased protein breakdown such as tumor growth and neurodegenerative diseases.31 Post-translational methylation of arginine residues results in the formation of two isomers; asymmetric and symmetric dimethylarginines.32 Levels of dimethylarginine are substantially increased in subjects with CKD. Asymmetric dimethylarginines act as an endogenous inhibitor of nitric oxide synthesis, and thus counter-regulate their favorable properties33 and may underlie many of the clinical symptoms related to renal diseases and their vascular complications.34 CKD is a chronic inflammatory state. Chronic inflammation has been described in the pathogenesis of atherosclerosis. Markers of inflammation have been studied in patients with CKD and albuminuria. Plasma levels of IL-1b, IL-1RA, IL-6, TNF-a, hs-CRP have been found to be inversely proportional to the level of kidney function and increased with higher levels of albuminuria.35 Plasma levels of fibrinogen, IL-6, and TNF-α have been shown to have positive independent associations with a composite of incident MI, PAD, stroke, and death.36
Moderate kidney disease has also been shown to inhibit the regression of atherosclerosis in a mouse model as a result of impaired chemokine receptor 7 signaling. This resulted in macrophage accumulation in the atherosclerotic lesions that may increase foam cell formation.37 A newly described hormone, called adiponectin, is a biomarker for metabolic syndrome which is closely correlated to kidney disease.38 Adiponectin levels are inversely related to several metabolic parameters, such as body mass index and glucose levels, thus levels are suppressed in obesity and DM. It appears to have a protective role via anti-atherosclerotic, insulin-sensitizing, antioxidant and anti-inflammatory effects on the vascular endothelium. It may reduce albuminuria by stabilizing podocyte function as well.39 In mouse models, low adiponectin levels are associated with renal fibrosis and albuminuria.40 Hashimoto et al demonstrated that adiponectin levels correlated positively with HDL and negatively with triglyceride levels in Japanese men undergoing coronary angiography. Hypoadiponectinemia was also found to be associated with early onset of coronary artery disease and a greater number of atherosclerotic lesions in the coronary vessels.41 In addition to the previously described mechanisms, adiponectin may have direct beneficial effects on cardiomyocytes by inhibiting apoptosis caused by ischemia-reperfusion injury.42 In a cohort study of chronic hemodialysis patients, it has been postulated that decreased plasma levels of adiponectin are associated with increased risk of cardiovascular disease mortality.43 Thus, the role of adiponectin and its association to mild and moderate kidney disease may also be of clinical importance.
Other contributing factors to increased cardiovascular risk in patients with CKD include increased RAAS and sympathetic activity, anemia, hyperphosphatemia, vascular calcification as well as vitamin D deficiency.44
The discovery of novel compounds has helped us to better understand some of the links between kidney disease and cardiovascular disease. However, whether there is a direct causative role of CKD and albuminuria on cardiovascular disease or a common underlying pathogenesis is still unclear.
The risk factors and novel biomarkers that affect cardiac and kidney function are depicted in Figure 1.
Figure 1.
Pathophysiological mechanisms involved in the development of cardiovascular disease in CKD. Factors that have bidirectional action and may affect both kidney and cardiac function are labeled with #.Abbreviations: CCR7, chemokine receptor 7; CKD, Chronic Kidney Disease.
Treatment and cardiovascular outcomes
The effect of intensive treatment of T2DM on cardiovascular and renal outcomes was examined in a few other studies with a similar design to ORIGIN, that are summarized in Table 1.45–49 The most important of those studies was the Action to Control Cardiovascular Risk in Diabetes (ACCORD) trial. ACCORD was a randomized, controlled, but not-blinded trial with a 2×3 factorial design, and it was conducted in 10,251 high-risk patients with T2D and a glycated hemoglobin level ≥7.5%.50 The study examined the effect of intensive glycemic control, intensive BP and lipid control of cardiovascular and renal outcomes. The primary outcome of the main glycemia study suggested that intensive glucose-lowering was associated with increased risk for cardiovascular and all-cause mortality, as compared to standard therapy.45 Our team performed post hoc analyses to assess the impact of intensive therapies on cardiovascular and renal events in patients with and without CKD.51–54
Table 1.
Summary of the most important clinical studies assessing cardiovascular risk and renal outcomes in patients with T2D and CKD other than ORIGIN, ACCORD, and EMPA-REG
| Study | Number of participants | Comparators | Outcome |
|---|---|---|---|
| ABCD [45] | 480 normotensive patients with diabetes mellitus | Intensive decrease in DBP vs target for DBP of 80–89 mmHg | −15 vs 8 patients reverted from microalbuminuria to normoalbuminuria* -lower risk for progressing in macroalbuminuria and overt albuminuria* -1.7% vs 5.4% Cerebrovascular events* |
| IDNT [46] | 590 patients with hypertension, diabetes and microalbuminuria | Irbesartan 150 or 300 mg vs placebo | Time of onset of diabetic nephropathy: HR: 0.3 (95%CI: 0.14–0.61)* |
| RENAAL [47] | 1,513 patients with hypertension, diabetes and nephropathy | Baseline SBP: 140–159 mmHg vs <130 mmHg | Risk for ESRD of death HR: 0.62* |
| UKPDS [48] | 5,097 patients with diabetes | After 10 years of follow-up | -Patients with nephropathy had an annual death rate of 19.2%* -Risk for cardiovascular death increased with increasing nephropathy* |
| VA Nephron [49] | 1,449 with diabetes mellitus, macroalbuminuria and eGFR 30–89 mL/min/1.73 m2 | Losartan with lisinopril vs losartan with placebo | -Mortallity HR: 1.04 (95%CI: 0.73–1.49) -No significant difference in cardiovascular outcomes |
Abbreviations: T2D, type 2 diabetes; CKD, chronic kidney disease; DBP, diastolic blood pressure; SBP, systolic blood pressure; ESRD, end-stage renal disease; eGFR, estimated glomerular filtration rate.
In the first post hoc analysis of ACCORD, Papademetriou et al assessed the influence of CKD IIII on cardiovascular morbidity and mortality, as well as disparities of intensive glucose management between participants with and without CKD.51 Cardiovascular outcomes were available in all ACCORD participants (10,251), whereas renal data were available for 10,142 participants. Among ACCORD participants 36% were diagnosed with CKD stages 1–3. Patients with CKD were older, had higher body mass index, HbA1c and fasting glucose, systolic BP, the prevalence of cardiovascular disease and heart failure, and duration of diabetes. Of note, CKD patients used more insulin and antihypertensive agents, while oral hypoglycemic agents were used less frequently as compared to patients with no CKD. Compared to non-CKD, patients with CKD had a higher rate of cardiovascular events and higher and higher cardiovascular and all-cause mortality (HR of 2.19; 95% CI: 1.76–2.73, and HR: 1.97; 95% CI: 1.70–2.29). The risk of the primary composite outcome of nonfatal myocardial infarction, nonfatal stroke, and cardiovascular death was increased by approximately 87% (HR: 1.87; 95% CI: 1.65–2.11) in CKD compared with non-CKD patients. Similarly, CKD participants experienced a higher risk for nonfatal myocardial infarction, nonfatal and any type of stroke, major coronary artery disease, and congestive heart failure by 62%, 149%, 141%, 56%, and 219%. Compared with standard therapy, intensive glucose control in patients with CKD was associated with a higher risk for cardiovascular (HR: 1.41; 95% CI: 1.05–1.89) and all-cause mortality (HR: 1.30; 95% CI: 1.07–1.60); that remained statistically significant even after multivariate adjustments. Of note, the test for interaction was not significant, suggesting that these observations may need validation. In contrast, no significant differences in cardiovascular and all-cause mortality were observed between intensive and standard therapy in participants free of CKD. Likewise, CKD participants had a significantly higher risk for hypoglycemia compared with non-CKD participants. Of note, insulin was used in approximately 25% of the study participants, with higher doses by individuals randomized to the intensive compared with the standard glucose-lowering group, as the study design recommended a titration in previous insulin dose by 10% when the glycemic-target was not achieved.
The 2018 Consensus Report from the American Diabetes Association and the European Association for the Study of Diabetes now recommends the use of sodium-glucose cotransporter-2 inhibitors (SGLT2i) in patients with DM with established atherosclerotic cardiovascular disease (ASCVD), heart failure and CKD as recent data suggest that they improve both cardiovascular outcomes and slow progression of renal disease.55 The EMPA-REG OUTCOME, CANVAS Program and DECLARE-TIMI 58 were RCTs that evaluated the effect of SGLT2i on cardiovascular and renal outcomes in patients with T2DM.55–57 When stratified by eGFR, a recent meta-analysis of these SGLT2i trials showed a 40% reduction in hospitalization for heart failure and 18% reduction in major cardiovascular events in patients with GFR <60 mL/min per 1.73 m2, and 31% reduction in hospitalization for heart failure and major cardiovascular events in patients with stage 2 CKD.58 Of note, SGLT2i are contraindicated in severe CKD. Dapagliflozin is contraindicated when eGFR <60 mL/min/1.73 m2 and canagliflozin and empagliflozin when eGFR <45 mL/min/1.73 m2. As such, these agents are of particular benefit in early CKD rather than advanced stages to reduce cardiovascular events. Moreover, a post-hoc analysis of pre-specified renal outcomes of the EMPA-REG OUTCOME study showed that empagliflozin was associated with nephroprotection.59 More than one out of four participants had CKD stage 3 and more than one out of 10 had albuminuria ≥300mg/day. Empagliflozin was significantly associated with a lower hazard of incident or worsening nephropathy, progression to macro-albuminuria, doubling serum creatinine, as well as initiating renal replacement therapy compared to placebo (relative risk 0.61; 0.62; 0.56; and 0.45, respectively).
The EMPA-Kidney trial is an ongoing Phase 3 trial to investigate the effect of empagliflozin on kidney disease progression or cardiovascular death vs placebo on top of standard of care in patients with preexisting CKD.60 This study will include patients with advanced kidney disease with eGFR as low as 20 mL/min/1.73 m2 as well as patients with milder degrees of kidney dysfunction with albuminuria. The estimated completion date is in 2022 and, if shown to have benefit, has the potential to impact the management of a large number of at-risk patients.
In the second post hoc ACCORD analysis,47 the impact of intensive BP control was examined in patients with and without CKD. Intensive antihypertensive treatment in participants free of CKD showed a statistically significant reduction in any cerebrovascular event and non-fatal stroke by 55% and 50%, respectively. Similarly, in CKD participants, intensive blood pressure therapy was associated with a significant reduction of any cerebrovascular event and non-fatal stroke by 38% and 65%, respectively. However, changes in other cardiovascular disease outcomes were not significant. The third sub-analysis of the ACCORD trial assessed the impact of fenofibrate on cardiovascular and mortality outcomes according to CKD status.48 It was found that in CKD participants, the addition of fenofibrate had no effect on any of the outcomes. In contrast, in patients without CKD, the addition of fenofibrate resulted in a significant 36% reduction of cardiovascular mortality (95% CI 0.42–0.97), and 44% lower rate of congestive heart failure (95% CI 0.37–0.84).
Recently, Mottl and colleagues conducted a post-hoc analysis of the long-term outcomes of the ACCORD study (ACCORDION) to investigate the impact of intensive BP control, antidiabetic therapy, and fenofibrate on renal and mortality outcomes.49 In 10 years of follow-up, incidence of macro-albuminuria, doubling of serum creatinine, need for dialysis, and death were observed in 988, 954, 351, and 1,905 participants, respectively. From the therapeutic trinity, only intensive glucose-lowering therapy was associated with a significant reduction in the composite outcome by 8% (HR: 0.92; 95% CI: 0.86–0.98). Nevertheless, multivariable analysis of secondary outcomes unveiled that benefit was driven by a reduction in macro-albuminuria (HR: 0.68; 95% CI: 0.59–0.77), which was the only outcome that was reduced with intensive treatment. In contrast, both intensive BP therapy and fenofibrate were associated with a significantly higher incidence of serum creatinine doubling (HR: 1.64; 95% CI: 1.30–2.06, and HR: 2.00; 95% CI: 1.61–2.49, respectively).
Conclusion
All in all, data show that intensive treatment of diabetes in patients with mild to moderate CKD may lead to an improvement in proteinuria, but may worsen cardiovascular outcomes and even increase cardiovascular and all-cause mortality. Newer agents, like SGLT2 inhibitors, have been shown to improve cardiovascular and renal outcomes. In recent years, a number of novel factors have been identified in patients with CKD that may independently contribute to the development of cardiovascular disease. These novel factors can be potential therapeutic targets in the future, but there is a need for ongoing research in this arena.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Schmit AM; Highlighting diabetes mellitus: The epidemic continues. Atheroscler Thromb Vasc Biol; 2018;38:e1–e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.United States Renal Data System. 2018 USRDS Annual Data Report: Epidemiology of Kidney Disease in the United States. Bethesda (MD): National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; 2018. [Google Scholar]
- 3.Pálsson R, Patel UD. Cardiovascular complications of diabetic kidney disease. Adv Chronic Kidney Dis. 2014;21(3):273–280. doi: 10.1053/j.ackd.2014.03.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Debella YT, Giduma HD, Light RP, Agarwal R. Chronic kidney disease as a coronary disease equivalent-a comparison with diabetes over a decade. Clin J Am Soc Nephrol. 2011;6(6):1385–1392. doi: 10.2215/CJN.10271110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gargiulo R, Suhail F, Lerma EV. Cardiovascular disease and chronic kidney disease. Dis Mon Sep. 2015;61(9):403–413. doi: 10.1016/j.disamonth.2015.07.005 [DOI] [PubMed] [Google Scholar]
- 6.ORIGIN Trial Investigators, Gerstein HC, Bosch J, Dagenais GR, et al. Basal insulin and cardiovascular and other outcomes in dysglycemia. N Engl J Med. 2012;367(4):319–328. [DOI] [PubMed] [Google Scholar]
- 7.Papademetriou V, Nylen ES, Doumas M, et al. Chronic kidney disease, basal insulin glargine, and health outcomes in people with dysglycemia: the ORIGIN Study. Am J Med. 2017;130(12):e27–e39. [DOI] [PubMed] [Google Scholar]
- 8.Go AS, Chertow GM, Fan D, McCulloch CE, Hsu CY. Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med. 2004;351(13):1296–1305. [DOI] [PubMed] [Google Scholar]
- 9.Tonelli M, Muntner P, Lloyd A, et al. Risk of coronary events in people with chronic kidney disease compared with those with diabetes: a population level cohort study. Lancet. 2012;380(9844):807–814. [DOI] [PubMed] [Google Scholar]
- 10.Ninomiya T, Perkovic V, de Galan BE, et al. Albuminuria and kidney function independently predict cardiovascular and renal outcomes in diabetes. J Am Soc Nephrol. 2009;20(8):1813–1821. doi: 10.1681/ASN.2008121270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Svensson MK, Cederholm J, Eliasson B, Zethelius B, Gudbjörnsdottir S, Register SND. Albuminuria and renal function as predictors of cardiovascular events and mortality in a general population of patients with type 2 diabetes: a nationwide observational study from the Swedish National Diabetes Register. Diab Vasc Dis Res. 2013;10(6):520–529. doi: 10.1177/1479164113500798 [DOI] [PubMed] [Google Scholar]
- 12.Spoelstra-de Man AME, Brouwer TB, Stehouwer CDA, Smulders YM. Rapid progression of albumin excretion is an independent predictor of cardiovascular mortality in patients with type 2 diabetes and microalbuminuria. Diabetes Care. 2001;24(12):2097–2101. [DOI] [PubMed] [Google Scholar]
- 13.Yuyun MF, Dinneen SF, Edwards OM, Wood E, Wareham NJ. Absolute level and rate of change of albuminuria over 1 year independently predict mortality and cardiovascular events in patients with diabetic nephropathy. Diabet Med. 2003;20(4):277–282. doi: 10.1046/j.1464-5491.2003.00940.x [DOI] [PubMed] [Google Scholar]
- 14.de Chickera SN, Bota SE, Kuwornu JP, et al. Albuminuria, Reduced Kidney Function, and the Risk of ST - and non-ST-segment-elevation myocardial infarction. J Am Heart Assoc. 2018;7(20):1–10. doi: 10.1161/JAHA.118.009995 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gerstein HC, Mann JF, Yi Q, et al. Albuminuria and risk of cardiovascular events, death, and heart failure in diabetic and nondiabetic individuals. JAMA. 2001;286(4):421–426. [DOI] [PubMed] [Google Scholar]
- 16.Matsushita K, van der Velde M, Astor BC, et al. Association of estimated glomerular filtration rate and albuminuria with all-cause and cardiovascular mortality in general population cohorts: a collaborative meta-analysis. Lancet. 2010;375(9731):2073–2081. doi: 10.1016/S0140-6736(10)60674-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Van der Velde M, Matsushita K, Coresh J, et al. Lower estimated glomerular filtration rate and higher albuminuria are associated with all-cause and cardiovascular mortality. A collaborative meta-analysis of high-risk population cohorts. Kidney Int. 2011;79(12):1341–1352. doi: 10.1038/ki.2010.536 [DOI] [PubMed] [Google Scholar]
- 18.Dahlöf B, Devereux R, de Faire U, et al. The Losartan Intervention For Endpoint reduction (LIFE) in Hypertension study: rationale, design, and methods. The LIFE Study Group. Am J Hypertens. 1997;10(7 Pt 1):705–713. [PubMed] [Google Scholar]
- 19.Ronco C, House AA, Haapio M. Cardiorenal syndrome: refining the definition of a complex symbiosis gone wrong. Intensive Care Med. 2008;34(5):957–962. doi: 10.1007/s00134-008-1017-8 [DOI] [PubMed] [Google Scholar]
- 20.Herzog CA, Asinger RW, Berger AK, et al. Cardiovascular disease in chronic kidney disease. A clinical update from Kidney Disease: improving Global Outcomes (KDIGO). Kidney Int. 2011;80(6):572–586. doi: 10.1038/ki.2011.223 [DOI] [PubMed] [Google Scholar]
- 21.Bova S, Blaustein MP, Ludens J, Harris D, DuCharme D, Hamlyn JM. Effect of an endogenous ouabainlike compound on heart and aorta. Hypertension. 1991;17(6):944–950. [DOI] [PubMed] [Google Scholar]
- 22.Ooi H, Colucci W. Pharmacological treatment of heart failure In: Hardman JE, Limbird LE, Gilman AG, editors. Goodman and Gilman’s Pharmacological Basis of Therapeutics. 10th ed. New York (NY): McGraw-Hill; 2001.901–932. [Google Scholar]
- 23.Puschett JB, Agunanne E, Uddin MN. Emerging role of the bufadienolides in cardiovascular and kidney diseases. Am J Kidney Dis. 2010;56(2):359–370. doi: 10.1053/j.ajkd.2010.01.023 [DOI] [PubMed] [Google Scholar]
- 24.Stehouwer CD, Smulders YM. Microalbuminuria and risk for cardiovascular disease: analysis of potential mechanisms. J Am Soc Nephrol. 2006;17(8):2106–2111. doi: 10.1681/ASN.2005121288 [DOI] [PubMed] [Google Scholar]
- 25.Deckert T, Feldt-Rasmussen B, Borch-Johnsen K, Jensen T, Kofoed-Enevoldsen A. Albuminuria reflects widespread vascular damage. The Steno hypothesis. Diabetologia. 1989;32(4):219–226. [DOI] [PubMed] [Google Scholar]
- 26.Haraldsson B, Sorensson J. Why do we not all have proteinuria? An update of our current understanding of the glomerular barrier. News Physiol Sci. 2004;19:7–10. [DOI] [PubMed] [Google Scholar]
- 27.Deen WM. What determines glomerular permeability? J Clin Invest. 2004;114(10):1412–1414. doi: 10.1172/JCI23577 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nieuwdorp M, Meuwese MC, Vink H, Hoekstra JB, Kastelein JJP, Stroes ES. The endothelial glycocalix: a potential barrier between health and vascular disease. Curr Opin Lipidol. 2005;16(5):507–511. doi: 10.1097/01.mol.0000181325.08926.9c [DOI] [PubMed] [Google Scholar]
- 29.Goligorsky MS. Vascular endothelium in diabetes. Am J Physiol Renal Physiol. 2017;312(2):F266–F275. doi: 10.1152/ajprenal.00473.2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Schwedhelm E, Böger RH. The role of asymmetric and symmetric dimethylarginines in renal disease. Nat Rev Nephrol. 2011;7(5):275–285. doi: 10.1038/nrneph.2011.31 [DOI] [PubMed] [Google Scholar]
- 31.W K P, Kim S. Protein methylation: chemical, enzymological, and biological significance. Adv Enzymol Relat Areas Mol Biol. 1975;42:227–286. [DOI] [PubMed] [Google Scholar]
- 32.Leiper JM, Santa Maria J, Chubb A, et al. Identification of two human dimethylarginine dimethylaminohydrolases with distinct tissue distributions and homology with microbial arginine deiminases. Biochem J. 1999;343:209–214. doi: 10.1042/bj3430209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Vallance P, Leone A, Calver A, Collier J, Moncada S. Accumulation of an endogenous inhibitor of NO synthesis in chronic renal failure. Lancet. 1992;339(8793):572–575. [DOI] [PubMed] [Google Scholar]
- 34.Kielstein JT, Boger RH, Bode-Boger SM, et al. Marked increase of asymmetric dimethylarginine in patients with incipient primary chronic renal disease. J Am Soc Nephrol. 2002;13(1):170–176. [DOI] [PubMed] [Google Scholar]
- 35.Gupta J, Mitra N, Kanetsky PA, et al. Association between albuminuria, kidney function, and inflammatory biomarker profile in CKD in CRIC. Clin J Am Soc Nephrol. 2012;7(12):1938–1946. doi: 10.2215/CJN.03500412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Amdur RL, Feldman HI, Dominic EA, et al. Use of measures of inflammation and kidney function for prediction of atherosclerotic vascular disease events and death in patients with CKD: findings from the CRIC Study. Am J Kidney Dis. 2019;73(3):344–353. doi: 10.1053/j.ajkd.2018.09.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ponda MP, Barash I, Feig JE, Fisher EA, Skolnik EY. Moderate kidney disease inhibits atherosclerosis regression. Atherosclerosis. 2010;210(1):57–62. doi: 10.1016/j.atherosclerosis.2009.10.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ryo M, Nakamura T, Kihara S, et al. Adiponectin as a biomarker of the metabolic syndrome. Circ J. 2004;68(11):975–981. [DOI] [PubMed] [Google Scholar]
- 39.Ruster C, Wolf G. Adipokines promote chronic kidney disease. Nephrol Dial Transplant. 2013;28(Suppl. 4):iv8–iv14. doi: 10.1093/ndt/gft191 [DOI] [PubMed] [Google Scholar]
- 40.Sharma K. The link between obesity and albuminuria: adiponectinand podocyte dysfunction. Kidney Int. 2009;76(2):145–148. doi: 10.1038/ki.2009.137 [DOI] [PubMed] [Google Scholar]
- 41.Hashimoto N, Kanda J, Nakamura T, et al. Association of hypoadiponectinemia in men with early onset of coronary heart disease and multiple coronary artery stenoses. Metabolism. 2006;55(12):1653–1657. doi: 10.1016/j.metabol.2006.08.005 [DOI] [PubMed] [Google Scholar]
- 42.Tao L, Gao E, Jiao X, et al. Adiponectin cardioprotection after myocardial ischemia/reperfusion involves the reduction of oxidative/nitrative stress. Circulation. 2007;115(11):1408–1416. doi: 10.1161/CIRCULATIONAHA.106.666941 [DOI] [PubMed] [Google Scholar]
- 43.Zoccali C, Mallamaci F, Tripepi G, et al. Adiponectin, metabolic risk factors, and cardiovascular events among patients with end-stage renal disease. J Am Soc Nephrol. 2002;13(1):134–141. [DOI] [PubMed] [Google Scholar]
- 44.Gansevoort RT, Correa-Rotter R, Hemmelgarn BR, et al. Chronic kidney disease and cardiovascular risk: epidemiology, mechanisms, and prevention. Lancet. 2013;382(9889):339–352. doi: 10.1016/S0140-6736(13)60595-4 [DOI] [PubMed] [Google Scholar]
- 45.Schrier RW, Estacio RO, Esler A, Mehler P. Effects of aggressive blood pressure control in normotensivetype 2 diabetic patients on albuminuria, retinopathy and strokes. Kidney Int. 2002;61(3):1086–1097. doi: 10.1046/j.1523-1755.2002.00213.x [DOI] [PubMed] [Google Scholar]
- 46.Parving HH, Lehnert H, Bröchner-Mortensen J, Gomis R, Andersen S, Arner P. Irbesartan in patients with type 2 diabetes and microalbuminuria study group. N Engl J Med. 2001;345(12):870–878. doi: 10.1056/NEJMoa011489 [DOI] [PubMed] [Google Scholar]
- 47.Keane WF, Brenner BM, de Zeeuw D, et al. The risk of developing end-stage renal disease in patients with type 2 diabetes and nephropathy: the RENAAL Study. Kidney Int. 2003;63(4):1499–1507. doi: 10.1046/j.1523-1755.2003.00885.x [DOI] [PubMed] [Google Scholar]
- 48.Adler AI, Stevens RJ, Manley SE, et al. Development and progression of nephropathy in type 2 diabetes: the United Kingdom Prospective Diabetes Study (UKPDS 64). Kidney Int. 2003;63(1):225–232. doi: 10.1046/j.1523-1755.2003.00712.x [DOI] [PubMed] [Google Scholar]
- 49.Fried LF, Emanuele N, Zhang JH, et al. Combined angiotensin inhibition for the treatment of diabetic nephropathy. N Engl J Med. 2013;369(20):1892–1903. doi: 10.1056/NEJMoa1303154 [DOI] [PubMed] [Google Scholar]
- 50.The Action to Control Cardiovascular Risk in Diabetes Study Group. Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med. 2008;358(24):2545–2559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Papademetriou V, Lovato L, Doumas M, et al. Chronic kidney disease and intensive glycemic control increase cardiovascular risk in patients with type 2 diabetes. Kidney Int. 2015;87(3):649–659. [DOI] [PubMed] [Google Scholar]
- 52.Papademetriou V, Zaheer M, Doumas M, et al. Cardiovascular outcomes in action to control cardiovascular risk in diabetes: impact of blood pressure level and presence of kidney disease. Am J Nephrol. 2016;43(4):271–280. [DOI] [PubMed] [Google Scholar]
- 53.Papademetriou V, Lovato L, Tsioufis K, et al. Effects of high density lipoprotein raising therapies on cardiovascular outcomes in patients with type 2 diabetes mellitus, with or ithout renal impairment: the action to control cardiovascular risk in diabetes study. Am J Nephrol. 2017;45(2):136–145. [DOI] [PubMed] [Google Scholar]
- 54.Mottl AK, Buse JB, Ismail-Beigi F, et al. Long-term effects of intensive glycemic and blood pressure control and fenofibrate use on kidney outcomes. Clin J Am Soc Nephrol. 2018;13(11):1693–1702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Zinman B, Wanner C, Lachin JM, et al. Empagliflozin, cardiovascular outcomes and mortality in type 2 diabetes. N Engl J Med. 2015;373(22):2177–2128. [DOI] [PubMed] [Google Scholar]
- 56.Neal B, Perkovic V, Mahaffey KW, et al. Canagliflozin and cardiovascular and renal events in type 2 diabetes. N Engl J Med. 2017;377:644–657. [DOI] [PubMed] [Google Scholar]
- 57.Wiviott SD, Raz I, Bonaca MP, et al. Dapagliflozin and cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2019;380(4):347–357. [DOI] [PubMed] [Google Scholar]
- 58.Zelniker TA, Wiviott S, Raz I, et al. SGLT2 inhibitors for primary and secondary prevention of cardiovascular and renal outcomes in type 2 diabetes: a systematic review and meta-analysis of cardiovascular outcome trials. Lancet. 2019;393(10166):31–39. [DOI] [PubMed] [Google Scholar]
- 59.Wanner C, Inzucchi SE, Lachin JM, et al. Empagliflozin and progression of kidney disease in type 2 diabetes. N Engl J Med. 2016;375(4):323–334. [DOI] [PubMed] [Google Scholar]
- 60.The Study of Heart and Kidney Protection With Empagliflozin (EMPA-KIDNEY). ClinicalTrials.govidentifier:NCT03594110 [Updated April 11, 2019]. Available from: https://clinicaltrials.gov/ct2/show/NCT03594110. Accessed April 12, 2019.