Abstract
Objective:
Different domains of internalizing symptoms (somatic, anxiety, depressive) often occur concurrently, suggesting that they may share common etiology. In longitudinal analyses of internalizing among youth, anxiety is often found to precede depression. However, relatively few studies have also assessed how somatic problems, the third symptom domain, are involved in longitudinal patterns of internalizing. In addition, temporal relations among internalizing symptom domains may vary by cultural group as somatic symptoms are posited to be a more culturally-normative way of communicating or experiencing distress in non-Western, interdependent cultures. Thus, the present study examined longitudinal relations among these three internalizing symptom domains in three ethnocultural adolescent samples.
Methods:
304 European American, 420 Vietnamese American, and 717 Vietnamese adolescents’ self-reported internalizing symptoms (somatic, anxiety, depressive) were assessed at three time points, spaced three months apart, using multigroup cross-lagged path analysis.
Results:
Anxiety symptoms consistently predicted increases in depressive symptoms in European American adolescents. In contrast, for Vietnamese and Vietnamese American adolescents, the most consistent relation was with somatic complaints predicting increases in anxiety. Anxiety and depressive symptoms bidirectionally predicted each other among the Vietnamese and Vietnamese American adolescents.
Conclusions:
Cultural group differences were evident in the temporal course of internalizing symptoms. The pattern of results have implications for culturally relevant intervention targets, during a developmental period of risk for internalizing disorders.
Keywords: Asian, Somatic, Internalizing, Adolescents, Depressive, Culture
1. Introduction
Internalizing psychopathology, comprising somatic complaints, anxiety symptoms, and depressive symptoms [1], are prevalent, frequently co-occurring [2], and are associated with significant functional impairment [3,4]. The tripartite model suggests these symptoms overlap in non-specific negative affect, with anxiety distinguished by autonomic hyperactivity and depression distinguished by reduced positive affect [5]. Several decades of research in adults and youth, across a number of different cultures [6–9], indicate that these three internalizing domains have unique but also substantial shared variance. This suggests that development of somatic complaints, or anxiety, or depression may increase vulnerability for the other internalizing symptom types over time. The most commonly investigated prospective internalizing symptoms relation has been between anxiety and depression, and meta-analyses suggest that anxiety symptoms more strongly predict depressive symptoms across the lifespan than vice-versa [10]. Prospective studies including all three internalizing domains have been infrequent, however, despite physiological hyperarousal—a key feature of somatic complaints—being a core component of the tripartite model [11] and an abundance of research linking somatic symptoms to anxiety or depression [12–17].
Another important but relatively less known aspect of internalizing symptoms is whether culture influences the relationship among the internalizing domains. Culture defines how different ways of being and feeling are socially appropriate, as well as the preferred enactment of affect expression, all of which influence well-being [18,19]. Therefore, differing cultural contexts may relate to distinct temporal sequencing of internalizing symptoms over time.
Somatic symptoms, in particular, may have implications for the other internalizing symptoms in Asian versus Western cultural contexts given that many Asian cultures favor somatic expressions of distress [20], and have been characterized as shaping a somatic-emphasis variant of internalizing (e.g., [21]). Somatic symptoms may play a less significant role in Western cultural contexts (e.g., Canada or the U.S.) with a history of dualism in medicine (i.e., separating issues of the mind and the body) [22]. In line with dualistic philosophical origins, Western cultural groups have been found to “psychologize” distress by emphasizing cognitive-affective depressive or anxiety symptoms despite the presence of somatic symptoms [20,23].
Two main hypotheses are typical for the somatic emphasis in Asian heritage interdependent cultures, in which the self is interconnected with others and a priority is placed on serving group goals [24]: Somatic complaints may represent differences in the communication of internalizing distress, or in the actual experience of internalizing distress. Somatic symptoms, as opposed to affective symptoms, may be used to communicate distress given the value placed on: emotional restraint for preserving social harmony [25,26], suppression of negative affect as a prosocial coping strategy [26,27], and avoidance of emotional support to prevent increased burden on social relationships [28,29]. Thus, somatic symptoms may serve to effectively garner support [30]. On the other hand, the same cultural influences may shape the actual experience of internalizing distress. Daily living and enacting of cultural scripts may influence cognitive perceptions as well as biology, so that somatic symptoms are generated and amplified to be prominently experienced when distressed [31]. To the extent that somatic symptoms limit daily functioning [32–34], individuals with interdependent values may become distressed if they feel they are burdening others or failing in their social roles. Thus, the actual experience of somatic symptoms may also predict later increases in other internalizing (cognitive-affective) symptoms in interdependent Asian-heritage groups.
Cross-cultural variations in the temporal sequencing of symptoms may be particularly evident in adolescence, a developmental period where notable increases in internalizing symptoms occur [35]. Cultural norms may render somatic symptoms to be predominant in the temporal course of internalizing symptoms among Asian-heritage adolescents, but earlier anxiety may also precede depression as commonly found in youth [36–40]. Conceptually, anxiety may lead to increases in future depression through a threat avoidance [41] involving forgoing enjoyment-producing behaviors and resulting in anhedonia [42], a central component of depression reflecting anticipatory impairments [43]. This temporal relationship between anxiety and depression may be consistent across cultures, given that adolescence is a universal period of biopsychosocial change [44], with major development in neural systems. However, the premise that anxiety precedes depression is largely based on majority European-heritage samples, and it is unknown whether this association is robust across cultures when including somatic complaints in statistical models. Few have examined longitudinal relations among adolescents’ somatic complaints, anxiety, and depression more generally [45,46] or cross-culturally [16].
1.1. Current study
The present study assessed variation in the prospective associations among internalizing symptoms over six months, across three cultural adolescent groups: Vietnamese, Vietnamese American, and European American. Vietnamese culture is primarily interdependent, emphasizing group harmony and familistic values [47,48]. Therefore, we hypothesized that somatic symptoms would predict increases in other internalizing symptoms for Vietnamese adolescents, to a greater extent than observed among European American adolescents, for whom the expression of emotions is viewed as adaptive functioning [49]. We expected Vietnamese American youth (exposed to both sets of cultural distress manifestation norms, from their heritage culture and mainstream American culture) to occupy an intermediate position, with somatic symptoms relating to other internalizing symptoms to a lesser degree (i.e., in magnitude or number of significant paths). We also hypothesized that anxiety symptoms would predict subsequent depressive symptoms across all groups.
2. Methods
2.1. Participants and procedure
The current study was part of a larger study examining cultural variation in adolescents’ stress experiences, coping, and mental health among Vietnamese, Vietnamese American, and European American 10th and 11th grade students. The Vietnamese American and European American adolescents were recruited from 10 ethnically diverse public high schools in Los Angeles and San Jose, California, of which five were lower-income and Title 1 eligible. The Vietnamese adolescents were recruited from 12 Vietnamese public high schools near Ho Chi Minh City and Danang City. Like Los Angeles, Ho Chi Minh City is a geographically-extended major industrial area and a cultural center of the country. Like San Jose, Danang is a progressive secondary city located near the coast. Students were introduced to the study in brief classroom presentations. Consent packets with a parental consent form were distributed to interested students. Participants who provided assent and had parental consent completed a self-report questionnaire battery at baseline (T1), 3-months (T2), and 6-months (T3) within the same school year. All procedures in this study were approved by the Institutional Review Boards at the University of California–Los Angeles, Vanderbilt University, and the U.S. FWA IRB at the Danang Psychiatric Hospital.
2.2. Internalizing symptom measurement
The Youth Self Report (YSR) [50,51] was administered at each timepoint to assess internalizing symptoms. The Vietnamese language version, validated in Vietnam [52,53], was used for the Vietnamese sample. The YSR consists of 112 items assessing internalizing and externalizing symptoms in youth, with response options of 0 (not true), 1 (somewhat/sometimes true), and 2 (very true/often true). The three YSR narrowband scales were used in the current study: Somatic Complaints, Anxious/Depressed Symptoms, and Withdrawn/Depressed Symptoms. The Somatic Complaints scale includes 10 items (e.g., “I have headaches (with no known medical cause)”), the Anxious/Depressed scale includes 12 items (e.g., “I am too fearful or anxious”), and the Withdrawn/Depressed scale includes eight items (e.g., “There is very little that I enjoy”). These internalizing narrowband scales are well-established in the adolescent development literature and have shown good reliability and validity cross-culturally, including in a Vietnamese sample [7–9,52]. For the sake of brevity, in this paper we refer to the narrowband scales as somatic, anxiety, and depressive symptoms, reflecting the predominant symptom types in each of the scales.
2.3. Analysis
Multigroup cross-lagged panel analysis was conducted in Mplus 8.0, to examine relations between the three internalizing symptom domains across the three assessments (baseline, 3-months, and 6-months). The models controlled for the effects of sex and age at baseline assessment. Full information maximum likelihood was applied to use all available data and robust maximum likelihood estimation was used to provide model fit and statistical inference robust to non-normality.
3. Results
3.1. Descriptive statistics
Participant demographics, including self-construal scores indicating cultural orientation [54], are shown in Table 1. Means and standard deviations for the primary study variables are presented in Table 2. Bivariate correlations are reported in Appendix A.
Table 1.
Participant demographics at baseline
| European | Vietnamese | ||
|---|---|---|---|
| American | American | Vietnamese | |
| (n = 304) | (n = 420) | (n = 717) | |
| M (SD) or % | M (SD) or % | M (SD) or % | |
| Males | 47.4% | 45.7% | 51.2% |
| Age | 15.6 (0.7) | 15.6 (0.6) | 15.8 (0.7) |
| Born in the U.S. | 96.4% | 79.0% | - |
| Immigrant generation | 2.83 (0.44) | 1.81 (0.41) | - |
| Self-construal score† | 0.07 (1.06) | −0.02 (0.90) | −0.14 (0.66) |
| Education | |||
| Father graduated high school | 94.8% | 86.9% | 85.6% |
| Mother graduated high school | 97.1% | 79.4% | 49.0% |
| Father graduated college or vocational school | 50.6% | 45.9% | 7.4% |
| Mother graduated college or vocational school | 57.4% | 36.0% | 21.6% |
Note.
The interdependent self-construal items mean was subtracted from the independent self-construal items mean. Positive scores indicate a higher mean of independent vs. interdependent self-construal. Negative scores indicate a higher mean of interdependent vs. independent self-construal.
Table 2.
Means and standard deviations of Youth Self Report internalizing symptom T-scores among cultural groups.
| European American (n = 304) |
Vietnamese American (n = 420) |
Vietnamese (n = 717) |
|||||
|---|---|---|---|---|---|---|---|
| M | SD | M | SD | M | SD | p-value | |
| Baseline (T1) | |||||||
| YSR Anxiety | 60.43a | 9.36 | 62.44ab | 9.52 | 60.23b | 8.27 | <.001 |
| YSR Depressive | 60.31a | 9.91 | 63.08a | 9.19 | 58.72a | 8.46 | <.001 |
| YSR Somatic | 58.64 | 8.16 | 58.88 | 8.66 | 59.84 | 9.27 | .069 |
| 3 months (T2) | |||||||
| YSR Anxiety | 58.21ab | 8.49 | 60.67a | 9.55 | 59.63b | 8.16 | .003 |
| YSR Depressive | 59.11a | 9.39 | 61.54ab | 8.89 | 58.84b | 8.54 | <.001 |
| YSR Somatic | 56.70a | 7.59 | 57.60b | 8.06 | 59.19ab | 9.17 | <.001 |
| 6 months (T3) | |||||||
| YSR Anxiety | 57.30ab | 8.18 | 59.95a | 9.33 | 59.41b | 8.73 | .001 |
| YSR Depressive | 58.13a | 8.69 | 61.45ab | 9.97 | 58.64b | 8.84 | <.001 |
| YSR Somatic | 56.29a | 7.38 | 57.10b | 8.13 | 58.58ab | 9.71 | .002 |
Note. p-Values are from ANOVA with Bonferroni-corrected comparisons or Welch test with Games-Howell correction; groups differing significantly are denoted by the same alphabetic letter.
3.2. Multiple-group cross-lagged panel model
The multiple-group (three cultural groups), three time point, cross lagged model examining relations among the internalizing symptoms showed excellent fit with RMSEA = 0.04, CFI = 0.99, TLI = 0.98, and SRMR = 0.03. The model with all parameter estimates free to vary across groups was a better fit than a structurally constrained model holding the regression paths constant (χ2diff(48) = 104.53; p < .001), or a fully constrained model additionally holding the covariances constant (χ2diff(66) = 169.97; p < .001). Table 3 shows the parameters of the models. As expected, all internalizing symptoms were moderately stable across time for all three cultural groups. The magnitude of the stability paths were not significantly different overall, with the exception of European Americans’ T1 to T2 somatic symptom relationship being significantly smaller than for the Vietnamese (χ2 (1) = 11.04, p = .0009).
Table 3.
Main multigroup cross-lagged path analysis parameters.
| European American (n = 304) |
Vietnamese American (n = 420) |
Vietnamese (n = 717) |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| β | B | SE | β | B | SE | β | B | SE | |
| Stability paths | |||||||||
| T1 to T2 | |||||||||
| YSR Anxiety | 0.69 | 0.63 | 0.05 | 0.59 | 0.59 | 0.05 | 0.54 | 0.53 | 0.05 |
| YSR Depressive | 0.61 | 0.58 | 0.06 | 0.62 | 0.60 | 0.05 | 0.59 | 0.59 | 0.05 |
| YSR Somatic | 0.45 | 0.42 | 0.06 | 0.60 | 0.56 | 0.05 | 0.70 | 0.69 | 0.05 |
| T2 to T3 | |||||||||
| YSR Anxiety | 0.48 | 0.46 | 0.09 | 0.52 | 0.51 | 0.06 | 0.58 | 0.61 | 0.06 |
| YSR Depressive | 0.42 | 0.38 | 0.08 | 0.48 | 0.53 | 0.08 | 0.55 | 0.57 | 0.08 |
| YSR Somatic | 0.53 | 0.51 | 0.08 | 0.43 | 0.43 | 0.08 | 0.63 | 0.66 | 0.08 |
| Cross-lagged paths | |||||||||
| T1 to T2 | |||||||||
| YSR Anxiety → YSR Depressive | 0.19 | 0.19 | 0.06 | 0.09 | 0.08 | 0.04 | 0.06 | 0.06 | 0.05 |
| YSR Anxiety → YSR Somatic | 0.06 | 0.05 | 0.06 | 0.05 | 0.04 | 0.05 | 0.01 | 0.01 | 0.05 |
| YSR Depressive → YSR Anxiety | 0.08 | 0.06 | 0.06 | 0.12 | 0.13 | 0.05 | 0.06 | 0.05 | 0.04 |
| YSR Depressive → YSR Somatic | 0.16 | 0.12 | 0.07 | 0.01 | 0.01 | 0.05 | 0.07 | 0.07 | 0.04 |
| YSR Somatic → YSR Anxiety | 0.04 | 0.04 | 0.05 | 0.11 | 0.12 | 0.05 | 0.15 | 0.13 | 0.04 |
| YSR Somatic → YSR Depressive | 0.02 | 0.02 | 0.06 | 0.09 | 0.09 | 0.04 | 0.11 | 0.11 | 0.04 |
| T2 to T3 | |||||||||
| YSR Anxiety → YSR Depressive | 0.24 | 0.24 | 0.08 | 0.19 | 0.20 | 0.06 | 0.18 | 0.19 | 0.05 |
| YSR Anxiety → YSR Somatic | 0.03 | 0.03 | 0.07 | 0.16 | 0.14 | 0.08 | 0.11 | 0.13 | 0.06 |
| YSR Depressive → YSR Anxiety | 0.16 | 0.14 | 0.08 | 0.14 | 0.15 | 0.07 | 0.11 | 0.11 | 0.04 |
| YSR Depressive → YSR Somatic | 0.14 | 0.11 | 0.06 | 0.01 | 0.01 | 0.06 | 0.09 | 0.10 | 0.06 |
| YSR Somatic → YSR Anxiety | 0.09 | 0.09 | 0.08 | 0.10 | 0.11 | 0.05 | 0.16 | 0.15 | 0.05 |
| YSR Somatic → YSR Depressive | 0.06 | 0.06 | 0.08 | −0.001 | −0.001 | 0.06 | 0.08 | 0.07 | 0.04 |
Note. Bolded are p < .05. β = standardized beta.
As seen in Fig. 1, there were group differences in which cross-lagged paths were significant across time although the paths did not significantly differ across groups in magnitude. The Vietnamese American and Vietnamese groups had five significant cross-lagged paths in common. Somatic symptoms predicted anxiety symptoms from T1 to T2, and from T2 to T3. Somatic symptoms also predicted depressive symptoms from T1 to T2. Depressive symptoms predicted anxiety symptoms from T2 to T3, and anxiety predicted depressive symptoms from T2 to T3. The Vietnamese American adolescents had one cross lagged path that was not shared across groups, with depressive symptoms also predicting anxiety from T1 to T2. For European American adolescents, only one type of cross-lagged relationship was significant, with anxiety predicting depressive symptoms from T1 to T2, and from T2 to T3. Although anxiety did not predict depressive symptoms for Vietnamese Americans and Vietnamese adolescents from T1 to T2, it did predict depressive symptoms from T2 to T3, for both groups.
Figure 1.
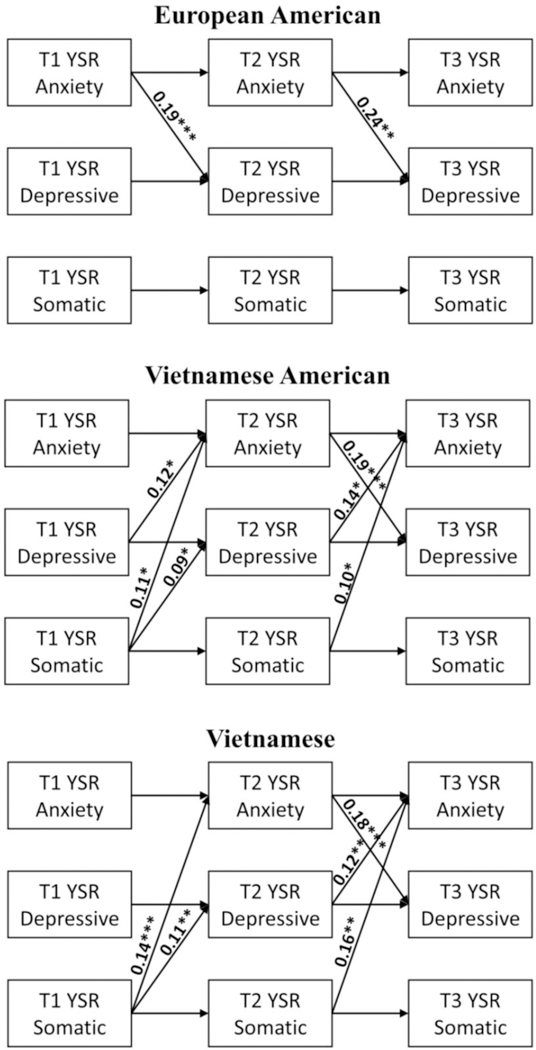
Significant paths for internalizing symptoms. Only cross-lagged standardized coefficients displayed. Covariates (sex, age), correlated errors for all symptoms at each timepoint, as well as between T1 and T3 are not shown in this figure. ***p ≤ .001, **p < .01, *p < .05.
4. Discussion
The present study examined cross-cultural differences in the prospective relationships among three domains of internalizing symptoms (somatic, anxiety, depressive) in Vietnamese, Vietnamese American, and European American adolescents. Our results support a long line of extant research that somatic complaints are an integral part of internalizing symptoms. There was also some support for culturally generalizable prospective linkages across symptom domains (i.e., T2 anxiety predicted T3 depressive symptoms for all three groups) as well as evidence of culturally distinctive patterns of cross-lagged associations (i.e., somatic complaints predicted anxiety and depressive symptoms for the Vietnamese and Vietnamese Americans, but not for the European-Americans). Considering the geographic distance of approximately 8,000 miles between Vietnam and the U.S., with questionnaires administered in different languages, the similarity of results across the Vietnamese and Vietnamese American groups emphasizes the underlying power of the cultural commonalities between them. The greater similarities in longitudinal symptom patterns for Vietnamese and Vietnamese American adolescents (sharing ethnocultural heritage) compared to Vietnamese American and European Americans (sharing the U.S. cultural context and from the same schools) underscores the importance of ethnocultural heritage values and norms in shaping symptom associations over time.
Prior research suggests that somatic symptoms may be emphasized in cultural contexts de-emphasizing emotional expression and accepting of somatic distress narratives [29], either for the purposes of communicating distress in a culturally-normative manner or due to differences in the actual experience of symptoms matching cultural expectations. Our study provides some evidence that the temporal influence of somatic symptoms is due to the actual distress experience over time rather than a communication preference. Private self-reports on questionnaires can reflect a communication preference for garnering support [30], and somatic symptom scores may have been higher than the cognitive-affective (anxiety or depressive) symptom scores if adolescents’ internalizing symptom reporting was modulated by selective presentation of symptoms fitting cultural norms of distress. However, somatic symptom scores were not the highest internalizing symptom domain for Vietnamese American and Vietnamese adolescents for whom this culturally adaptive symptom reporting style may apply. Somatic symptoms were endorsed alongside concurrent anxiety and depressive symptoms, suggesting that somatic symptoms are not experienced in isolation or to a greater extent. Rather, the cultural salience of somatic symptoms may be why later increases in anxiety or depressive symptoms are observed. Both Vietnamese American and Vietnamese adolescents are socialized in largely interdependent familial contexts in which cultural scripts signal what types of symptoms are more acceptable and warrant attention (i.e., somatic symptoms). Adolescents’ daily-lived cultural scripts may influence how cognitive-affective internalizing symptoms are increased at a later point in time (from somatic symptoms), rather than resulting in comparatively different endorsements of internalizing symptoms at any cross-sectional point in time. This potential influence of culture on the temporal sequence of symptoms may have been unrecognized in prior cross-cultural studies due to a time-limited focus on internalizing symptom reports.
Why might somatic symptoms predict increases in anxiety and depressive symptoms among Vietnamese American and Vietnamese adolescents? It is possible that although somatic symptoms are a culturally acceptable form of distress manifestation, the associated interim (i.e., 3 month) consequences of these symptoms in turn increase cognitive-affective distress that extends beyond the boundary of somatic symptoms. The YSR somatic narrowband symptoms are similar to functional somatic symptoms (i.e., symptoms not assumed to have psychiatric etiology but are medically-unexplained [55–57]) that can be highly disruptive to adolescents’ successful actualization of responsibilities and social roles. Longitudinal studies demonstrate that impairment from preceding symptoms strongly predicts future depression for adolescents [58]; likewise, somatic symptoms impairing social role-fulfillment may later create feelings of uncertainty, failure, or a desire to withdraw from others.
Initial depressive symptoms predicting anxiety could also represent a similar process among adolescents of interdependent cultural contexts. The YSR Withdrawn-Depressed narrowband involves items that reflect reduced social engagement in the family and social community, which may create internal dissonance for not fulfilling social roles as a child or peer. These resultant feelings may be captured by the YSR Anxiety-Depressed narrowband scale items such as guilt, nervousness, and low self-worth. Just as a cultural fit in behaviors and emotions (i.e., matching others’ behaviors or emotions and meeting cultural mandates) predicts well-being [18,19,59–61], it may be that a cultural misfit in symptom-related consequences predicts the opposite: further distress.
The cross-culturally significant prospective linkage from anxiety to depressive symptoms supports the notion that adolescents’ internalizing symptoms may be a result of anxiety-related behaviors (e.g., avoidance of settings that also have rewarding qualities) leading to factors (e.g., social withdrawal and lessened enjoyment) that increase risk for depression. The cross-lagged path from anxiety to depressive symptoms was significant across both time lags for the European Americans but only from T2 to T3 for the Vietnamese Americans and Vietnamese. T2 to T3 spans from Winter to Spring semester when final grades are determined. It is possible that for ethnically Vietnamese students, relatively greater cultural emphasis on educational vs. noneducational achievement [62] may amplify the anxiety-depressive symptom link when academic stress increases. Anxiety can be related to avoidant coping [63], and anxiety may culminate in depressive symptoms in the second semester when culturally congruent avoidant or accommodating behaviors become functionally maladaptive during periods of added pressure. In contrast, role-impairing somatic symptoms consistently predicted other internalizing symptoms across all time frames for Vietnamese and Vietnamese American teens.
One implication of our study relates to the prevention of depression. Prior research with adolescents has suggested targeting early anxiety symptoms for depression prevention [36–40,64], but the initial focus for adolescents of Vietnamese-heritage, and possibly for other adolescents in more interdependent cultures, may need to be with somatic symptoms. Providing ways to recognize psychosocial influences on somatic symptoms, and providing strategies for coping with somatic symptoms and the related socio-environmental factors could reduce risk for future depression. It will also be important to provide this support within appropriate cultural framing, for adolescents to improve their understanding of what contributes to the development and maintenance of internalizing symptoms within their cultural context (e.g., how cultural expectations shape distress experiences and progression of symptoms).
One consideration for our study findings is the three month longitudinal lag. It is possible that other predictive symptom patterns might emerge if adolescents are followed for shorter or longer periods of time. Another consideration is that the study used adolescents’ self-report of symptoms but these, nevertheless, robustly predict psychiatric diagnoses [65] and other adjustment indices such as suicidality [66]. Moreover, including other informants (e.g., parents, teachers, peers) would be interesting for understanding how adolescents are perceived by others and how this relates to internalizing symptoms prospectively. Promising directions for future research include further unpacking cultural group variations by examining how specific cultural orientations, values, and norms contribute to differentiated prospective trajectories of internalizing symptoms, as well as gender comparisons of symptoms considering the differing rates of internalizing during adolescence.
Acknowledgements
Funding: This research was supported by the National Institute of Mental Health (R01 MH077697), the UCLA Asian American Studies Center, and the Peabody College of Education and Human Development (PIF Fund 6402). Jacqueline H. J. Kim was supported by the National Institute of Mental Health (5 T32 MH015750; Christine Dunkel Schetter).
Appendix A.
Correlations between study variables for each cultural group
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Sexa | -- | ||||||||||
| 2. Age | −.01/−.03/−.05 | -- | |||||||||
| 3. T1 YSR Anxiety | .16/−.02/−.11 | .09/.00/.05 | -- | ||||||||
| 4. T1 YSR Depressive | .05/.06/−.03 | .04/.04/.09 | .70/.59/.65 | -- | |||||||
| 5. T1 YSR Somatic | .15/.01/−.13 | .05/.03/.12 | .51/.53/.71 | .50/.42/.56 | -- | ||||||
| 6. T2 YSR Anxiety | .15/.10/−.11 | .02/.00/.04 | .77/.71/.67 | .59/.51/.48 | .41/.46/.55 | ||||||
| 7. T2 YSR Depressive | .05/.06/−.01 | .05/.04/.13 | .63/.49/.51 | .74/.71/.68 | .39/.38/.48 | .74/.62/.68 | -- | ||||
| 8. T2 YSR Somatic | .11/.04/−.13 | .07/−.01/.13 | .40/.35/.54 | .40/.27/.46 | .55/.64/.73 | .50/.50/.69 | .51/.46/.60 | -- | |||
| 9. T3 YSR Anxiety | .11/.05/−.06 | .05/.03/.02 | .67/.64/.72 | .50/.47/.56 | .35/.39/.60 | .71/.73/.80 | .57/.54/.61 | .40/.42/.63 | -- | ||
| 10. T3 YSR Depressive | .05/.09/−.02 | .08/.02/.09 | .53/.46/.54 | .64/.67/.72 | .33/.31/.51 | .58/.53/.62 | .69/.71/.79 | .40/.33/.55 | .77/.65/.70 | -- | |
| 11. T3 YSR Somatic | .18/.05/−.08 | .15/.01/.14 | .40/.31/.55 | .42/.26/.53 | .47/.57/.78 | .39/.40/.63 | .42/.35/.56 | .63/.64/.84 | .57/.58/.72 | .58/.47/.62 | -- |
Note. Bolded are p < .05. Correlations shown in this order: European American/ Vietnamese American/ Vietnamese.
1 = Male and 2 = Female.
Footnotes
Declaration of Competing Interest
The authors have no competing interests to report.
Contributor Information
Jacqueline H. J. Kim, Department of Psychology, University of California, Los Angeles
William Tsai, Department of Applied Psychology, New York University
Tamar Kodish, Department of Psychology, University of California, Los Angeles
Lam T. Trung, Da Nang Psychiatric Hospital
Anna S. Lau, Department of Psychology, University of California, Los Angeles
Bahr Weiss, Department of Psychology and Human Development, Vanderbilt University
References
- 1.Achenbach TM, Edelbrock CS, The classification of child psychopathology: a review and analysis of empirical efforts, Psychol. Bull. 85 (6) (1978) 1275–1301. [PubMed] [Google Scholar]
- 2.Henningsen P, Löwe B, Depression, pain, and somatoform disorders, Curr. Opin. Psychiatry 19 (1) (2006. January) 19–24. [DOI] [PubMed] [Google Scholar]
- 3.Campo JV, Jansen-Mcwilliams L, Comer DM , Somatization in pediatric primary care: association with psychopathology, functional impairment, and use of services, J. Am. Acad. Child Adolesc. Psychiatry 38 (9) (1999) 1093–1101. [DOI] [PubMed] [Google Scholar]
- 4.Löwe B, Spitzer RL, Williams JBW, et al. , Depression, anxiety and somatization in primary care: syndrome overlap and functional impairment, Gen. Hosp. Psychiatry 30 (3) (2008) 191–199. [DOI] [PubMed] [Google Scholar]
- 5.Clark LA, Watson D, Tripartite model of anxiety and depression: psychometric evidence and taxonomic implications, J. Abnorm. Psychol. 100 (3) (1991) 316–336. [DOI] [PubMed] [Google Scholar]
- 6.Simms LJ, Prisciandaro JJ, Krueger RF, et al. , The structure of depression, anxiety and somatic symptoms in primary care, Psychol. Med. 42 (1) (2012) 15–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ivanova MY, Achenbach TM, Rescorla LA, et al. , The generalizability of the youth selfreport syndrome structure in 23 societies, J. Consult. Clin. Psychol. 75 (5) (2007) 729–738. [DOI] [PubMed] [Google Scholar]
- 8.Rescorla LA, Ginzburg S, Achenbach TM, et al. , Cross-informant agreement between parent-reported and adolescent self-reported problems in 25 societies, J. Clin. Child Adolesc. Psychol. 42 (2) (2013) 262–273. [DOI] [PubMed] [Google Scholar]
- 9.Ivanova MY, Achenbach TM, Rescorla LA, et al. , Testing syndromes of psychopathology in parent and youth ratings across societies, J. Clin. Child Adolesc. Psychol. 48 (4) (2019) 596–609. [DOI] [PubMed] [Google Scholar]
- 10.Jacobson NC, Newman MG, Anxiety and depression as bidirectional risk factors for one another: a meta-analysis of longitudinal studies, Psychol. Bull. 143 (11) (2017) 1155–1200. [DOI] [PubMed] [Google Scholar]
- 11.Anderson ER, Hope DA, A review of the tripartite model for understanding the link between anxiety and depression in youth, Clin. Psychol. Rev. 28 (2) (2008) 276–288. [DOI] [PubMed] [Google Scholar]
- 12.Weersing VR, Rozenman MS, Maher-Bridge M, et al. , Anxiety, depression, and somatic distress: developing a transdiagnostic internalizing toolbox for pediatric practice, Cogn. Behav. Pract. 19 (1) (2012) 68–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Vaccarino AL, Sills TL, Evans KR, et al. , Prevalence and association of somatic symptoms in patients with Major Depressive Disorder, J. Affect. Disord. 110 (3) (2008) 270–276. [DOI] [PubMed] [Google Scholar]
- 14.Egger HL, Costello EJ, Erkanli A, et al. , Somatic complaints and psychopathology in children and adolescents: stomach aches, musculoskeletal pains, and headaches, J. Am. Acad. Child Adolesc. Psychiatry 38 (7) (1999) 852–860. [DOI] [PubMed] [Google Scholar]
- 15.Lipsitz JD, Masia-Warner C, Apfel H, et al. , Anxiety and depressive symptoms and anxiety sensitivity in youngsters with noncardiac chest pain and benign heart murmurs, J. Pediatr. Psychol. 29 (8) (2004) 607–612. [DOI] [PubMed] [Google Scholar]
- 16.Lieb R, Meinlschmidt G, Araya R, Epidemiology of the association between somatoform disorders and anxiety and depressive disorders: an update, Psychosom. Med. 69 (9) (2007) 860–863. [DOI] [PubMed] [Google Scholar]
- 17.Campo JV, Bridge J, Ehmann M, et al. , Recurrent abdominal pain, anxiety, and depression in primary care, Pediatrics 113 (4) (2004) 817–824. [DOI] [PubMed] [Google Scholar]
- 18.Kitayama S, Karasawa M, Curhan KB, et al. , Independence and interdependence predict health and wellbeing: divergent patterns in the United States and Japan, Front. Psychol. 1 (2010) 163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.De Leersnyder J, Kim H, Mesquita B, Feeling right is feeling good: psychological well-being and emotional fit with culture in autonomy versus relatedness-promoting situations, Front. Psychol. 6 (May) (2015) 630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ryder AG, Yang J, Zhu X, et al. , The cultural shaping of depression: somatic symptoms in China, psychological symptoms in North America? J. Abnorm. Psychol. 117 (2) (2008) 300–313. [DOI] [PubMed] [Google Scholar]
- 21.Dreher A, Hahn E, Diefenbacher A, et al. , Cultural differences in symptom representation for depression and somatization measured by the PHQ between Vietnamese and German psychiatric outpatients, J. Psychosom. Res. 102 (September) (2017) 71–77. [DOI] [PubMed] [Google Scholar]
- 22.Ryder AG, Yang J, Heine SJ, Somatization vs. Psychologization of Emotional Distress: A Paradigmatic Example for Cultural Psychopathology, Online Readings Psychol. Cult. 10 (2) (2002). [Google Scholar]
- 23.Parker G, Cheah YC, Roy K, Do the Chinese somatize depression? A cross-cultural study, Soc. Psychiatry Psychiatr. Epidemiol. 36 (6) (2001. June) 287–293. [DOI] [PubMed] [Google Scholar]
- 24.Markus HR, Kitayama S, Culture and the self: implications for cognition, emotion, and motivation, Psychol. Rev. 98 (2) (1991) 224–253. [Google Scholar]
- 25.Matsumoto D, Yoo SH, Fontaine J, et al. , Mapping expressive differences around the world: the relationship between emotional display rules and individualism versus collectivism, J. Cross-Cult. Psychol. 39 (1) (2008) 55–74. [Google Scholar]
- 26.Butler EA, Lee TL, Gross JJ, Emotion regulation and culture: are the social consequences of emotion suppression culture-specific? Emotion. 7 (1) (2007) 30–48. [DOI] [PubMed] [Google Scholar]
- 27.Le BM, Impett EA, When holding back helps: suppressing negative emotions during sacrifice feels authentic and is beneficial for highly interdependent people, Psychol. Sci. 24 (9) (2013) 1809–1815. [DOI] [PubMed] [Google Scholar]
- 28.Taylor SE, Sherman DK, Kim HS, et al. , Culture and social support: who seeks it and why? J. Pers. Soc. Psychol. 87 (3) (2004) 354–362. [DOI] [PubMed] [Google Scholar]
- 29.Choi E, Chentsova-Dutton Y, Parrott WG, The effectiveness of somatization in communicating distress in Korean and American cultural contexts, Front. Psychol. 7 (March 2016) 383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Weiss B, Tram JM, Weisz JR, et al. , Differential symptom expression and somatization in Thai vs. American children, J. Consult. Clin. Psychol. 77 (5) (2009) 987–992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ryder AG, Chentsova-Dutton YE, Depression in cultural context: “Chinese somatization,” revisited, Psychiatric Clinics of North America 35 (2012) 15–36 Elsevier. [DOI] [PubMed] [Google Scholar]
- 32.Konijnenberg AY, Uiterwaal CSPM, Kimpen JLL, et al. , Children with unexplained chronic pain: substantial impairment in everyday life, Arch. Dis. Child. 90 (7) (2005) 680–686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Claar RL, Walker LS, Smith CA, Functional disability in adolescents and young adults wroth symptoms of irritable bowel syndrome: the role of academic, social, and athletic competence, J. Pediatr. Psychol. 24 (3) (1999) 271–280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Roth-Isigkeit A, Pain among children and adolescents: restrictions in daily living and triggering factors, Pediatrics 115 (2) (2005) e152–e162. [DOI] [PubMed] [Google Scholar]
- 35.Rohde P, Lewinsohn PM, Klein DN, et al. , Key characteristics of major depressive disorder occurring in childhood, adolescence, emerging adulthood, and adulthood, Clin. Psychol. Sci 1 (1) (2013) 41–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gallerani CM, Garber J, Martin NC, The temporal relation between depression and comorbid psychopathology in adolescents at varied risk for depression, J. Child Psychol. Psychiatry 51 (3) (2010) 242–249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kovacs M, Gatsonis C, Paulauskas SL, et al. , Depressive disorders in childhood, Arch. Gen. Psychiatry 46 (9) (1989) 776–782. [DOI] [PubMed] [Google Scholar]
- 38.Rohde P, Lewinsohn PM, Seeley JR, Comorbidity of unipolar depression: II. Comorbidity with other mental disorders in adolescents and adults, J. Abnorm. Psychol. 100 (2) (1991) 214. [PubMed] [Google Scholar]
- 39.Cole DA, Peeke LG, Martin JM, et al. , A longitudinal look at the relation between depression and anxiety in children and adolescents, J. Consult. Cin. Psychol. 66 (3) (1998) 451–460. [DOI] [PubMed] [Google Scholar]
- 40.Brady EU, Kendall PC, Comorbidity of anxiety and depression in children and adolescents: 20 years after, Psychol. Bull. 111 (2) (1992) 244–255. [DOI] [PubMed] [Google Scholar]
- 41.Price RB, Rosen D, Siegle GJ, et al. , From anxious youth to depressed adolescents: prospective prediction of 2-year depression symptoms via attentional bias measures, J. Abnorm. Psychol. 125 (2) (2016) 267–278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Winer ES, Bryant J, Bartoszek G, et al. , Mapping the relationship between anxiety, anhedonia, and depression, J. Affect. Disord. 221 (2017) 289–296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Thomsen KR, Measuring anhedonia: impaired ability to pursue, experience, and learn about reward, Front. Psychol. 6 (September) (2015) 1409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Holmbeck GN, Kendall PC. Introduction to the special section on clinical adolescent psychology: developmental psychopathology and treatment, J. Consult. Clin. Psychol. 70 (1) (2002) 3. [PubMed] [Google Scholar]
- 45.Ask H, Waaktaar T, Seglem KB, et al. , Common etiological sources of anxiety, depression, and somatic complaints in adolescents: a multiple rater twin study, J. Abnorm. Child Psychol. 44 (1) (2016) 101–114. [DOI] [PubMed] [Google Scholar]
- 46.Janssens KAM, Rosmalen JGM, Ormel J, et al. , Anxiety and depression are risk factors rather than consequences of functional somatic symptoms in a general population of adolescents: the TRAILS study, J. Child Psychol. Psychiatry 51 (3) (2010) 304–312. [DOI] [PubMed] [Google Scholar]
- 47.Nguyen NA, Williams HL, Transition from East to West: Vietnamese adolescents and their parents, J. Am. Acad. Child Adolesc. Psychiatry 28 (4) (1989) 505–515. [DOI] [PubMed] [Google Scholar]
- 48.Phan T, Interdependent self: Self-perceptions of Vietnamese-American youths, Adolescence 40 (158) (2005) 425–441. [PubMed] [Google Scholar]
- 49.Matsumoto D, Yoo SH, Nakagawa S, et al. , Culture, emotion regulation, and adjustment, J. Pers. Soc. Psychol. 94 (6) (2008) 925–937. [DOI] [PubMed] [Google Scholar]
- 50.Achenbach TM, Rescorla LA, Manual for the ASEBA School-age Forms & Profiles, University of Vermont, Research Center for Children, Youth, & Families, Burlington, VT, 2001. [Google Scholar]
- 51.Achenbach TM, Achenbach system of empirically based assessment (ASEBA), Encycl. Clin. Neuropsychol. (2018) 26–33. [Google Scholar]
- 52.Achenbach TM, Becker A, Döpfner M, et al. , Multicultural assessment of child and adolescent psychopathology with ASEBA and SDQ instruments: research findings, applications, and future directions, J. Child Psychol. Psychiatry Allied Discip. 49 (3) (2008) 251–275. [DOI] [PubMed] [Google Scholar]
- 53.Achenbach TM, Rescorla LA, Sach huong dan su dung phieu hoi he thong danh gia Achenbach (ASEBA), Vietnam National University Press, Hanoi, 2012. [Google Scholar]
- 54.Singelis TM, The measurement of independent and interdependent self-construals, Personal. Soc. Psychol. Bull. 20 (5) (1994) 580–591. [Google Scholar]
- 55.Mayou R, Farmer A, ABC of psychological medicine: functional somatic symptoms and syndromes, BMJ 325 (3) (2002) 265–268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Wessely S, Nimnuan C, Sharpe M, Functional somatic syndromes: one or many? Lancet. 354 (9182) (1999) 936–939. [DOI] [PubMed] [Google Scholar]
- 57.Beck JE, A developmental perspective on functional somatic symptoms, J. Pediatr. Psychol. 33 (5) (2008) 547–562. [DOI] [PubMed] [Google Scholar]
- 58.Bittner A, Goodwin RD, Wittchen HU, et al. , What characteristics of primary anxiety disorders predict subsequent major depressive disorder? J. Clin. Psychiatry 65 (5) (2004) 618–626. [DOI] [PubMed] [Google Scholar]
- 59.Diener E, Oishi S, Lucas RE, Personality, culture, and subjective well-being: emotional and cognitive evaluations of life, Annu. Rev. Psychol 54 (1) (2003) 403–425. [DOI] [PubMed] [Google Scholar]
- 60.Kang S-M, Shaver PR, Sue S, et al. , Culture-specific patterns in the prediction of life satisfaction: roles of emotion, relationship quality, and self-esteem, Personal. Soc. Psychol. Bull. 29 (12) (2003) 1596–1608. [DOI] [PubMed] [Google Scholar]
- 61.Tsai JL, Knutson B, Fung HH, Cultural variation in affect valuation, J. Pers. Soc. Psychol. 90 (2) (2006) 288–307. [DOI] [PubMed] [Google Scholar]
- 62.Sue S, Okazaki S, Asian-American educational achievements: a phenomenon in search of an explanation, Am. Psychol. 45 (8) (1990) 913–920. [DOI] [PubMed] [Google Scholar]
- 63.Braje SE, Hall GCN, Coping as a mediator between losing face and depressive and social anxiety symptoms among Asian Americans, J. Cross-Cult. Psychol. 47 (8) (2016) 1114–1129. [Google Scholar]
- 64.Snyder J, Bullard L, Wagener A, et al. , Childhood anxiety and depressive symptoms: trajectories, relationship, and association with subsequent depression, J. Clin. Child Adolesc. Psychol. 38 (6) (2009) 837–849. [DOI] [PubMed] [Google Scholar]
- 65.Morgan CJ, Cauce AM, Predicting DSM-III-R disorders from the youth self-report: analysis of data from a field study, J. Am. Acad. Child Adolesc. Psychiatry 38 (10) (1999) 1237–1245. [DOI] [PubMed] [Google Scholar]
- 66.Ivarsson T, Gillberg C, Arvidsson T, et al. , The Youth Self-Report (YSR) and the Depression Self-Rating Scale (DSRS) as measures of depression and suicidality among adolescents, Eur. Child Adolesc. Psychiatry 11 (1) (2002) 31–37. [DOI] [PubMed] [Google Scholar]


