Abstract
Background and Purpose:
The DEFUSE 3 trial demonstrated that endovascular thrombectomy in the 6-16 hour time window improves functional outcomes of patients with evidence of salvageable tissue on baseline CT or MRI. The purpose of this study is to assess the effect of endovascular therapy on length of hospital stay, home-time during the first 3 months post-stroke, and living situation post-stroke in DEFUSE 3.
Methods:
Duration of hospital stay and home-time (number of days during the 90-day post-stroke period that the patient resides in their own home or in that of a relative) were compared between treatment groups using the Wilcoxon rank-sum test. Patient living situation was assessed at discharge, 30 days, and 90 days on an ordinal 4-point scale (home, acute rehabilitation unit, institutionalized care, or hospice/death) and differences between groups were analyzed using the Cochran-Armitage trend test.
Results:
Median length of hospital stay was 9.1 (IQR, 6.2–15.0) days in the medical group vs. 6.5 (IQR, 3.7–9.3) days in the endovascular group (p<0.001). Median home-time during the first 90 days following stroke was 0 (IQR, 0 –53) days in the medical group vs. 55 (IQR, 0–83) days in the endovascular group (p<0.001). The endovascular group had more favorable living situations at time of discharge (p<0.001), 30 days (p<0.001), and 90 days (p<0.001) post-stroke.
Conclusions:
Endovascular thrombectomy resulted in reduced hospital stay, more home-time, and more desirable living situations in the 90 days after stroke. These results provide evidence that endovascular therapy in the delayed time window can improve quality of life for stroke patients and reduce healthcare costs.
Keywords: stroke, brain ischemia, quality of life, endovascular treatment, hospital stay
BACKGROUND
Recent clinical trials have demonstrated that endovascular thrombectomy is effective in the treatment of ischemic stroke beyond the previously accepted window of 6 hours from stroke symptom onset.1,2 The DAWN (DWI or CTP Assessment with Clinical Mismatch in the Triage of Wake Up and Late Presenting Strokes Undergoing Neurointervention with Trevo) and DEFUSE 3 (Endovascular Therapy Following Imaging Evaluation for Ischemic Stroke) trials showed improved 90-day functional outcomes among patients who had evidence of salvageable brain tissue on CT or MR perfusion imaging and received thrombectomy more than 6 hours after stroke onset.1,2 While 90-day functional status is the standard primary outcome for acute stroke trials, secondary outcome measures may provide additional useful data. For example, the ability of a patient to return to live at home may be an important determinant of quality of life post-stroke, and both length of hospital stay and living situation post-stroke are relevant in terms of healthcare costs.
In this study, we aimed to determine the effect of endovascular treatment on length of hospitalization, home-time, and living situation in the 90 days post-stroke in DEFUSE 3.
METHODS
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Study Design
The study design for DEFUSE 3 has been published previously.1 The DEFUSE 3 trial was an open-label randomized controlled trial with blinded outcome assessment that compared endovascular therapy plus medical therapy versus medical therapy alone in stroke patients presenting in the 6- to 16-hour time window with imaging evidence of large vessel occlusion and salvageable brain tissue.1 The study was approved by a Central Institutional Review Board and all patients or their proxy provided informed consent.
Outcomes
The outcomes of interest in this study were length of hospital stay, living situation post-stroke (immediately after hospital discharge and at 30 and 90 days post-stroke), and home-time during the 90 days post-stroke.
Living Situation:
Discharge destination after the acute hospitalization and living location at 30 and 90 days post-stroke were obtained from the patient, their caregiver, or the medical record. Living situation was classified into one of four categories: 1) Home, defined as the patient’s home or the home of a relative; 2) Acute rehabilitation, defined as a transitional facility or hospital ward designed for physical medicine and rehabilitation; 3) Institutionalized care or skilled nursing facility, defined as a facility that provides 24-hour assistance with healthcare and activities of daily living; and 4) Death, which included patients who had died as well as patients discharged on hospice care (n=12; all died in the 90-day post-stroke period with a median time from hospital discharge to death of 4 days).
Length of Hospital Stay:
Length of hospital stay was considered the duration of time from patient arrival at the enrollment hospital to discharge. In cases of readmission to any acute care hospital, the time of the subsequent hospitalization was included in the overall length of hospitalization. Study coordinators queried the medical records, the patient, and/or their caregiver about any hospital readmissions during the 30- and 90-day follow-up visits and each readmission prompted the collection of the patient’s hospital records. Patients who died during acute hospitalization were not included in this analysis (n=15).
Home-Time:
Home-time was defined as the number of days during the 90-day post-stroke period that a patient spends residing in their own home or in that of a relative.3 Home-time was calculated by subtracting the days spent in the hospital for acute stroke treatment plus the number of days spent at any other facility (acute rehabilitation unit or institutionalized care) from a total of 90 days.
Statistical Analyses
The effect of treatment on length of hospital stay and home-time was assessed with the Wilcoxon rank-sum test. The effect of treatment on living situation (ordinally ranked as home, acute rehabilitation, institutionalized care, and death) and functional outcome (ordinally ranked by the modified Rankin Scale) at 90 days stratified by living situation was assessed with the Cochran-Armitage trend test. All statistical tests were two-sided and conducted using a level of significance of 0.05. Statistical analysis was performed with SAS version 9.4.
RESULTS
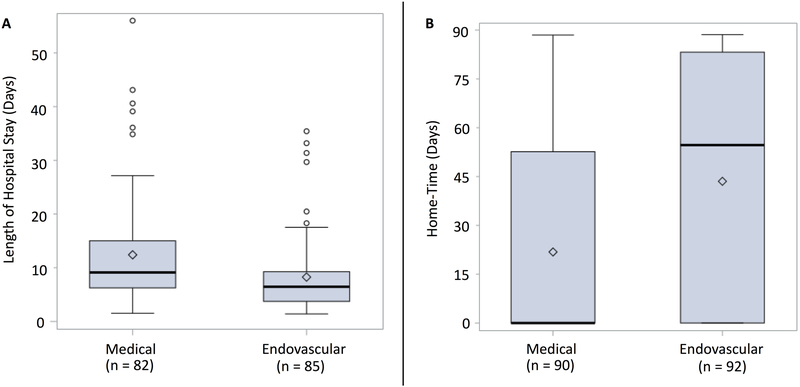
A total of 182 patients underwent randomization (92 to endovascular therapy and 90 to medical therapy). Among the 167 patients who did not die during acute hospitalization, median length of hospital stay was 9.1 (IQR, 6.2–15.0) days in the medical group vs. 6.5 (IQR, 3.7–9.3) days in the endovascular group (p<0.001, Figure 1A). Median home-time during the first 90 days post-stroke was 0 (IQR, 0–53) days in the medical group vs. 55 (IQR, 0–83) days in the endovascular group (p<0.001) and mean home-time was 22 days (SD 33) in the medical group vs. 44 days (SD 38) in the endovascular group (Figure 1B).
Figure 1. Boxplot showing length of hospital stay (A) and home-time (B) by treatment group.
Black bars represent medians. Diamonds represent means. Circles represent outliers.
A – Length of hospital stay in days was decreased in the endovascular group compared to the medical group.
B – Home-time was increased in the endovascular group compared to the medical group.
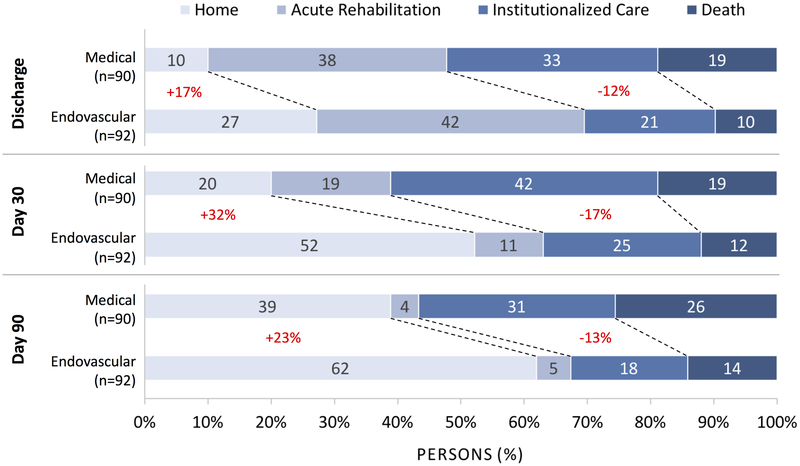
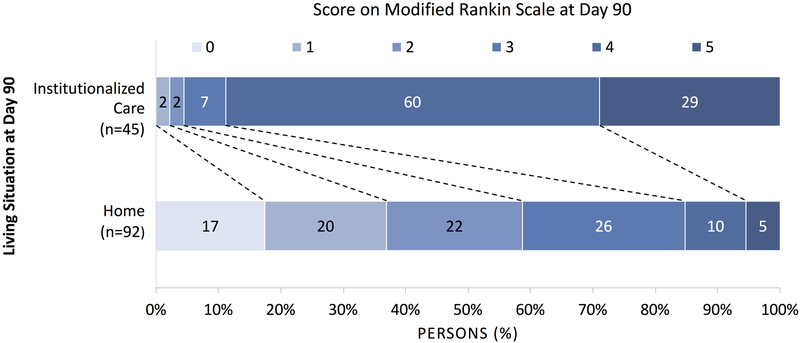
Endovascular therapy was associated with a favorable shift in the distribution of living situation away from institutionalized care and death and towards home, at time of discharge, 30 days, and 90 days post-stroke (p<0.001 for all time-points, Figure 2). At day 90, patients living at home had better functional outcomes as measured by the modified Rankin Scale compared to patients living in institutionalized care (p<0.001, Figure 3). The percentage of patients who were functionally independent (mRS≤2) was 59% among patients at home vs. 4% among patients in institutionalized care.
Figure 2. Discharge destination and living situation at 30 and 90 days post-stroke.
Percentage of patients in the medical and endovascular groups with living situation categorized as home, acute rehabilitation, institutionalized care, or death at time of hospital discharge, 30 days, and 90 days post-stroke.
Figure 3. Functional outcomes at 90 days stratified by living situation.
At 90 days post-stroke, patients living in institutionalized care had worse functional outcomes compared to patients living at home.
DISCUSSION
Endovascular thrombectomy in the 6-16 hour time window is associated with more favorable outcomes for length of hospital stay, home-time, and living situation during the 90 days post-stroke.
Our results indicate that length of hospital stay is reduced by a median of 2.6 days with endovascular therapy (29% reduction). These results are consistent with findings from EXTEND-IA (Extending the Time for Thrombolysis in Emergency Neurological Deficits – Intra-Arterial), which found that the median length of stay in the acute stroke unit was reduced by 3 days with endovascular therapy.4 The reduced length of hospital stay with endovascular therapy seen in DEFUSE 3 will have an important impact on the overall costs associated with acute ischemic stroke care as the average cost per inpatient day is $1,878 in the US.4
The absolute effect of endovascular therapy on home-time was even more profound. In DEFUSE 3, median home-time was increased by 55 days with endovascular therapy. This is consistent with the treatment benefit of thrombectomy in EXTEND-IA, which showed an increase in median home-time of 58 days in the endovascular group.5 Increased home-time has important implications for patient quality of life and well-being as home-time has been shown to be a highly desired outcome by patients post-stroke.3
Our results show a favorable shift in living situation with endovascular therapy at all time points from hospital discharge to 90 days post-stroke. We also demonstrated better functional outcomes among patients living at home compared to those living in institutionalized care. Other studies have shown that two key features of living at home —faster community reintegration and reduced reliance on medical aides and health professionals— contribute to improved quality of life.6 Taken together, these findings indicate that endovascular therapy not only results in better functional outcomes, but also in more favorable living situations associated with improved quality of life. The favorable shift in living situation is associated with significant cost savings, as the average cost of a private room for nursing home care is $275 daily or $100,375 annually in the US.7
A limitation of this study is that we were unable to adjust for variables which may influence post-stroke living situation. For example, pre-stroke living arrangement, which was not documented in DEFUSE 3, is known to be an important predictor of discharge to home. Level of family support is also likely an important factor influencing post-stroke living situation. Lastly, patient insurance status, the availability of discharge services, and other economic factors can influence hospital stay and post-discharge living situation. Although we were not able to control for these potential confounding variables, they were likely balanced between treatment groups because of randomization. Another limitation of this study is that the results depend heavily on the healthcare infrastructure at the study centers. Since DEFUSE 3 was only conducted at US sites, the results may not extrapolate to other countries.
In conclusion, this study demonstrates that endovascular therapy shortens length of hospital stay, increases home-time, and results in more desirable living situations in the 90 days post-stroke. Each of these outcomes provides additional evidence for the effectiveness of endovascular therapy in the delayed time window and captures other elements of the benefit of this treatment. These results also provide valuable data to inform cost-effectiveness studies of endovascular therapy.
Supplementary Material
Acknowledgments
Funding Sources
The study was funded by two grants from the National Institute for Neurological Disorders and Stroke (U10NS086487 and U01NS092076, Albers).
Footnotes
Potential Conflicts of Interest
GW Albers has equity in and is a consultant for iSchemaView, which produces the software used in DEFUSE 3 for post-processing of CT and MR perfusion studies. GW Albers holds a patent related to that software and has been a consultant for Medtronic. JJ Heit is a consultant for Medtronic and MicroVention and a member of the iSchemaView Medical and Scientific Advisory Board. M Marks is a shareholder in ThrombX Medical.
Clinical Trial Registration Information:
URL: http://www.clinicaltrials.gov. Unique identifier: .
REFERENCES
- 1.Albers GW, Marks MP, Kemp S, Christensen S, Tsai JP, Ortega-Gutierrez S, et al. Thrombectomy for Stroke at 6 to 16 Hours with Selection by Perfusion Imaging. N Engl J Med. 2018;378:708–718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nogueira RG, Jadhav AP, Haussen DC, Bonafe A, Budzik RF, Bhuva P, et al. Thrombectomy 6 to 24 Hours after Stroke with a Mismatch between Deficit and Infarct. N Engl J Med. 2018;378:11–21. [DOI] [PubMed] [Google Scholar]
- 3.Quinn TJ, Dawson J, Lees JS, Chang TP, Walters MR, Lees KR, et al. Time Spent at Home Poststroke: “Home-Time” a Meaningful and Robust Outcome Measure for Stroke Trials. Stroke. 2008;39:231–233. [DOI] [PubMed] [Google Scholar]
- 4.Rappleye E Average Cost per Inpatient Day Across 50 States. Becker’s Hospital Review. https://www.beckershospitalreview.com/finance/average-cost-per-inpatient-day-across-50-states.html. Accessed January 31, 2019.
- 5.Campbell BCV, Mitchell PJ, Churilov L, Keshtkaran M, Hong KS, Kleinig TJ, et al. Endovascular Thrombectomy for Ischemic Stroke Increases Disability-Free Survival, Quality of Life, and Life Expectancy and Reduces Cost. Front Neurol. 2017;8:657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brosseau L, Potvin L, Philippe P, Boulanger YL. Post-stroke Inpatient Rehabilitation. II. Predicting Discharge Disposition. Am J Phys Med Rehabil. 1996;75:431–436. [DOI] [PubMed] [Google Scholar]
- 7.Cost of Long Term Care. Cost of Care Survey 2018. Genworth Financial, Inc; https://www.genworth.com/aging-and-you/finances/cost-of-care.html. Accessed January 31, 2019. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.