Abstract
Working or studying is a common goal among people with recent-onset psychosis. Cognitive deficits have been reported to influence occupational outcome, but to date few studies have evaluated if cognitive deficits independently predict occupational outcome when taking into account other important determinants, such as self-esteem, motivation, length of time absent from employment/school, job/school search behaviours, subjective cognitive complaints and psychotic symptoms. Hence, this longitudinal study aimed to evaluate the role of cognition, as well as other key factors relevant to occupational outcome, to predict occupational status six months after baseline in people with recent-onset psychosis. A total of 27 participants receiving treatment in rehabilitation programs were included in the study. Neuropsychological, psychological, clinical and occupational measures were administered at baseline, and occupational status was collected six months later. Ordinal regression indicated that working memory and length of time absent from employment/school at baseline predicted 48.1% of the variance of occupational status at six months, with both variables showing a unique significant contribution to the model. These results suggest that working memory could be integrated in comprehensive models of occupational outcome in people with recent-onset psychosis. In addition, supported employment and education programs could target cognitive deficits and length of time absent from employment/school to help these individuals to acquire a job or return to school given their strong predictive value on occupational outcome.
Keywords: Recent-onset psychosis, Cognition, Occupational outcome, Recovery, Rehabilitation program, Cognitive remediation
1. Introduction
Personal recovery is defined as the process of achieving a full, satisfying and meaningful life beyond one's illness and associated symptoms (Roe et al., 2007). In this context, job acquisition or returning to school is a common yet challenging goal for people with a psychotic disorder (Brown, 2011; Morgan et al., 2012; Rinaldi et al., 2010), due to which it has become a major treatment target (Doroud et al., 2015; Mueser et al., 2013). Despite the positive results reported by some interventional studies supporting employment/education (e.g., Carmona et al., 2017), it is estimated that only 20% have a paid job (Rosenheck et al., 2006). Furthermore, chances of gaining employment drop from 52% at diagnosis to 25% one year after a psychiatric diagnosis (Marwaha and Johnson, 2004), which reflects the pivotal role of the first few years of illness. This high unemployment rate is also associated with high costs for society in health care and financial support (e.g., pension disability, welfare) (Neil et al., 2014). Education is also disrupted, with 44% of people with a psychotic disorder having dropped-out of school (compared to 13–18% in the general population; Goulding et al., 2010) It is thus of importance to better understand the barriers to occupational outcome in order to inform practitioners and guide interventions for people with psychiatric disorders.
In the most recent meta-analysis on factors predicting successful occupational outcomes Tsang et al. (2010), include among those negative symptoms, age, level of education, marital status, public support, diagnosis and cognitive deficits (executive functioning and general intelligence). However, since occupational disruptions tend to occur in the early stages of the illness (Goulding et al., 2010), there is a need for more studies on the determinants not only of job acquisition, but also of returning to school, in a recent-onset psychosis population, in order to lead interventions to prevent long-term disabilities (Alvarez-Jimenez et al., 2012). Indeed, the first five years of the disorder is widely known to be a critical period to implant interventions and enhance recovery (Birchwood et al., 1998).
Some existing neurocognitive studies assessing individuals with recent-onset psychosis have reported an association of poor occupational functioning with cognitive deficits such as attention (Milev et al., 2005; Tandberg et al., 2011), working memory (Grau et al., 2016), speed of processing (Milev et al., 2005; Stouten et al., 2017), intelligence quotient (IQ) (Bratlien et al., 2013) and social cognition (Achim et al., 2012, Achim et al., 2013; Fett et al., 2011; Horan et al., 2012; Ventura et al., 2015). However, in their review on recent-onset psychosis, Allott et al. (2011) found no association between cognitive deficits and job acquisition. Moreover, a study conducted by Nuechterlein et al. (2011) assessing a recent-onset population found that working memory, attention, early processing, verbal memory and speed of processing explained 52% of the variance of job acquisition or return to school. While this percentage is high, it would have been interesting to include social cognition, defined as the mental processes underlying social interactions, including the abilities involved in perceiving and interpreting social information in order to guide social interactions (Pinkham, 2014), since it is a variable that could influence occupational outcome (Ventura et al., 2015). In addition, measuring one's job acquisition or return to school is often done using a dichotomous variable (i.e., yes/no) or a general occupational functioning scale. This dichotomous variable is thus not able to account for factors such as the number of hours spent at work/school or the number of hours spent at non-competitive occupations (e.g., volunteering). Hence, addressing occupational status while considering these aspects could provide a more detailed profile of occupation functioning in this population.
Many factors in addition to cognitive deficits could also disrupt occupational outcome (Campbell et al., 2010; Catty et al., 2008; Corbière et al., 2017; Corbière et al., 2011; Kausto et al., 2017). For instance, many of these factors, notably self-esteem, could influence level of performance in various skills (e.g., social behaviour, personal presentation) essential in job acquisition or return to school (Zanon and Merceron, 2017). In addition, in a recent study on people with a severe mental illness, Corbière et al. (2017) identified that length of time absent from employment, self-esteem, severity of symptoms, motivation, job search behaviours and cognition independently predicted job acquisition. Since this study included a single cognitive test (Corbière et al., 2017), it is still not clear which specific cognitive deficits could have an independent predictive value to explain occupational outcome in recent-onset psychosis.
To address the limitations highlighted above, the current study will examine the role of cognitive functioning (i.e., speed of processing, attention/vigilance, working memory, verbal memory, visual memory, reasoning and problem solving, social cognition, global cognition and subjective cognitive complaints) in predicting level of occupational functioning, combining work or school and taking into account that these outcomes are ordinal, in an early psychosis population. Hence, measures other than cognition - motivation, job search behaviours, duration of the absence from work/school, psychotic symptoms and self-esteem were included as covariates in multivariate analyses to identify the predictive power unique to cognitive variables. These variables were selected because they had been previously associated with occupational outcome. We hypothesise that cognition, such as working memory, attention, verbal memory or speed of processing (Nuechterlein et al., 2011), will have an independent predictive weight on occupational outcome in the final model.
2. Materials and methods
2.1. Participants
Participants were recruited in Quebec City (Canada) from two clinics: an early-intervention program for first-episode psychosis and a clinic that offers follow-up for patients who require intensive treatment after the early-intervention program. The clinical team referred patients to the research team if they mentioned a goal of returning to school or acquiring a job. All participants met the following inclusion criteria: (1) aged between 18 and 39 years; (2) a diagnosis of a psychotic disorder; (3) less than five years of treatment for their psychotic disorder; (4) a stable clinical status that permitted neuropsychological assessment, as confirmed by scores of 1, 2, 5 or 6 on the Clinical Global Impressions-Clinical Benefits (CGI-CB); (5) no current full-time occupation (part-time work of 24 h per week or less was permitted) and (6) had verbally reported their willingness to improve their current occupational status. Exclusion criteria were: (1) a history of moderate or severe traumatic brain injury or brain surgery; (2) a neurological disorder known to cause neuropsychological impairments and (3) a confirmed IQ below 70 according to the participant's medical file. This study was approved by the ethics committee of the CERVO Brain Research Centre in the Centre intégré universitaire de santé et de services sociaux de la Capitale-Nationale (CIUSSS-CN), Quebec City, Canada (project #2016-128/399-2015), and all participants signed a written consent. Participants received $30 for the baseline evaluation and $10 at follow-up.
2.2. Measures
2.2.1. Neuropsychological assessment
The MATRICS Consensus Cognitive Battery (MCCB) was used to provide a cognitive profile of all participants (Nuechterlein et al., 2008). This neuropsychological battery consists of 10 tests categorised into seven cognitive domains, including (1) attention/vigilance; (2) speed of processing; (3) working memory; (4) verbal learning and memory; (5) visual learning and memory; (6) reasoning and problem solving and (7) social cognition. The MCCB also provides a global cognitive index. An additional aspect of social cognition, theory of mind (ToM), was also assessed using the Combined Stories Task (COST) (Achim et al., 2012). The COST requires participants to read short stories aloud and to answer one or two related ToM questions (in addition to control questions). Responding to the ToM questions requires taking into account the characters' mental states (i.e., their intentions, beliefs, or emotions). Answers are rated 0, 1, or 2 points for a total of 52 points. The task has excellent psychometric properties. More details on this task can be found in Achim et al. (2012) and Thibaudeau et al. (2018).
2.2.2. Subjective cognitive complaints
The Subjective Scale to Investigate Cognition in Schizophrenia (SSTICS) was used as a self-report measure of cognitive complaints (Stip et al., 2003). This questionnaire contains 21 items in which participants are asked to estimate the frequency (0 = never, 1 = rarely, 2 = sometimes, 3 = often, 4 = very often) of cognitive difficulties they encounter in their daily life. A global score is computed between 0 and 84, with higher scores representing greater subjective cognitive complaints.
2.2.3. Clinical assessment
Psychotic symptoms were assessed using the Positive and Negative Symptoms Scale (PANSS) (Kay et al., 1989). The PANSS provides a global score, and sub-scores for negatives, positives and general symptoms are also typically considered. However, given that a five factors structure has been shown to better represent patients' symptoms (Lehoux et al., 2009), the current study used the five factors structure of the PANSS. The following sub-scores were thus assessed: (1) positive; (2) negative; (3) cognitive/disorganization; (4) depression/anxiety and (5) excitability/hostility.
General social and occupational functioning was rated with the Social and Occupational Functioning Assessment Scale (SOFAS) (Goldman et al., 1992). The SOFAS provides a global score ranging from 0 to 100, with higher scores indicating better functioning.
2.2.4. Psychological assessment
Self-esteem was assessed using the Self-Esteem Rating Scale-Short Form (SERS-SF). This scale consists of 20 items measured on a Likert scale ranging from 1 (never) to 7 (always) (Lecomte et al., 2006). The SERS is divided into two dimensions, positive self-esteem (e.g. “When I am with other people, I feel that they are glad I am with them.”) and negative self-esteem (e.g. “I wish that I were someone else.”). Each dimension includes 10 items, and a score is computed for each dimension (11 to 70; −70 to −11; respectively), with higher scores representing higher self-esteem.
Motivation to go back to work or to school was provided by the Motivation to Find a Job scale (MTFJ) (Villotti et al., 2015). This scale includes seven items that participants are asked to rate on a Likert scale ranging from 1 (Completely disagree) to 7 (Completely agree). A higher global score indicates a higher motivation to obtain a job. Even though this questionnaire was originally developed to measure motivation to obtain a job, for the present study it was adapted to reflect participants' motivation to go back to school (when return to school was their goal). For example, the item “Right now, getting a job is one of my main objectives” was replaced by “Right now, going back to school is one of my main objectives.”
2.2.5. Occupational assessment
Current occupational status of participants was collected to provide information on current work and school status at baseline and at six months. Participants were asked to describe their occupations (work and school) for the last six months. Current occupational status and occupational status at six months was then transformed into one of the following ordinal variables: (1) no occupation; (2) social economy occupation (e.g. volunteer work or non-degree studies); (3) part-time occupation; (4) full-time occupation. Definitions of occupational categories are presented in Table 1. School and work participation were combined in one score. Prior occupational history was also collected with this questionnaire to obtain the length of time that participants had been absent from employment or school prior to the assessment.
Table 1.
Definition of each category of the dependant variable Occupational status.
| Occupational status | Work description | School description |
|---|---|---|
| 1: No occupation |
|
|
| 2: Social economy occupation |
|
|
| 3: Part-time occupation |
|
|
| 4: Full-time occupation |
|
|
The Job Search Behaviours questionnaire includes 14 items rated on a dichotomous scale (yes/no) (Corbière et al., 2011). Participants responded whether they had done each job search behaviour activity included in the questionnaire during the last six months. A score from 0 to 14 was calculated (1 point for each behaviour completed). When a participant's goal was to return to school, an adapted questionnaire (created by authors of the present study) was used instead of the original questionnaire to reflect behaviours related to return to school. For example, in the adapted assessment, the item “Consult a job placement organization” became “Consult an organization supporting return to school”.
2.3. Procedure
Inclusion and exclusion criteria, as well as the scoring of the CGI-CB, were assessed during an appointment with the participants' psychiatrist. Informed consent was then obtained by a member of the research team. At baseline, participants were invited to take part in a two-step evaluation. The first step included the neuropsychological assessment (MCCB, COST and SSTICS), the psychological assessment (MTFJ and SERS) and the occupational assessment (questionnaire). The second step was administered by the psychiatrist to rate the SOFAS and the PANSS. Participants were contacted again six months after baseline for a brief phone interview to collect occupational data.
2.4. Statistical analyses
All analyses were performed using SPSS Statistics version 25 software, with the exception of the ordinal regression that was performed using SAS 9.04.01 M6 software. The significance level was set at 0.05. First, correlations were computed between all potential determinants to evaluate multicollinearity (Criterion of r = 0.90). Potential predictors included: in the cognitive domain, T scores for attention/vigilance, speed of processing, working memory, verbal memory, visual memory, reasoning and problem solving, managing emotions, global cognitive index, and raw score on the COST and on the SSTICS; variables in the clinical domain include scores on motivation to return to work or to school, job search behaviours, duration of absence from workplace/school, the five symptom dimensions of the PANSS (positive, negative, cognitive/disorganization, depression/anxiety, excitability/hostility, as well as the PANSS total score), and positive, negative and total SERS. No potential determinant was excluded based on this analysis. Second, to predict occupational status six months later (i.e., dependent variable), a stepwise ordinal regression was performed using a cumulative logit model with all potential determinants. The factors in the final model were included using the stepwise approach, computed manually. At the first step, we perform ordinal regression models between the occupation status six months later and each of the p = 22 explanatory determinants. The most significant determinant (D1), according to the effect size (i.e., Nagelkerke R2), was then forced into the model. At the second step, we then fit other models with the previous identified determinant (D1) and one of the remaining p = 21 explanatory determinants. Again, the most significant determinant (D2) was then included into the model (D1 + D2). Before going to the next step, we look if the variable identified in the previous step (D2) accounted for a significant proportion of the final model, and if not, it was excluded from the model. We repeated the steps again and again until no more variables can be entered in the model, or until we have 3 variables in the model. We included this large amount of potential determinants to ensure that, if a cognitive variable was included in the final model, we would have a comprehensive perspective of occupational outcome that also takes into account potential determinants other than cognition. Finally, to explore the role of other cognitive domains in occupational outcome, Spearman correlations were performed between all cognitive domains and occupational status six months later.
3. Results
3.1. Participant characteristics
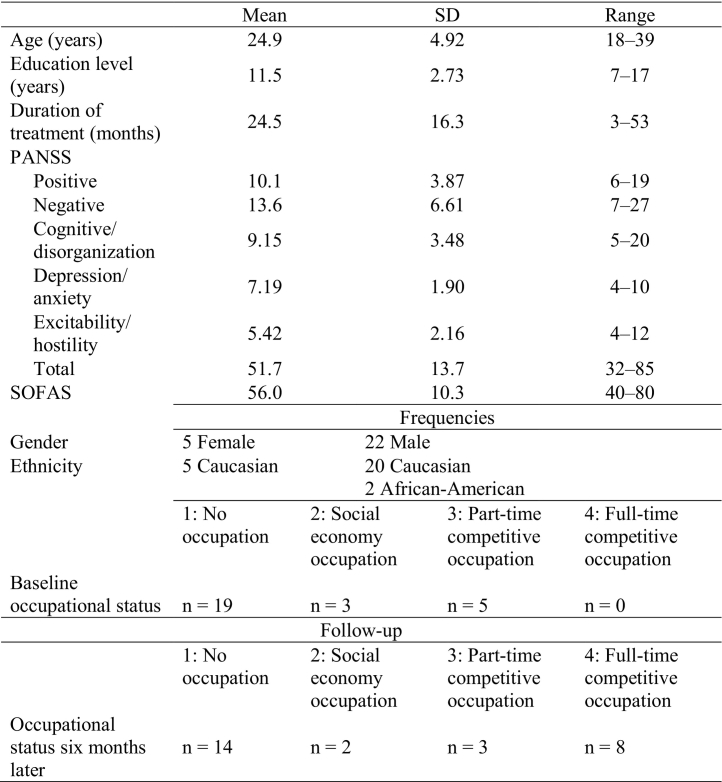
A total of 27 individuals fitting the inclusion criteria were recruited and accepted to take part in the study both at baseline and at the six-month follow-up phase. Table 2 summarizes the individual characteristics of the study sample at baseline. At follow up, 14 participants did not have an occupation (51.9%), two had a social economy occupation (7.4%), three had a part-time competitive occupation (11.1%) and eight had a full-time competitive occupation (29.6%). At follow-up, among the 27 participants, nine were found to have improved their occupational status (33.3%).
Table 2.
Characteristics of participants at baseline and occupational status six months later.
Note: all variables in Table 2 were evaluated at baseline to describe the sample, except for “occupational status six months later” which describe the sample at follow-up. Abbreviations: PANSS, Positive and Negative Syndrome Scale; SOFAS, Social and Occupational Functioning Assessment Scale.
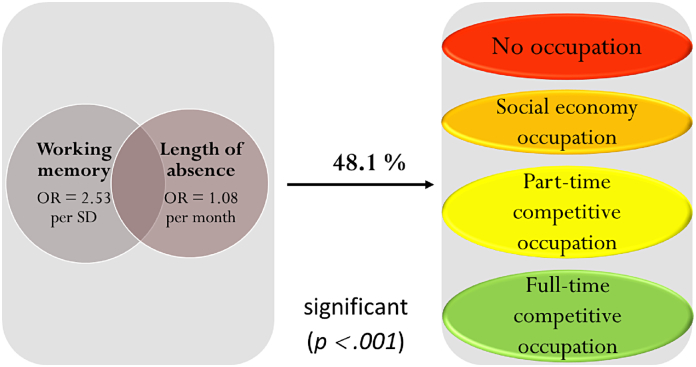
3.2. Determinants of occupational status at six months
As the primary analysis, a stepwise ordinal regression with a cumulative logit model was computed to predict participants' occupational status at six months, while considering all the potential determinants in our study. The correlation matrix between all potential determinants is presented in Table S1 in supplementary material. The final model showed that working memory and length of time absent from employment/school significantly predicted 48.1% (Nagelkerke R2 = 0.481) of the variance of occupational status at six months (χ2 (2, N = 27) = 15.269, p < .001). Both working memory (Wald χ2 (1) = 4.258, p = .039) and length of time absent from employment/school (Wald χ2 (1) = 4.791, p = .029), contributed significantly to the final model. Results showed that the chances of having an improved occupational status at six months were increased by 2.53 (95% CI, 1.05 to 6.17) times for each increment of one SD of improvement in working memory but were decreased by 1.08 (95% CI, 1.01 to 1.15) times for each month of absence from employment/school. Fig. 1 summarizes the results.
Fig. 1.
Illustration of the final model predicting 48.1% of occupational status with working memory and length of time absent from employment/school.
OR represents the chances of improving occupational status for each increment of one SD on working memory and for each decrease of one month on length of time absent from employment/school; OR: odd ratio; SD: standard deviation.
3.3. Exploring the role of other cognitive domains
In order to account for the strengths of association between all potential cognitive determinants and occupational status, Spearman correlations were computed between cognitive variables and occupational status at six months. Results are reported in Table 3. The positive relationships between attention/vigilance (r = 0.36, p = .034), speed of processing (r = 0.39, p = .022), global cognition (r = 0.32, p = .05) and occupational status at six months were similar to the relationship found between working memory and occupational status at six months (r = 0.38, p = .024).
Table 3.
Mean cognitive performances at baseline and Spearman correlations between cognitive domains and occupational status at six months (N = 27).
| Cognitive domain | Mean (T score) |
SD | Correlation |
|---|---|---|---|
| Speed of processing | 35.15 | 12.32 | .39a |
| Attention/vigilance | 36.70 | 10.4 | .36a |
| Working memory | 36.63 | 11.02 | .38a |
| Verbal memory | 37.30 | 7.26 | 0.20 |
| Visual memory | 40.19 | 11.46 | 0.14 |
| Reasoning and problem solving | 42.41 | 10.32 | 0.16 |
| Managing emotions | 41.70 | 8.9 | 0.13 |
| Global cognition | 31.44 | 12.1 | .32a |
| Theory of mind | 38.81 | 7.08 | 0.10 |
p ≤ .05.
4. Discussion
The aim of this longitudinal study was to evaluate the role of cognition in predicting occupational outcome in a recent-onset psychosis population. Specifically, the study evaluated this relationship while taking into account other outcomes relevant to job acquisition or return to school. Results showed that working memory and length of time absent from employment/school were significant determinants of occupational status at six months after baseline. The ordinal regression model including those two determinants significantly explained 48.1% of the variance of occupational status. Both determinants showed a significant individual contribution to the model, confirming our hypothesis that cognition is an important factor in occupational outcome in people with recent-onset psychosis.
The current study showed that the longer participants had been absent from a competitive occupation, the lower their occupational status was at six months. This finding is in line with previous literature reporting that the length of time absent from employment is one of the strongest and most consistent determinants of occupational outcome (Campbell et al., 2010; Catty et al., 2008; Corbière et al., 2011; Corbière et al., 2017; Kausto et al., 2017). Corbière et al., 2011, Corbière et al., 2017 found that, among participants with mental illness, the longer they had been absent from work, the more barriers to job acquisition that they perceived. Longer absence from work was also associated with lower reported self-esteem and perception of self-efficacy in this population. In our study, the length of time absent from employment/school was negatively related to motivation (r = −0.627, p < .001) (Table S1). This relationship may suggest that past work/school experiences could also reflect patients' motivation to return to work or to school.
The current study also showed that working memory plays a role in occupational status. Previous studies (Grau et al., 2016; Nuechterlein et al., 2011) have already reported its involvement in the occupational outcome of people with recent-onset psychosis. However, none of these previous studies added other clinical and psychosocial factors, such as the length of time absent from employment/school, self-esteem, motivation, job search strategies and severity of symptoms in their analyses; this is an important distinction given that the literature has shown that these are significant factors related to job acquisition or return to school (Corbière et al., 2011; Corbière et al., 2017). Hence, results of our study should encourage researchers to include working memory in future models accounting for occupational outcome in recent-onset psychosis. Indeed, working memory is a central cognitive function in various work- and school-related tasks because it involves retaining and manipulating information for short periods of time. This importantly forms the basis of many high-level processes like learning and implies other low-level processes, such as attention (Alloway and Alloway, 2010; Baddeley, 2000). Working memory is involved, for instance, when an individual receives multiple instructions from an employer or when an individual listens to a teacher's instructions while taking notes (Gathercole et al., 2006; Holmes et al., 2010).
Aside from working memory, other cognitive domains should also be examined when trying to understand the complex process that is occupational outcome. In our study, attention/vigilance (r = 0.356), speed of processing (r = 0.390) and global cognition (r = 0.316) showed a moderate association with occupational status at six months. This is consistent with the model proposed by Nuechterlein et al. (2011) which included mostly lower-level functions. However, other studies have shown on the contrary that higher-level functions (i.e. verbal and visual learning, social cognition, executive functioning) are more related to occupational functioning (Fett et al., 2011; Horan et al., 2012; Tsang et al., 2010; Ventura et al., 2015). These mixed results could be partially explained by the concept of individual deficits, which suggests that each cognitive deficit exhibited by an individual could potentially be a barrier to job acquisition or return to school. Indeed, a recent meta-analysis indicated that the key to enhance occupational outcome was to combine supported employment/education with interventions targeting each individual's deficits (Carmona et al., 2017). In addition, some authors suggested that higher-level functions, such as social cognition, were more relevant to predict occupation maintaining compared to occupation acquisition, as it is measured in the present study (Sauvé et al., 2019).
The observed contribution of length of time absent from employment/school and working memory in occupational status can have important clinical implications. For instance, studies suggest that Cognitive remediation therapy (CRT) combined with supportedemployment/education could improve cognition and enhance occupational outcome (Bell et al., 2005; Bell et al., 2008; Bell et al., 2014; Bowie et al., 2017; Kukla et al., 2018; Lystad et al., 2017; McGurk et al., 2005; McGurk et al., 2007; McGurk et al., 2009; Revell et al., 2015; Wykes et al., 2011). Additionally, Lystad et al. (2017) have shown that improvement in working memory was a significant determinant of number of hours worked after CRT and supported employment. Furthermore, length of time absent could be reduced by applying current guidelines of Individual Placement and Support (IPS) programs, which suggest that patients should quickly try to acquire a job or return to school (Becker and Drake, 2003). This could also enhance CRT efficacy since acquiring an occupation quickly during CRT could give participants more opportunities to practice the strategies learned during CRT (Bowie et al., 2017; Wykes and Huddy, 2009). Moreover, supported employment/education could include interventions targeting motivation (e.g., motivational interview), because of its interplay with the length of time absent from employment/school and its influence on occupational outcome (Choi et al., 2013; Saperstein et al., 2011). Furthermore, it has been reported that motivational interview could increase adherence to CRT in people with a psychotic disorder (Fiszdon et al., 2016), highlighting the relevance of combining interventions that target determinants of occupational outcome.
4.1. Limitations
Our study has some limitations that should be considered. First of all, the relatively small sample size of the current study and the high number of potential determinants prevented us from drawing firm conclusions on results of ordinal regressions. Being aware of this limitation, we included two determinants in the final model while performing our analyses, but we acknowledge that it may have prevented us to find significant effects (e.g., social cognition). Secondly, the MCCB presents another limitation, considering that it is not able to evaluate every component of executive functioning or social cognition. To address social cognition we added a test of theory of mind, since it has been frequently associated with social functioning, to help account for this limitation. However, further studies using the MCCB should also include other tests to evaluate independently each component of executive functioning (Miyake et al., 2000; Shallice and Burgess, 1996). Third, we acknowledge that due to our selection criterion requiring that the person has shown interest in going back at work or school, our results apply only to a population that has at least some motivation for doing so.
4.2. Conclusion
In conclusion, this study supports that the length of time absent from employment or school is a strong determinant of occupational status in recent-onset psychosis. Furthermore, it shows that cognitive deficits also play an important role in occupational status in this population and therefore represent barriers to acquiring a job or returning to school. Working memory was the cognitive domain that accounted for the most variance in predicting occupational status at the six-month follow-up, despite the inclusion of length of time absent from employment/school in the final model. Overall, the results suggest that participants should receive interventions that target pre-existing cognitive deficits and reduce the length of time absent from employment or school to enhance occupational outcome.
The following is the supplementary data related to this article.
Correlation matrix final.
Funding
This work was supported by the Chaire Richelieu de recherche sur la jeunesse, l'enfance et la famille, by a salary grant from Fonds de Recherche du Québec - Santé (FRQS) for AMA, a studentship from FRQS for ET and a studentship from Canadian Institutes of Health Research (CIHR) for WP.
Contributors
M. Pothier, Dr. Cellard and Dr. Roy designed the study and wrote the protocol. Dr. Corbière helped to design the study. M. Pothier managed the literature search and analyses. M. Pothier, Ms. Lavoie, Ms. Turcotte and Ms. Vallières were involved in the data collection. M. Pothier undertook statistical analyses. Ms. Villotti, Ms. Turcotte and Ms. Lavoie reviewed data and analyses. M. Pothier, Dr. Cellard, Dr. Corbière, Ms. Villotti, Dr. Achim and Dr. Roy were involved in the interpretation of the results. M. Pothier prepared the first draft, and all authors edited the first draft. Dr. Cellard and Dr. Roy supervised the research. All authors contributed to and have approved the final manuscript.
Declaration of Competing Interest
The authors declare that they have no conflict of interest.
Acknowledgments
The authors would like to thank all the members of the clinical team for their help with the recruitment. We also acknowledge the contribution of the patients who participated to this research.
References
- Achim A.M., Ouellet R., Roy M.A., Jackson P.L. Mentalizing in first-episode psychosis. Psychiatry Res. 2012;196(2–3):207–213. doi: 10.1016/j.psychres.2011.10.011. [DOI] [PubMed] [Google Scholar]
- Achim A.M., Ouellet R., Lavoie M.A., Vallieres C., Jackson P.L., Roy M.A. Impact of social anxiety on social cognition and functioning in patients with recent-onset schizophrenia spectrum disorders. Schizophr. Res. 2013;145(1–3):75–81. doi: 10.1016/j.schres.2013.01.012. [DOI] [PubMed] [Google Scholar]
- Allott K., Liu P., Proffitt T.M., Killackey E. Cognition at illness onset as a predictor of later functional outcome in early psychosis: systematic review and methodological critique. Schizophr. Res. 2011;125(2–3):221–235. doi: 10.1016/j.schres.2010.11.001. [DOI] [PubMed] [Google Scholar]
- Alloway T.P., Alloway R.G. Investigating the predictive roles of working memory and IQ in academic attainment. J. Exp. Child Psychol. 2010;106(1):20–29. doi: 10.1016/j.jecp.2009.11.003. [DOI] [PubMed] [Google Scholar]
- Alvarez-Jimenez M., Gleeson J.F., Henry L.P., Harrigan S.M., Harris M.G., Killackey E., Bendall S., Amminger G.P., Yung A.R., Herrman H., Jackson H.J., McGorry P.D. Road to full recovery: longitudinal relationship between symptomatic remission and psychosocial recovery in first-episode psychosis over 7.5 years. Psychol. Med. 2012;42(3):595–606. doi: 10.1017/S0033291711001504. [DOI] [PubMed] [Google Scholar]
- Baddeley A.D. The episodic buffer: a new component of working memory? Trends Cogn. Sci. 2000;4(11):417–423. doi: 10.1016/s1364-6613(00)01538-2. [DOI] [PubMed] [Google Scholar]
- Becker D.R., Drake R.E. Oxford University Press; 2003. A Working Life for People with Severe Mental Illness. [Google Scholar]
- Bell M.D., Bryson G.J., Greig T.C., Fiszdon J.M., Wexler B.E. Neurocognitive enhancement therapy with work therapy: productivity outcomes at 6- and 12-month follow-ups. J. Rehabil. Res. Dev. 2005;42(6):829–838. doi: 10.1682/jrrd.2005.03.0061. [DOI] [PubMed] [Google Scholar]
- Bell M.D., Zito W., Greig T., Wexler B.E. Neurocognitive enhancement therapy with vocational services: work outcomes at two-year follow-up. Schizophr. Res. 2008;105(1–3):18–29. doi: 10.1016/j.schres.2008.06.026. [DOI] [PubMed] [Google Scholar]
- Bell M.D., Choi K.H., Dyer C., Wexler B.E. Benefits of cognitive remediation and supported employment for schizophrenia patients with poor community functioning. Psychiatr Serv. (Washington, D.C.) 2014;65(4):469–475. doi: 10.1176/appi.ps.201200505. [DOI] [PubMed] [Google Scholar]
- Birchwood M., Todd P., Jackson C. Early intervention in psychosis: the critical period hypothesis. Br. J. Psychiatry. 1998;172(S33):53–59. [PubMed] [Google Scholar]
- Bowie C.R., Grossman M., Gupta M., Holshausen K., Best M.W. Action-based cognitive remediation for individuals with serious mental illnesses: effects of real-world simulations and goal setting on functional and vocational outcomes. Psychiatr Rehabil J. 2017;40(1):53–60. doi: 10.1037/prj0000189. [DOI] [PubMed] [Google Scholar]
- Bratlien U., Oie M., Lien L., Agartz I., Lie Romm K., Vaskinn A., Ueland T., Andreassen O.A., Melle I. Social dysfunction in first-episode psychosis and relations to neurocognition, duration of untreated psychosis and clinical symptoms. Psychiatry Res. 2013;207(1–2):33–39. doi: 10.1016/j.psychres.2012.10.010. [DOI] [PubMed] [Google Scholar]
- Brown J.A. Talking about life after early psychosis: the impact on occupational performance. Can. J. Occup. Ther. 2011;78(3):156–163. doi: 10.2182/cjot.2011.78.3.3. [DOI] [PubMed] [Google Scholar]
- Campbell K., Bond G.R., Drake R.E., McHugo G.J., Xie H. Client predictors of employment outcomes in high-fidelity supported employment: a regression analysis. The J Nerv Ment Dis. 2010;198(8):556–563. doi: 10.1097/NMD.0b013e3181ea1e53. [DOI] [PubMed] [Google Scholar]
- Carmona V.R., Gomez-Benito J., Huedo-Medina T.B., Rojo J.E. Employment outcomes for people with schizophrenia spectrum disorder: a meta-analysis of randomized controlled trials. Int. J. Occup. Med. Environ. Health. 2017;30(3):345–366. doi: 10.13075/ijomeh.1896.01074. [DOI] [PubMed] [Google Scholar]
- Catty J., Lissouba P., White S., Becker T., Drake R.E., Fioritti A., Knapp M., Lauber C., Rossler W., Tomov T., van Busschbach J., Wiersma D., Burns T. Predictors of employment for people with severe mental illness: results of an international six-Centre randomised controlled trial. Br. J. Psychiatry. 2008;192(3):224–231. doi: 10.1192/bjp.bp.107.041475. [DOI] [PubMed] [Google Scholar]
- Choi K.H., Fiszdon J.M., Bell M.D. Beyond cognition: a longitudinal investigation of the role of motivation during a vocational rehabilitation program. J. Nerv. Ment. Dis. 2013;201(3):173–178. doi: 10.1097/NMD.0b013e3182848bd4. [DOI] [PubMed] [Google Scholar]
- Corbière M., Zaniboni S., Lecomte T., Bond G., Gilles P.Y., Lesage A., Goldner E. Job acquisition for people with severe mental illness enrolled in supported employment programs: a theoretically grounded empirical study. J. Occup. Rehabil. 2011;21(3):342–354. doi: 10.1007/s10926-011-9315-3. [DOI] [PubMed] [Google Scholar]
- Corbière M., Lecomte T., Reinharz D., Kirsh B., Goering P., Menear M., Berbiche D., Genest K., Goldner E.M. Predictors of Acquisition of Competitive Employment for people enrolled in supported employment programs. J. Nerv. Ment. Dis. 2017;205(4):275–282. doi: 10.1097/NMD.0000000000000612. [DOI] [PubMed] [Google Scholar]
- Doroud N., Fossey E., Fortune T. Recovery as an occupational journey: a scoping review exploring the links between occupational engagement and recovery for people with enduring mental health issues. Aust. Occup. Ther. J. 2015;62(6):378–392. doi: 10.1111/1440-1630.12238. [DOI] [PubMed] [Google Scholar]
- Fett A.K., Viechtbauer W., Dominguez M.D., Penn D.L., van Os J., Krabbendam L. The relationship between neurocognition and social cognition with functional outcomes in schizophrenia: a meta-analysis. Neurosci. Biobehav. Rev. 2011;35(3):573–588. doi: 10.1016/j.neubiorev.2010.07.001. [DOI] [PubMed] [Google Scholar]
- Fiszdon J.M., Kurtz M.M., Choi J., Bell M.D., Martino S. Motivational interviewing to increase cognitive rehabilitation adherence in schizophrenia. Schizophr. Bull. 2016;42(2):327–334. doi: 10.1093/schbul/sbv143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gathercole S.E., Lamont E., Alloway T.P. Working Memory and Education. 2006. Working memory in the classroom; pp. 219–240. [Google Scholar]
- Goldman H.H., Skodol A.E., Lave T.R. Revising axis V for DSM-IV: a review of measures of social functioning. American J Psychiatry. 1992;149(9):1148–1156. doi: 10.1176/ajp.149.9.1148. [DOI] [PubMed] [Google Scholar]
- Goulding S.M., Chien V.H., Compton M.T. Prevalence and correlates of school drop-out prior to initial treatment of nonaffective psychosis: further evidence suggesting a need for supported education. Schizophr. Res. 2010;116(2–3):228–233. doi: 10.1016/j.schres.2009.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grau N., Rubio-Abadal E., Usall J., Barajas A., Butjosa A., Dolz M., Banos I., Sanchez B., Rodriguez M.J., Pelaez T., Sammut S., Carlson J., Huerta-Ramos E., Ochoa S. Influence of cognition, premorbid adjustment and psychotic symptoms on psycho-social functioning in first-episode psychosis. Psychiatry Res. 2016;242:157–162. doi: 10.1016/j.psychres.2016.04.121. [DOI] [PubMed] [Google Scholar]
- Holmes J., Gathercole S.E., Dunning D.L. Poor working memory: impact and interventions. Adv. Child Dev. Behav. 2010;39:1–43. doi: 10.1016/b978-0-12-374748-8.00001-9. [DOI] [PubMed] [Google Scholar]
- Horan W.P., Green M.F., DeGroot M., Fiske A., Hellemann G., Kee K., Kern R.S., Lee J., Sergi M.J., Subotnik K.L., Sugar C.A., Ventura J., Nuechterlein K.H. Social cognition in schizophrenia, part 2: 12-month stability and prediction of functional outcome in first-episode patients. Schizophr. Bull. 2012;38(4):865–872. doi: 10.1093/schbul/sbr001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kausto J., Pentti J., Oksanen T., Virta L.J., Virtanen M., Kivimaki M., Vahtera J. Length of sickness absence and sustained return-to-work in mental disorders and musculoskeletal diseases: a cohort study of public sector employees. Scand J Environ Health. 2017;43(4):358–366. doi: 10.5271/sjweh.3643. [DOI] [PubMed] [Google Scholar]
- Kay S.R., Opler L.A., Lindenmayer J.P. The positive and negative syndrome scale (PANSS): rationale and standardisation. Br J Psychiatry Suppl. 1989;(7):59–67. [PubMed] [Google Scholar]
- Kukla M., Bell M.D., Lysaker P.H. A randomized controlled trial examining a cognitive behavioral therapy intervention enhanced with cognitive remediation to improve work and neurocognition outcomes among persons with schizophrenia spectrum disorders. Schizophr. Res. 2018 doi: 10.1016/j.schres.2018.01.012. [DOI] [PubMed] [Google Scholar]
- Lecomte T., Corbière M., Laisne F. Investigating self-esteem in individuals with schizophrenia: relevance of the self-esteem rating scale-short form. Psychiatry Res. 2006;143(1):99–108. doi: 10.1016/j.psychres.2005.08.019. [DOI] [PubMed] [Google Scholar]
- Lehoux C., Gobeil M., Lefèbvre A., Maziade M., Roy M.A. The five-factor structure of the PANSS: a critical review of its consistency across studies. Clinical schizophrenia & related psychoses. 2009;3(2):103–110. [Google Scholar]
- Lystad J.U., Falkum E., Haaland V.O., Bull H., Evensen S., McGurk S.R., Ueland T. Cognitive remediation and occupational outcome in schizophrenia spectrum disorders: a 2year follow-up study. Schizophr. Res. 2017;185:122–129. doi: 10.1016/j.schres.2016.12.020. [DOI] [PubMed] [Google Scholar]
- Marwaha S., Johnson S. Schizophrenia and employment - a review. Soc. Psychiatry Psychiatr. Epidemiol. 2004;39(5):337–349. doi: 10.1007/s00127-004-0762-4. [DOI] [PubMed] [Google Scholar]
- McGurk S.R., Mueser K.T., Pascaris A. Cognitive training and supported employment for persons with severe mental illness: one-year results from a randomized controlled trial. Schizophr. Bull. 2005;31(4):898–909. doi: 10.1093/schbul/sbi037. [DOI] [PubMed] [Google Scholar]
- McGurk S.R., Mueser K.T., Feldman K., Wolfe R., Pascaris A. Cognitive training for supported employment: 2-3 year outcomes of a randomized controlled trial. Am. J. Psychiatry. 2007;164(3):437–441. doi: 10.1176/ajp.2007.164.3.437. [DOI] [PubMed] [Google Scholar]
- McGurk S.R., Mueser K.T., DeRosa T.J., Wolfe R. Work, recovery, and comorbidity in schizophrenia: a randomized controlled trial of cognitive remediation. Schizophr. Bull. 2009;35(2):319–335. doi: 10.1093/schbul/sbn182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milev P., Ho B.C., Arndt S., Andreasen N.C. Predictive values of neurocognition and negative symptoms on functional outcome in schizophrenia: a longitudinal first-episode study with 7-year follow-up. Am. J. Psychiatry. 2005;162(3):495–506. doi: 10.1176/appi.ajp.162.3.495. [DOI] [PubMed] [Google Scholar]
- Miyake A., Friedman N.P., Emerson M.J., Witzki A.H., Howerter A., Wager T.D. The unity and diversity of executive functions and their contributions to complex “Frontal Lobe” tasks: a latent variable analysis. Cogn. Psychol. 2000;41(1):49–100. doi: 10.1006/cogp.1999.0734. [DOI] [PubMed] [Google Scholar]
- Morgan V.A., Waterreus A., Jablensky A., Mackinnon A., McGrath J.J., Carr V., Bush R., Castle D., Cohen M., Harvey C., Galletly C., Stain H.J., Neil A.L., McGorry P., Hocking B., Shah S., Saw S. People living with psychotic illness in 2010: the second Australian national survey of psychosis. Aust N Z J Psychiatry. 2012;46(8):735–752. doi: 10.1177/0004867412449877. [DOI] [PubMed] [Google Scholar]
- Mueser K.T., Deavers F., Penn D.L., Cassisi J.E. Psychosocial treatments for schizophrenia. Annu. Rev. Clin. Psychol. 2013;9:465–497. doi: 10.1146/annurev-clinpsy-050212-185620. [DOI] [PubMed] [Google Scholar]
- Neil A.L., Carr V.J., Mihalopoulos C., Mackinnon A., Morgan V.A. Costs of psychosis in 2010: findings from the second Australian National Survey of psychosis. Aust N Z J Psychiatry. 2014;48(2):169–182. doi: 10.1177/0004867413500352. [DOI] [PubMed] [Google Scholar]
- Nuechterlein K.H., Green M.F., Kern R.S., Baade L.E., Barch D.M., Cohen J.D., Essock S., Fenton W.S., Frese F.J., 3rd, Gold J.M., Goldberg T., Heaton R.K., Keefe R.S., Kraemer H., Mesholam-Gately R., Seidman L.J., Stover E., Weinberger D.R., Young A.S., Zalcman S., Marder S.R. The MATRICS consensus cognitive battery, part 1: test selection, reliability, and validity. American J Psychiatry. 2008;165(2):203–213. doi: 10.1176/appi.ajp.2007.07010042. [DOI] [PubMed] [Google Scholar]
- Nuechterlein K.H., Subotnik K.L., Green M.F., Ventura J., Asarnow R.F., Gitlin M.J., Yee C.M., Gretchen-Doorly D., Mintz J. Neurocognitive predictors of work outcome in recent-onset schizophrenia. Schizophr. Bull. 2011;37(Suppl. 2):S33–S40. doi: 10.1093/schbul/sbr084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinkham A.E. Social cognition in schizophrenia. J Clin Psychiatry. 2014;75(Suppl. 2):14–19. doi: 10.4088/JCP.13065su1.04. [DOI] [PubMed] [Google Scholar]
- Revell E.R., Neill J.C., Harte M., Khan Z., Drake R.J. A systematic review and meta-analysis of cognitive remediation in early schizophrenia. Schizophr. Res. 2015;168(1–2):213–222. doi: 10.1016/j.schres.2015.08.017. [DOI] [PubMed] [Google Scholar]
- Rinaldi M., Killackey E., Smith J., Shepherd G., Singh S.P., Craig T. First episode psychosis and employment: a review. Int Rev Psychiatry. 2010;22(2):148–162. doi: 10.3109/09540261003661825. [DOI] [PubMed] [Google Scholar]
- Roe D., Rudnick A., Gill K.J. The concept of “being in recovery”. Psychiatr Rehabil J. 2007;30(3):171–173. doi: 10.2975/30.3.2007.171.173. [DOI] [PubMed] [Google Scholar]
- Rosenheck R., Leslie D., Keefe R., McEvoy J., Swartz M., Perkins D., Stroup S., Hsiao J.K., Lieberman J. Barriers to employment for people with schizophrenia. Am. J. Psychiatry. 2006;163(3):411–417. doi: 10.1176/appi.ajp.163.3.411. [DOI] [PubMed] [Google Scholar]
- Saperstein A.M., Fiszdon J.M., Bell M.D. Intrinsic motivation as a predictor of work outcome after vocational rehabilitation in schizophrenia. J. Nerv. Ment. Dis. 2011;199(9):672–677. doi: 10.1097/NMD.0b013e318229d0eb. [DOI] [PubMed] [Google Scholar]
- Sauvé G., Lepage M., Corbière M. Impacts de la combinaison de programmes de soutien à l’emploi et de remédiation cognitive sur le maintien en emploi de personnes souffrant de schizophrénie: une méta-analyse. Annales Médico-psychologiques, revue psychiatrique. 2019;177(6):534–543. [Google Scholar]
- Shallice T., Burgess P. The domain of supervisory processes and temporal organization of behaviour. Philos. Trans. R. Soc. Lond. Ser. B Biol. Sci. 1996;351(1346):1405–1411. doi: 10.1098/rstb.1996.0124. discussion 1411-1402. [DOI] [PubMed] [Google Scholar]
- Stip E., Caron J., Renaud S., Pampoulova T., Lecomte Y. Exploring cognitive complaints in schizophrenia: the subjective scale to investigate cognition in schizophrenia. Compr. Psychiatry. 2003;44(4):331–340. doi: 10.1016/S0010-440X(03)00086-5. [DOI] [PubMed] [Google Scholar]
- Stouten L.H., Veling W., Laan W., van der Helm M., van der Gaag M. Psychosocial functioning in first-episode psychosis and associations with neurocognition, social cognition, psychotic and affective symptoms. Early Interv Psychiatry. 2017;11(1):23–36. doi: 10.1111/eip.12210. [DOI] [PubMed] [Google Scholar]
- Tandberg M., Ueland T., Sundet K., Haahr U., Joa I., Johannessen J.O., Larsen T.K., Opjordsmoen S., Rund B.R., Rossberg J.I., Simonsen E., Vaglum P., Melle I., Friis S., McGlashan T. Neurocognition and occupational functioning in patients with first-episode psychosis: a 2-year follow-up study. Psychiatry Res. 2011;188(3):334–342. doi: 10.1016/j.psychres.2011.04.021. [DOI] [PubMed] [Google Scholar]
- Thibaudeau E., Cellard C., Legendre M., Villeneuve K., Achim A.M. Reliability of two social cognition tests: the combined stories test and the social knowledge test. Psychiatry Res. 2018;262:63–69. doi: 10.1016/j.psychres.2018.01.026. [DOI] [PubMed] [Google Scholar]
- Tsang H.W., Leung A.Y., Chung R.C., Bell M., Cheung W.M. Review on vocational predictors: a systematic review of predictors of vocational outcomes among individuals with schizophrenia: an update since 1998. Aust N Z J Psychiatry. 2010;44(6):495–504. doi: 10.3109/00048671003785716. [DOI] [PubMed] [Google Scholar]
- Ventura J., Ered A., Gretchen-Doorly D., Subotnik K.L., Horan W.P., Hellemann G.S., Nuechterlein K.H. Theory of mind in the early course of schizophrenia: stability, symptom and neurocognitive correlates, and relationship with functioning. Psychol. Med. 2015;45(10):2031–2043. doi: 10.1017/S0033291714003171. [DOI] [PubMed] [Google Scholar]
- Villotti P., Corbière M., Zaniboni S., Lecomte T., Fraccaroli F. Evaluating the motivation to obtain and sustain employment in people with psychiatric disabilities. Psicologia sociale. 2015;10(1):57–70. [Google Scholar]
- Wykes T., Huddy V. Cognitive remediation for schizophrenia: it is even more complicated. Curr Opin Psychiatry. 2009;22(2):161–167. doi: 10.1097/YCO.0b013e328322fbf4. [DOI] [PubMed] [Google Scholar]
- Wykes T., Huddy V., Cellard C., McGurk S.R., Czobor P. A meta-analysis of cognitive remediation for schizophrenia: methodology and effect sizes. Am. J. Psychiatry. 2011;168(5):472–485. doi: 10.1176/appi.ajp.2010.10060855. [DOI] [PubMed] [Google Scholar]
- Zanon D., Merceron K. Cognitive functioning and work outcome among people with schizophrenia spectrum disorder: the contribution of the international classification of functioning. Sante mentale au Quebec. 2017;42(2):71–85. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Correlation matrix final.