Abstract
Herlyn-Werner-Wunderlich (HWW) syndrome is a rare congenital disease characterized by Mullerian duct anomalies. The characteristic triad of this syndrome includes didelphys uterus, obstructed hemivagina, and ipsilateral renal agenesis (hence, also known as Obstructed Hemivagina and Ipsilateral Renal Agenesis or OHVIRA syndrome). The clinical presentation of HWW is nonspecific and patients may present with abdominal/pelvic pain, dyspareunia, or dysmenorrhea. However, the imaging findings of HWW are characteristic and discussed in this case report of a 16-year-old female who presented with abdominal pain and dyspareunia.
Keywords: Herlyn-Werner-Wunderlich syndrome, Obstructed Hemivagina and Ipsilateral Renal Agenesis syndrome, Dyspareunia, Magnetic Resonance Imaging
Clinical history
Sixteen-year-old sexually active female, with no relevant past medical or surgical history, presented with acute onset of worsening left lower abdominal pain of 3-4 days duration. She also reported dyspareunia, post coital bleeding, and occasional hematochezia.
She denied fever, chills, vomiting, nausea, abdominal distension, diarrhea, or constipation. There was no history of vaginal discharge, or burning micturition. She also denied recent weight loss, change in bowel habits, or irregular menses.
Physical examination revealed mild lower abdominal tenderness without rebound or guarding. No abdominal distension was noted. Bowel sounds were normal. Review of systems was otherwise negative.
Urine pregnancy test was negative. Complete blood counts were unremarkable and urine examination was negative for signs of infection.
Imaging findings
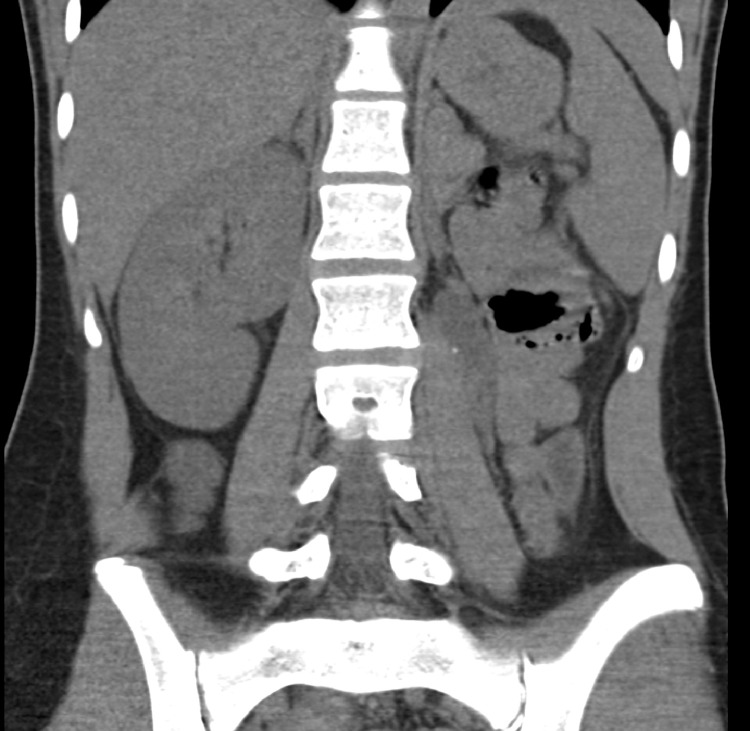
Recent previous CT scan from a different institution showed absence of left kidney, a low attenuation lesion (1.9 × 3.0 × 3.9 cm) with punctate calcification in the left renal fossa, and no colon or bowel pathology. Appendix was normal.
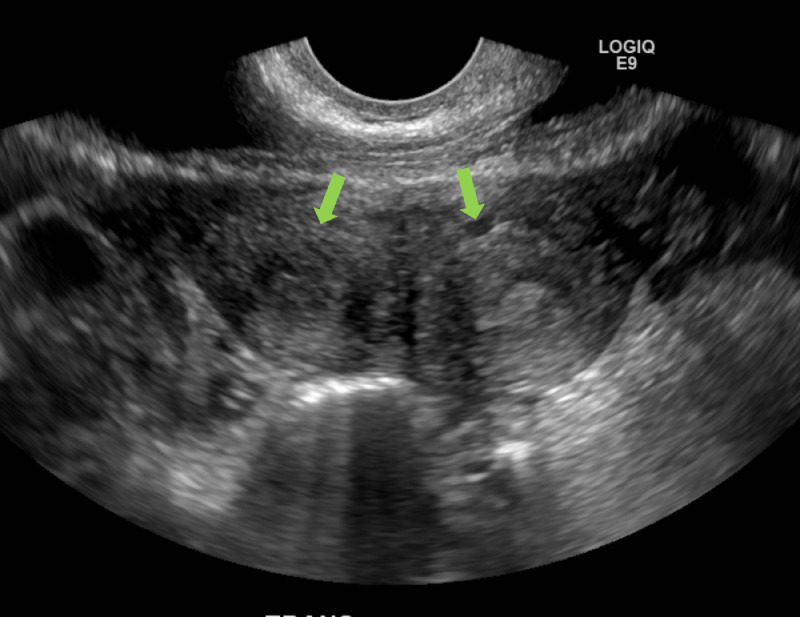
Pelvic ultrasound was obtained for further evaluation which showed normal ovaries bilaterally, a tubular structure in the left adnexal region with thickened walls and surrounding hypervascularity, and a duplicated uterine cavity. The absence of left kidney was noted.
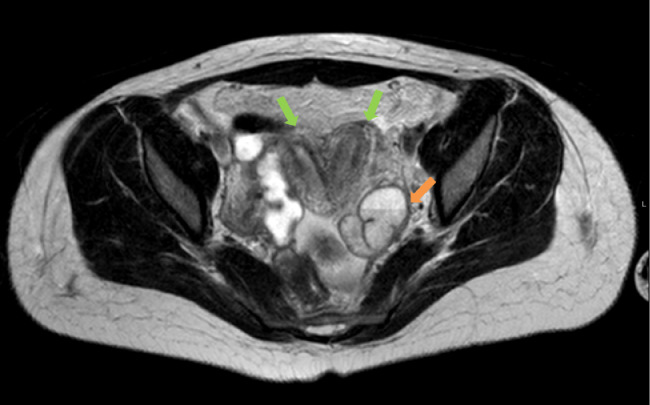
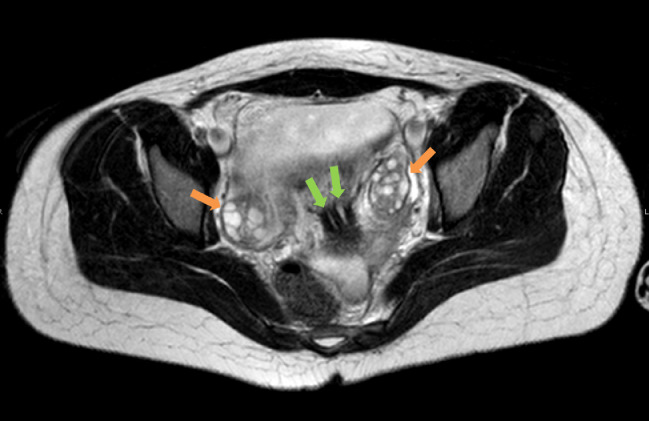
Subsequently, MRI of the abdomen and pelvis was obtained which demonstrated complete duplication of the uterine horns, endometrial cavities, and endocervical canal consistent with uterine didelphys. A cystic structure just distal to the left endocervical canal likely represented an obstructed left hemivagina. A collapsed right hemivagina was seen communicating with the right endocervical canal.
A tortuous, dilated left Fallopian tube was seen with fluid-fluid level, and with restricted diffusion within the dependent fluid. Enhancement of the left fallopian tubal wall was noted on postcontrast images. This was consistent with hematosalpinx or pyosalpinx. Bilateral ovaries were normal.
Based on the imaging findings, the patient was diagnosed with Obstructed Hemivagina and Ipsilateral Renal Agenesis (OHVIRA) Syndrome.
Discussion
Herlyn-Werner-Wunderlich (HWW) syndrome is a rare form of Mullerian Duct Anomalies (MDA) which have a reported prevalence of 2%-3% and incidence of 1 in 200 to 1 in 600 among fertile women. [1], [2]. The characteristic triad of this syndrome includes didelphys uterus, obstructed hemivagina, and ipsilateral renal agenesis (hence, also known as OHVIRA or OHVIRA syndrome). Uterine didelphys accounts for 11% of MDA while aplasia/hypoplasia of the uterus and proximal vagina make up approximately 5%-10% of MDA [1]. An estimated 45% of cases of uterine didelphys are associated with unilateral renal agenesis [1]. While the pathogenesis of MDA is related to maldevelopment (aplasia, hypoplasia, defective fusion, or failed resorption) of the paramesonephric ducts, the close proximity of the mesonephric ducts that give rise to the kidney and ureter is thought to result in anomalies of the genital tract that often accompany MDA [2].
The most widely accepted classification of MDA by the American Society for Reproductive Medicine groups these anomalies into those related to agenesis/hypoplasia of the vagina, cervix, fundus or fallopian tubes, or a combination of these (Class I), unicornuate uterus (Class II), uterine didelphys (Class III), bicornuate uterus (Class IV), septate uterus (Class V), arcuate uterus (Class VI), and anomalies related to diethylstilbestrol exposure (Class VII) [3]
Patients with HWW syndrome typically present after menarche with pelvic pain, dysmenorrhea, or palpable mass in the vagina or pelvis [1]. Although pelvic ultrasound is usually used to investigate pelvic pain/palpable mass initially, MRI of the pelvis is the most accurate modality to characterize and classify the genital tract anomalies and associated pelvic findings [1]. Laparoscopy remains the gold standard for diagnosis of female genital tract abnormalities but is only used when MRI is unavailable or fails to establish a diagnosis [4]
Characteristic findings on MRI include complete duplication of uterine and endocervical cavities (didelphys uterus). Typically, a cystic structure is seen distal to and communicating with one of the endocervical canals, representing obstructed hemivagina. The obstructed vagina usually contains blood or proteinaceous fluid that appears bright on T1-weighted images. A fluid-fluid level may be seen. Other findings including hematometrosis and or hematosalpinx may be seen as bright T1 intensity filling the cavities of the uterus or fallopian tubes. Associated endometriosis may be present.
Imaging of the abdomen will show ipsilateral renal agenesis on the same side as the obstructed hemivagina in HWW syndrome. While didelphys uterus accounts for approximately 11% of MDA, upto 30%-50% of patients with MDAs have concomitant renal anomalies [5].
Resection of the vaginal septum is the mainstay of treatment for HWW syndrome [6]. A study by Wang et al reported a 52.9% ipsilateral pregnancies following excision of the vaginal septum [7]. Although uterine didelphys has not shown to affect fertility, the rates of spontaneous abortions have been reported ranging from 23%-40% [1], [2]. Cesarean section may be required for successful delivery.
To summarize, HWW is a rare disorder of MDA characterized by didelphys uterus, OHVIRA. MRI is most accurate for providing details regarding the altered anatomy and for identifying associated hematocolpos, hematosalpinx, hematometros, Pelvic inflammatory disease (PID), or endometriosis. Additional imaging should be obtained to assess for renal anomalies that often accompany MDA (Fig. 1, Fig. 2, Fig. 3, Fig. 4, Fig. 5, Fig. 6, Fig. 7).
Fig. 1.
Coronal View of the CT abdomen and Pelvis shows absent left kidney.
Fig. 2.
Ultrasound examination of the pelvis shows duplicated uterine cavities (arrows).
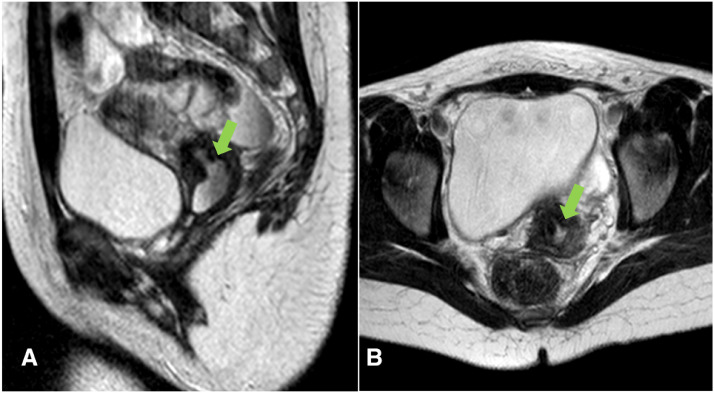
Fig. 3.
Axial T2-weighted image of the pelvis shows duplication of the uterine horns and endometrial cavities (green arrows) consistent with didelphys. A tortuous, dilated tubular structure was noted in the left adnexa with fluid-fluid levels consistent with hematosalpinx or pyosalpinx (orange arrow). This tubular structure showed enhancement on postcontrast images (not shown). (Color version of figure is available online.)
Fig. 4.
Axial T2-weighted image of the pelvis shows duplication of the cervical canals (green arrows). Normal ovaries are seen bilaterally (orange arrows). (Color version of figure is available online.)
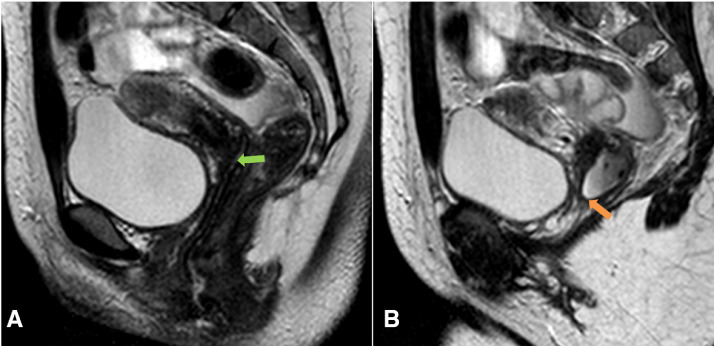
Fig. 5.
Sagittal (A) and axial (B) T2-weighted image of the pelvis show the left cervical canal connecting with a blind ended pouch/ structure, the obstructed hemivagina (green arrows). (Color version of figure is available online.)
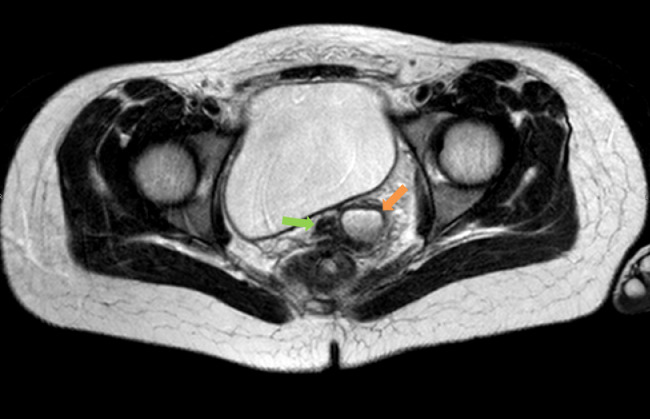
Fig. 6.
Axial T2-weighted image of the pelvis shows the right-sided patent hemivagina (green arrow) the left sided obstructed hemivagina (orange arrow). (Color version of figure is available online.)
Fig. 7.
Sagittal T2-weighted images of the pelvis show the right-sided patent hemivagina (green arrow) the left sided obstructed hemivagina (orange arrow). (Color version of figure is available online.)
Footnotes
Declaration of Competing Interest: The authors have no COIs to disclose.
References
- 1.Del Vescovo R., Battisti S., Di Paola V., Piccolo C.L., Cazzato R.L., Sansoni I. Herlyn-Werner-Wunderlich syndrome: MRI findings, radiological guide (two cases and literature review), and differential diagnosis. BMC Med Imaging. 2012;12:4. doi: 10.1186/1471-2342-12-4. http://www.ncbi.nlm.nih.gov/pubmed/22405336 [Accessed March 9, 2012] Available from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gholoum S., Puligandla P.S., Hui T., Su W., Quiros E., Laberge J.-M. Management and outcome of patients with combined vaginal septum, bifid uterus, and ipsilateral renal agenesis (Herlyn-Werner-Wunderlich syndrome) J Pediatr Surg. 2006;41(5):987–992. doi: 10.1016/j.jpedsurg.2006.01.021. http://www.ncbi.nlm.nih.gov/pubmed/16677898 [Accessed 2006 May, 1] Available from. [DOI] [PubMed] [Google Scholar]
- 3.The American fertility society classifications of adnexal adhesions, distal tubal occlusion, tubal occlusion secondary to tubal ligation, tubal pregnancies, mullerian anomalies and intrauterine adhesions. [DOI] [PubMed]
- 4.Park N.H., Park H.J., Park C.S., Park S.I. Herlyn-Werner-Wunderlich Syndrome with unilateral hemivaginal obstruction, ipsilateral renal agenesis, and contralateral renal thin GBM disease: a case report with radiological follow-up. J Korean Soc Radiol. 2008;62(4) https://synapse.koreamed.org/DOIx.php?id=10.3348/jksr.2010.62.4.383 [cited 2008] Available from. [Google Scholar]
- 5.Behr S.C., Courtier J.L., Qayyum A. Imaging of müllerian duct anomalies. Radiographics. 2012;32(6):E233–E250. doi: 10.1148/rg.326125515. http://www.ncbi.nlm.nih.gov/pubmed/23065173 [Accessed October 1, 2012] Available from. [DOI] [PubMed] [Google Scholar]
- 6.Jindal G., Kachhawa S., Meena G.L., Dhakar G. Uterus didelphys with unilateral obstructed hemivagina with hematometrocolpos and hematosalpinx with ipsilateral renal agenesis. J Hum Reprod Sci. 2009;2(2):87–89. doi: 10.4103/0974-1208.57230. http://www.ncbi.nlm.nih.gov/pubmed/19881156 [Accessed July 1, 2009] Available from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang J., Zhu L., Lang J., Liu Z., Sun D., Leng J. Clinical characteristics and treatment of Herlyn-Werner-Wunderlich syndrome. Arch Gynecol Obstet. 2014;290(5):947–950. doi: 10.1007/s00404-014-3286-5. http://www.ncbi.nlm.nih.gov/pubmed/24866888 [Accessed November 28, 2014] Available from. [DOI] [PubMed] [Google Scholar]