Abstract
Dysfunctional affective processes are central to the experience of internalizing disorders (e.g., depression, anxiety, and related disorders). Specifically, extreme positive affect and elevated negative affect each have unique and robust patterns of associations with internalizing symptoms This article examines affect as both an individual difference and a within-person dynamic process that unfolds over time. Recent research is reviewed that clarifies the hierarchical structure of affect and facet-level associations with symptoms, affect-laden traits that confer risk for internalizing psychopathology, models of emotion regulation, and how emotion regulation abilities and strategies contribute to or detract from psychological well-being. Several measurement challenges in this literature are identified and discussed, including possible conceptual and content overlap, mood-state distortion, naturalistic assessment in daily life, and the benefits and limitations of self-reported affective experience.
Keywords: positive affectivity, negative affectivity, internalizing symptoms, emotion regulation, clinical traits
Our daily lives are accompanied by a constant stream of affect, marked by frequent shifts in intensity and quality. Most of the time, people experience relatively subtle feelings that are primarily in the background (e.g., calmness, mild boredom, pleasantness), but these are punctuated by stronger feelings that dominate our conscious awareness (e.g., sorrow, rage, joy, excitement, terror) (Barrett, Mesquita, Ochsner, & Gross, 2007). Affect is defined as the feeling state that is central to emotional experience, though emotions also include other loosely-coupled components (e.g., facial expressions, physiological responses, behavioral tendencies; Barrett et al., 2007; Mauss, Levenson, McCarter, Wilhelm, & Gross, 2005). Affect can be broken down into independent dimensions of valence (ranging from very unpleasant to very pleasant) that indicates valuation of an experience as good vs. bad, and arousal (ranging from very weak to very strong) that indicates felt activation (Barrett et al., 2007; Russell & Barrett, 1999).
Current contextual features— such as external events and our interpretations of them, the presence of thoughts about the past or future, physical states, and motivations— help determine one’s affective experience at any given moment. It goes without saying that a person is likely to feel quite different when at a park with a friend on a beautiful day, relative to waiting to hear about the outcome of a job interview. The dynamic and contextually-bound nature of affect reflects an important evolutionary function of emotions: to provide information about the ongoing demands of our environment and aid in adaptive responding (Barrett et al., 2007). A person’s changing affective experiences across time and situations is referred to as within-person variability, which can be correlated with other within-person variables. For example, it is likely that on a day when a person feels less enthusiastic than is typical for them, they may also feel more depressed than is typical for them. Understanding what contributes to affective changes within a person and how these changes relate to important outcomes such as psychological symptoms can provide insight into modifying affective experiences or their consequences in a clinical setting.
At the same time, individuals also tend to have some degree of stability in their affect. For example, some people are more likely to experience excitement than others, even given identical situations. These individual differences—which are similar to personality traits— constitute between-person variability in affect. Individual differences in affect can be summarized by two relatively independent traits: positive affectivity (i.e., the tendency to frequently experience positive affective states) and negative affectivity (i.e., the tendency to frequently experience negative affective states). These two dimensions may be mapped onto the valence and arousal dimensions via a 45 degree rotation, interpretable as relatively activated instantiations of each type of valence (Russell & Barrett, 1999; Watson & Naragon-Gainey, 2014).1 Why do people differ in their tendencies to experience positive and negative emotions? Positive and negative affectivity are linked to evolutionarily-based dimensions of temperament and personality that develop early in life and have a genetic component, though they are also shaped by experience (e.g., Watson & Naragon-Gainey, 2014; Watson, Wiese, Vaidya, & Tellegen, 1999). High levels of negative affectivity reflect the tendency to withdraw from potentially dangerous situations and react strongly to stress. Someone with high levels of negative affectivity is more likely to feel upset when receiving minor critical feedback than someone with lower levels of negative affectivity, who may be either unfazed or only mildly and briefly upset. In contrast, high levels of positive affectivity are associated with the tendency to approach potentially rewarding or enjoyable situations and engage in social interactions (Watson & Clark, 1992; Watson & Naragon-Gainey, 2014). A person high in positive affectivity is likely to derive more pleasure from rewarding experiences (e.g., social events, vacations, hobbies/leisure activities, academic achievements) and expend more effort in seeking them out.
Overview
Affect is broadly relevant to many areas of psychology and related fields, given its close association with basic cognitive and interpersonal processes. In particular, affect is fundamental to understanding a wide range of psychopathology, as the vast majority of psychological disorders include dysfunctional affective experiences (e.g., Barrett et al., 2007). It is arguably most central to internalizing disorders (depression, various types of anxiety, and other related disorders), which are all characterized by excessive negative affect. In addition, a subset of internalizing disorders exhibit excessive or deficient positive affect (Mineka, Watson, & Clark, 1998; Watson & Naragon-Gainey, 2014).
In this article, we review the current state of the literature on the associations of affect and its regulation with internalizing symptoms, including a consideration of measurement challenges and recommendations. Although affective experiences certainly have associated biological and behavioral underpinnings, we focus here on subjective experiences as measured via self-report, because this method most directly assesses feeling states in explicit awareness. We also consider both within-person and between-person variability in affect, as each gives important and complementary information about affective processes (though research on within-person processes is relatively new and so limited information is available). Specifically, within-person analyses help clarify contributors to or consequences of variations in affect for a given person, answering questions such as how momentary increases in sadness relate to well-being at that time or shortly after. In contrast, between-person analyses can predict who is likely to have certain affective experiences or consequences, due to their general tendencies, answering questions like whether people who tend to experience more sadness in general also tend to have lower well-being in general.
Affective Foundations of Internalizing Symptoms
Basic Associations.
The associations of negative and positive affectivity (and closely-related traits such as neuroticism and extraversion, respectively) with internalizing symptoms are well-characterized by many studies, with largely consistent findings across clinical and non-clinical samples. Importantly, this is not just a cross-sectional phenomenon, as these traits prospectively predict changes in depressive and anxiety symptoms over months or years (for meta-analyses of longitudinal studies, see Jeronimus, Kotov, Riese, & Ormel, 2016; Khazanov & Ruscio, 2016).
Overall, negative affectivity is elevated in nearly all of the internalizing disorders, although the magnitude of the association varies by disorder, where associations are generally strongest for depression and generalized anxiety disorder (GAD) (e.g., Mineka et al., 1998; Watson & Naragon-Gainey, 2014). Positive affectivity shows much greater specificity in its associations with internalizing disorders than does negative affectivity. Whereas positive affectivity is elevated among individuals with bipolar disorder (Gruber, 2011; Stanton & Watson, 2015; Watson et al., 2012), it is inversely associated with depression and social anxiety, and it is not substantially related to most other types of anxiety (Mineka et al., 1998; Watson & Naragon-Gainey, 2010, 2014). One possible explanation for why low positive affectivity is specific to depression and social anxiety is that they are both associated with social withdrawal, which is linked to low positive affectivity because they are both components of extraversion. However, when the facets of extraversion were modeled, only low positive affectivity was associated with both depression and social anxiety (Naragon-Gainey, Watson, & Markon, 2009; Spinhoven, Elzinga, van Hemert, de Rooij, & Penninex, 2014), suggesting that it is a specific contributor to their high rates of comorbidity.
One limitation of these studies is that most rely on retrospective measures of affect and symptoms that ask participants to generalize about their experiences over long periods of time, which may not accurately reflect moment-by-moment experiences as they occur in daily life. However, one study that assessed affect and symptoms repeatedly in daily life in real time supported the generalizability of these findings to daily life. Specifically, between-person analyses revealed that treatment-seeking individuals with elevated daily ratings of negative affect had more severe internalizing symptoms (e.g., depression, social anxiety, panic, worry) assessed throughout the study, whereas people with lower positive affect in daily life reported greater daily depression (Naragon-Gainey, 2018). Furthermore, this study provided initial evidence that within-person associations (here, how a person’s current affect—relative to their average affect— is associated with their current symptoms and symptoms later that day) mirror the previously-reviewed findings on individual differences in affect and symptoms. Results indicated that affective states may systematically influence downstream symptoms even over short periods (i.e., 8 to 24 hours) (Naragon-Gainey, 2018). These within-person findings suggest that if we can reduce instances of negative affect (or increase positive affect) as they occur, we may be able to prevent greater symptoms of depression or anxiety soon after.
Taken together, there is robust evidence that negative affectivity is broadly and positively associated with internalizing disorders, whereas positive affectivity is more selectively and variably associated with a few disorders. Based on these findings, we can roughly estimate someone’s level of risk for mood and anxiety disorders if we know their trait negative and positive affectivity levels, though our ability to distinguish between specific disorders with these traits is limited.
Facets of Affectivity.
Trait affect is hierarchical, meaning that negative and positive affectivity both can be partitioned into several narrower facets. For negative affectivity, these facets include specific feelings such as sadness, anxiety or fear, anger or hostility, and guilt (Naragon-Gainey & Watson, in press; Watson & Clark, 1999; Watson, Stasik, Chimielewski, & Naragon-Gainey, 2012). Similarly, positive affectivity can be decomposed into facets such as joviality, attentiveness, self-assurance, and vitality (Naragon-Gainey & Watson, in press; Stanton & Watson, 2015; Watson & Clark, 1999; Watson et al., 2012). One study found a replicable two-factor structure across numerous faceted measures of positive affectivity, consisting of joviality (i.e., joyfulness, feeling energetic, attentiveness) and experience-seeking (i.e., experience-seeking, self-assurance) (Stanton & Watson, 2015).
There is limited research examining how these specific facets relate to internalizing disorders. For negative affectivity and neuroticism, shared variance among the facets— rather than the unique effects of a specific facet— may be primarily responsible for associations with symptoms. Although the sadness facet uniquely contributes to the prediction of depression, and the anxiety facet uniquely contributes to the prediction of generalized anxiety in some studies (Naragon-Gainey & Watson, 2014, 2018; Uliaszek et al.,2009; Zinbarg et al., 2016), this is likely due in part to overlapping content between the facets and symptoms (examined in more detail later in this review). Thus, distinctions among different types of negative affect do not seem to be key to understanding risk for internalizing symptoms. In contrast, there may be greater differentiation in the associations between positive affectivity facets and symptoms. For example, the joviality component was most strongly inversely related to internalizing symptoms (including depression and social anxiety), whereas the experience-seeking component was uniquely elevated for manic symptoms (Stanton & Watson, 2015). Further research at the lower-order level is important to clarify the specific components that drive associations, because this will allow for more precise conclusions about why and how affect contributes to symptoms and which types of affective experiences are most important for psychological well-being (Ormel et al., 2013; Watson & Naragon-Gainey, 2014).
Affect-Laden Clinical Traits.
Affective traits are relatively distal predictors of internalizing symptoms that interact with many other factors. As such, trait affect alone cannot completely predict which specific disorders an individual will develop or whether they will develop a disorder at all (Nolen-Hoeksema & Watkins, 2011). Clinical traits are more proximal individual differences that can better describe who is likely to develop which specific symptoms, beyond the broad risk conferred by affective traits (e.g., Paulus, Talkovsky, Heggeness, & Norton, 2015). Clinical traits can help clinicians and researchers make more specific predictions about whether, for example, a particular individual with elevated negative affectivity is at risk for panic disorder vs. specific phobia.
Researchers have identified and studied a multitude of clinical traits that are associated with high negative affectivity over the past several decades, including anxiety sensitivity, rumination, perfectionism, intolerance of uncertainty, dysfunctional attitudes, fear of negative evaluation, thought-action fusion, and self-criticism, to name a few. Most often, these clinical traits were developed and conceptualized with regard to a particular disorder (e.g., anxiety sensitivity was thought to be specific to panic, rumination to depression, intolerance of uncertainty to GAD). However, numerous clinical traits are better characterized as transdiagnostic risk factors of internalizing disorders, meaning that they are broadly and nonspecifically associated with a variety of internalizing disorders. Some well-studied transdiagnostic traits include anxiety sensitivity (Naragon-Gainey, 2010), rumination (Aldao, Nolen-Hoeksema, & Schweizer, 2010; Olatunji, Naragon-Gainey, & Wolitzky-Taylor, 2013), intolerance of uncertainty (Gentes & Ruscio, 2011), and perfectionism (Limburg, Watson, Hagger, & Egan, 2017). Furthermore, in studies that accounted for comorbidity, clinical traits were still significantly associated with symptoms, indicating that the observed transdiagnostic associations were not solely due to comorbidity (Naragon-Gainey, 2010; Olatunji et al., 2013).
These findings suggest that the above clinical traits may be good candidates for proximal and specific risk factors that bridge the association between trait affect and internalizing symptoms. But since all of the clinical traits are characterized by negatively-valenced cognitions or responses to negative stimuli, it is possible that they simply reflect levels of negative affectivity. Thus, it is important to examine whether clinical traits convey unique incremental information in understanding risk for internalizing disorders, above and beyond what we already know from negative affectivity. One approach to addressing this question is to test whether clinical traits are empirically distinct from negative affectivity/neuroticism and from one another. Two studies found that a variety of clinical traits were largely indistinguishable from neuroticism (Mahaffey, Watson, Clark, & Kotov, 2016; Naragon-Gainey & Watson, 2018), and that they were most closely related to the anxiety facet specifically (Naragon-Gainey & Watson, 2018). Similarly, a variety of clinical traits loaded onto a single, unified factor in a meta-analysis and longitudinal study (Hong & Cheung, 2015; Hong, Lee, Tsai, & Tan, 2017). These studies confirm that most clinical traits are empirically very closely related to one another and to negative affectivity. Nonetheless, there is some evidence for their incremental validity—beyond affectivity and personality traits— when predicting mood and anxiety disorders in clinical and non-clinical samples (Mahaffey et al., 2016), particularly for anxiety sensitivity (e.g., Naragon-Gainey & Watson, 2018; Norr et al., 2013; Paulus et al., 2015; Zinbarg et al., 2016) and intolerance of uncertainty (e.g., Brown & Naragon-Gainey, 2013; Norr et al., 2013; Paulus et al., 2015).
This research indicates that even though clinical traits share much in common with negative affectivity, some of them still provide unique and important information in predicting internalizing disorder risk. As such, they are valuable to consider— along with affectivity— when trying to understand risk for these disorders. In addition, clinical traits may offer more tractable treatment targets than affectivity because they are narrower in scope, yet still contribute to the development and maintenance of multiple disorders. Further research is needed to clarify the utility of incorporating treatment of clinical traits in interventions, but initial results are promising, particularly for anxiety sensitivity (e.g., Schmidt, Norr, Allan, Raines, & Capron, 2017; Timpano et al., 2016).
Regulation of Affect and its Consequences
Clearly, affect and related traits are important contributors to psychological well-being, but individuals are not simply passive vessels of feeling states that “happen” to them. Rather, people frequently attempt to modify the way they feel via their thoughts or actions. For example, individuals may try to maintain their contentment by sharing their emotions with a friend, reduce their sadness by distracting themselves from an upsetting situation, or increase their anger by ruminating on how they were wronged. Broadly, emotion regulation2 refers to any attempt— even those that are implicit or habitual— to alter the course of an emotional experience, and it is one important mechanism linking affect to psychopathology (e.g., Sheppes et al., 2015).
Models of Emotion Regulation.
Though the definition of emotion regulation is fairly straightforward, measurement and theoretical models are complex and varied. Emotion regulation is operationalized quite differently across studies, sometimes resulting in confusion when synthesizing research. Current models of emotion regulation may be divided into three broad groupings: (1) underlying abilities or skills that contribute to emotion regulation, (2) the temporal process of emotion regulation, and (3) specific strategies one uses in regulation attempts (see Naragon-Gainey, McMahon, & Chacko, 2017, for more detail). Ability models center around dispositional skills that are thought to facilitate adaptive emotion regulation, such as those embodied in the Difficulties in Emotion Regulation Scale (DERS; Gratz & Roemer, 2004) and the Emotion Regulation Skills Questionnaire (ERSQ; Berking et al., 2008). Emotion regulation abilities include emotional awareness, emotional clarity, distress tolerance, acceptance of aversive thoughts and emotions, controlling one’s emotion-driven impulses, and effective utilization of emotion regulation strategies. Emotion regulation flexibility, or accurately matching one’s strategy use to the demands of the current context, is also emerging as a potentially important ability (e.g., Bonanno & Burton, 2013).
The dominant temporal model is Gross’ (1998, 2015) process model, which describes in detail the temporal stages that unfold during an emotion regulation attempt. The most recent version of the model (i.e., extended process model; Gross, 2015) conceptualizes emotion regulation as a series of valuation cycles that lead to numerous sequential outputs. These decisions include whether to attempt regulation or not, selection of a specific strategy, implementation of the strategy, and monitoring processes that determine maintaining, switching, or stopping use of a given strategy.
Much of the literature on emotion regulation has focused on specific emotion regulation strategies (e.g., reappraisal, avoidance, social support, drinking alcohol, distraction, acceptance, exercising, etc.) and their outcomes, perhaps because they are amenable to clean experimental manipulation and quick self-report assessment. Within the clinical literature, common strategy-focused approaches include the adaptive-maladaptive framework, and grouping strategies based on their temporal placement as specified in Gross’ process model.
In the adaptive-maladaptive model (e.g., Aldao et al., 2010; Aldao & Nolen-Hoeksema, 2012), dispositionally-assessed emotion regulation strategies are organized based on their empirical associations with psychopathology: strategies inversely associated with psychopathology are labeled adaptive, and strategies positively associated with psychopathology are labeled maladaptive. Although the associations between strategies and symptoms appear robust (see Aldao et al., 2010 for a meta-analysis), this framework is limited in that it assumes a uniform relationship between strategies and outcomes, which neglects the role of context that contributes to variability of use and to differential consequences of a given strategy (e.g., Bonanno & Burton, 2013). The process model (Gross, 1998, 2015) can be used to map specific strategies onto the temporal course of the emotion generation and regulation process in a way that is more contextually-sensitive and incorporates emotion dynamics. For example, antecedent-based strategies such as reappraisal occur prior to the emotional experience, whereas response-based strategies such as suppression occur after the emotional experience is underway. However, the granularity required to study this approach can be challenging, as the entire regulatory process can unfold over the course of seconds. The few studies that empirically evaluated the temporal deployment of specific strategies were mixed as to whether different strategies occur at hypothesized stages of an emotional experience or whether order of strategy use is important (e.g., Goldin, McRae, Ramel, & Gross, 2008; Kalokerinos, Resibois, Verduyn, & Kuppens, 2017).
While all of the above models have utility, it is important to note that they are not interchangeable, and that each is better suited for some research questions or for use with some methods. We focus next on the sizeable literature on specific emotion regulation strategies and their outcomes.
Structural Analyses of Strategy Use.
A recent approach to organizing and modeling the large array of emotion regulation strategies is to empirically identify patterns of strategy use (Lee et al., 2015; Naragon-Gainey et al., 2017; Seligowski & Orcutt, 2015). These studies seek to reduce the many possible strategies (likely hundreds) to a few underlying dimensions that show which strategies tend to be used together and how much a given individual tends to use those strategies. A meta-analytic examination (Naragon-Gainey et al., 2017) capitalized on the vast existing empirical literature on self-reported dispositional measures, focusing on 12 commonly studied and enacted strategies. An exploratory factor analysis was conducted on the meta-analytic correlation matrix among all of these strategies, revealing three groupings: Disengagement (behavioral avoidance, distraction, low mindfulness), Aversive Cognitive Perseveration (rumination, experiential avoidance, low acceptance, low distraction), and Adaptive Engagement (reappraisal, problem solving, mindfulness) (Naragon-Gainey et al., 2017). Given that there are many possible strategies, these groupings can help researchers and clinicians focus on important underlying dimensions that are shared across strategies.
Similar to affect, there are both between-person tendencies and within-person variability in strategy use (e.g., Brans et al., 2013). For example, a person may try to change his emotions by drinking alcohol in many situations, such that he uses alcohol as an emotion regulation strategy more frequently than most people. Despite this tendency, he probably does not use alcohol to regulate his emotions in every situation. Rather, he is likely to use another emotion regulation strategy (e.g., distraction or mindfulness) instead of alcohol in situations where he believes alcohol would be detrimental (e.g., when he is anxious while giving a speech or annoyed while driving in bad traffic). To better capture this within-person variability in strategy use in daily life, a study examined the daily use of 11 strategies in intensive longitudinal data collected from two samples (one clinical and one student). These data allow for the exploration of (1) the between-person structure of these strategies, which is conceptually similar to the meta-analysis described above except that it is assessed as the strategy use occurs in daily life, and (2) the within-person structure of the emotion regulation strategies, or which strategies people tend to use together on a given occasion (McMahon & Naragon-Gainey, 2018).
At the between-person level, a two-factor structure emerged in both samples, with factors labeled Engagement (similar to Adaptive Engagement in the meta-analysis) and Avoidance (similar to Disengagement and Aversive Cognitive Perseveration in the meta-analysis). These results are generally consistent with the long-standing avoidance vs. approach categories in the coping literature (e.g., Roth & Cohen, 1986), as well as the adaptive-maladaptive model (e.g., Aldao et al., 2010). However, the within-person structure found in this study was more complicated: factors of Attentional Shift (i.e., experiential avoidance, distraction, reappraisal, reflection), Avoidance (similar to above), and Emotional Expression (i.e., social support, low suppression) emerged in both samples, whereas low acceptance and savoring broke off from Avoidance to form its own factor in the student sample (McMahon & Naragon-Gainey, 2018). With further research on variables related to the selection and implementation of these strategy groupings as they are naturalistically employed on a given occasion, these studies may provide clinicians with tools to efficiently assess their clients’ strategy use and to guide clients toward more adaptive emotion regulation attempts in their daily lives.
Associations of Emotion Regulation with Internalizing Symptoms.
Emotion regulation abilities and strategies have been linked to a wide array of psychopathology and to psychological well-being across many studies, with a range of designs and methods. In a meta-analytic review of the effects of six strategies (acceptance, problem-solving, reappraisal, avoidance, rumination, and suppression) assessed with dispositional self-report measures, all of the strategies except acceptance were significantly associated with depression, anxiety, eating pathology, and substance use in clinical and non-clinical samples (Aldao et al., 2010). These results provide support for the notion that adaptive strategies are transdiagnostic protective factors (and, conversely, maladaptive strategies confer risk) for a range of symptoms. Though acceptance was not significantly associated with symptoms in this meta-analysis, more recent individual studies reported significant relationships of acceptance with internalizing symptoms and well-being (e.g., Boelen, & Lenferink, 2018; Kotsou, Leys, & Fossion, 2018).
The above associations also extend to reports of strategies and symptoms in daily life, in both clinical and nonclinical samples. Within-person analyses indicated that on occasions when people used more maladaptive strategies (such as avoidance, rumination, thought suppression, and expressive suppression), they also had higher levels of internalizing symptoms at that time or shortly after (Kashdan et al., 2014; Li, Starr, & Hershenberg, 2017; McMahon & Naragon-Gainey, 2018; Short et al., 2018). In contrast, on occasions when people used more adaptive strategies (such as acceptance, reappraisal, savoring, and reflection), they had fewer subsequent internalizing symptoms (e.g., Li et al., 2017; McMahon & Naragon-Gainey, 2018). Similarly, perceived emotion regulation success on a given occasion was associated with fewer subsequent internalizing symptoms (depression, social anxiety, panic, worry) in a clinical sample (Park & Naragon-Gainey, in press). Some of these studies also examined between-person effects, finding that people with more adaptive and less maladaptive emotion regulation strategy use (McMahon & Naragon-Gainey, 2018) and greater perceived emotion regulation success in daily life (Park & Naragon-Gainey, in press) had fewer internalizing symptoms overall. Finally, there is evidence that the simultaneous use of multiple strategies interact with one another. Generally, adaptive strategies are most strongly (negatively) related to symptoms among those who also use maladaptive strategies, suggesting that adaptive strategy use can help reduce the negative consequences of maladaptive strategies (Aldao, Jazaieri, Goldin, & Gross, 2014; Aldao & Nolen-Hoeksema, 2012; McMahon & Naragon-Gainey, in press).
Beyond a simple direct association, the use of specific emotion regulation strategies and abilities is also a proximal mechanism contributing to the development and maintenance of psychopathology. For example, emotion regulation strategies (e.g., acceptance, suppression, reappraisal) and abilities (e.g., flexibly shifting attention, tolerating negative emotions, access to emotion regulation strategies) mediated the associations of a variety of risk or protective factors with depression (Boden & Thompson, 2015; Vine & Aldao, 2014) and with several types of anxiety symptoms (O’Connor, Staiger, Kambouropoulos, & Smillie, 2014; Tull, Berghoff, Wheeless, Cohen, & Gratz, 2018; Vine & Aldao, 2014). In addition, a recent study in daily life found that perceived emotion regulation success mediated the association of daily emotional clarity with reduced subsequent internalizing symptoms in a clinical sample. These effects were both within-person (when a person has more momentary clarity than they typically do, this predicted fewer symptoms on the next occasion) and between-persons (people who had greater clarity overall had fewer symptoms overall) (Park & Naragon-Gainey, in press). Taken together, these findings —particularly those using a longitudinal method examining within-person changes— suggest that emotion regulation may be a relatively proximal predictor of internalizing symptoms that can help explain how extreme affect contributes to symptoms.
Consistent with theory, there is growing empirical evidence that effective emotion regulation can also weaken the associations between risk factors for psychopathology and symptom severity. For example, greater decentering – an emotion regulation ability that enables individuals to take an observer perspective on their own thoughts and feelings – attenuated the impact of high negative affectivity and low positive affectivity on symptoms such as dysphoria, panic, and anhedonia, using both a cross-sectional design and momentary assessment in daily life, in both clinical and non-clinical samples (Naragon-Gainey & DeMarree, 2017). Decentering also reduced the association between parasympathetic inflexibility (a broad physiological risk factor for psychopathology) and subsequent depressive symptoms in a sample of undergraduates (Stange, Hamilton, Fresco, & Alloy, 2017). Likewise, higher levels of cognitive reappraisal attenuated the association of emotional reactivity with depressive symptoms in a community sample of adolescents (Shapero, Abramson, & Alloy, 2016), and of emotional clarity with PTSD symptoms among veterans with PTSD (Boden, Bonn-Miller, Kashdan, Alvarez, & Gross, 2012). On the other hand, on occasions when people engaged in more rumination than was typical for them, the association of negative events and depressive symptoms that day was stronger, and on occasions when participants engaged in more dampening than usual, the association between positive events and decreased depressive symptoms that day was weakened (Li et al., 2016). These findings have important implications for treatment, as they suggest that adaptive emotion regulation can decrease symptoms even among those who have strong temperamental, biological, or environmental risk factors, or who have already developed a disorder. As such, numerous therapies have incorporated emotion regulation as an explicit treatment target (e.g., the unified protocol, emotion regulation therapy, dialectical behavior therapy).
Summary and Schematic Model
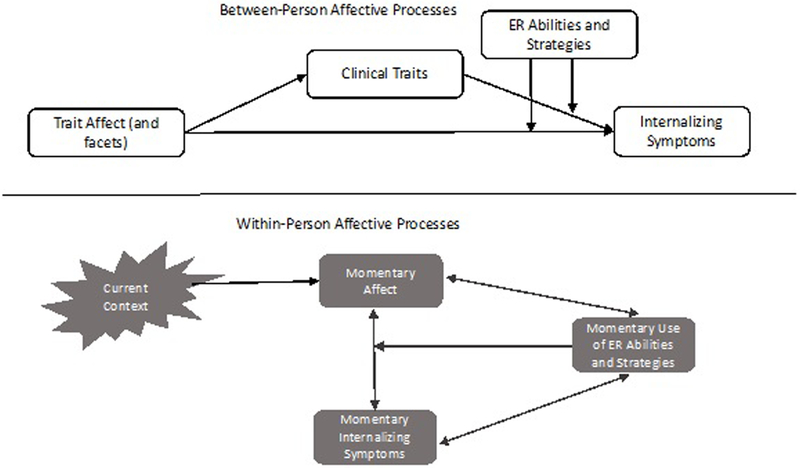
Figure 1 provides an illustration of the associations among the major variables described in this review. The top portion of the figure shows between-person processes, or person-level tendencies that predict individual differences in symptoms. Trait affect and its facets begins to develop early in life, and individuals with elevated negative affectivity and extreme positive affectivity—in combination with certain life experiences— are likely to develop high levels of particular clinical traits. Trait affect predicts risk for internalizing symptoms directly, as well as indirectly via clinical traits. For individuals with relatively poor emotion regulation abilities or ineffective use of emotion regulation strategies, affectivity and clinical traits are more strongly associated with internalizing symptoms. In contrast, affective traits and symptoms are more weakly associated among those with more adaptive emotion regulation, decoupling their link.
Figure 1.
Schematic figure showing associations among affect, clinical traits, emotion regulation (ER), and internalizing symptoms. The top portion of the figure shows between-person processes, or individual differences on each variable that predict individual differences in symptoms. The bottom portion of the figure shows within-person processes, or how these variables relate to one another for a given individual on a given occasion.
At the within-person level, or how these variables relate to one another for a given individual on a given occasion, current external and internal contextual features are an important determinant of momentary affect. Given the very quick timescale at which emotional processes change, many of the associations shown are bidirectional and cyclical. For example, if someone is currently feeling anxious because her dog is sick, that may increase her panic symptoms, but greater panic may also make her feel more anxious. Upon noting that she feels anxious, she may attempt to modify that emotion using a particular ability (for example, decentering from worried thoughts) and/or strategy (for example, problem-solving how she can get her dog the care he needs). Depending on the success of this attempt, her affect and symptoms may change in type or intensity. In addition, emotion regulation may function as a moderator at the within-person level, interrupting the prepotent tendency for an affective experience to immediately influence a particular symptom. As these processes unfold over time, they may lead to a new context (for example, her friends asking why she seems upset) or a new affective experience (now she feels not only anxious, but also embarrassed), triggering another iteration of this cycle.
Measurement Challenges and Recommendations
We conclude this article by considering several issues in measuring affect and related traits, along with some recommendations for improving research on affect and psychopathology.
Conceptual and Methodological Overlap.
The definitions of trait affect and internalizing symptoms, as well as an examination of their measures, show that they have some overlapping content (Ormel, Rosmalen, & Farmer, 2004; Uliaszek et al., 2009; Watson & Naragon-Gainey, 2014). Specifically, one of the required criteria for major depression (depressed mood) corresponds to the sadness component of negative affectivity, whereas the other required criteria (anhedonia) is highly similar to the joviality component of low positive affectivity. Conversely, mania is defined in part by sustained experiences of very intense positive affect. The anxiety facet of negative affectivity varies somewhat in its content across measures, but it is often a combination of anxious apprehension or worry (especially relevant to GAD) and anxious arousal (especially relevant to panic). This overlap has led some researchers to question the utility of affectivity and related traits as risk factors for internalizing symptoms, suggesting that if associations primarily reflect shared content, they are tautological and non-informative (e.g., Ormel et al., 2004). However, several empirical studies have not supported this assertion, finding that the associations of negative affectivity and neuroticism with internalizing disorders are not fully accounted for by shared content (e.g., Naragon-Gainey & Watson, 2014; Ormel et al., 2013; Uliaszek et al., 2009).
Nonetheless, to the extent that there is overlap, how can this problem be addressed and minimized? One straightforward solution is to remove conceptually-overlapping items from trait affectivity scales when examining associations with internalizing symptoms, but this may negatively impact the validity of affectivity measures by eliminating definitive and key content (Nicholls, Licht, & Pearl, 1982; Riese, Ormel, Aleman, Servaas, & Jeronimus, 2016; Uliaszek et al., 2009). For example, if any reference to experiencing sadness or anxiety is removed from a measure of negative affectivity, it is likely no longer measuring negative affectivity and the interpretation of its scores becomes muddled. With longitudinal data, a viable approach may be to statistically control for baseline symptoms when predicting subsequent symptoms from trait affect, though this decision should be grounded in whether it clarifies one’s specific research question (Riese et al., 2016).
Unfortunately, a cross-sectional design does not allow one to control for baseline symptoms, and this design introduces a new related concern. Mood-state distortion describes the tendency of currently distressed individuals to rate their personality traits in an overly-negative manner, potentially artificially inflating associations with internalizing symptoms. While mood-state distortion is a legitimate problem, it is encouraging that several studies have found that it does not substantially alter basic conclusions about personality-symptom associations (e.g., Clark, Vittengl, Kraft, & Jarrett, 2003; Naragon-Gainey et al., 2013). In fact, statistically-removing transient variance in trait affect ratings over time (which includes influences due to current mood state) increased the associations of negative and positive affect with internalizing symptoms in a clinical sample (Naragon-Gainey et al., 2013). Regardless, when a longitudinal design is not possible, we recommend assessing the facets of trait affect or related personality traits, which allows for an empirical examination of the content that is driving observed associations (i.e., shared variance across facets vs. the unique effects of one or more facets) (Ormel et al., 2013; Watson & Naragon-Gainey, 2014). The substantive meaning of any facet-level associations can then be considered when interpreting results, including the degree of overlap in specific measures (see, for example, Naragon-Gainey & Watson, 2014).
Measurement in Daily Life.
Given the dynamic and contextually-bound nature of affect, its regulation, and internalizing symptoms, we encourage researchers to consider and employ a naturalistic intensive longitudinal design when possible. Advantages of this design include the collection of contextual information, elucidation of within-person processes, increased ecological validity, and reduced response biases associated with retrospective recall. Fortunately, the technology needed to conduct this type of research is developing rapidly and becoming more affordable and common, allowing for relatively non-invasive collection of a variety of data (including GPS location, movement, physiological monitoring, and cognitive measures) using smartphones or other wearable sensors. Despite these strengths, a number of challenges arise when using intensive longitudinal designs (see Mehl & Conner, 2012, for a detailed discussion of these issues), such as balancing comprehensive measurement with a feasible protocol that does not overly burden participants. In addition, there is a lack of (brief) self-report measures that have been developed and validated for repeated use in daily life, leading to the proliferation of untested ad-hoc composites or the use of single items. Well-validated intensive longitudinal measures of affect, symptoms, and other variables are an important next step.
The nature of affective processes introduces some additional concerns for intensive longitudinal designs. Real-time reporting on affect and its regulation may interrupt the emotional experience prematurely, and responses may vary depending upon the point in the regulation process at which a participant responds to questions. Most intensive longitudinal research on affect utilizes a signal-contingent design, which randomly samples experiences of affect throughout the day. When a particular type of affective experience (e.g., a specific emotion, or a high-intensity emotion of any type) or the experience of an episodic symptom is the focus of a study, an event-contingent design in which participants initiate reports upon specific emotional experiences may be better. However, initiating these reports requires greater motivation and awareness of experiences (because there is no prompt), as well as a clear definition of what constitutes a “triggering event” for the report. When examining lagged associations (e.g., between affect now and symptoms at the next report), it is important to match the sampling frequency to the actual time-course of effects (their onset, persistence, and decay), but there is little empirical data to guide such decisions (see Naragon-Gainey, 2018; Schenk, Bos, Slaets, de Jonge, & Rosmalen, 2017, for examples). In cases where the appropriate interval is unknown, more frequent sampling is preferable (as longer lags can still be examined), and some statistical tools such as a differential time-varying effect model can help empirically identify the optimal lags (Roche, Jacobson, & Pincus, 2016). Overall, assessment in daily life opens up a range of exciting possibilities for addressing nuanced research questions related to affect and psychopathology that are well worth the challenges they present.
Reflections on Self-Reported Assessment.
In recent years, there has been renewed attention to an enduring issue: limitations of self-report and the importance of connecting multiple levels of assessment in a single study (Haeffel & Howard, 2010; Kozak & Cuthbert, 2016; see also Nisbett & Wilson, 1977). Self-report measures are appropriate only for experiences of which individuals have conscious awareness, and so they cannot provide information about implicit cognitive or biological processes underlying emotional experiences. Furthermore, these reports are inaccurate at times due to poor insight or awareness, recall biases, response biases, social desirability, and weak instruments (e.g., Nisbett & Wilson, 1977), and all too often self-report is used for its expediency, without careful consideration of the optimal level of measurement for a given study (Haeffel & Howard, 2010).
But we argue that just as self-report should not be mindlessly utilized, neither should it automatically or unilaterally be dismissed as inferior to other approaches (Haeffel & Howard, 2010). Across many theories, subjective experience is considered the core of emotion (e.g., Russell & Barrett, 1999; Barrett et al., 2007; LeDoux & Hofmann, 2018), and measurement of subjective experience by definition requires introspection that is explicitly described by the participant (that is, self-reported). Furthermore, one fundamental goal of psychopathology research is to understand— and when there is extensive suffering, to alter—the subjective human experience of emotion (LeDoux & Hofmann, 2018). Thus, although self-report is not sufficient for a comprehensive assessment of affective processes and internalizing symptoms, it does provide necessary and critical information. Whenever possible, self-report measures should be used in conjunction with other levels of analysis (e.g., genes, psychophysiology, neurological circuits, cognitive measures, behavioral outcomes) to combine complementary sources of information and yield a more complete picture of affective experience (see, for example, Stange et al., 2017; Tull et al., 2018). It is also important to use psychometrically-sound self-report measures that were thoughtfully selected for the specific research question at hand.
Conclusions
A rich body of research demonstrates that affect has important implications for psychological well-being. Individual differences in affect and related clinical traits can help predict who is at risk for internalizing disorders, and recently research has begun to explore how variability in each person’s momentary affective experience may influence their subsequent well-being in daily life. Emotion regulation is also essential to consider in tandem with affect, because it can elucidate the nature of affectivity-symptom associations, as well as modify the strength of these associations. We urge researchers when possible to simultaneously study large networks of affective traits and emotion regulation variables with a variety of symptoms, to facilitate identification of unique and robust associations that may serve as potent treatment targets. Without such an approach, constructs and studies will proliferate but remain difficult to synthesize, and research progress will be slowed. Finally, we hope that addressing some of the challenges to measuring affect—an elusive, subjective phenomenon— will help further this important area of research as it is studied in the lab and in daily life.
Footnotes
While both models have utility, this review focuses on the positive affectivity/negative affectivity dimensions (rather than the valence/arousal dimensions) for two reasons: self-report measures of trait affect most commonly use this rotation as a model, and a pure arousal dimension that is independent of valence (for example, quiet or still vs. aroused or astonished) is less relevant to psychological symptoms.
We use the common term emotion regulation throughout this article (rather than affect regulation), as it focuses on modifying feeling states and typically subsumes affect regulation.
References
- Aldao A, Jazaieri H, Goldin PR, & Gross JJ (2014). Adaptive and maladaptive emotion regulation strategies: Interactive effects during CBT for social anxiety disorder. Journal of Anxiety Disorders, 28(4), 382–389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aldao A, & Nolen-Hoeksema S (2012). When are adaptive strategies most predictive of psychopathology? Journal of Abnormal Psychology, 121(1), 276–281. [DOI] [PubMed] [Google Scholar]
- Aldao A, Nolen-Hoeksema S, & Schweizer S (2010). Emotion-regulation strategies across psychopathology: A meta-analytic review. Clinical Psychology Review, 30(2), 217–237. [DOI] [PubMed] [Google Scholar]
- Barrett LF, Mesquita B, Ochsner KN, & Gross JJ (2007). The experience of emotion. Annual Review of Psychology, 58, 373–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berking M, Wupperman P, Reichardt A, Pejic T, Dippel A, & Znoj H (2008). Emotion-regulation skills as a treatment target in psychotherapy. Behaviour Research and Therapy, 46(11), 1230–1237. [DOI] [PubMed] [Google Scholar]
- Boden MT, Bonn-Miller MO, Kashdan TB, Alvarez J, & Gross JJ (2012). The interactive effects of emotional clarity and cognitive reappraisal in posttraumatic stress disorders. Journal of Anxiety Disorders, 26(1), 233–238. [DOI] [PubMed] [Google Scholar]
- Boden MT, & Thompson RJ (2015). Facets of emotional awareness and associations with emotion regulation and depression. Emotion, 15(3), 399–410. [DOI] [PubMed] [Google Scholar]
- Boelen PA, & Lenferink LIM (2018). Experiential acceptance and trait-mindfulness as predictors of analogue post-traumatic stress. Psychology and Psychotherapy: Theory, Research and Practice, 91(1), 1–14. [DOI] [PubMed] [Google Scholar]
- Bonanno GA, & Burton CL (2013). Regulatory flexibility: An individual differences perspective on coping and emotion regulation. Perspectives on Psychological Science, 8(6), 591–612. [DOI] [PubMed] [Google Scholar]
- Brans K, Koval P, Verduyn P, Lim YL, & Kuppens P (2013). The regulation of negative and positive affect in daily life. Emotion, 13(5), 926–939. [DOI] [PubMed] [Google Scholar]
- Brown TA, & Naragon-Gainey K (2013). Evaluation of the unique and specific contributions of dimensions of the triple vulnerability model to the prediction of DSM-IV anxiety and mood disorder constructs. Behavior Therapy, 44, 277–292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark LA, Vittengl J, Kraft D, & Jarrett RB (2003). Separate personality traits from states to predict depression. Journal of Personality Disorders, 17, 152–172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gentes EL, & Ruscio AM (2011). A meta-analysis of the relation of intolerance of uncertainty to symptoms of generalized anxiety disorder, major depressive disorder, and obsessive–compulsive disorder. Clinical Psychology Review, 31(6), 923–933. [DOI] [PubMed] [Google Scholar]
- Goldin PR, McRae K, Ramel W, & Gross JJ (2008). The neural bases of emotion regulation: Reappraisal and suppression of negative emotion. Biological Psychiatry, 63(6), 577–586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gratz KL, & Roemer L (2004). Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the difficulties in emotion regulation scale. Journal of Psychopathology and Behavioral Assessment, 26(1), 41–54. [Google Scholar]
- Gross JJ (1998). The emerging field of emotion regulation: An integrative review. Review of General Psychology, 2(3), 271–299. [Google Scholar]
- Gross JJ (2015). Emotion regulation: Current status and future prospects. Psychological Inquiry, 26(1), 1–26. [Google Scholar]
- Gruber J (2011). A review and synthesis of positive emotion and reward disturbance in bipolar disorder. Clinical Psychology & Psychotherapy, 18(5), 356–365. [DOI] [PubMed] [Google Scholar]
- Haeffel GJ, & Howard GS (2010). Self-report: Psychology’s four-letter word. The American Journal of Psychology, 123(2), 181–188. [DOI] [PubMed] [Google Scholar]
- Hong RY, & Cheung MW (2015). The structure of cognitive vulnerabilities to depression and anxiety: Evidence for a common core etiologic process based on a meta-analytic review. Clinical Psychological Science, 3(6), 892–912. [Google Scholar]
- Hong RY, Lee SM, Tsai F, & Tan SH (2017). Developmental trajectories and origins of a core cognitive vulnerability to internalizing symptoms in middle childhood. Clinical Psychological Science, 5(2), 299–315. [Google Scholar]
- Jeronimus BF, Kotov R, Riese H, & Ormel J (2016). Neuroticism’s prospective association with mental disorders halves after adjustment for baseline symptoms and psychiatric history, but the adjusted association hardly decays with time: A meta-analysis on 59 longitudinal/ prospective studies with 443 313 participants. Psychological Medicine, 46(14), 2883–2906. [DOI] [PubMed] [Google Scholar]
- Kalokerinos EK, Résibois M, Verduyn P, & Kuppens P (2017). The temporal deployment of emotion regulation strategies during negative emotional episodes. Emotion, 17, 450–458. [DOI] [PubMed] [Google Scholar]
- Kashdan TB, Goodman FR, Machell KA, Kleiman EM, Monfort SS, Ciarrochi J, & Nezlek JB (2014). A contextual approach to experiential avoidance and social anxiety: Evidence from an experimental interaction and daily interactions of people with social anxiety disorder. Emotion, 14(4), 769–781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khazanov GK, & Ruscio AM (2016). Is low positive emotionality a specific risk factor for depression? A meta-analysis of longitudinal studies. Psychological Bulletin, 142(9), 991–1015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kotsou I, Leys C, & Fossion P (2018). Acceptance alone is a better predictor of psychopathology and well-being than emotional competence, emotion regulation and mindfulness. Journal of Affective Disorders, 226, 142–145. [DOI] [PubMed] [Google Scholar]
- Kozak MJ, & Cuthbert BN (2016). The NIMH Research Domain Criteria initiative: Background, issues, and pragmatics. Psychophysiology, 53(3), 286–297. [DOI] [PubMed] [Google Scholar]
- LeDoux JE, & Hofmann SG (2018). The subjective experience of emotion: A fearful view. Current Opinion in Behavioral Sciences, 19, 67–72. [Google Scholar]
- Lee DJ, Witte TK, Weathers FW, & Davis MT (2015). Emotion regulation strategy use and posttraumatic stress disorder: Associations between multiple strategies and specific symptom clusters. Journal of Psychopathology and Behavioral Assessment, 37(3), 533–544. [Google Scholar]
- Li YI, Starr LR, & Hershenberg R (2017). Responses to positive affect in daily life: Positive rumination and dampening moderate the association between daily events and depressive symptoms. Journal of Psychopathology & Behavioral Assessment, 39, 412–425. [Google Scholar]
- Limburg K, Watson HJ, Hagger MS, & Egan SJ (2017). The relationship between perfectionism and psychopathology: A meta-analysis. Journal of Clinical Psychology, 73(10), 1301–1326. [DOI] [PubMed] [Google Scholar]
- Mahaffey BL, Watson D, Clark LA, & Kotov R (2016). Clinical and personality traits in emotional disorders: Evidence of a common framework. Journal of Abnormal Psychology, 125(6), 758–767. [DOI] [PubMed] [Google Scholar]
- Mauss IB, Levenson RW, McCarter L, Wilhelm FH, & Gross JJ (2005). The tie that binds? Coherence among emotion experience, behavior, and physiology. Emotion, 5(2), 175–190. [DOI] [PubMed] [Google Scholar]
- Mineka S, Watson D, & Clark LA (1998). Comorbidity of anxiety and unipolar mood disorders. Annual Review of Psychology, 49, 377–412. [DOI] [PubMed] [Google Scholar]
- McMahon TP, & Naragon-Gainey K (2018). The Multilevel Structure of Daily Emotion Regulation Strategy Use: An Examination of Within- and Between-Person Associations in Naturalistic Settings Manuscript under review.
- McMahon TP, & Naragon-Gainey K (in press). The moderating effect of maladaptive emotion regulation strategies on reappraisal: A daily diary study. Cognitive Therapy and Research
- Mehl MR, & Conner TS (2012). Handbook of Research Methods for Studying Daily Life New York, NY: Guilford Press. [Google Scholar]
- Naragon-Gainey K (2010). Meta-analysis of the relations of anxiety sensitivity to the depressive and anxiety disorders. Psychological Bulletin, 136, 128–150. [DOI] [PubMed] [Google Scholar]
- Naragon-Gainey K (2018). Affective Models of Depression and Anxiety: Extension to Within-Person Processes in Daily Life Manuscript under review. [DOI] [PubMed]
- Naragon-Gainey K, & DeMarree KG (2017). Decentering attenuates the associations of negative affect and positive affect with psychopathology. Clinical Psychological Science, 5, 1027–1047. [Google Scholar]
- Naragon-Gainey K, Gallagher MW, & Brown TA (2013). Stable “trait” variance of temperament as a predictor of the temporal course of depression and social phobia. Journal of Abnormal Psychology, 122, 611–623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naragon-Gainey K, McMahon TP, & Chacko TP (2017). The structure of common emotion regulation strategies: A meta-analytic examination. Psychological Bulletin, 143, 384–427. [DOI] [PubMed] [Google Scholar]
- Naragon-Gainey K, & Watson D (2014). Consensually-defined facets of personality as prospective predictors of change in depression symptoms. Assessment, 21, 387–403. [DOI] [PubMed] [Google Scholar]
- Naragon-Gainey K, & Watson D (2018). What lies beyond neuroticism? An examination of the unique contributions of social-cognitive vulnerabilities to internalizing disorders. Assessment, 25, 143–158. [DOI] [PubMed] [Google Scholar]
- Naragon-Gainey K, & Watson D (in press). Positive affectivity: The disposition to experience positive emotional states. In Snyder CR, Lopez SJ, Edwards LM, & Marques SC (Eds.), Oxford Handbook of Positive Psychology, 3rd Ed. New York, NY: Oxford Press. [Google Scholar]
- Naragon-Gainey K, Watson D, & Markon KE (2009). Differential relations of depression and social anxiety symptoms to the facets of extraversion/positive emotionality. Journal of Abnormal Psychology, 118, 299–310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nisbett R, & Wilson T (1977). Telling more than we can know: Verbal reports on mental processes. Psychological Review, 84, 231–259. [Google Scholar]
- Nicholls JG, Licht BG, & Pearl RA (1982). Some dangers of using personality questionnaires to study personality. Psychological Bulletin, 92(3), 572–580. [Google Scholar]
- Nolen-Hoeksema S, & Watkins ER (2011). A heuristic for developing transdiagnostic models of psychopathology: Explaining multifinality and divergent trajectories. Perspectives on Psychological Science, 6(6), 589–609. [DOI] [PubMed] [Google Scholar]
- Norr AM, Oglesby ME, Capron DW, Raines AM, Korte KJ, & Schmidt NB (2013). Evaluating the unique contribution of intolerance of uncertainty relative to other cognitive vulnerability factors in anxiety psychopathology. Journal of Affective Disorders, 151(1), 136–142. [DOI] [PubMed] [Google Scholar]
- O’Connor EJ, Staiger PK, Kambouropoulos N, & Smillie LD (2014). Pathways to social anxiety: The role of reinforcement sensitivities and emotion regulation. Psychiatry Research, 220(3), 915–920. [DOI] [PubMed] [Google Scholar]
- Olatunji BO, Naragon-Gainey K, & Wolitzky-Taylor KB (2013). Specificity of rumination in anxiety and depression: a multimodal meta-analysis. Clinical Psychology: Science and Practice, 20, 225–257. [Google Scholar]
- Ormel J, Jeronimus BF, Kotov K, Riese H, Bos EH, Hankin B, Rosmalen JGM, & Oldehinkel AJ (2013). Neuroticism and common mental disorders: Meaning and utility of a complex relationship. Clinical Psychology Review, 33(5), 686–697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ormel J, Rosmalen J, & Farmer A (2004). Neuroticism: a non-informative marker of vulnerability to psychopathology. Social Psychiatry and Psychiatric Epidemiology, 39(11), 906–912. [DOI] [PubMed] [Google Scholar]
- Paulus DJ, Talkovsky AM, Heggeness LF, & Norton PJ (2015). Beyond negative affectivity: A hierarchical model of global and transdiagnostic vulnerabilities for emotional disorders. Cognitive Behaviour Therapy, 44(5), 389–405. [DOI] [PubMed] [Google Scholar]
- Park J, & Naragon-Gainey K (in press). Daily experiences of emotional clarity and their association with internalizing symptoms in naturalistic settings. Emotion [DOI] [PubMed]
- Prenoveau JM, Craske MG, Zinbarg RE, Mineka S, Rose RD, & Griffith JW (2011). Are anxiety and depression just as stable as personality during late adolescence? Results from a three-year longitudinal latent variable study. Journal of Abnormal Psychology, 120(4), 832–843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riese H, Ormel J, Aleman A, Servaas MN, & Jeronimus BF (2016). Don’t throw the baby out with the bathwater: Depressive traits are part and parcel of neuroticism. NeuroImage, 125, 1103. [DOI] [PubMed] [Google Scholar]
- Roche MJ, Jacobson NC, & Pincus AL (2016). Using repeated daily assessments to uncover oscillating patterns and temporally-dynamic triggers in structures of psychopathology: Applications to the DSM-5 alternative model of personality disorders. Journal of Abnormal Psychology, 125(8), 1090–1102. [DOI] [PubMed] [Google Scholar]
- Roth S, & Cohen LJ (1986). Approach, avoidance, and coping with stress. American Psychologist, 41(7), 813–819. [DOI] [PubMed] [Google Scholar]
- Russell JA, & Barrett LF (1999). Core affect, prototypical emotional episodes, and other things called emotion: Dissecting the elephant. Journal of Personality and Social Psychology, 76(5), 805–819. [DOI] [PubMed] [Google Scholar]
- Schenk HM, Bos EH, Slaets JJ, Jonge P, & Rosmalen JM (2017). Differential association between affect and somatic symptoms at the between-and within-individual level. British Journal of Health Psychology, 22(2), 270–280. [DOI] [PubMed] [Google Scholar]
- Schmidt NB, Norr AM, Allan NP, Raines AM, & Capron DW (2017). A randomized clinical trial targeting anxiety sensitivity for patients with suicidal ideation. Journal of Consulting and Clinical Psychology, 85(6), 596–610. [DOI] [PubMed] [Google Scholar]
- Seligowski AV, & Orcutt HK (2015). Examining the structure of emotion regulation: A factor-analytic approach. Journal of Clinical Psychology, 71(10), 1004–1022. [DOI] [PubMed] [Google Scholar]
- Shapero BG, Abramson LY, & Alloy LB (2016). Emotional reactivity and internalizing symptoms: Moderating role of emotion regulation. Cognitive Therapy and Research, 40(3), 328–340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheppes G, Suri G, & Gross JJ (2015). Emotion regulation and psychopathology. Annual Review of Clinical Psychology, 11, 379–405. doi:10.1146/annurev-clinpsy-032814-112739 [DOI] [PubMed] [Google Scholar]
- Short NA, Boffa JW, Clancy K, & Schmidt NB (2018). Effects of emotion regulation strategy use in response to stressors on PTSD symptoms: An ecological momentary assessment study. Journal of Affective Disorders, 230, 77–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spinhoven P, Elzinga BM, van Hemert AM, de Rooij M, & Penninx BW (2014). A longitudinal study of facets of extraversion in depression and social anxiety. Personality and Individual Differences, 71, 39–44. [Google Scholar]
- Stange JP, Hamilton JL, Fresco DM, & Alloy LB (2017). Perseverate or decenter? Differential effects of metacognition on the relationship between parasympathetic inflexibility and symptoms of depression in a multi-wave study. Behaviour Research and Therapy, 97, 123–133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stanton K, & Watson D (2015). Replicable facets of positive emotionality and their relations to psychopathology. Assessment, 22(6), 665–680. [DOI] [PubMed] [Google Scholar]
- Timpano KR, Raines AM, Shaw AM, Keough ME, & Schmidt NB (2016). Effects of a brief anxiety sensitivity reduction intervention on obsessive compulsive spectrum symptoms in a young adult sample. Journal of Psychiatric Research, 83, 8–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tull MT, Berghoff CR, Wheeless LE, Cohen RT, & Gratz KL (2018). PTSD symptom severity and emotion regulation strategy use during trauma cue exposure among patients with substance use disorders: Associations with negative affect, craving, and cortisol reactivity. Behavior Therapy, 49(1), 57–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vine V, & Aldao A (2014). Impaired emotional clarity and psychopathology: A transdiagnostic deficit with symptom-specific pathways through emotion regulation. Journal of Social and Clinical Psychology, 33(4), 319–342. [Google Scholar]
- Uliaszek AA, Hauner KKY, Zinbarg RE, Craske MG, Mineka S, Griffith JW, & Rose RD (2009). An examination of content overlap and disorder-specific predictions in the associations of neuroticism with anxiety and depression. Journal of Research in Personality, 43(5), 785–794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson D, & Clark LA (1992). On traits and temperament: General and specific factors of emotional experience and their relation to the five-factor model. Journal of Personality, 60(2), 441–476. [DOI] [PubMed] [Google Scholar]
- Watson D, & Clark LA (1999). The PANAS-X: Manual for the Positive and Negative Affect Schedule- Expanded Form Unpublished manuscript, University of Iowa, Iowa City, IA. [Google Scholar]
- Watson D, & Naragon-Gainey K (2010). On the specificity of positive emotional dysfunction in psychopathology: Evidence from the mood and anxiety disorders and schizophrenia/ schizotypy. Clinical Psychology Review, 30, 839–848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson D, & Naragon-Gainey K (2014). Personality, emotions, and the emotional disorders. Clinical Psychological Science, 2, 422–442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson D, O’Hara MW, Naragon-Gainey K, Koffel E, Chmielewski M, Kotov R, … Ruggero CJ (2012). Development and validation of new anxiety and bipolar symptom scales for an expanded version of the IDAS (the IDAS-II). Assessment, 19(4), 399–420. [DOI] [PubMed] [Google Scholar]
- Watson D, Stasik SM, Chmielewski M, & Naragon-Gainey K (2015). Development and validation of the Temperament and Affectivity Inventory. Assessment, 22, 540–560. [DOI] [PubMed] [Google Scholar]
- Watson D, Wiese D, Vaidya J, & Tellegen A (1999). The two general activation systems of affect: Structural findings, evolutionary considerations, and psychobiological evidence. Journal of Personality and Social Psychology, 76(5), 820–838. [Google Scholar]
- Zinbarg RE, Mineka S, Bobova L, Craske MG, Vrshek-Schallhorn S, Griffith JW, … Anand D (2016). Testing a hierarchical model of neuroticism and its cognitive facets: Latent structure and prospective prediction of first onsets of anxiety and unipolar mood disorders during 3 years in late adolescence. Clinical Psychological Science, 4(5), 805–824. [Google Scholar]