Abstract
Acupuncture is widely used for improving poststroke care. Knowing the condition of meridian can help traditional Chinese medicine (TCM) doctors make a tailored choice of acupoints for every patient. The establishment of an objective meridian energy measurement for acute ischemic stroke that can be used for future acupuncture treatment and research is an important area in stroke-assisted therapy. In this study, a total of 102 subjects diagnosed with acute ischemic stroke within 7 days of onset were recruited, and the meridian energy analysis device (MEAD) was used to record the meridian electrical conductance (MEC) values of twelve meridians on unaffected and affected limbs. We found that the MEC value of the twelve meridians on the affected limbs was significantly higher than that on the unaffected limbs (P=0.001). Compared with the unaffected limbs, there was a higher value of MEC on the affected limbs of the lung meridian, heart meridian, pericardium meridian, and small intestine meridian, with significant differences (P < 0.05, P < 0.001, P < 0.001, and P < 0.05, respectively). Further analysis revealed that the MEC values of both Yin and Yang meridians of the affected limbs were significantly higher than those of the unaffected limbs (P=0.001 and P < 0.05, respectively). Meanwhile, the mean of the index of sympathovagal balance in patients with acute ischemic stroke (5.49 ± 4.21) was higher than the normal range (1–1.5), indicating autonomic imbalance. The results of this study are consistent with TCM theory as well as clinical observation and pathological mechanisms, suggesting that the measurement of MEC values may be used as a supplementary diagnostic method for acupuncture in patients with acute ischemic stroke.
1. Introduction
The global incidence of stroke is 258 per 100,000 people per year, and it is estimated that approximately 16.9 million patients suffer from this disease each year [1]. Stroke is the 3rd leading cause of death, with a 7.2% mortality rate and long-term disability in Taiwan, and it results in an expenditure of 475 million dollars annually on Taiwan hospital health-care resources [2]. Stroke is categorized into ischemic stroke and hemorrhagic stroke. There is a higher incidence of ischemic than hemorrhagic stroke, accounting for approximately 74% of stroke patients in Taiwan [3]. Stroke causes disability sequelae such as hemiplegia, aphasia, and dysphagia. Clinically, in addition to conventional Western medicine treatment, acupuncture is widely used in the adjuvant treatment of subacute stroke and stroke sequelae. The reduced stroke recurrence rate is also observed in ischemic stroke patients with acupuncture treatment form Taiwan National Health Insurance Research Database [4]. However, the application of acupuncture in the acute phase of stroke is relatively rare in clinical practice [5].
In TCM theory, the etiology of stroke is classified into “Blood stasis,” “Wind,” “Phlegm,” “Qi deficiency,” “Fire-heat,” and “Yin deficiency with Yang hyperactivity” [6]. All of these etiologies can cause the change of meridian energy in different degrees, which is the therapeutic target of acupuncture [7]. It is known that acupuncture can dredge the disturbance of Yin and Yang and balance the energy of meridians, which involves the modulation of autonomic imbalance [8, 9]. TCM doctors tend to choose different treatment in accordance with the patient's individuality. It is important to know the condition of the meridians, which may indicate the choice of acupoints [7, 10, 11]. The excess and deficiency of meridians may change the treatment strategy of acupuncture [12]. Therefore, understanding the condition of the meridians in patients with acute ischemic stroke can provide a basis for clinical acupuncture treatment.
The meridian energy analysis device (MEAD), developed by Dr. Yoshio in the 1950s [13], has become the main instrument for meridian diagnosis. The instrument is based on the Ryodoraku theory and the principle of electronic skin measurement [14]. The values of meridian electrical conductance (MEC) reflect the conditions of the related meridians and organs. Previous studies have revealed that there is higher electrical conductance and potential in acupoints than in the surrounding tissue [15–17], and there is greater electrodermal conduction in the meridians than in the nonmeridians [18]. MEAD has been widely used in meridian studies because it is noninvasive and low in cost and has high reproducibility and stability [19–21]. Many researchers have used MEAD to assess the physiological status, evaluate the effectiveness of the treatment, or conduct clinical trials of TCM treatment [12, 22–28]. In addition, MEAD has been used in the diagnosis of many diseases, such as gastroesophageal structural lesions, tennis elbow pain, low back pain, and obesity [21, 29–31].
Yu-Chih et al. found that patients with stroke sequelae have lower meridian electrical conductance (MEC) values compared with those in healthy people [32]. In recent years, there have been few studies on the meridian energy change in the acute phase of ischemic stroke. Since the condition of acute stroke is complicated and critical, the purpose of this study is to use MEAD to measure the meridian energy change in patients suffering from ischemic stroke within 7 days after onset in an attempt to determine the underlying rules to provide a reference for acupuncture treatment.
2. Materials and Methods
2.1. Study Design
The protocol was approved by the Human Ethics Committee of the study hospital (Chang Gung Medical Foundation Institutional Review Board no. 104-2081B) and was performed from 1 April 2015 to 9 January 2017. Written and oral informed consent was obtained from all participants at the beginning of the study.
2.2. Participants
The participants were recruited from the inpatients diagnosed with acute ischemic stroke in the Neurology Department at Chang Gung Memorial Hospital in Linkou, Taiwan, and all met the inclusion and exclusion criteria described below.
2.2.1. Inclusion Criteria
Diagnosis of acute ischemic stroke based on the clinical manifestations and CT or MRI
Onset of stroke within 7 days
No complications involving other major organs (heart, liver, kidney, and lung)
First-ever stroke or recurrent stroke with a Rankin scale score ≤1 before the current stroke
Willingness to receive MEAD measurements
2.2.2. Exclusion Criteria
Complications of sepsis or other infections
Consciousness unclear or impaired cognition
Pacemaker implanted
Pregnant
Bilateral limb weakness or normal muscle power in four limbs
2.3. Measures
The TCM doctors who participated in this study all obtained TCM medical licenses and received short-term training in the use of the meridian energy analysis device (MEAD, ME-PRO 6.1.1, Medpex Enterprises, Taiwan).
The participants were asked to remove all metal materials and lie flat and rest for at least 10 minutes before the assessment. Starting with MEAD, one metal cylinder with a clip was held in the left hand of the participant, and a pressure sensitive examination rod moistened with 3% saline was applied sequentially to 24 acupoints in the 12 left meridians and the 12 right meridians (Supplementary Figure 1 and Supplementary Table 1). The MEC values of each acupoint were recorded automatically by MEAD. We defined the limbs with hemiparesis as the affected limbs and the healthy limbs with normal muscle power as the unaffected limbs.
The twelve meridians are symmetrically distributed on both the left side and right side of the body, and each meridian was divided into the Yin meridian or Yang meridian on the basis of its distribution. There are six Yin meridians distributed on the inner region of the limbs, chest, and abdomen, while there are six Yang meridians distributed on the outside region of the limbs, head, and trunk. According to the location of the meridians in the upper or lower limbs, these six Yin and Yang meridians are further subdivided into three Yin meridians of the arm (heart, lung, and pericardium), three Yang meridians of the arm (small Intestine, large Intestine, and triple energizer), three Yin meridians of the leg (liver, kidney, and spleen), and three Yang meridians of the leg (bladder, gallbladder, and stomach) (Supplementary Figure 2).
For MEAD analysis on the basis of the manufacturer's protocol, the index of sympathovagal balance is defined as the ratio of the highest average MEC value of the dorsal or ventral side of four limbs to the lowest average MEC value, which fits the subgroups of three Yin meridians of the arm, three Yang meridians of the arm, three Yin meridians of the leg, and three Yang meridians of the leg (a total of 8 subgroups because both left side and right side are included). This index is calculated automatically by the device and is normally between 1.0 and 1.5. If it is not within this range, there may be autonomic imbalance.
2.4. Statistical Analysis
The statistical analysis was performed using SPSS software version 20.0 (IBM, Armonk, NY, USA). Demographic data, including sex, age, personal history, and past medical history, were analyzed by descriptive statistics expressed as the mean ± standard deviation or n (%). The MEC values of each meridian were expressed as the mean ± standard deviation. A paired sample t-test was used to compare the mean MEC values of unaffected limbs and affected limbs. When the P value was less than 0.05, the result was considered statistically significant.
3. Result
3.1. Patient Characteristics
From April 1, 2015, to January 9, 2017, 1087 participants suffered from acute ischemic stroke within 7 days after onset and were assessed for eligibility. After screening, 129 inpatients met the inclusion and exclusion criteria, and their meridian energy changes were measured using MEAD. 27 participants were excluded due to bilateral limb weakness or normal muscle power in four limbs. A total of 102 subjects were included in the statistical analysis, including 59 males and 47 females, with an average age of 65 years. The study flow chart is presented in Figure 1. Other characteristics, such as personal history, past medical history, and the condition of affected limbs, are shown in Table 1.
Figure 1.
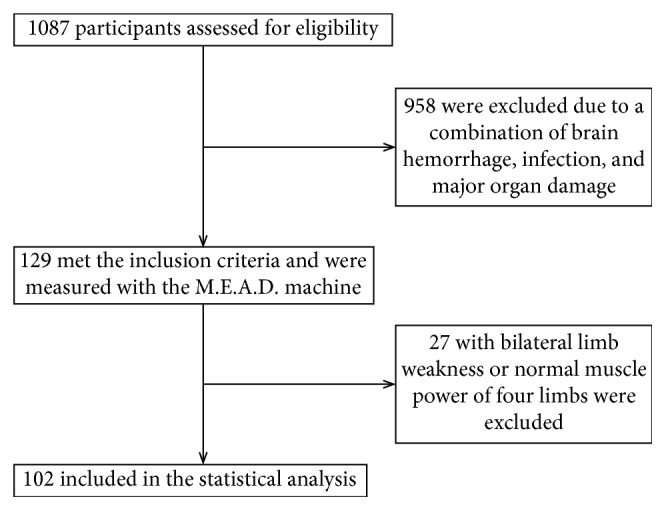
Flow chart of patients included for statistical analysis.
Table 1.
Participant characteristics.
| Characteristic | Value |
|---|---|
| Age (y) | 65.38 ± 12.62 |
| Sex | |
| Male, n (%) | 59 (55.9) |
| Female, n (%) | 47 (44.1) |
| Personal history | |
| Smoke, n (%) | 36 (35.3%) |
| Alcohol, n (%) | 20 (19.6%) |
| Medical history | |
| Hypertension, n (%) | 72 (70.6) |
| Diabetes mellitus, n (%) | 42 (41.2) |
| Hyperlipidemia, n (%) | 36 (35.3) |
| Arrhythmia, n (%) | 17 (16.7) |
| Affected limbs | |
| Upper limbs, n (%) | 14 (13.7%) |
| Lower limbs, n (%) | 6 (5.9%) |
| Both upper and lower limbs, n (%) | 82 (80.4%) |
3.2. Primary Outcome
The MEC values of twelve meridians of 102 participants were measured by MEAD. The analysis results of the MEC values are listed in Table 2. The index of sympathovagal balance calculated from these values was 5.49 ± 4.21, indicating that patients with acute ischemic stroke were in a state of autonomic imbalance. The MEC values of the four meridians of the affected limbs were significantly higher than those of the unaffected limbs, including lung meridian (33.43 ± 27.96 vs 28.86 ± 23.97), pericardium meridian (32.50 ± 25.42 vs 27.33 ± 22.52), heart meridian (24.79 ± 21.47 vs 18.91 ± 17.15), and small intestine meridian (26.82 ± 25.12 vs 18.91 ± 17.15) and showed significant differences (P < 0.05, P < 0.001, P < 0.001 and P < 0.05, respectively) (Table 2).
Table 2.
Comparison of unaffected and affected limbs of each meridian electrical conductance values.
| Meridian | Unaffected limbs (μA, mean ± SD) | Affected limbs (μA, mean ± SD) | P value |
|---|---|---|---|
| Lung | 28.86 ± 23.97 | 33.43 ± 27.96 | 0.009∗ |
| Pericardium | 27.33 ± 22.52 | 32.50 ± 25.42 | <0.001∗∗ |
| Heart | 18.91 ± 17.15 | 24.79 ± 21.47 | <0.001∗∗ |
| Small intestine | 22.94 ± 23.82 | 26.82 ± 25.12 | 0.03∗ |
| Triple energizer | 25.24 ± 23.09 | 28.54 ± 26.67 | 0.09 |
| Large intestine | 26.36 ± 24.63 | 30.11 ± 26.28 | 0.67 |
| Spleen | 19.90 ± 20.85 | 20.77 ± 21.32 | 0.24 |
| Liver | 17.06 ± 18.58 | 16.13 ± 18.83 | 0.33 |
| Kidney | 16.16 ± 19.66 | 16.03 ± 17.98 | 0.93 |
| Bladder | 16.66 ± 17.53 | 18.27 ± 19.51 | 0.15 |
| Gall bladder | 11.74 ± 13.69 | 11.18 ± 13.74 | 0.56 |
| Stomach | 15.64 ± 16.84 | 15.89 ± 18.08 | 0.83 |
∗ P < 0.05; ∗∗ P < 0.001.
3.3. Secondary Outcome
TCM doctors tend to choose specific acupoints for poststroke treatment on the basis of different acupuncture faction and theory. A study revealed the acupoints of Yang meridians were applied more frequent than those of Yin meridian [33]. Therefore, the condition of Yin and Yang meridians between unaffected and affected limbs was further analyzed. First, we compared the MEC values of the twelve meridians of the affected and unaffected limbs and found that the MEC values of the twelve meridians of the affected limbs were higher than those of the unaffected limbs (P=0.001). Second, we divided the twelve meridians into Yin meridians and Yang meridians for analysis, and we observed that the MEC values of Yin or Yang meridians of the affected limbs were significantly higher than those of the unaffected limbs (P=0.001 and P=0.02, respectively). Third, we subdivided the Yin and Yang meridians into the Yin meridians of the arm, Yang meridians of the arm, Yin meridians of the leg, and Yang meridians of the leg for analysis. We found that the MEC values of Yin or Yang meridians of the affected arm were significantly higher than those of the unaffected arm (P=0.001 and P=0.01, respectively), but there was no statistically significant difference in the MEC values of Yin or Yang meridians of the affected leg (P=0.93, P=0.57, respectively) (Table 3).
Table 3.
Comparison of unaffected and affected limbs of classified meridian electrical conductance values.
| Meridian | Unaffected side (μA, mean ± SD) | Affected side (μA, mean ± SD) | P value |
|---|---|---|---|
| Twelve meridians | 20.57 ± 15.35 | 22.87 ± 17.57 | <0.001∗∗ |
| Yin meridians | 21.37 ± 16.28 | 23.94 ± 18.59 | <0.001∗∗ |
| Yang meridians | 19.77 ± 15.53 | 21.80 ± 17.56 | 0.02∗ |
| Yin meridians of arm | 25.03 ± 19.86 | 30.24 ± 23.55 | <0.001∗∗ |
| Yang meridians of arm | 24.85 ± 20.74 | 28.49 ± 23.89 | 0.01∗ |
| Yin meridians of leg | 17.71 ± 16.31 | 17.64 ± 16.58 | 0.93 |
| Yang meridians of leg | 14.68 ± 13.68 | 15.11 ± 14.36 | 0.57 |
∗ P < 0.05 and ∗∗ P < 0.001.
4. Discussion
We found significant differences in the MEC values between the unaffected and affected sides of patients with acute ischemic stroke. Some interference factors, such as age, sex, underlying disease, body fat, weather, and humidity, may affect the MEC values [12, 27, 28, 34–36]. Xie measured the MEC values of twelve meridians of healthy people, and the results showed that the MEC values of males were higher than those of females [37]. Li discovered that the MEC values were statistically higher in the afternoon than in the morning [20]. On the other hand, it was found that every individual's MEC values had a fixed pattern with a relatively high reappearance rate [19], and there was no statistically significant difference in MEC values between the right and left sides in healthy people [37]. Therefore, instead of using the control group for analysis, we compared the MEC values of the unaffected and affected sides of the same patient to avoid these interference factors and to ensure the stability of the experiment.
Yu-Chih et al. investigated the changes in the MEC values of 82 stroke patients with a sequela of hemiplegia in Taiwan from 1993 to 1996 and found that there was no statistically significant difference in the MEC values between the unaffected and affected limbs [32, 38]. However, the inclusion criteria of the participants in these studies were different from ours in that they comprised a variety of different time courses (from 3 days to 13 years) and types (hemorrhagic and ischemic) of stroke. Because the pathophysiological processes of ischemic and hemorrhagic stroke were dissimilar and the disease condition changed over time, the results of these studies were different [39–41]. Therefore, we selected only patients with ischemic stroke in the acute stage (within 7 days of onset) to minimize the bias of patients' characteristics.
Lin et al. showed that the MEC value of the bladder meridian of the affected side was higher than that of the unaffected side and that the index of sympathovagal balance was high in the patient with acute renal colic [42]. After one month of treatment, the MEC value of the bladder meridian of the affected side decreased to a level similar to that of the unaffected side, with an improvement in sympathovagal balance. Another prospective study of acute renal colic also reported that patients with a ureteral calculus had a higher index of sympathovagal balance than that of the control group, which represented autonomic imbalance [43]. In our study, the MEC values of the affected limbs were significantly higher than those of the unaffected limbs (P=0.001), while the mean of the index of sympathovagal balance of patients with acute ischemic stroke (5.49 ± 4.21) was higher than the normal range (1–1.5). As a consequence, we proposed that patients with acute ischemic stroke tend to have higher MEC values on the affected side and autonomic imbalance.
There are 27 patients excluded by bilateral limb weakness or normal muscle power of four limbs. One was found to develop brain abscess and 8 were disclosed that no new-onset stroke by the final MRI report. There is only one stroke patient with bilateral limb weakness, and there are 18 stroke patients with normal muscle power. Hence, we also analyzed the MEC values of twelve meridians of these 18 subjects, and there is no significant difference between right and left limbs (Table 4), but the index of sympathovagal balance remained high (4.20 ± 2.20), indicating that, to some degree, patients suffering from acute ischemic stroke have autonomic imbalance regardless of the involvement of limb weakness.
Table 4.
Comparison of left and right limbs of each meridian electrical conductance in patients with normal muscle power.
| Meridian | Left limbs | Right limbs | P value |
|---|---|---|---|
| Lung | 22.36 ± 24.07 | 22.63 ± 27.25 | 0.93 |
| Pericardium | 21.96 ± 20.77 | 22.90 ± 24.41 | 0.61 |
| Heart | 15.16 ± 15.93 | 16.29 ± 20.58 | 0.55 |
| Small intestine | 21.19 ± 27.48 | 17.66 ± 19.92 | 0.39 |
| Triple energizer | 20.15 ± 26.96 | 19.83 ± 20.38 | 0.94 |
| Large intestine | 20.21 ± 24.13 | 19.50 ± 22.99 | 0.72 |
| Spleen | 20.92 ± 22.88 | 23.85 ± 24.37 | 0.06 |
| Liver | 12.95 ± 15.17 | 13.18 ± 14.47 | 0.95 |
| Kidney | 11.13 ± 13.90 | 20.45 ± 26.17 | 0.11 |
| Bladder | 17.28 ± 23.30 | 16.66 ± 21.76 | 0.80 |
| Gall bladder | 8.52 ± 11.44 | 8.29 ± 10.83 | 0.89 |
| Stomach | 13.74 ± 18.61 | 14.43 ± 13.93 | 0.88 |
Researchers have observed that patients with acute ischemic stroke had impaired autonomic function, and the mechanism is still not fully understood [44]. It has also been found that the increased sympathetic activity after acute ischemic stroke was associated with poor prognosis [45, 46]. The hyperactivity of the sympathetic nervous system causes sweat gland secretions, which in turn increases skin conductance. Accordingly, MEAD was used to measure the MEC values at acupoints to assess peripheral autonomic function [38]. We also found a high autonomic imbalance rate in this study (101 of 102 patients, 99.02%).
On the basis of meridian and collateral theory, the body forms a system where Qi and blood circulate through the meridians and collaterals connecting to the viscera, extremities, and superficial organs and tissues [47]. Using MEAD measurements at acupoints can reflect excessive or insufficient meridians [48]. Acupuncture is a treatment method that harmonizes Qi and blood and balances excess and deficiency of meridians as well as Yin and Yang. The therapeutic effect of acupuncture is known as the involvement of autonomic regulation [8, 9]. In other words, acupuncture can modulate the imbalance of parasympathetic and sympathetic activities. Our study discovered that patients with acute ischemic stroke have a relatively high index of sympathovagal balance, which could be selected as a parameter for assessing the efficacy of acupuncture in future studies.
TCM emphasizes that the treatment should be based on the syndrome differentiation. According to the eight principles (Yin, Yang, exterior, interior, cold, heat, deficiency, and excess), syndrome differentiation is used to analyze and distinguish pathological conditions, which is an important component of TCM diagnostics. The vital Qi of the body and the virulence of the pathogenic factors can be determined using the syndrome differentiation of deficiency and excess. In general, the deficiency syndrome refers to the syndrome with deficiency of vital Qi, and the excess syndrome is manifested by exuberant pathogens [49]. Under the principle of diagnosis, most patients with acute stroke represent excess syndrome, while patients with chronic stroke represent mainly deficiency syndrome. A previous study enrolled 253 acute ischemic stroke inpatients (onset within 48 to 72 hours) to analyze TCM syndromes and found that wind, phlegm, and blood stagnation syndromes were the major pathological mechanisms underlying acute ischemic stroke [50]. The wind, phlegm, and blood stagnation syndromes were all classified as excess syndrome. Our study discovered that patients with acute ischemic stroke had higher MEC values in their affected limbs, indicating excessive conditions of the affected limbs. This finding was also consistent with the pathological condition of TCM syndromes.
It is well known that Qi and blood are closely related in TCM theory: “Qi is the commander of blood, and blood is the mother of Qi.” This means that Qi is the motive force of blood, while blood carries Qi and provides nutrients for its movement. The concept of “heart” in TCM controls blood circulation, and “lung” dominates Qi as well as governs Qi diffusion [47]. Tsai discovered that the most common syndrome in acute ischemic stroke was blood stasis (98.4%) [50], indicating that the blood circulation of patients with acute ischemic stroke was blocked. Our study found significant imbalances between the affected and unaffected limbs, particularly in the lung, heart, and pericardium meridians (P < 0.05, P < 0.001, and P < 0.001, respectively). This result provides evidence of close linkages between TCM theory, clinical observation, and pathological mechanisms underlying acute ischemic stroke.
According to our clinical practices, most stroke patients who received acupuncture therapy in the chronic stage had sequela of either flaccid or spastic paralysis. On the basis of TCM theory, because of “treating flaccid paralysis by Yang Ming alone” [51] and “the liver governs the body's sinews,” there is a tendency to choose acupoints of the stomach or liver meridian at first [47]. A study revealed the acupoints of Yang meridians were the major components of the acupuncture prescription for stroke sequelae management (74.7%), with more frequent choice of acupoints in lower limbs (28.1%) than that in upper limbs (22.1%) [33], but our study found the MEC values of both Yin and Yang meridians of the affected arm to be significantly higher than those of the unaffected arm. There was no statistically significant difference in the MEC values of Yin or Yang meridians of the affected leg.
Compared with Huang's research [32, 38], we found that the MEC values of patients with stroke in the acute and chronic stages were different, suggesting that the energy status of meridians in patients with stroke changed with the disease course. Therefore, we believe that acupuncture therapy for stroke patients should be adjusted based on the stage of stroke, and the MEC values may provide us with a reference for the meridian status. In addition, the MEC values of acupoints of the lung, heart, and pericardium meridians may be considered first for acute ischemic stroke. Moreover, due to the significant excess of the affected side meridians, particularly the Yin meridian, an additional strategy using acupuncture to balance the affected and unaffected limbs should also be evaluated.
5. Conclusion
We performed MEAD analyses of 102 patients with acute ischemic stroke and found that the MEC values of the affected limbs were higher than those of the unaffected limbs, especially in the lung, heart, and pericardium meridians. In addition, the MEC values of both Yin and Yang meridians of the affected arm were significantly higher than those of the unaffected arm. These patients also had a relatively high index of sympathovagal balance. The results reveal the linkages between the TCM theory, clinical observation, and pathological mechanism underlying acute ischemic stroke and provide a clinical strategy for acupuncture therapy of acute ischemic stroke.
Acknowledgments
The study was supported by the Chang Gung Memorial Hospital under the Medical Research Project (contract no. CMRPG 5G004).
Abbreviations
- MEAD:
Meridian energy analysis device
- MEC:
Meridian electrical conductance
- TCM:
Traditional Chinese medicine.
Data Availability
The data used to support the findings of this study are included within the article.
Ethical Approval
The study was approved by the Human Ethics Committee of Chang Gung Medical Foundation Institutional Review Board (no. 104-2081B)
Consent
Informed consent was provided by all participants.
Conflicts of Interest
The authors declare that they have no conflicts of interest.
Authors' Contributions
All authors contributed to the study concept and design. Shih-An Chang and Yi-Xiang Weng contributed to the data collection, statistical analysis, interpretation of the data, literature review, and writing initial drafts. Shih-An Chang, Yi-Xiang Weng, Shu-Chen Cheng, and Chung-Yuan Hsu contributed to later drafts. Chung-Yuan Hsu provided administrative support and supervised the study. All authors revised the text for intellectual content and have read and approved the final version of the manuscript. Shih-An Chang and Yi-Xiang Weng contributed equally to this article.
Supplementary Materials
Supplementary Figure 1: the acupoints used in the measurement of MEC values shown are the locations of acupoints that are used in the measurement of MEC values, including LU-9 = Taiyuan (lung); PC-7 = Daling (pericardium); HT-7 = Shenmen (heart); SI-5 = Yanggu (small intestine); SJ-4 = Yangchi (triple energizer); LI-5 = Yangxi (Large Intestine); SP-3 = Taibai (spleen); LR-3 = Taichong (liver); KI-4 = Dazhong (kidney); BL-65 = Shugu (bladder); GB-40 = Qiuxu (gallbladder); and ST-42 = Chongyang (stomach). Supplementary Figure 2: the distribution of Yin and Yang meridians of the arm and leg. (a) The Yin meridians of the arm are distributed on the inner region of the upper limb (heart, lung, and pericardium). (b) The Yang meridians of the arm are distributed on the outside region of the upper limb (small intestine, large intestine, and triple energizer). (c) Yin meridians of the leg are located in the inner region of the lower limb (liver, kidney, and spleen), and Yang meridians of the leg are located in the outer region of the lower limb (bladder, gallbladder, and stomach). The short dash line represents the yin meridians, and the continuous line represents the yang meridians. Supplementary Table 1: the acupoints used in the measurement of MEC Values.
References
- 1.Feigin V. L., Forouzanfar M. H., Krishnamurthi R., et al. Global and regional burden of stroke during 1990–2010: findings from the global burden of disease study 2010. The Lancet. 2014;383(9913):245–255. doi: 10.1016/s0140-6736(13)61953-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hsieh F.-I., Chiou H.-Y. Stroke: morbidity, risk factors, and care in Taiwan. Journal of Stroke. 2014;16(2):59–64. doi: 10.5853/jos.2014.16.2.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lai E. C.-C., Man K. K. C., Chaiyakunapruk N., et al. Brief report. Epidemiology. 2015;26(6):815–820. doi: 10.1097/ede.0000000000000325. [DOI] [PubMed] [Google Scholar]
- 4.Shih C.-C., Liao C.-C., Sun M.-F., et al. A retrospective cohort study comparing stroke recurrence rate in ischemic stroke patients with and without acupuncture treatment. Medicine. 2015;94(39):p. e1572. doi: 10.1097/md.0000000000001572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Xu M., Li D., Zhang S. Acupuncture for acute stroke. Cochrane Database of Systematic Reviews. 2018;3 doi: 10.1002/14651858.cd003317.pub3.CD003317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cheng S.-C., Lin C.-H., Chang Y.-J., et al. Fire-heat and qi deficiency syndromes as predictors of short-term prognosis of acute ischemic stroke. The Journal of Alternative and Complementary Medicine. 2013;19(8):721–728. doi: 10.1089/acm.2012.0546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhou W., Luo L., Cao L., et al. Clinical study for stroke treated with meridian-collateral diagnosis and therapy by WANG Juyi. Zhongguo Zhen Jiu. 2016;36(10):1023–1026. doi: 10.13703/j.0255-2930.2016.10.005. [DOI] [PubMed] [Google Scholar]
- 8.Beissner F., Deichmann R., Henke C., Bär K.-J. Acupuncture—deep pain with an autonomic dimension? Neuroimage. 2012;60(1):653–660. doi: 10.1016/j.neuroimage.2011.12.045. [DOI] [PubMed] [Google Scholar]
- 9.Stener-Victorin E., Jedel E., Janson P. O., Sverrisdottir Y. B. Low-frequency electroacupuncture and physical exercise decrease high muscle sympathetic nerve activity in polycystic ovary syndrome. American Journal of Physiology-Regulatory, Integrative and Comparative Physiology. 2009;297(2):R387–R395. doi: 10.1152/ajpregu.00197.2009. [DOI] [PubMed] [Google Scholar]
- 10.Xia W., Zheng C., Xia J., Zhang Y. Post-stroke dysphagia treated with acupuncture of meridian differentiation:a randomized controlled trial. Zhongguo Zhen Jiu. 2016;36(7):673–678. doi: 10.13703/j.0255-2930.2016.07.001. [DOI] [PubMed] [Google Scholar]
- 11.Zhou W., Benharash P. Effects and mechanisms of acupuncture based on the principle of meridians. Journal of Acupuncture and Meridian Studies. 2014;7(4):190–193. doi: 10.1016/j.jams.2014.02.007. [DOI] [PubMed] [Google Scholar]
- 12.Lin M. L., Wu H.-C., Hsieh Y.-H., et al. Evaluation of the effect of laser acupuncture and cupping with ryodoraku and visual analog scale on low back pain. Evidence-Based Complementary and Alternative Medicine. 2012;2012:7. doi: 10.1155/2012/521612.521612 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yoshio N. Skin electric resistance and ryodoraku. Journal of the Autonomic Nervous System. 1956;6:p. 52. [Google Scholar]
- 14.Sancier K. M. Electrodermal measurements for monitoring the effects of a qigong workshop. The Journal of Alternative and Complementary Medicine. 2003;9(2):235–241. doi: 10.1089/10755530360623347. [DOI] [PubMed] [Google Scholar]
- 15.Ahn A. C., Martinsen Ø. G. Electrical characterization of acupuncture points: technical issues and challenges. The Journal of Alternative and Complementary Medicine. 2007;13(8):817–824. doi: 10.1089/acm.2007.7193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Reichmanis M., Marino A. A., Becker R. O. Electrical correlates of acupuncture points. IEEE Transactions on Biomedical Engineering. 1975;22(6):533–535. doi: 10.1109/tbme.1975.324477. [DOI] [PubMed] [Google Scholar]
- 17.Hyvärinen J., Karlsson M. Low-resistance skin points that may coincide with acupuncture loci. Medical Biology. 1977;55(2):88–94. [PubMed] [Google Scholar]
- 18.Lee M. S., Jeong S.-Y., Lee Y.-H., Jeong D.-M., Eo Y.-G., Ko S.-B. Differences in electrical conduction properties between meridians and non-meridians. The American Journal of Chinese Medicine. 2005;33(5):723–728. doi: 10.1142/s0192415x05003405. [DOI] [PubMed] [Google Scholar]
- 19.Yeh M.-H. Study of stability of the instrument analyzing electric resistance of acupuncture points. Taiwan Journal of Clinical Chinese Medicine. 2008;14(2) [Google Scholar]
- 20.Li Y.-H. Graduate Institute of Integrated Medicine. Taichung, Taiwan: China Medical University; 2006. Analysis on the change of ryodoraku values by time, age, or acupuncture, moxibustion, and ice stimulation on the zusanli acupoints. [Google Scholar]
- 21.Huang S. M., Chien L.-Y., Chang C.-C., Chen P.-H., Tai C.-J. Abnormal gastroscopy findings were related to lower meridian energy. Evidence-Based Complementary and Alternative Medicine. 2011;2011:7. doi: 10.1155/2011/878391.878391 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chien T.-J., Liu C.-Y., Ko P.-H., Hsu C.-H. A Chinese decoction, Kuan-Sin-Yin, improves autonomic function and cancer-related symptoms of metastatic colon cancer. Integrative Cancer Therapies. 2016;15(1):113–123. doi: 10.1177/1534735415617282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Huang S.-M., Chien L.-Y., Tai C.-J., Chen P.-H., Lien P.-J., Tai C.-J. Effects of symptoms and complementary and alternative medicine use on the yang deficiency pattern among breast cancer patients receiving chemotherapy. Complementary Therapies in Medicine. 2015;23(2):233–241. doi: 10.1016/j.ctim.2015.01.004. [DOI] [PubMed] [Google Scholar]
- 24.Chien L.-W., Chen F.-C., Hu H.-Y., Liu C.-F. Correlation of electrical conductance in meridian and autonomic nervous activity after auricular acupressure in middle-aged women. The Journal of Alternative and Complementary Medicine. 2014;20(8):635–641. doi: 10.1089/acm.2012.0900. [DOI] [PubMed] [Google Scholar]
- 25.Chang J.-S., Lin W.-Y., Liu H.-P. Acupuncture at SP6 point in lower extremities improved patients’ insomnia, which was also shown through ryodoraku electrical measurements. Acupuncture & Electro-Therapeutics Research. 2016;41(2):79–93. doi: 10.3727/036012916x14666839504550. [DOI] [PubMed] [Google Scholar]
- 26.Hsu C.-C., Weng C.-S., Liu T.-S., Tsai Y.-S., Chang Y.-H. Effects of electrical acupuncture on acupoint BL15 evaluated in terms of heart rate variability, pulse rate variability and skin conductance response. The American Journal of Chinese Medicine. 2006;34(1):23–36. doi: 10.1142/s0192415x06003606. [DOI] [PubMed] [Google Scholar]
- 27.Lin C.-H., Lee L.-S., Su L.-H., Huang T.-C., Liu C.-F. Thermal therapy in dialysis patients—a randomized trial. The American Journal of Chinese Medicine. 2011;39(5):839–851. doi: 10.1142/s0192415x1100924x. [DOI] [PubMed] [Google Scholar]
- 28.Chien T.-J., Liu C.-Y., Lu R.-H., Kuo C.-W., Lin Y.-C., Hsu C.-H. Therapeutic efficacy of traditional chinese medicine, “Kuan-Sin-Yin,” in patients undergoing chemotherapy for advanced colon cancer—a controlled trial. Complementary Therapies in Medicine. 2016;29:204–212. doi: 10.1016/j.ctim.2016.10.001. [DOI] [PubMed] [Google Scholar]
- 29.Weng C.-S., Hung Y.-L., Shyu L.-Y., Chang Y.-H. A study of electrical conductance of meridian in the obese during weight reduction. The American Journal of Chinese Medicine. 2004;32(3):417–425. doi: 10.1142/s0192415x04002077. [DOI] [PubMed] [Google Scholar]
- 30.Weng C.-S., Shu S.-H., Chen C.-C., Tsai Y.-S., Hu W.-C., Chang Y.-H. The evaluation of two modulated frequency modes of acupuncture-like tens on the treatment of tennis elbow pain. Biomedical Engineering: Applications, Basis and Communications. 2005;17(5):236–242. doi: 10.4015/s1016237205000354. [DOI] [Google Scholar]
- 31.Weng C.-S., Tsai Y.-S., Yang C.-Y. Using electrical conductance as the evaluation parameter of pain in patients with low back pain treated by acupuncture like tens. Biomedical Engineering: Applications, Basis and Communications. 2004;16(4):205–212. doi: 10.4015/s1016237204000281. [DOI] [Google Scholar]
- 32.Yu-Chih H., Chen W.-Z., Chang Y.-H., Chi-Mei H. Changes in ryodoraku values in stroke. Journal of Chinese Medicine. 1993;4(3):191–198. [Google Scholar]
- 33.Wu L. T., Li Y., Ren Y. L. Exploration on the characteristics of meridian points in the treatment of post-stroke disorder with acupuncture and moxibustion based on the data mining technology. Zhongguo Zhen Jiu. 2013;33(2):125–130. [PubMed] [Google Scholar]
- 34.Huang K.-F., Tang S.-T., Chuang C.-Y., Han W.-R., Lin J.-H., Young S.-T. Different patterns of dynamic variations on electrical conductances of acupoints between qi vacuity and qi non-vacuity after glucose ingestion. The Journal of Alternative and Complementary Medicine. 2011;17(9):843–849. doi: 10.1089/acm.2010.0528. [DOI] [PubMed] [Google Scholar]
- 35.Chen C. W., Tai C.-J., Choy C.-S., et al. Wave-induced flow in meridians demonstrated using photoluminescent bioceramic material on acupuncture points. Evidence-Based Complementary and Alternative Medicine. 2013;2013:11. doi: 10.1155/2013/739293.739293 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lin C. Y., Wei T.-T., Wang C.-C., Chen W.-C., Wang Y.-M., Tsai S.-Y. Acute physiological and psychological effects of qigong exercise in older practitioners. Evidence-Based Complementary and Alternative Medicine. 2018;2018:10. doi: 10.1155/2018/4960978.4960978 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Xie W.-X. Biomedical Engineering. Taoyuan City, Taiwan: Chung Yuan Christian University; 2003. Using ryodoraku device to evaluate the treatment effects of different frequency modes of electrical stimulation on muscular pains. [Google Scholar]
- 38.Yu-Chih H., Chang Y.-H., Wei-Zein C. Evaluation of ryodoraku value change with related factors in stroke. Journal of Chinese Medicine. 1996;7(2):95–100. [Google Scholar]
- 39.Adams H. P., Jr., Bendixen B. H., Kappelle L. J., et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in acute stroke treatment. Stroke. 1993;24(1):35–41. doi: 10.1161/01.str.24.1.35. [DOI] [PubMed] [Google Scholar]
- 40.Rannikmäe K., Woodfield R., Anderson C. S., et al. Reliability of intracerebral hemorrhage classification systems: a systematic review. International Journal of Stroke. 2016;11(6):626–636. doi: 10.1177/1747493016641962. [DOI] [PubMed] [Google Scholar]
- 41.Taylor R. A., Sansing L. H. Microglial responses after ischemic stroke and intracerebral hemorrhage. Clinical and Developmental Immunology. 2013;2013:10. doi: 10.1155/2013/746068.746068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lin W. C., Chen Y.-H., Xu J.-M., Chen D.-C., Chen W.-C., Lee C.-T. Application of skin electrical conductance of acupuncture meridians for ureteral calculus: a case report. Case Reports in Nephrology. 2011;2011:4. doi: 10.1155/2011/413532.413532 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lee C.-T., Chang Y.-H., Lin W.-Y., et al. Applications of meridian electrical conductance for renal colic: a prospective study. The Journal of Alternative and Complementary Medicine. 2010;16(8):861–866. doi: 10.1089/acm.2009.0273. [DOI] [PubMed] [Google Scholar]
- 44.Sykora M., Diedler J., Turcani P., Hacke W., Steiner T. Baroreflex: a new therapeutic target in human stroke? Stroke. 2009;40(12):e678–e682. doi: 10.1161/strokeaha.109.565838. [DOI] [PubMed] [Google Scholar]
- 45.Sander D., Winbeck K., Klingelhofer J., Etgen T., Conrad B. Prognostic relevance of pathological sympathetic activation after acute thromboembolic stroke. Neurology. 2001;57(5):833–838. doi: 10.1212/wnl.57.5.833. [DOI] [PubMed] [Google Scholar]
- 46.Colivicchi F., Bassi A., Santini M., Caltagirone C. Prognostic implications of right-sided insular damage, cardiac autonomic derangement, and arrhythmias after acute ischemic stroke. Stroke. 2005;36(8):1710–1715. doi: 10.1161/01.str.0000173400.19346.bd. [DOI] [PubMed] [Google Scholar]
- 47.World Health Organization. Regional Office for the Western Pacific. WHO International Standard Terminologies on Traditional Medicine in the Western Pacific Region. Geneva, Switzerland: World Health Organization; 2007. [Google Scholar]
- 48.Tsai M., Chen S., Lin C. Theoretical basis, application, reliability, and sample size estimates of a meridian energy analysis device for traditional Chinese medicine research. Clinics. 2017;72(4):254–257. doi: 10.6061/clinics/2017(04)10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Jiang M., Lu C., Zhang C., et al. Syndrome differentiation in modern research of traditional Chinese medicine. Journal of Ethnopharmacology. 2012;140(3):634–642. doi: 10.1016/j.jep.2012.01.033. [DOI] [PubMed] [Google Scholar]
- 50.Tsai F.-K. Analysis of TCM syndromes of ischemic stroke patients at acute stage. Journal of Chinese Medicine. 2011;22(1-2):95–105. [Google Scholar]
- 51.Ju S., Zong L. Discussion on acupuncture for flaccid paralysis from “treating flaccid paralysis by yangming alone”. Zhongguo Zhen Jiu. 2015;35(9):956–959. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Figure 1: the acupoints used in the measurement of MEC values shown are the locations of acupoints that are used in the measurement of MEC values, including LU-9 = Taiyuan (lung); PC-7 = Daling (pericardium); HT-7 = Shenmen (heart); SI-5 = Yanggu (small intestine); SJ-4 = Yangchi (triple energizer); LI-5 = Yangxi (Large Intestine); SP-3 = Taibai (spleen); LR-3 = Taichong (liver); KI-4 = Dazhong (kidney); BL-65 = Shugu (bladder); GB-40 = Qiuxu (gallbladder); and ST-42 = Chongyang (stomach). Supplementary Figure 2: the distribution of Yin and Yang meridians of the arm and leg. (a) The Yin meridians of the arm are distributed on the inner region of the upper limb (heart, lung, and pericardium). (b) The Yang meridians of the arm are distributed on the outside region of the upper limb (small intestine, large intestine, and triple energizer). (c) Yin meridians of the leg are located in the inner region of the lower limb (liver, kidney, and spleen), and Yang meridians of the leg are located in the outer region of the lower limb (bladder, gallbladder, and stomach). The short dash line represents the yin meridians, and the continuous line represents the yang meridians. Supplementary Table 1: the acupoints used in the measurement of MEC Values.
Data Availability Statement
The data used to support the findings of this study are included within the article.


