Abstract
Introduction:
Parkinson's disease (PD) is a chronic, progressive disorder that mainly affects the central nervous system and, consequently, the patient's functional status. This study aimed to compare the effect of 8-week rebound therapy-based exercise program and weight-supported exercises on the range of motion, proprioception, and the quality of life in patients with PD.
Methods:
Twenty patients were randomly divided into two equal groups of weight-bearing exercises and rebound exercise with no significant differences in age, weight, and height. The variables of the range of motion, proprioception, and the quality of life were assessed in pre- and posttest. Data were analyzed using repeated measure ANOVA and t-test at a significant level of P < 0.05.
Results:
All of the variables in the two groups were significantly improved after 8 weeks of exercise, whereas the improvement rate in the rebound therapy group was more than the weight-bearing exercises group in range of motion (134.60 ± 13.22 vs. 118.38 ± 12.48), proprioception (7.60 ± 3.22 vs. 10.38 ± 2.48), and the quality of life (147.60 ± 13.22 vs. 118.38 ± 12.48) of the patients (P < 0.001 for all variables).
Conclusions:
Given that both rebound and weight-supported exercises are effective on improving the range of motion, proprioception, and the quality of life of people with PD, it is recommended that the benefits of these exercises to be used in physical rehabilitation programs. However, rebound therapy exercises have had a greater effect on people with PD, and it seems better to use these exercises more than others.
Keywords: Parkinson's disease, proprioception, quality of life, range of motion, rebound exercises, weight-supported exercises
Introduction
Parkinson's disease (PD) is the second most common neurodegenerative disorder after Alzheimer's disease[1] and affecting approximately 7.5 million patients worldwide is a chronic disorder in the brain that affects body movement. Because of the aging population, this is expected to increase up to more than 9 million in 2030.[2] This disease is the result of the loss or weakening of or damage to the nerve cells, which produce dopamine in the midbrain or mesencephalon.[3] Reducing levels of dopamine leads to movement disorders in these patients.[4] Early clinical signs of PD start after the destruction of 80% of the dopamine-producing cells.[5] The cause of the disease is unknown, but it may be multifactorial. Nowadays, the primary treatment method for PD in different countries is the use of anti-Parkinson drugs such as levodopa, Madopar, and Selegiline. Unfortunately, the side effects of levodopa disappear over time and lead to the emergence of dyskinesia.[6] Moreover, most important side effects of other drugs include depression, weakness, and fatigue.[7] The most prominent psychosocial manifestations in people with PD are anxiety and depression because of physical symptoms, and constraints associated with them. Shaking, rigidity, slowness of movement, and difficulty with movements cause social isolation of patients,[6] and can affect the quality of life of them.
Exercise and physical activity are also used as complementary therapies in addition to drug therapy. The ability and functional status of patients with PD reduce with increasing age and decreased levels of physical activity.[4] It seems that exercise programs can be considered as an effective strategy to delay or reverse functional impairment in these patients. Weight-bearing exercise for better balance (WEBB) is considered as one of the comprehensive therapeutic programs, which its exercises can cover various aspects of motion control. The useful effects of this program have been observed on the quality of life and the risk of falling in the elderly and people with PD. Reyisi Dehkordi et al. concluded that body--weight-supported treadmill training (BWSTT) exercises can be more effective than conventional exercises in improving the sense and movement, as well as the quality and quantity of walking in people who have or had paraplegia.[8] Moreover, these exercises can be done at home easily, and no special and expensive equipment is needed. Lucareli et al. showed that the BWSTT exercises had better effects on walking in patients than common exercises and physiotherapy.[9] So far, no study has been conducted on people with PD directly. Different methods of physical rehabilitation such as sports exercises are considered as noninvasive therapy methods that in an active or inactive way allow the patient to stimulate and affect the affected area by engaging in movements.[1]
On the other hand, rebound exercises are considered as one of the effective rehabilitation exercises on functional status in past studies.[10,11,12,13,14,15] The rebound therapy exercises belong to a plyometric exercise group that includes jumping up and down, landing upon both feet of one foot, and various movements of the shoulders, arms, hands, trunk, thighs, knees, and legs.[10] Several studies are carried out on rebound therapy as an exercise, the main component of which is the rebounder (mini-trampoline or trampoline). In rehabilitation processes, rebound therapy is used in rehabilitation programs because rebound therapy is considered as a positive way to increase muscle strength, body balance, and mechanical capability of bones, as well as improving health levels and even improving injuries.[12] Smith et al. during a study concluded that improving equilibrium responses and facilitating movement were among benefits of these exercises.[13] In rebound exercises, more muscles are involved in maintaining body position in space and against gravity.[12] Investigating the effect of trampolining exercise program on students aged 7-11 years with developmental coordination disorder (DCD) also indicated that the use of trampolining could improve neuromuscular coordination.[15] BWSTT is widely used for rehabilitation and improving sense and motion in many neurological and orthopedic diseases. BWSTT activates the muscular nervous system below the level of damage, and leads to improve motor skills.[16]
This study aimed to compare the effect of 8-week rebound therapy-based exercise program and weight-supported exercises on the range of motion, proprioception, and the quality of life in patients with PD.
Methods
The present study was a cross-sectional quasi-experimental research with pre-/posttest design. From the patients with PD referred to the Alzahra Hospital in Isfahan City, Iran, 20 patients were selected using purposive and convenience sampling method. They were randomly divided into two equal research groups (n = 10) using Morgan table. In other words, this was a factorial clinical trial study with allocation ratio of 1:1.
With α = 0.05 and β = 0.2, the sample size was calculated as 10 for each group to have a statistical power of 0.8; using Cochran's formula, the sample size was calculated as 20 for the study which was in agreement with previous formula.
Inclusion criteria were as being a known case of PD in stages 2 or 3 according to Hoehn and Yahr scale,[17] being at the age of 20--50 years old, being at the onset stage of the disease (response to drugs), being at the moderate stage of the disease according to the Parkinson's disease rating scale (UPDRS),[18] and voluntary agreement of the patient to participate in the research.
Patients with any history of spinal or lower limb severe injury or surgery during last year, those with any skeletal deformity who were not able to do the exercises, those who were absent in more than 30% of sessions, and those who did not agree to participate the study were excluded from the study.
All the pre- and posttest clinical assessments were done by a unique neurologist who was blind to the study groups.
The Ethics Committee of the Deputy of Research of the University of Isfahan approved this study as a PhD thesis.
First, all subjects read the consent and signed it. They then became familiar with the test process. Demographic data of each subject were collected. All pretest and posttests were performed at the Corrective Exercise Laboratory of School of Physical Education, University of Isfahan.
The Biodex Isokinetic testing machine (Shirley, NY, USA) was used to examine the proprioception, torque, and lower extremity muscle strength. To investigate the time to peak torque, according to the age and condition of the PD, the acceleration time was assessed with a speed and angle that did not cause injury in participant. Validity and reliability of the machine was evaluated in previous studies ranging 0.86-0.95 using different studies.[19] Moreover, proprioception accuracy was measured through the active repositioning test for the nondominant joint. It has been proved to be a valid and reliable test for proprioception.[20,21]
The metal goniometer was used to measure the range of motion of the knee. For measurement with a goniometer, the optimal condition is that it is placed side by side or on the joint with little contact between the skin and the goniometer. The patient lies on back and flexes the thigh and knee and then extends the knee for measuring knee range of motion (KROM). To do this, the goniometer axis is placed on the outer epicondyle of the thigh, and the fixed arm is aligned with a large hip and moving arm is in line with the outer ankle. Then, the angle from flexion to extension is recorded.[19]
The Parkinson's disease questionnaire (PDQ39) was used as a standardized and validated questionnaire in scientific studies to investigate the quality of life of the people with PD.[22] Roshani et al. had made a valid and Persian reliable version of PDQ39,[23] which was used in this study. This questionnaire, as its name suggests, has 39 items, and should be completed by the patients. Filling out this questionnaire would take an average of 10 min. There are 39 questions in eight separate dimensions in the Persian version of the PDQ-39. These questions are divided into 8 dimension of: mobility (10 questions), activities of daily living (ADL, 6 questions), emotional well-being (6 questions), stigma (4 questions), social support (3 questions), cognition (4 questions), communication (3 questions), and bodily discomfort (3 questions). Each question in this questionnaire has five points on the Likert scale, where only one option is marked. The score for each question ranges from zero (0) to four (4): “never” = 0, “occasionally” = 1, “sometimes” = 2, “often” = 3, and “always” = 4. The final score is the result of the following equation: the sum of each question score divided by the result times 4 (the maximal score for each question), divided by the total number of questions. This result is multiplied times by 100. Each dimension score ranges from 0-100 in a linear scale, in which zero is the best and 100 the worst quality of life. Moreover, the mean score of all dimensions is considered as a single index called the Parkinson's Disease summary index (PDSI). PDSI varies between 0 and 100; again, 0 is the best and 100 the worst quality of life.
All the participants completed the PDQ39 before and 1 week after the end of the intervention.
In both groups, training protocol was done in 8 weeks, 3 sessions per week, and each session lasted 20-45 min, at the University of Isfahan. It should be noted that the whole period was led by the researchers, and training sessions were held individually.
The program for the first day was different with the rest of the sessions. On the first day, the instructor spoke to the subjects about the program, and how to do the exercises and its characteristics, and the subjects were asked to share their problems about the feeling of fatigue or not to have ability to do exercise or dealing with any other problem inside or between sessions with their instructor or researcher. It should be noted that because of sensory impairment of patients, the instructor can not only rely on the feeling of fatigue or not be well-being expressed by the subjects but also they should be monitored and the decisions of the exercises should be made according to their expression of the feeling and the observation of the movements. After 20 min of speaking, the subjects learned how to do it. The duration of each training session lasts from 20-45 min, which was divided into three parts:
Warm up: It lasted 20 min which the subject did it with the help of the instructor. This stage included stretching of the body and lower limb muscles
The aim of each session: It lasted 10--30 min and the main exercises related to each session were trained to the patients. These exercises were mostly done aimed at creating independence in the person for doing the movements. Besides, creating vitality and diversity in doing exercises was one of the important goals of the training program
Drop out: It lasted 5 min and in this stage the subject with the help of instructor did simple movement with low intensity.
Exercise intensity and duration
In the trampolining training (rebound exercise) group, with the progress of the training program, the movements were performed in pairs on the trampolining surface. Trampoline was designed and built in suitable size (3.30 in diameter and 70 cm in high) to make possible using it by people with PD easily to do the training prototype. The exercises in each session were selected by the researcher in such a way that, in addition to the attractiveness, it included movements that help improve the cardiovascular system, digestive system and excretion, balance, etc. Some tools such as ball, elastic band, bar, etc., were used to increase the variety of exercises. The intensity of the exercises was controlled by the polar system (Pulse oximetry). Moreover, fatigue, skin color, weakness, excessive sweating, and respiratory state were monitored by the researcher.
Speaking was used as a tool to understand exercise pressure in people in addition to the duration of workout and heart rate. Changing exercises from lying position to sitting and standing was another method for making changes in the exercises pressure. Moreover, conversation one-player exercise into two-layer exercises was another method to increase the intensity of exercise. Table 1 shows a summary of the training program considered in group. The selection of exercises and how to do them was expressed from simple to difficult. That was, in the initial sessions, the movements had less intensity, number, repetition, and time. Besides, patients performed the movements with more resting time.[11]
Table 1.
Training protocol for rebound exercise group
| Week | Warm up | The number of Sessions | Description of exercises | Drop out |
|---|---|---|---|---|
| 1 | 5-10 min | 1 to 3 | Familiarization stage: During the first 3 sessions, attended by all subjects, while the various stages of the exercises are reviewed, and the exercises are done, the level of ability of individuals to do exercises is also evaluated and recorded in order to be considered in the design of a specific training for each subject | 5-10 min |
| The first session is more lying, second session sitting, and third session standing | ||||
| The factors of time, intensity and volume are not prioritized, and depend on the individual’s ability and are arisen merely to be familiar with the matter | ||||
| 2 | 5-10 min | 1 to 3 | Lying Exercises (Supportive): Exercises in this week were done during 1 to 3 sessions in lying on the abdomen position and lateral position. During a training exercise, the instructor was always on the trampoline next to the subject | 5-10 min |
| The exercises began with standing positions, and continued with the motions of the instructor to the trampoline surface, which allowed him/her to move | ||||
| 3 | 5-10 min | 1 to 3 | Independent Laying Exercises: The first session in the lying on the back position, Abdominal muscle contraction when up and down movements of the body on the Trampoline. The second session: Sit-up (or curl-up) as long as possible and/or rolling to the side while holding the ball in hand. The third session: The subject was asked to move up and down in the above situation | 5-10 min |
| 4 | 5-10 min | 1 to 3 | Sitting exercises (Supportive): First session: Merely in sitting position with the ball or without the ball. The second session: Shaking creating intervention on the trampoline surface with or without the ball (balloon). The third session: More complicated stretching movements with or without vibration (intervention) by the instructor | 5-10 min |
| 5 | 5-10 min | 1 to 3 | Independent sitting exercises: At this stage, the fourth week exercises without support of the instructor were done. At the second and third session, the subject was asked to move up and down in a sitting position or play with a balloon | 5-10 min |
| 6 | 5-10 min | 1 to 3 | Standing exercises (Supportive): Throughout the exercises of this stage, the instructor is next to the subject. The first session: Just standing on foot and with open eyes. Second session: Standing on two feet and shaking creating by the instructor. Third session: Intervention with balloon | 5-10 min |
| 7 | 5-10 min | 1 to 3 | Independent Standing Exercises: 6-week exercises without supportive presence of the instructor | 5-10 min |
| 8 | 5-10 min | 1 to 3 | Combined exercises (advanced): All independent exercises: The first session: Moving up and down while walking. Second session: Playing with a balloon while walking. Third session: Drop training (sitting from the standing position and Standing up with a reactive force to the standing position) | 5-10 min |
In the treadmill training group, two factors of treadmill speed and weight-bearing percentage were controlled and modified by the researcher. The duration of exercise was another very important factor to control the exercise intensity. In this group, the program was designed for each participant individually, based on his ability and function because of the nature of the program. The exercises of the group began from standing and walking in a simple way and it continued also up to the running stage. The intensity of the exercises was controlled by the treadmill heart rate monitor. Moreover, fatigue, skin color, weakness, excessive sweating, and respiratory state of the patients were monitored by the researcher. Speaking during exercises was used as an effective way to understand exercise pressure in people in addition to the duration of exercise and heart rate. Table 2 shows a summary of the training program considered in group.[9]
Table 2.
Treadmill group training protocol with body weight supporting (BWS)
| Week | Warm up | Sessions number | Time | Load rate (Percentage of body weight) | Speed (km/h) | Drop out |
|---|---|---|---|---|---|---|
| 1 | 15 min | 1 to 3 | 10 min | 50 | 1-2 | 15 min |
| 2 | 15 min | 1 to 3 | 15 min | 50 | 2-3 | 15 min |
| 3 | 15 min | 1 to 3 | 15 min | 50 | 3-4 | 15 min |
| 4 | 15 min | 1 to 3 | 20 min | 75 | 4-5 | 15 min |
| 5 | 15 min | 1 to 3 | 20 min | 75 | 4-5 | 15 min |
| 6 | 15 min | 1 to 3 | 25 min | 75 | 5-6 | 15 min |
| 7 | 15 min | 1 to 3 | 25 min | 100 | 5-6 | 15 min |
| 8 | 15 min | 1 to 3 | 30 min | 100 | 6-7 | 15 min |
All the participants ended the study. SPSS software (version 22, IBM Corp., Armonk, NY, USA) was used to analyze the collected data. Shapiro--Wilk statistical test was used in order to investigate the normal distribution of data in two groups, and t-test and the repeated measures ANOVA were used to compare the variables in and between the groups at a significant level of less than 0.05.
Results
Twenty patients in two equal groups were enrolled in this study. The two study groups were not statistically different in age, height, and weight [Table 3].
Table 3.
Demographic data of the subjects (mean±standard deviation)
| Variable Group | Rebound therapy Mean±SD | Weight bearing Mean±SD | t | P |
|---|---|---|---|---|
| Age (year) | 55.8±6.5 | 57.0±8.4 | 0.344 | 0.79 |
| Height (cm) | 173.3±4.1 | 175.6±5.1 | 0.743 | 0.48 |
| Weight (kg) | 74.0±11.2 | 75.4±10.6 | 0.870 | 0.43 |
SD: Standard deviation
Table 4 shows the mean and standard deviation of the range of motion, the proprioception, and quality of life in the two groups in the pre- and posttest. In the repeated measures ANOVA, three intergroup, intragroup, and interactive comparisons were made. All of the variables in the two groups were significantly improved. Bet, there were significant differences in all three studied variables in the intergroup comparison, which means that rebound exercise was more effective in improving range of motion, the proprioception, and quality of life compared with weight-supported exercises.
Table 4.
The general results of the repeated measures ANOVA to analyze the variables of the research
| Factor | Group | Posttest Mean±SD | Pretest Mean±SD | Inter-group | Intera-group | Group interaction | ETA Coefficient |
|---|---|---|---|---|---|---|---|
| Proprioception (degree) | Rebound | 13.66±3.46 | 7.60±3.22 | F=120.28 | F=127.125 | 176.13 | 0.42 |
| Weight-supported | 12.25±3.34 | 10.38±2.48 | P<0.001 | P<0.001 | P<0.001 | ||
| Range of motion (degree) | Rebound | 103.66±10.46 | 134.60±13.22 | F=103.98 | F=38.12 | F=27.77 | 0.36 |
| Weight-supported | 105.25±13.34 | 118.38±12.48 | P<0.001 | P<0.001 | P<0.001 | ||
| Quality of life (points) | Rebound | 105.66±10.46 | 147.60±13.22 | F=215.10 | F=173.21 | F=45.00 | 0.27 |
| Weight-supported | 107.25±13.34 | 118.38±12.48 | P<0.001 | P<0.001 | P<0.001 |
Moreover, as shown in Figure 1, it is clearly observed that the slope of the rebound exercise group line was significantly higher than that of the weight-supported group, which was significantly higher in all three studied variables. It indicated that the rebound exercises had a significant effect on these variables in patients with PD.
Figure 1.
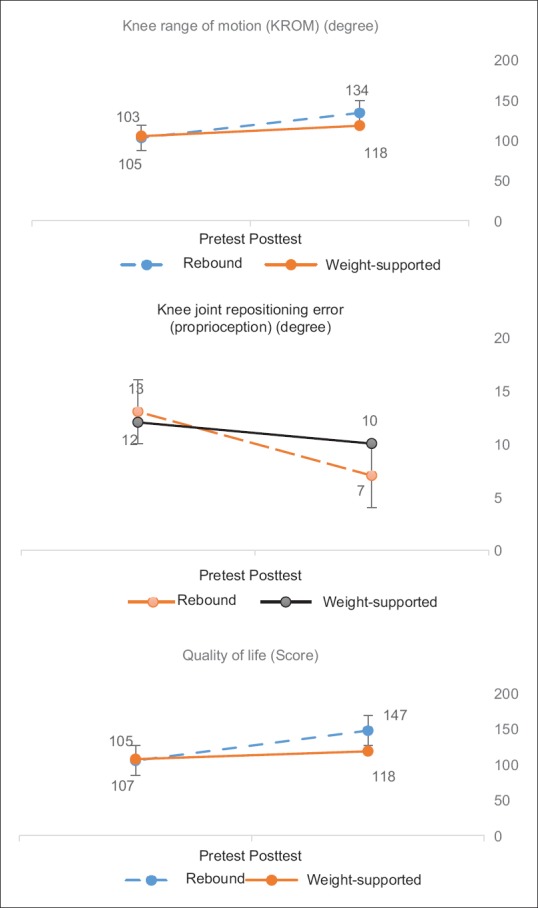
Changes in the scores of the variables of proprioception, range of motion and quality of life in two study groups in pretest and posttest
Discussion
According to the results of this study, after 8-week training, the range of motion in both training groups was significantly improved, whereas this rate was more improved in the rebound therapy group after 8 weeks.
The range of motion is defined as the flexibility of a joint or series of joints. Most daily activities require a good amount of range of motion or flexibility in relevant joints. Disease is considered as one of the important factors in determining the range of motion of patients. Since patients with PD in their daily life only carry out limited movements in terms of their level, lifestyle, and job functional status, therefore, it is expected that these patients have a more limited range of motion than healthy people. As mentioned earlier, reduced flexibility, ankylosis is one of the characteristics of the muscle stiffness syndrome. Another symptom is the ligament stiffness and the articular capsule, which reduces the range of motion in the joints.[24]
Reduced range of motion can result in a person's unaware of his actions and movements and ultimately lead to the destruction of articular receptors and damage proprioception.[25] In the study conducted on the range of motion in each group, both rebound exercises and weight-supported exercises have increased the range of motion, but rebound exercises have more increased the range of motion compared with weight-bearing exercises. Patients with PD usually have a small range of motion because of their low movements. According to the results of analysis of statistical data, there is a significant difference in the range of motion between the two training groups. Roshani et al. during a study showed that exercise can have a significant effect on the range of motion of individuals.[23] No study has been carried out on the effect of two types of rebound exercises and weight bearing on the range of motion in patients with PD.
Moreover, according to the results of this study, the training protocol has improved the proprioception in both training groups, so that this variable has more improved in the rebound therapy group. According to theoretical foundations, exercises can improve functional status by increasing the sensitivity of muscle spasms and Golgi tendon organs,[26] but the results of studies conducted on some exercises have questioned this theory. According to the results of Larsen et al.[26] and Torres et al.,[27] stretching exercises do not affect the receptors in the sense of joint position.
Streepey et al. also during a study concluded that the knee muscles stretching reduced the sensitivity of the proprioception receptors in the knee joint,[28] but according to the results of this study, both rebound and weight-bearing exercises could improve the sense of joint position but rebound exercises was considered as an important and effective factor in the sense of joint position. According to available data, no independent study has been carried out on the effect of rebound and weight-bearing exercises on the sense of joint position. Therefore, because of the lack of similar research, the comparison of the results of this study with other similar studies was ignored and the analysis, causes, and research topics that were similar to those in some variables, most of which have examined the effect of stretching exercises on various functional status were investigated, which most of these studies have examined the effect of stretching exercises on various functional status and their results show that stretching exercises improve functional status and proprioception.
Yamaguchi et al. during a study concluded that exercise has improved this functional status. They believe that an increase in muscle temperature and also a postactivation potentiation phenomenon to increase muscle strength after a period of muscle contraction is the possible reason of the improvement in exercise-induced functional status.[29] The nature of the rebound therapy exercises protocol is an active nature. A subject during doing these exercises does a pattern repetitive movement with a low to moderate intensity. This feature of the activation of rebound exercises increases the muscle temperature.[14] According to the results of various scientific reports, increased muscle temperature has a positive effect, such as decreased muscle stiffness and ligaments, increased sensitivity of neural receptors, increased neural network guidance, increased glycogenolysis, increased glycolysis, increased use of high energy phosphate,[30,31] and disposal of wastes from the body.[32] Repetition of movement in a specific movement pattern in rebound and weight-bearing exercises is another possible mechanism that affects the improvement of the sense of joint status. According to the results reported by Fletcher and Jones,[30] Perrier,[32] Little and Williams,[33] and Fletcher and Anness,[34] one of the possible effective factors on functional status improvement after exercising is to perform repetitive motions in a particular movement pattern, which leads to improve neuromuscular coordination of the pattern of movement. Fletcher and Jones during a study concluded that the repetition of movement in a particular pattern in the exercises helps proprioception to have a faster and more efficient switch from eccentric contraction to constrictive contraction during the sprinting.[30] Given that the sense of joint status is considered as one of the proprioception subsets, this mechanism can also use one of the causes for improving knee joint status after exercise protocols.
Another result of this study was that quality of life in both training groups was significantly improved, but this improvement was higher in the rebound therapy group. Different studies have proved the effect of different training protocols on the quality of life of various diseases.[35] In terms of the protocol and the effect of quality of life on exercise in patients with PD, these studies are consistent with this study.
PD is considered as one of the debilitating disease. These patients lose their physical fitness much faster, and their self-confidence and coordination reduces. Functional capacity of these patients is reduced with progressive stages and severe clinical status. However, many studies have reported the effects of depression on reduced motor function and increased disability following the progression of the disease. Physical disability leads to reducing the quality of life on average to severe.[36] One of the effective factors on the level of physical activity level is type of physical activity and training tools. Selection of the type of physical activity depends on the feasibility and motivation and positive attitude of the subject. Safety and attractiveness are another effective factor on this case.[37] Given that the proper trampoline was used in this study, the problem of access and the possibility of using have been reduced. Other important features of rebound exercises include a flexible level of exercise that does on it, this level absorbs force as a result of reduced pressure on the body. The less pressure on the joints can reduce the risk of vulnerability and increase safety.[38] Therefore, from this view, rebound exercises can be more effective exercises for the patient. These exercises can be effective on the continuation of these exercises by the users and their motivation and creating positive attitude due to attractiveness (due to its high mobility) and its less fatigability (due to its effects on the lymph system).[11] Therefore, rebound exercises in addition to physical health can lead to better mental health and leads to create a positive feeling and self-confidence. This is can be considered as other factors influencing rebound exercises on quality of life.[39]
It should be noted that rebound exercises can be done in a sitting and lying position by an individual. It converts the mentioned exercises into a useful and practical exercise for patients, which is done by the individual in an active manner. Improved stress, anxiety and depression, which can be considered as a psychological dimension, can be considered as another important factor in improving the quality of life. It includes happiness, well-being (positive emotions), being satisfied with life, and the lack of depression and anxiety (negative emotions) and leads to reduce stress perception and increase the individual's ability to work. These cases all refer to healthy psychological states that can result in mental health and quality of life.[35]
It has been shown that depression is the most important quality of life-related factor and physical performance, only the clinical stage of the disease has a more significant relationship with depression. Depression is a mood or personality disorder that involves boredom and unconsciousness and reluctance, and can affect one's thoughts, feelings and health, and well-being.[40] Although the mechanism of the effect of exercises on mental status is still unknown, but there are various hypotheses about how physical activity affects depression. Increased body temperature during physical activity is considered as one of the hypotheses that is known as the Pyrogen mechanism. Because of the high level of cellular involvement in rebound exercises and the significant increase in body temperature during these exercises, this factor can be one of the mentioned possible causes on depression. On the other hand, it has been shown that endurance training and aerobic exercises improve the depression by affecting various factors in the body, such as plasma catecholamine and monoamine in the brain.[41] In addition, the body secretes a hormone called endorphins during exercise, which is an antidepressant hormone that creates vitality in the body. The most effective way to increase the level of endorphins in the body is to have a regular and exciting exercise.[42] Trampoline is a training tool that has a very high excitement and vitality. Therefore, it can be said that it improves depression and the quality of life.
Conclusions
According to the results of the present study, it was observed that 8-week rebound therapy and weight-bearing exercises in patients with PD can significantly improve the range of motion, proprioception, and quality of life in patients with PD. According to the results of comparison of the studied groups, the rebound therapy group showed significant improvement in all research variables. The results show that 8-week training can be used to improve the range of motion, proprioception, and quality of life because of the low risk nature and available risk with the ability to control the pressure, but according to the results of this study, the superiority of rebound therapy exercises are superior to the other. But, according to the limitations of our study, as sample size, and duration of study and follow-up, more studies with more patients and longer periods are recommended.
Financial support and sponsorship
This research was sponsored by University of Isfahan.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Argue J. Parkinson's Disease and the Art of Moving. 1st ed. Oakland: New Harbinger Publications; 2000. [Google Scholar]
- 2.Pringsheim T, Jette N, Frolkis A, Steeves TD. The prevalence of Parkinson's disease: A systematic review and meta-analysis. Mov Disord. 2014;29:1583–90. doi: 10.1002/mds.25945. [DOI] [PubMed] [Google Scholar]
- 3.Pallone JA. Introduction to Parkinson's disease. Dis Mon. 2007;53:195–9. doi: 10.1016/j.disamonth.2007.05.001. [DOI] [PubMed] [Google Scholar]
- 4.Herman T, Giladi N, Hausdorff JM. Treadmill training for the treatment of gait disturbances in people with Parkinson's disease: A mini-review. J Neural Transm. 2009;116:307–18. doi: 10.1007/s00702-008-0139-z. [DOI] [PubMed] [Google Scholar]
- 5.Hirsch MA, Toole T, Maitland CG, Rider RA. The effects of balance training and high-intensity resistance training on persons with idiopathic Parkinson's disease. Am J Phys Med Rehabil. 2003;84:1109–17. doi: 10.1016/s0003-9993(03)00046-7. [DOI] [PubMed] [Google Scholar]
- 6.Hirsch MA, Farley BG. Exercise and neuroplasticity in persons living with Parkinson's disease. Eur J Phys Rehabil Med. 2009;45:215–29. [PubMed] [Google Scholar]
- 7.Rezaei H, Shafi Abadi A. Effect of group logotherapy on depression in multiple sclerosis patients. Educ Res J Bojnourd Univ. 2009;16:1–14. [Google Scholar]
- 8.Raeisi Dehkordi M, Sadeghi H, Bani Talebi E. The comparison of traditional exercises and Body Weight Supported Training (BWST) exercises on sensory-motor function, quality and quantity of walking in paraplegic spinal cord injured persons (Persian)] Archives of Rehabilitation. 2015;15:22–31. [Google Scholar]
- 9.Lucareli PR, Lima MO, Lima FP, de Almeida JG, Brech GC, D'Andréa Greve JM. Gait analysis following treadmill training with body weight support versus conventional physical therapy: A prospective randomized controlled single blind study. Spinal Cord. 2011;49:1001–7. doi: 10.1038/sc.2011.37. [DOI] [PubMed] [Google Scholar]
- 10.Lloyd F. Unpublished MSc thesis. Exeter: University Exeter; 1998. A pilot study into the effect of rebound therapy on the behaviour of adults with moderate and profound learning disabilities. [Google Scholar]
- 11.Sadeghi M, Ghasemi G, Karimi M. Effect of 12-week-rebound therapy exercise on static stability of patients with spinal cord injury? J Sport Rehabil. 2018:1–16. doi: 10.1123/jsr.2017-0303. doi: 10.1123/jsr. 2017-0303. [DOI] [PubMed] [Google Scholar]
- 12.Giagazoglou P, Kokaridas D, Sidiropoulou M, Patsiaouras A, Karra C, Neofotistou K. Effects of a trampoline exercise intervention on motor performance and balance ability of children with intellectual disabilities. Res Dev Disabil. 2013;34:2701–7. doi: 10.1016/j.ridd.2013.05.034. [DOI] [PubMed] [Google Scholar]
- 13.Smith T, Rana RS, Missiaen P, Rose KD, Sahni A, Singh H, et al. High bat (Chiroptera) diversity in the Early Eocene of India. Naturwissenschaften. 2007;94:1003–9. doi: 10.1007/s00114-007-0280-9. [DOI] [PubMed] [Google Scholar]
- 14.Ghasemi GA, Rahimi N, Tahmasebi RK. The effects of rebound exercises on health-related physical fitness in educable children with mental retardation. Sadra Med Sci J. 2017:4. [Google Scholar]
- 15.Mitsiou M, Sidiropoulo M, Giagkazoglou P, Tsimaras V. Effect of trampoline based intervention program in static balance of children with development coordination disorder. J Sport Med. 2010;45:125–43. [Google Scholar]
- 16.Miyai I, Fujimoto Y, Ueda Y, Yamamoto H, Nozaki S, Saito T, et al. Treadmill training with body weight support: Its effect on Parkinson's disease. Arch Phys Med Rehabil. 2000;81:849–52. doi: 10.1053/apmr.2000.4439. [DOI] [PubMed] [Google Scholar]
- 17.Hoehn M, Yahr M. Parkinsonism: Onset, progression and mortality. Neurology. 1967;17:427–42. doi: 10.1212/wnl.17.5.427. [DOI] [PubMed] [Google Scholar]
- 18.Fahn S, Elton R Members of the updrs development committee. In: Recent Developments in Parkinson's Disease. Fahn S, Marsden CD, Calne DB, Goldstein M, editors. Vol. 2. Florham Park, NJ: Macmillan Health Care Information; 1987. pp. 153–63. 293-304. [Google Scholar]
- 19.Rajabi R, Samadi H. Corrective Exercise Laboratory for Postgraduate Students. 2nd ed. Tehran University Publications; 2013. [Google Scholar]
- 20.Contu S, Cappello L, Konczak J, Masia L. Preliminary analysis of non-dominant proprioceptive acuity and interlimb asymmetry in the human wrist. Conf Proc IEEE Eng Med Biol Soc. 2015;2015:3598–601. doi: 10.1109/EMBC.2015.7319171. [DOI] [PubMed] [Google Scholar]
- 21.Elangovan N, Herrmann A, Konczak J. Assessing proprioceptive function: Evaluating joint position matching methods against psychophysical thresholds. Phys Ther. 2014;94:553–61. doi: 10.2522/ptj.20130103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rodrigues de Paula F, Teixeira-Salmela LF, Coelho de Morais Faria CD, Rocha de Brito P, Cardoso F. Impact of an exercise program on physical, emotional, and social aspects of quality of life of individuals with Parkinson's disease. Mov Disord. 2006;21:1073–7. doi: 10.1002/mds.20763. [DOI] [PubMed] [Google Scholar]
- 23.Roshani S, Moghaddasi A, Maryam A. Effect of a4-week comprehensive rehabilitation program on increasing the range of motion and reducing pain in men with frozen shoulder. Salmand Sci J. 2010;5:33–24. [Google Scholar]
- 24.Ebaugh DD, McClure PW, Karduna AR. Effects of shoulder muscle fatigue caused by repetitive overhead activities on scapulothoracic and glenohumeral kinematics. J Electromyogr Kinesiol. 2006;16:224–35. doi: 10.1016/j.jelekin.2005.06.015. [DOI] [PubMed] [Google Scholar]
- 25.Lohrer H, Alt W, Gollhofer A. Neuromuscular properties and functional aspects of taped ankles. Am J Sports Med. 1999;27:69–75. doi: 10.1177/03635465990270012001. [DOI] [PubMed] [Google Scholar]
- 26.Larsen R, Lund H, Christensen R, Røgind H, Danneskiold-Samsøe B, Bliddal H. Effect of static stretching of quadriceps and hamstring muscles on knee joint position sense. Br J Sports Med. 2005;39:43–6. doi: 10.1136/bjsm.2003.011056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Torres R, Duarte JA, Cabri JM. An acute bout of quadriceps muscle stretching has no influence on knee joint proprioception. J Hum Kinet. 2012;34:33–9. doi: 10.2478/v10078-012-0061-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Streepey JW, Mock MJ, Riskowski JL, Vanwye WR, Vitvitskiy BM, Mikesky AE. Effects of quadriceps and hamstrings proprioception neuromuscular facilitation stretching on knee movement sensation. J Strength Cond Res. 2010;24:1037–42. doi: 10.1519/JSC.0b013e3181d09e87. [DOI] [PubMed] [Google Scholar]
- 29.Yamaguchi T, Ishii K. Effects of static stretching for 30 seconds and dynamic stretching on leg extension power. J Strength Cond Res. 2005;19:677–83. doi: 10.1519/15044.1. [DOI] [PubMed] [Google Scholar]
- 30.Fletcher IM, Jones B. The effect of different warm-up stretch protocols on 20 meter sprint functional status in trained rugby union players. J Strength Cond Res. 2004;18:885–8. doi: 10.1519/14493.1. [DOI] [PubMed] [Google Scholar]
- 31.Sekir U, Arabaci R, Akova B, Kadagan SM. Acute effects of static and dynamic stretching on leg flexor and extensor isokinetic strength in elite women athletes. Scand J Med Sci Sports. 2010;20:268–81. doi: 10.1111/j.1600-0838.2009.00923.x. [DOI] [PubMed] [Google Scholar]
- 32.Perrier ET. The effects of static and dynamic stretching on reaction time and functional status in a countermovement jump. 2009 [Google Scholar]
- 33.Little T, Williams AG. Effects of differential stretching protocols during warm-ups on high-speed motor capacities in professional soccer players. J Strength Cond Res. 2006;20:203–7. doi: 10.1519/R-16944.1. [DOI] [PubMed] [Google Scholar]
- 34.Fletcher IM, Anness R. The acute effects of combined static and dynamic stretch protocols on fifty-meter sprint functional status in track-and-field athletes. J Strength Cond Res. 2007;21:784–7. doi: 10.1519/R-19475.1. [DOI] [PubMed] [Google Scholar]
- 35.Quel de Oliveira C, Refshauge K, Middleton J, de Jong L, Davis GM. Effects of activity-based therapy interventions on mobility, independence, and quality of life for people with spinal cord injuries: A systematic review and meta-analysis. J Neurotrauma. 2017;34:1726–43. doi: 10.1089/neu.2016.4558. [DOI] [PubMed] [Google Scholar]
- 36.Lucas RE. Long-term disability is associated with lasting changes in subjective well-being: Evidence from two nationally representative longitudinal studies. J Pers Soc Psychol. 2007;92:717–30. doi: 10.1037/0022-3514.92.4.717. [DOI] [PubMed] [Google Scholar]
- 37.Pelletier CA, Ditor DS, Latimer-Cheung AE, Warburton DE, Hicks AL. Exercise equipment preferences among adults with spinal cord injury. Spinal Cord. 2014;52:874–9. doi: 10.1038/sc.2014.146. [DOI] [PubMed] [Google Scholar]
- 38.Carter AE. The New Miracles of Rebound Exercise. ALM Publishers; 1988. [Google Scholar]
- 39.Jordan S, Gruber J.D. On the rebound: A fun easy way to vibrant Health and well- Being. 2004 [Google Scholar]
- 40.Lim SW, Shiue YL, Ho CH, Yu SC, Kao PH, Wang JJ, et al. Anxiety and depression in patients with traumatic spinal cord injury: A nationwide population-based cohort study. PloS One. 2017;12:e0169623. doi: 10.1371/journal.pone.0169623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Martinsen EW. Benefits of exercise for the treatment of depression. Sports Med. 1990;9:380–9. doi: 10.2165/00007256-199009060-00006. [DOI] [PubMed] [Google Scholar]
- 42.Cleare A, Pariante CM, Young AH, Anderson IM, Christmas D, Cowen PJ, et al. Evidence-based guidelines for treating depressive disorders with antidepressants: A revision of the 2008 British Association for Psychopharmacology guidelines. J Psychopharmacol. 2015;29:459–525. doi: 10.1177/0269881115581093. [DOI] [PubMed] [Google Scholar]


