ABSTRACT
Background
The panelists of the Joint National Committee recently published new recommendations for the management of hypertension. Our study aims to evaluate how current practice compares.
Hypothesis
Current practice likely deviates from the recent JNC 8 panelists' recommendations.
Methods
A survey was sent to cardiology providers at 3 academic medical centers: Mayo Clinic, Jacksonville, Florida; Mayo Clinic, Scottsdale, Arizona; and Mayo Clinic, Rochester, Minnesota. Providers were asked to select which blood‐pressure goal would be deemed appropriate in various cases based on individual practice in both the maintenance of patients already on therapy as well as threshold of when to initiate therapy. Comparisons with current recommendations were made, as well as geographic location and level of experience.
Results
A total of 251 survey requests were sent (May 2014), and 77 responses (30.7%) were received. Cardiologists tended not to practice according to the new guidelines, with most variation seen in patients age >60 years without comorbidities on active treatment. Providers' selection of initial pharmacologic agents in non–African American patients, African American patients, and patients with diabetes mellitus reflected congruency with guidelines.
Conclusions
Our study found that clinical practice does not correlate well with the new blood‐pressure goal recommendations published by the Joint National Committee 8 panelists, particularly in patients age >60 years. Practitioners are likely to follow the recommendations in regard to pharmacologic management.
Introduction
The Joint National Committee (JNC) has been tasked with composing guidelines and recommendations to assist physicians in the diagnosis and management of hypertension since the Committee's first report in 1977.1 The panelists of the JNC 8 published a revision to the JNC 7 recommendations in the Journal of the American Medical Association in December 2013.2 Unlike prior guidelines, the National Heart, Lung, and Blood Institute (NHLBI) withdrew official support from development of the JNC 8 guidelines, and therefore the guidelines were produced based on the recommendations of the panelists.3 The JNC 8 publication incorporated notable changes in the blood pressure at which to initiate and maintain therapy and provided a narrower focus, compared with the former JNC 7 guidelines.1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11 The most significant and controversial change in blood‐pressure management involves patients age >60 years, in which a blood‐pressure goal of 150/90 mm Hg was selected. Because of this, much contention and disagreement evolved.3, 4, 5, 6, 7, 8, 9, 10
Evidence‐based studies were panelists' focus in forming their current recommendations. Randomized controlled trials from 1966 to 2013 with sample sizes of ≥2000 patients with a minimum of 1 year's follow‐up were reviewed, without the incorporation of meta‐analyses, systematic reviews of the literature, post‐hoc analyses, or observational studies. Criticism of this methodology resulted.4, 5, 8, 9
In 2009, Germino et al voiced expectations that the new guidelines would be evidence‐based, yet warned that, because it is a consensus document, not all committee members will agree on certain recommendations.1 This proved true in a publication by 3 panel members stating that certain recommendations may be controversial and that physicians, including cardiologists, may show hesitancy in their incorporation into clinical practice.5 To that same extent, the American College of Cardiology and American Heart Association (ACC/AHA) released a statement shortly after the publication of the panelists' recommendations confirming that there may be concerns with the new recommendations and recognized the older JNC 7 guidelines for the diagnosis and management of hypertension.7 Numerous other publications have followed, including a contrast of the new recommendations with those established by the Canadian Hypertension Education Project.1, 2, 3, 4, 5, 6, 7, 8, 9, 10
Considering the debate and editorial criticisms, there is much uncertainty as to whether the current recommendations are reflected in clinical practice.1, 2, 3, 4, 5, 6, 7, 8, 9, 10 Although numerous editorials disagree with portions of the recommendations, there are no data assessing how current practice compares with these new recommendations. Our study examines current diagnosis and management of hypertension and compares such with the panelists' new recommendations.
Methods
We performed a multisite survey of all clinical cardiology providers at 3 academic medical centers: Mayo Clinic, Scottsdale, Arizona (MCA); Mayo Clinic, Jacksonville, Florida (MCF); and Mayo Clinic, Rochester, Minnesota (MCR). Providers were identified by search of the Mayo Clinic intranet system and confirmed by lists provided by the department coordinators. Providers included both cardiology fellows and faculty physicians. Providers were sent an online questionnaire to complete via email. Three separate emails were sent to providers 1 week apart during May 2014. The questionnaire was comprised of 3 main components (Figure 1). The first component identified respondent demographic information, including practice location and experience level. The second component consisted of clinical questions regarding blood‐pressure levels used for the diagnosis and management of hypertension. Case scenarios for these questions were based on the panelists' recommendations and included blood‐pressure goals in patients already treated for hypertension as well as blood‐pressure values at which to initiate therapy. The third component assessed pharmacotherapy in the treatment of hypertension.
Figure 1.
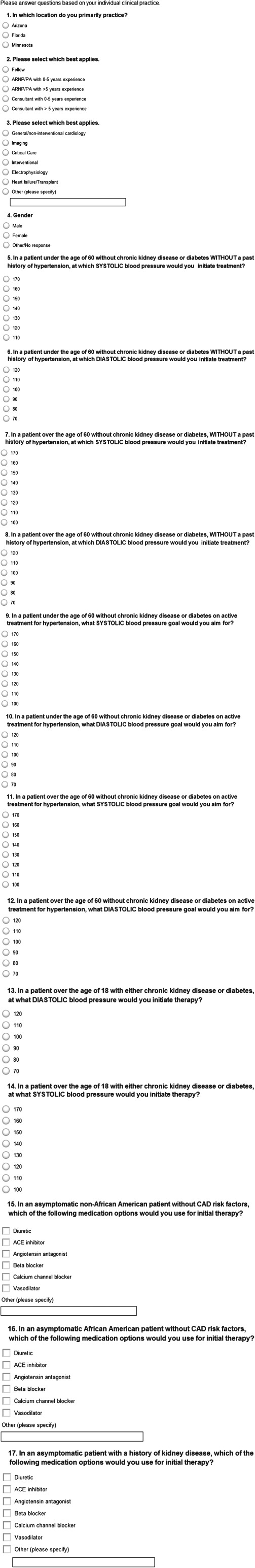
Survey image.
Analyses comparing hypertension diagnosis and management with the panelists' recommendations were made, along with comparisons between level of training and geographic location. Analysis of variance and the Fisher t test were used to compare the results. P values <0.05 were considered significant. Institutional review board approval was obtained prior to the initiation of this study.
Results
Of 251 surveys sent, 77 responses were received (30.7% response rate). Sixteen of 38 (42.1%) surveys were from MCA, 13 of 25 (52.0%) were from MCF, and 48 of 188 (25.6%) were from MCR. The majority of the respondents were faculty physicians (n = 50, 64.9%) and were male (n = 61, 79.2%). Most practitioners practiced general, noninterventional cardiology (n = 31, 40.3%), followed by imaging (n = 16, 20.8%; Table 1).
Table 1.
Demographics of All Survey Respondents
| Variable | Response/Data |
|---|---|
| Location, n (%) | |
| Arizona | 16 (20.8) |
| Florida | 13 (16.9) |
| Minnesota | 48 (62.3) |
| Experience, n (%) | |
| Fellow | 27 (35.1) |
| Attending | 50 (64.9) |
| Subspecialty, n (%) | |
| General/noninterventional | 31 (40.3) |
| Imaging | 16 (20.8) |
| Interventional | 8 (10.4) |
| Heart failure/transplant | 8 (10.4) |
| Critical care | 4 (5.2) |
| Electrophysiology | 6 (7.8) |
| Other | 4 (5.2) |
| Sex, n (%) | |
| M | 61 (79.2) |
| F | 16 (20.8) |
Abbreviations: F, female; M, male.
Cumulative responses to the survey questions with comparisons with the panelists' recommendations are listed in Table 2. In general, respondents were likely to practice based on the panelists' recommendations in patients age <60 years without concomitant chronic kidney disease (CKD) or diabetes mellitus (DM). Almost 78% (n = 60) of respondents selected a systolic value of 140 mm Hg and a diastolic value of 90 mm Hg as goal to initiate therapy, with the overall average systolic and diastolic values being slightly higher. In patients age >18 years with either CKD or DM, respondents tended to initiate therapy at lower blood‐pressure values, and 53.3% (n = 41) and 61.0% (n = 47), respectively, would use the values of 140 and 90 mm Hg recommended by the panelists. In patients age >60 years without CKD or DM, respondents were more likely to initiate therapy at a lower systolic blood pressure (146.9 mm Hg) than the recommended value of 150 mm Hg, and only 46.8% (n = 36) respondents selected 150 mm Hg. A higher proportion of respondents was likely to follow the recommendations in regard to the diastolic pressure, with an average diastolic pressure of 92.5 mm Hg and 75.3% (n = 58) of respondents selecting 90 mm Hg.
Table 2.
All Survey Respondents Compared With Guidelines
| Variable | Response/Data | Guideline Comparison, n (%) |
|---|---|---|
| In a patient age <60 without CKD or DM WITHOUT a past history of hypertension, at which SYSTOLIC BP would you initiate therapy? (mm Hg) | 142.3 | 140 (77.9a) |
| In a patient age <60 without CKD or DM WITHOUT a past history of hypertension, at which DIASTOLIC BP would you initiate therapy? (mm Hg) | 91.9 | 90 (77.9a) |
| In a patient age >18 with either CKD or DM, at what SYSTOLIC BP would you initiate therapy? (mm Hg) | 136.1 | 140 (53.3a) |
| In a patient age >18 with either CKD or DM, at what DIASTOLIC BP would you initiate therapy? (mm Hg) | 89.2 | 90 (61.0a) |
| In a patient age >60 without CKD or DM, WITHOUT a past history of hypertension, at which SYSTOLIC BP would you initiate therapy? (mm Hg) | 146.9 | 150 (46.8a) |
| In a patient age >60 without CKD or DM, WITHOUT a past history of hypertension, at which DIASTOLIC BP would you initiate therapy? (mm Hg) | 92.5 | 90 (75.3a) |
| In a patient age <60 without CKD or DM on active treatment for hypertension, what SYSTOLIC BP goal would you aim for? (mm Hg) | 132.9 | 140 (45.5a) |
| In a patient age <60 without CKD or DM on active treatment for hypertension, what DIASTOLIC BP goal would you aim for? (mm Hg) | 83.9 | 90 (42.9a) |
| In a patient age >60 without CKD or DM on active treatment for hypertension, what SYSTOLIC BP goal would you aim for? (mm Hg) | 138.7 | 150 (22.1a) |
| In a patient age >60 without CKD or DM on active treatment for hypertension, what DIASTOLIC BP goal would you aim for? (mm Hg) | 86.4 | 90 (61.0a) |
| In an asymptomatic non–African American patient without CAD risk factors, which of the following medication options would you use for initial therapy? n (%) | Diuretic, 46 (59.7); ACEI, 34 (44.2); angiotensin ant, 12 (15.6); BB, 1 (1.3); CCB, 15 (19.5); vasodilator, 0 (0); other, 3 (3.9) | Guidelines allow for broad selection |
| In an asymptomatic African American patient without CAD risk factors, which of the following medication options would you use for initial therapy? n (%) | Diuretic, 43 (55.8); ACEI, 11 (14.3); angiotensin ant, 4 (5.2); BB, 2 (2.6); CCB, 31 (40.3); vasodilator, 5 (6.5); other, 3 (3.9) | CCBs and diuretics (thiazide) preferred |
| In an asymptomatic patient with a history of kidney disease, which of the following medication options would you use for initial therapy? n (%) | Diuretic, 4 (5.2); ACEI, 68 (88.3); angiotensin ant, 11 (14.3); BB, 0 (0); CCB, 6 (7.8); vasodilator, 1 (1.3); other, 3 (3.9) | ACEI |
Abbreviations: ACEI, angiotensin‐converting enzyme inhibitor; angiotensin ant, angiotensin antagonist; BB, β‐blocker; BP, blood pressure; CAD, coronary artery disease; CCB, calcium channel blocker; CKD, chronic kidney disease; DM, diabetes mellitus.
Percentage of respondents who selected the BP value recommended by the panelists.
In patients already on active pharmacologic treatment (compared with blood‐pressure levels at which treatment should be initiated) for hypertension, the goals were lower than those recommended by the panelists. In patients age <60 years without CKD or DM, the average goals were a systolic pressure of 132.9 mm Hg and diastolic of 83.9 mm Hg. A total of 45.5% (n = 35) and 42.9% (n = 33) of respondents selected the recommended goals of 140 mm Hg and 90 mm Hg, respectively. Similarly, in patients age >60 years without CKD or DM, the goal blood pressures were lower than those recommended by the panelists (83.9 mm Hg vs 90 mm Hg and 138.7 mm Hg vs 150 mm Hg), with 22.1% (n = 17) selecting the recommended systolic value of 150 mm Hg and 61.0% (n = 47) the diastolic value of 90 mm Hg.
Respondents were likely to use diuretics (n = 46, 59.7%) and angiotensin‐converting enzyme inhibitors (ACEIs; n = 34, 44.2%) for initial therapy in asymptomatic non–African American patients. Most respondents selected diuretic medications (n = 43, 55.8%), followed by calcium channel blockers (n = 31, 40.3%), in asymptomatic African American patients. In patients with a history of kidney disease, most practitioners selected ACEIs (n = 68, 88.3%).
A second analysis of the data was performed comparing providers' responses based on location (Table 3). No difference in baseline demographics was present between the 3 sites, although a higher proportion of respondents from MCR practiced subspecialties other than general, noninterventional cardiology. The responses grouped according to site are represented in Table 3. Overall, no significant difference in practice was noted between the 3 sites.
Table 3.
Subanalysis Based on Practice Location
| Variable | Arizona | Florida | Minnesota | P Value |
|---|---|---|---|---|
| Experience, n (%) | 0.618 | |||
| Fellow | 6 (37.5) | 3 (23.1) | 18 (37.5) | |
| Attending | 10 (62.5) | 10 (76.9) | 30 (62.5) | |
| Subspecialty, n (%) | 0.288 | |||
| General/noninterventional | 7 (43.8) | 8 (61.5) | 16 (33.3) | |
| Imaging | 4 (25.0) | 1 (7.7) | 11 (22.9) | |
| Interventional | 2 (12.5) | 1 (7.7) | 5 (10.4) | |
| Heart failure/transplant | 1 (6.3) | 2 (15.4) | 5 (10.4) | |
| Critical care | 0 (0) | 0 (0) | 4 (8.3) | |
| Electrophysiology | 2 (12.5) | 1 (7.7) | 3 (6.3) | |
| Other | 0 (0) | 0 (0) | 4 (8.3) | |
| Sex, n (%) | 0.066 | |||
| M | 1 (6.3) | 1 (7.7) | 14 (29.2) | |
| F | 15 (93.8) | 12 (92.3) | 34 (70.8) | |
| In a patient age <60 without CKD or DM WITHOUT a past history of hypertension, at which SYSTOLIC BP would you initiate therapy? (mm Hg) | 141.9 (81.3a) | 140.8 (76.9a) | 142.9 (77.1a) | 0.423 |
| In a patient age <60 without CKD or DM WITHOUT a past history of hypertension, at which DIASTOLIC BP would you initiate therapy? (mm Hg) | 91.3 (87.5a) | 90.8 (92.3a) | 92.5 (70.8a) | 0.34 |
| In a patient age >18 with either CKD or DM, at what SYSTOLIC BP would you initiate therapy? (mm Hg) | 136.3 (68.8a ) | 136.2 (69.2a) | 136.0 (43.8a) | 0.994 |
| In a patient age >18 with either CKD or DM, at what DIASTOLIC BP would you initiate therapy? (mm Hg) | 88.9 (62.5a ) | 90.0 (84.6a) | 89.2 (54.2a) | 0.892 |
| In a patient age >60 without CKD or DM, WITHOUT a past history of hypertension, at which SYSTOLIC BP would you initiate therapy? (mm Hg) | 147.5 (50a) | 144.6 (30.8a) | 147.3 (50a) | 0.436 |
| In a patient age >60 without CKD or DM, WITHOUT a past history of hypertension, at which DIASTOLIC BP would you initiate therapy? (mm Hg) | 92.5 (75a) | 90.8 (92.3a) | 92.9 (70.8a) | 0.289 |
| In a patient age <60 without CKD or DM on active treatment for hypertension, what SYSTOLIC BP goal would you aim for? (mm Hg) | 135.0 (56.3a) | 130.8 (30.8a) | 132.7 (45.8a) | 0.324 |
| In a patient age <60 without CKD or DM on active treatment for hypertension, what DIASTOLIC BP goal would you aim for? (mm Hg) | 85.6 (56.3a) | 81.5 (30.8a) | 84.0 (41.7a) | 0.154 |
| In a patient age >60 without CKD or DM on active treatment for hypertension, what SYSTOLIC BP goal would you aim for? (mm Hg) | 141.3 (31.3a) | 136.9 (30.8a) | 138.3 (16.7a) | 0.389 |
| In a patient age >60 without CKD or DM on active treatment for hypertension, what DIASTOLIC BP goal would you aim for? (mm Hg) | 88.1 (68.8a) | 84.6 (46.2a) | 86.3 (62.5a) | 0.18 |
| In an asymptomatic non–African American patient without CAD risk factors, which of the following medication options would you use for initial therapy? n (%) | Diuretic, 13 (81.3); ACEI, 8 (50); angiotensin ant, 3 (18.8); BB, 0 (0); CCB, 4 (25); vasodilator, 0 (0); other, 0 (0) | Diuretic, 6 (46.2); ACEI, 8 (61.5); angiotensin ant, 4 (30.8); BB, 0 (0); CCB, 3 (23.1); vasodilator, 0 (0); other, 1 (7.7) | Diuretic, 27 (56.3); ACEI, 18 (37.5); angiotensin ant, 5 (10.4); BB, 1 (2.1); CCB, 8 (16.7); vasodilator, 0 (0); other, 2 (4.2) | 0.553 |
| In an asymptomatic African American patient without CAD risk factors, which of the following medication options would you use for initial therapy? n (%) | Diuretic, 14 (87.5); ACEI, 1 (6.3); angiotensin ant, 0 (0); BB, 0 (0); CCB, 7 (43.8); vasodilator, 0 (0); other, 0 (0) | Diuretic, 7 (53.8); ACEI, 2 (15.4); angiotensin ant, 1 (7.7); BB, 0 (0); CCB, 6 (46.2); vasodilator, 1 (7.7); other, 1 (7.7) | Diuretic, 22 (45.8); ACEI, 8 (16.7); angiotensin ant, 3 (6.3); BB, 2 (4.2); CCB, 18 (37.5); vasodilator, 4 (8.3); other, 2 (4.2) | 0.266 |
| In an asymptomatic patient with a history of kidney disease, which of the following medication options would you use for initial therapy? n (%) | Diuretic, 1 (6.3); ACEI, 16 (100); angiotensin ant, 3 (18.8); BB, 0 (0); CCB, 1 (6.3); vasodilator, 0 (0); other, 0 (0) | Diuretic, 2 (15.4); ACEI, 10 (76.9); angiotensin ant, 3 (23.1); BB, 0 (0); CCB, 2 (15.4); vasodilator, 0 (0); other, 1 (7.7) | Diuretic, 1 (2.1); ACEI, 42 (87.5); angiotensin ant, 5 (10.4); BB, 0 (0); CCB, 3 (6.3); vasodilator, 1 (2.1); other, 2 (4.2) | 0.542 |
Abbreviations: ACEI, angiotensin‐converting enzyme inhibitor; angiotensin ant, angiotensin antagonist; BB, β‐blocker; BP, blood pressure; CAD, coronary artery disease; CCB, calcium channel blocker; CKD, chronic kidney disease; DM, diabetes mellitus; F, female; M, male.
Percentage of respondents that selected the BP value recommended by the panelists.
An additional analysis was performed based on level of training, comparing responses from cardiology fellows with cardiology attending physicians. Responses are demonstrated in Table 4. Similar to the analysis comparing location, no difference was found in practice based on level of experience.
Table 4.
Subanalysis Based on Level of Experience
| Fellow | Attending | P Value | |
|---|---|---|---|
| Location, n (%) | 0.822 | ||
| Arizona | 6 (22.2) | 10 (20) | |
| Florida | 3 (11.1) | 10 (20) | |
| Minnesota | 18 (66.7) | 30 (60) | |
| Subspecialty, n (%) | 0.055 | ||
| General/noninterventional | 15 (55.6) | 16 (32) | |
| Imaging | 5 (18.5) | 11 (22) | |
| Interventional | 2 (7.4) | 6 (12) | |
| Heart failure/transplant | 2 (7.4) | 6 (12) | |
| Critical care | 1 (3.7) | 3 (6) | |
| Electrophysiology | 2 (7.4) | 4 (8) | |
| Other | 0 (0) | 4 (8) | |
| Sex, n (%) | 0.164 | ||
| M | 8 (29.6) | 8 (16) | |
| F | 19 (70.4) | 42 (84) | |
| In a patient age <60 without CKD or DM WITHOUT a past history of hypertension, at which SYSTOLIC BP would you initiate therapy? (mm Hg) | 143.0 (44.4a) | 142.0 (78a) | 0.455 |
| In a patient age <60 without CKD or DM WITHOUT a past history of hypertension, at which DIASTOLIC BP would you initiate therapy? (mm Hg) | 92.6 (74.1a) | 91.6 (80a) | 0.338 |
| In a patient age >18 with either CKD or DM, at what SYSTOLIC BP would you initiate therapy? (mm Hg) | 134.4 (40.7a) | 137.0 (60a) | 0.122 |
| In a patient age >18 with either CKD or DM, at what DIASTOLIC BP would you initiate therapy? (mm Hg) | 88.1 (51.9a) | 89.8 (666a) | 0.328 |
| In a patient age >60 without CKD or DM, WITHOUT a past history of hypertension, at which SYSTOLIC BP would you initiate therapy? (mm Hg) | 146.7 (37.0a) | 147 (52a) | 0.842 |
| In a patient age >60 without CKD or DM, WITHOUT a past history of hypertension, at which DIASTOLIC BP would you initiate therapy? (mm Hg) | 92.6 (74.1a) | 92.4 (76a) | 0.854 |
| In a patient age <60 without CKD or DM on active treatment for hypertension, what SYSTOLIC BP goal would you aim for? (mm Hg) | 132.6 (48.1a) | 133.0 (44a) | 0.824 |
| In a patient age <60 without CKD or DM on active treatment for hypertension, what DIASTOLIC BP goal would you aim for? (mm Hg) | 84.4 (48.1a) | 83.6 (40a) | 0.535 |
| In a patient age >60 without CKD or DM on active treatment for hypertension, what SYSTOLIC BP goal would you aim for? (mm Hg) | 137.0 (18.5a) | 139.6 (24a) | 0.232 |
| In a patient age >60 without CKD or DM on active treatment for hypertension, what DIASTOLIC BP goal would you aim for? (mm Hg) | 86.7 (59.3a) | 86.2 (62a) | 0.705 |
| In an asymptomatic non–African American patient without CAD risk factors, which of the following medication options would you use for initial therapy? n (%) | Diuretic, 20 (74.1); ACEI, 10 (37.0); angiotensin ant, 6 (22.2); BB, 0 (0); CCB, 5 (18.5); vasodilator, 0 (0); other, 2 (7.4) | Diuretic, 26 (52); ACEI, 24 (48); angiotensin ant, 6 (12); BB, 1 (2); CCB, 10 (20); vasodilator, 0 (0); other, 1 (2) | 0.985 |
| In an asymptomatic African American patient without CAD risk factors, which of the following medication options would you use for initial therapy? n (%) | Diuretic, 14 (51.9); ACEI, 4 (14.8); angiotensin ant, 2 (7.4); BB, 1 (3.7); CCB, 10 (37.0); vasodilator, 3 (11.1); other, 2 (7.4) | Diuretic, 29 (58); ACEI, 7 (14); angiotensin ant, 2 (4); BB, 1 (2); CCB, 21 (42); vasodilator, 2 (4); other, 1 (2) | 0.401 |
| In an asymptomatic patient with a history of kidney disease, which of the following medication options would you use for initial therapy? n (%) | Diuretic, 0 (0); ACEI, 25 (92.6); angiotensin ant, 6 (22.2); BB, 0 (0); CCB, 1 (3.7); vasodilator, 0 (0); other, 2 (7.4) | Diuretic, 4 (8); ACEI, 43 (86); angiotensin ant, 5 (10); BB, 0 (0); CCB, 5 (10); vasodilator, 1 (2); other, 1 (2) | 0.613 |
Abbreviations: ACEI, angiotensin‐converting enzyme inhibitor; angiotensin ant, angiotensin antagonist; BB, β‐blocker; BP, blood pressure; CAD, coronary artery disease; CCB, calcium channel blocker; CKD, chronic kidney disease; DM, diabetes mellitus; F, female; M, male.
Percentage of respondents that selected the BP value recommended by the panelists.
Discussion
Our study found incongruences with cardiologists' management of hypertension and the JNC 8 panelists' new recommendations. The majority of practitioners did not select the goal values recommended by the panelists in most of the case presentations within the survey. As predicted by 3 panelists as well as several others, the most discordance with the recommendations was seen in the population group age >60 years, with <25% of respondents in our study agreeing with the goal systolic blood pressure of 150 mm Hg.1, 3, 4, 5, 6, 7, 8, 9, 10 Cardiologists were also less likely to follow the recommendations in deciding upon goal blood‐pressure values in patients on active treatment compared with blood‐pressure thresholds at which treatment should be initiated in patients not on pharmacologic therapy. In patients age <60 years not on pharmacologic treatment, the respondents showed more practice consistency with the JNC 8 panelists' recommendations; yet in patients already on treatment in either age group or patients with comorbidities of CKD or DM, respondents appeared more aggressive in blood‐pressure control with lower target values.
In regard to pharmacologic options, responses were similar to the recommendations. In non–African American patients, guidelines are broad and allow for physicians to decide among a variety of medications for appropriate pharmacologic therapy, which can be seen in the broad selection of choices in our data. The panelists' recommendations advise that African American patients should be placed on either calcium channel blockers or diuretics for initial management, and this is reflected in current management based on our cohort. Similarly, in patients with a history of kidney disease, most respondents selected ACEIs as initial therapy, as recommended by the panelists.
There was no difference in the management of hypertension between clinical sites. This may likely be attributed to the comfort with prior guidelines as well as consistent hesitancy to adopt the newer recommendations. Similarly, no difference was noted based on level of training. Trainees generally practice medicine based on what is taught by faculty physicians, and our study indicates that currently there is little influence in their practice by the new recommendations.
Just as the JNC 8 panelists' recommendations differ with the JNC 7 guidelines, published literature has shown that various cardiovascular‐related guidelines do change over time. A study assessing official ACC/AHA guidelines found that significant changes in guidelines are common in updated revisions.12 Other studies have shown that physicians have hesitancy in following newer guidelines, especially upon initiation.13, 14 Other reasons as to why clinical practice is not guided by the new recommendations include disagreement with the current recommendations and comfort with previous guidelines, including those by the JNC 7.
Study Limitations
This study has limitations. Although geographic comparisons were made, all locations are part of the same academic institution, which can potentially bias the data. Also, we had a low survey response rate, with approximately one‐third of those surveyed responding, and some variation was seen among the 3 sites. Study data were collected approximately 6 months following publication of the recommendations, yet without preguideline data it is difficult to assess how clinical practice has changed following the panelists' publication. Rather, this study offers a sense of how current practice compares with the current recommendations. To that same extent, the study was conducted within a relatively short period following the JNC 8 publication, and only cardiologists were surveyed among the institutions.
Conclusion
This is the first multisite survey assessing cardiologists' clinical practice compared with the new JNC 8 panelists' recommendations. Our study found that clinical practice does not correlate well with the new blood‐pressure goal recommendations published by the JNC 8 panelists, especially in those patients age >60 years. Practitioners are likely to follow the recommendations in regard to pharmacologic management. Although we assessed cardiologists' attitudes 6 months following publication of the JNC 8 recommendation, it would be interesting to investigate whether providers are more receptive to these recommendations in the future, as it may take a longer period of time until practitioners begin to change clinical practice to reflect these new recommendations.
The authors have no funding, financial relationships, or conflicts of interest to disclose.
References
- 1. Germino FW. JNC 8: expectations, challenges, and wishes—a primary care perspective. J Clin Hypertens (Greenwich). 2009;11:573–576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. James PA, Oparil S, Carter BL, et al. 2014 evidence‐based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8) [published correction appears in JAMA. 2014;311:1809]. JAMA . 2014;311:507–520. [DOI] [PubMed] [Google Scholar]
- 3. Krakoff LR. Recent guidelines for the management of hypertension: what is missing? Blood Press Monit . 2014;19:189–191. [DOI] [PubMed] [Google Scholar]
- 4. Thomas G, Shishehbor M, Brill D, et al. New hypertension guidelines: one size fits most? Cleve Clin J Med. 2014;81:178–188. [DOI] [PubMed] [Google Scholar]
- 5. Bauchner H, Fontanarosa PB, Golub RM. Updated guidelines for management of high blood pressure: recommendations, review, and responsibility. JAMA. 2014;311:477–478. [DOI] [PubMed] [Google Scholar]
- 6. Navar‐Boggan AM, Pencina MJ, Williams K, et al. Proportion of US adults potentially affected by the 2014 hypertension guideline [published correction appears in JAMA. 2014;312:848]. JAMA. 2014;311:1424–1429. [DOI] [PubMed] [Google Scholar]
- 7. Mitka M. Groups spar over new hypertension guidelines. JAMA. 2014;311:663–664. [DOI] [PubMed] [Google Scholar]
- 8. Myers MG, Tobe SW. A Canadian Perspective on the Eighth Joint National Committee (JNC 8) hypertension guidelines. J Clin Hypertens (Greenwich). 2014;16:246–248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Sox HC. Assessing the trustworthiness of the guideline for management of high blood pressure in adults. JAMA. 2014;311:472–474. [DOI] [PubMed] [Google Scholar]
- 10. Mancia G. Hypertension: strengths and limitations of the JNC 8 hypertension guidelines. Nat Rev Cardiol. 2014;11:189–190. [DOI] [PubMed] [Google Scholar]
- 11. Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure . The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. Hypertension . 2003;42:1206–1252. [DOI] [PubMed] [Google Scholar]
- 12. Neuman MD, Goldstein JN, Cirullo MA, et al. Durability of class I American College of Cardiology/American Heart Association clinical practice guideline recommendations. JAMA. 2014;311:2092–2100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Cabana MD, Rand CS, Powe NR, et al. Why don't physicians follow clinical practice guidelines? A framework for improvement. JAMA. 1999;282:1458–1465. [DOI] [PubMed] [Google Scholar]
- 14. Unverzagt S, Oemler M, Braun K, et al. Strategies for guideline implementation in primary care focusing on patients with cardiovascular disease: a systematic review. Fam Pract. 2014;31:247–266. [DOI] [PubMed] [Google Scholar]


