ABSTRACT
Background
Control of hypertension remains a major unmet need, worldwide.
Hypothesis
To test whether the presence of hypertension may improve global cardiovascular (CV) risk stratification and achievement of therapeutic targets for CV risk factors in adult outpatients in Italy.
Methods
Physicians were asked to submit data covering the first 10 consecutive adult outpatients. All data were centrally analyzed for global CV risk assessment and rates of control of major CV risk factors, mostly blood pressure (BP) levels, in different high‐risk subgroups of hypertensive patients.
Results
Overall, 1078 physicians collected data of 9864 outpatients (46.7% females, age 66.1 ± 10.3 years) with valuable data on BP levels, among which 7147 (72.5%) had a diagnosis of hypertension and 2717 (27.5%) were normotensive subjects. Hypertensive patients were older and had a higher prevalence of major risk factors, including smoking, obesity, dyslipidemia, and family history of cardiovascular disease, as well as comorbidities, than did normotensive subjects (P < 0.001 for all comparisons). Despite worse control of BP (66.9% vs 36.2%, P < 0.001), high‐density lipoprotein cholesterol (40.5% vs 37.4%, P < 0.005), triglycerides (72.1% vs 67.8%, P < 0.001), and fasting plasma glucose (71.2% vs 67.0%, P < 0.005), hypertension was associated with larger availability and frequency of diagnostic examinations and greater use of antihypertensive, glucose‐lowering, and lipid‐lowering drugs, as well as antiplatelet agents, compared with normotension (P < 0.001).
Conclusions
Presence of hypertension significantly improved clinical data collection and CV risk stratification. Such an approach, however, was not paralleled by better control of major CV risk factors.
Introduction
Uncontrolled hypertension remains a major problem for health care systems worldwide, being strictly related to a persistently elevated burden of cardiovascular (CV) morbidity and mortality.1 Randomized controlled clinical trials have demonstrated the clinical benefits obtained by achieving effective and sustained blood pressure (BP) control in terms of reduced incidence of major CV events, independently by age and comorbidities.2, 3, 4 Despite this solid evidence, clinical surveys and observational studies consistently report persistently low rates of BP control in treated hypertensive patients, particularly in those at high or very high CV risk,5, 6, 7, 8, 9 thus leading to an unacceptably high burden of hypertension‐related CV diseases.
In recent years, the possibility has been raised to apply several innovative, Web‐based interventions to improve the clinical management of hypertension and to achieve better BP‐control rates.10, 11 Even the recent sets of European guidelines for the clinical management of hypertension have highlighted the need for implementing multidimensional, integrated, and comprehensive interventions to improve BP control in the hypertensive population.12 This has prompted the need to review awareness, treatment, and control rates of high BP levels in different populations of hypertensive patients at risk for CV diseases and to analyze physicians' attitudes and preferences for the clinical management of these high‐risk hypertensive outpatients.
In the past, we had the opportunity to analyze clinical characteristics and the global CV‐risk profile of adult outpatients included in a large, multicenter, observational study performed in Italy.13, 14, 15, 16 The main findings from these analyses provided useful information on how adult outpatients having multiple concomitant CV risk factors and comorbidities were followed in our country.13, 14, 15, 16 In all these analyses, hypertension represented by far the most frequent concomitant CV risk factor, compared with any other risk factor or clinical condition.13, 14, 15, 16
In the present analysis, we aimed to evaluate to evaluate whether the presence of hypertension may induce a positive outcome: (1) on global CV risk stratification; (2) in achieving the recommended BP targets in different high‐risk subgroups of hypertensive outpatients; and (3) in achieving the recommended therapeutic targets for CV risk factors other than hypertension. Moreover, we also assessed whether the burden and type of clinical examinations for CV risk stratification affect the rate of BP control among hypertensive outpatients.
Methods
The methodology of the study has been previously described.13 Briefly, this was an educational program structured in 2 distinct phases, with the first stage designed to evaluate prevalence of major CV risk factors and the second stage designed to establish the potential influence of an educational intervention on global CV risk management among physicians practicing in Italy. The present article refers to the clinical data available from the first stage of the analysis.
The study conformed to the Declaration of Helsinki and its subsequent modifications and was authorized by the reference ethics committee. The confidentiality of the data was carefully and strictly protected. Written consent to participate to the educational program was obtained by all involved physicians, and confidentiality of demographic and clinical data of all patients was carefully preserved.
Physician Recruitment
To obtain a representative sample of physicians in Italy, participants involved in the program were randomly selected from a community of medical doctors who shared some specific features: (1) experience in data collection and clinical case‐report compilation; (2) routine practice of ≥60 patients per week, on average; and (3) free online access to a remote central database. The physicians were invited to participate in an educational training program aimed at evaluating the efficacy of a clinical problem‐oriented learning approach for improving individual global CV risk management in their routine clinical practice. Thus, involved physicians were blind to the final purposes of the study. Acceptance of this initial invitation placed physicians under no obligation, and physicians were allowed to drop out of the survey at any stage.
Written invitations were forwarded in a sizable number to ensure the study population sample was sufficiently representative and to achieve this target within a period of approximately 3 to 4 weeks. For this purpose, each of the 20 to 24 regional referral centers invited 60 physicians per region (35 general practitioners, 10 diabetologists, and 15 cardiologists) to participate in this survey, for a total of 1400 individual physicians selected on the basis of the above‐mentioned clinical habits and personal characteristics. Then, approximately 1250 invitations were issued, and physicians were asked to complete questionnaires about their characteristics and practice (age, sex, geographic location, professional expertise or specialty, use of electronic or conventional database) and to reply anonymously to their regional referral center.
Following their acceptance, involved physicians were asked to report specific, relevant clinical data extracted from their clinical records from the first 10 consecutive adult Caucasian outpatients age >50 years, for whatever the reason they were referred to their own attending physicians. The entire data collection was completed by participants on‐site and then delivered to the data‐collection center by online access to a remote database. Physicians who completed the program did not receive any compensation for their participation.
Data Collection
Patients' medical history and lifestyle habits were assessed by means of a standardized questionnaire. Information was obtained on current drug therapy for hypertension, dyslipidemia, diabetes mellitus (DM), and other CV diseases, including coronary artery disease (CAD), cerebrovascular disease (CVD), and peripheral artery disease, as well as any concomitant medication.
Clinical systolic and diastolic BP levels, serum lipids, and blood glucose levels were extracted from available clinical records, generally not exceeding 12 months. Information on diagnostic tests including electrocardiograms (ECG), echocardiograms, carotid or peripheral vascular ultrasonography, fundus oculi examination, dosage of microalbuminuria, and exercise stress tests was also recorded by physicians, when available.
Blood‐pressure measurements were performed according to recommendations from European guidelines available at the time of patients' inclusion in the study protocol.17, 18
Data Analysis
Available data were entered into a study‐designed case‐report form and were centrally analyzed. Normal values of clinic and metabolic parameters were defined according to current international guideline recommendations. In particular, specific parameters were defined as under control at the following levels: systolic and diastolic BP, ≤140/90 mm Hg12; total cholesterol, ≤190 mg/dL19; high‐density lipoprotein cholesterol, ≥40 mg/dL in men and ≥50 mg/dL in women20, 21; triglycerides, ≤150 mg/dL20, 21; and fasting glucose level, ≤126 mg/dL.22
According to the recent sets of European guidelines,12 BP control in diabetic patients with hypertension was defined for BP levels ≤140/85 mm Hg, whereas for elderly individuals it has been considered for BP levels from ≤140 to 150/90 mm Hg.
Statistical Analysis
All data were entered into Microsoft Access for Windows (Microsoft Corp, Redmond, WA). Baseline characteristics of patients are presented as number and percentage for dichotomous variables and mean ± SD of the mean for continuous variables. Normal distribution of data was assessed using the Kolmogorov‐Smirnov test. Differences between continuous variables were assessed using the Student t test. Categorical variables were compared among groups by the χ2 test. To evaluate the association among clinical variables, number or type of examinations, and BP control (primary endpoint), hazard ratios and 95% confidence intervals were derived from logistic regression analysis. A multivariable model was fitted with baseline covariates associated with the primary endpoint at the P < 0.05 significance level. All tests were 2‐sided, and P < 0.05 was considered statistically significant. All calculations were generated using SPSS version 15.0 (SPSS Inc., Chicago, IL).
Results
Study Population
The involved population included 1666 physicians, who provided data from an overall sample of 11 470 outpatients, among which 9864 had valuable clinical data on BP levels at baseline. Thus, the present analysis was based on those outpatients who had both systolic and diastolic BP levels recorded on their clinical report form, which represents 86.0% of the initial sample size. Among these outpatients, 7147 (72.5%) had a diagnosis of hypertension and 2717 (27.5%) were reported to be normotensive subjects.
General characteristics of the study population are reported in Table 1. On average, hypertensive outpatients were older and had a higher global CV risk profile than normotensive individuals. In particular, they were more obese, with higher weight, BMI, and waist circumference (P < 0.001 for all comparisons). Also, they had a higher prevalence of major risk factors, including family history of CV disease, smoking habit, dyslipidemia, and DM (P < 0.001 for all comparisons). Hypertension‐related clinical conditions, including CAD (previous myocardial infarction and coronary revascularization), CVD (previous stroke and transient ischemic attack), as well as vascular diseases, were significantly more prevalent in outpatients with hypertension than in those with normal BP levels (P < 0.001 for all comparisons).
Table 1.
General Clinical Characteristics and Prevalence of Major CV Risk Factors and Comorbidities in the Overall Population and in Subgroups of Outpatients With and Without Hypertension
| Overall Population | Normotensive Patients | Hypertensive Patients | P Value | |
|---|---|---|---|---|
| Outpatients, n (%) | 9864 (100.0) | 2717 (27.5) | 7147 (72.5) | <0.001 |
| Female sex, n (%) | 4589 (46.7) | 1288 (47.5) | 3301 (53.7) | 0.287 |
| Age, y | 66.1 ± 10.3 | 63.6 ± 11.3 | 67.1 ± 9.7 | <0.001 |
| Height, cm | 166.5 ± 8.3 | 166.8 ± 8.1 | 166.4 ± 8.3 | 0.033 |
| Weight, kg | 77.6 ± 14.1 | 74.8 ± 14.5 | 78.6 ± 13.9 | <0.001 |
| BMI, kg/m2 | 27.99 ± 4.78 | 26.84 ± 4.86 | 28.41 ± 4.68 | <0.001 |
| Waist circumference, cm | 98.5 ± 15.7 | 95.5 ± 15.5 | 99.5 ± 15.7 | <0.001 |
| SBP, mm Hg | 137.9 ± 15.0 | 130.6 ± 12.9 | 140.7 ± 14.8 | <0.001 |
| DBP, mm Hg | 81.7 ± 8.3 | 78.6 ± 7.4 | 82.8 ± 8.4 | <0.001 |
| FPG, mg/dL | 120.9 ± 41.4 | 117.2 ± 41.0 | 122.3 ± 41.5 | <0.001 |
| HbA1c (%) | 7.1 ± 1.4 | 7.0 ± 1.5 | 7.1 ± 1.4 | 0.133 |
| TOT‐C, mg/dL | 211.9 ± 40.0 | 212.2 ± 41.1 | 211.8 ± 39.6 | 0.721 |
| HDL‐C, mg/dL | 31.3 ± 27.6 | 31.8 ± 28.3 | 31.1 ± 27.3 | 0.255 |
| LDL‐C, mg/dL | 50.9 ± 67.8 | 49.6 ± 67.8 | 51.4 ± 67.9 | 0.241 |
| TG, mg/dL | 98.5 ± 96.6 | 92.3 ± 89.2 | 100.6 ± 99.4 | <0.001 |
| Cr, mg/dL | 0.56 ± 0.58 | 0.50 ± 0.53 | 0.58 ± 0.60 | <0.001 |
| Microalbuminuria, mg/dL | 0.08 ± 0.26 | 0.06 ± 0.23 | 0.10 ± 0.30 | <0.001 |
| Risk factors, n (%) | ||||
| Elderly, age >65 y | 5553 (57.4) | 1267 (47.5) | 4286 (61.1) | <0.001 |
| Family history of CV disease | 2859 (29.0) | 637 (23.4) | 2222 (31.1) | <0.001 |
| Smoking | 3241 (32.9) | 806 (29.7) | 2435 (34.1) | <0.001 |
| Dyslipidemia | 4926 (49.9) | 926 (34.1) | 4000 (56.0) | <0.001 |
| Obesity | 2125 (21.5) | 420 (15.5) | 1705 (23.9) | <0.001 |
| Comorbidities, n (%) | ||||
| DM | 3407 (34.5) | 715 (26.3) | 2692 (37.7) | <0.001 |
| CAD | 2230 (22.6) | 375 (13.8) | 1855 (26.0) | <0.001 |
| MI | 1202 (12.2) | 234 (8.6) | 968 (13.5) | <0.001 |
| AP | 762 (7.7) | 129 (4.7) | 633 (8.9) | <0.001 |
| Coronary revascularization | 883 (9.0) | 186 (6.8) | 697 (9.8) | <0.001 |
| CVD | 606 (6.1) | 86 (3.2) | 520 (7.3) | <0.001 |
| Stroke | 249 (2.5) | 39 (1.4) | 210 (2.9) | <0.001 |
| TIA | 436 (4.4) | 79 (2.1) | 357 (5.2) | <0.001 |
| Carotid atherosclerosis | 433 (4.4) | 58 (0.6) | 375 (3.8) | <0.001 |
| PAD | 1266 (12.8) | 159 (5.9) | 1107 (15.5) | <0.001 |
Abbreviations: AP, angina pectoris; BMI, body mass index; CAD, coronary artery disease; Cr, creatinine; CV, cardiovascular; CVD, cerebrovascular disease; DBP, diastolic blood pressure; DM, diabetes mellitus; FPG, fasting plasma glucose; HbA1c, glycated hemoglobin; HDL‐C, high‐density lipoprotein cholesterol; LDL‐C, low‐density lipoprotein cholesterol; MI, myocardial infarction; PAD, peripheral artery disease; SBP, systolic blood pressure; TG, triglycerides; TIA, transient ischemic attack; TOT‐C, total cholesterol.
Control of Major Cardiovascular Risk Factors
In the overall population, systolic and diastolic BP levels (140.7 ± 14.8/82.8 ± 8.4 vs 130.6 ± 12.9/78.6 ± 7.4 mm Hg, P < 0.001), fasting plasma glucose (122.3 ± 41.5 vs 117.2 ± 41.0 mg/dL, P < 0.001), and triglycerides (100.6 ± 99.4 vs 92.3 ± 89.2 mg/dL, P < 0.001) were higher in the hypertensive than in the normotensive group, whereas no significant differences were found with regard to glycated hemoglobin (HbA1c) and other lipid parameters. Also, serum creatinine (0.58 ± 0.60 vs 0.50 ± 0.53 mg/dL, P < 0.001) and microalbuminuria (0.10 ± 0.30 vs 0.06 ± 0.23 mg/dL, P < 0.001) levels were higher in hypertensive patients than in normotensive individuals.
The recommended therapeutic targets of major CV risk factors were less frequently achieved in hypertensive outpatients than in normotensive individuals, with BP (66.9% vs 36.2%, P < 0.001), high‐density lipoprotein cholesterol (40.5% vs 37.4%, P < 0.005), triglycerides (72.1% vs 67.8%, P < 0.001), and fasting plasma glucose (71.2% vs 67.0%, P < 0.005) significantly lower in the former than in the latter group.
Control of Blood Pressure Levels
The overall population sample was stratified according to the current hypertension classification12: optimal BP (n = 498, 5.0%), normal (n = 1485, 15.1%), high‐normal BP (n = 2703, 27.4%), grade I hypertension (n = 4101, 41.6%), grade II hypertension (n = 892, 9.0%), and grade III hypertension (n = 185, 1.9%).
In the Figure 1, (A) illustrates systolic and diastolic BP levels in different subgroups of patients with hypertension. Systolic BP levels were significantly higher in treated than in untreated hypertensive patients (140.8 ± 14.8 vs 136.8 ± 14.1 mm Hg, P < 0.001) without any significant difference for diastolic BP levels. Among treated outpatients, both systolic and diastolic BP levels were lower in controlled than in uncontrolled hypertensive patients (126.8 ± 7.2/77.3 ± 6.1 vs 148.6 ± 11.0/86.0 ± 7.9 mm Hg, P < 0.001), as expected. No gender differences were reported with regard to systolic and diastolic BP levels. Of note, systolic BP levels were above normal values in all high‐risk groups of hypertensive outpatients, including elderly (141.4 ± 15.0 mm Hg) and those with dyslipidemia (141.0 ± 15.2 mm Hg), DM (141.6 ± 15.1 mm Hg), CVD (140.8 ± 17.2 mm Hg), carotid atherosclerosis (145.3 ± 18.0 mm Hg), and peripheral artery disease (141.5 ± 15.9 mm Hg), with the only exception being CAD. Even in this case, however, systolic BP levels were in the high‐normal range, which has been recently considered to be lower than that recommended for very high‐risk hypertensive patients (139.3 ± 15.2 mm Hg).12 Diastolic BP levels were within the recommended targets in all subgroups of outpatients with hypertension.
Figure 1.
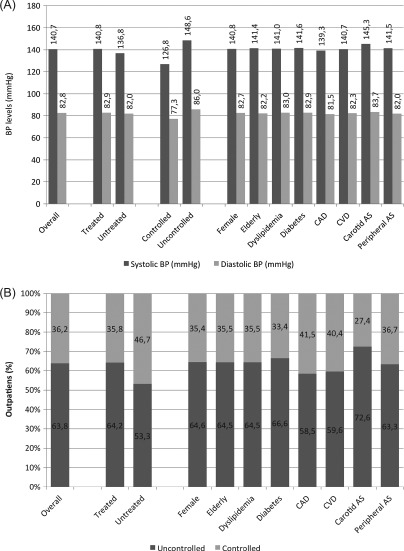
(A) Average systolic/diastolic BP levels in the overall population of hypertensive outpatients and in specific subgroups of treated/untreated, controlled/uncontrolled hypertensive patients, in female or elderly individuals, and in those patients with dyslipidemia, DM, CAD, CVD, carotid AS, and PAD. (B) Proportions of patients achieving recommended target BP levels (<140/90 mm Hg) in treated hypertensive outpatients and in specific subgroups of hypertensive outpatients, including female or elderly individuals and those patients with dyslipidemia, DM, CAD, CVD, carotid AS, and PAD. Abbreviations: AS, atherosclerosis; BP, blood pressure; CAD, coronary artery disease; CVD, cerebrovascular disease; DM, diabetes mellitus; PAD, peripheral artery disease.
Proportions of patients achieving effective BP control, as defined by the most recent sets of European guidelines,12 are shown in (B) of the Figure 1. In the overall population, about 36% of the patients get their systolic/diastolic BP levels within the recommended targets of 140/90 mm Hg. Substantially similar proportions were observed in treated hypertensive patients (35.8%), in elderly individuals (35.5%), and in hypertensive outpatients with dyslipidemia (35.5%), DM (33.4%), carotid atherosclerosis (27.4%), peripheral atherosclerosis (36.7%), CAD (41.5%), and CVD (40.4%), whereas about 47% of untreated hypertensive patients had normal BP levels.
Pharmacological Therapy
As shown in Table 2, nonpharmacological interventions, including smoking cessation, dietary changes, and increased physical activity, were more commonly prescribed to hypertensive outpatients than to normotensive individuals (P < 0.001 for all comparisons).
Table 2.
Lifestyle Recommendations and Pharmacologic Drug Prescriptions in the Overall Population and in Subgroups of Outpatients With and Without Hypertension
| Overall Population, N = 9864 | Normotensive Patients, n = 2717 | Hypertensive Patients, n = 7147 | |
|---|---|---|---|
| Smoking cessation | 1018 (10.3) | 230 (8.5) | 788 (11.0) |
| Dietary | 1637 (16.6) | 378 (13.9) | 1259 (17.6) |
| Physical activity | 1321 (13.4) | 307 (11.3) | 1014 (14.2) |
| BP‐lowering Tx | 7872 (79.8) | 969 (35.7) | 6903 (96.6) |
| ACEIs | 4818 (48.6) | 575 (21.2) | 4243 (59.4) |
| ARBs | 2204 (22.3) | 185 (6.8) | 2019 (28.2) |
| β‐Blockers | 2117 (21.5) | 253 (9.3) | 1864 (26.1) |
| CCBs | 2317 (23.5) | 183 (6.7) | 2134 (29.9) |
| Diuretics | 3211 (32.6) | 330 (12.1) | 2881 (40.3) |
| Glucose‐lowering Tx | 519 (5.3) | 117 (4.3) | 402 (5.6) |
| Insulin | 811 (8.2) | 180 (6.6) | 631 (8.8) |
| Metformin | 1938 (19.6) | 458 (16.9) | 1480 (20.7) |
| Lipid‐lowering Tx | 687 (7.0) | 151 (5.6) | 536 (7.5) |
| Statins | 3884 (39.4) | 826 (30.4) | 3058 (42.8) |
| Fibrates | 181 (1.8) | 48 (1.8) | 133 (1.9) |
| Ezetimibe | 63 (0.6) | 14 (0.5) | 49 (0.7) |
| Omega‐3 | 843 (8.5) | 207 (7.6) | 636 (8.9) |
| Resins | 18 (0.2) | 4 (0.1) | 14 (0.2) |
| Antiplatelet Tx | 1339 (13.6) | 240 (8.8) | 1009 (15.4) |
| ASA | 3472 (35.2) | 647 (23.8) | 2825 (39.5) |
| Clopidogrel | 258 (2.6) | 55 (2.0) | 203 (2.8) |
| Ticlopidine | 712 (7.2) | 146 (5.4) | 566 (7.9) |
| Oral anticoagulant Tx | 431 (4.4) | 75 (2.8) | 356 (5.0) |
| Antiarrhythmic agents | 437 (4.4) | 73 (2.7) | 364 (5.1) |
| Other drugs | 1054 (10.7) | 322 (3.3) | 732 (7.4) |
Abbreviations: ACEI, angiotensin‐converting enzyme inhibitor; ARB, angiotensin II receptor blocker; ASA, aspirin; BP, blood pressure; CCB, calcium channel blocker; Tx, therapy.
Data are presented as n (%) unless otherwise indicated. All differences between the 2 groups were statistically significant at P < 0.001 value, with the exception of glucose‐lowering Tx (P = 0.009), fibrates (P = 0.755), ezetimibe (P = 0.343), omega‐3 (P = 0.042), resins (P = 0.613) and other drugs (P = 0.021).
Nearly 97% of all hypertensive patients were prescribed antihypertensive drugs, whereas about 38% of normotensive subjects received BP‐lowering drugs. In particular, angiotensin‐converting enzyme inhibitors were the most frequently used drug class in both hypertensive and normotensive outpatients, followed by diuretics, calcium channel blockers, angiotensin II receptor blockers, and β‐blockers. All these classes of antihypertensive drugs were more frequently prescribed in the former than in the latter group (P < 0.001 for all comparisons).
Lipid‐lowering agents, including statins, fibrates, cholesterol‐absorption inhibitors, and omega‐3 fatty acids, as well as glucose‐lowering drugs, were more frequently prescribed in hypertensive than in normotensive outpatients (P < 0.001). Also, antiplatelet agents were more frequently prescribed to hypertensive than to normotensive outpatients (P < 0.001). Prescriptions of anticoagulant and antiarrhythmic agents were also higher in outpatients with hypertension than in those without hypertension.
Hypertension and Global Cardiovascular Risk Stratification
Proportions of patients having diagnostic tests and having recent (within 1 year) data on the same diagnostic tests in their own clinical records are reported in Table 3. The presence of hypertension provided a favorable impact on global CV risk stratification among physicians involved in this study, because ECG, echocardiogram, carotid and abdominal Doppler ultrasound, dosage of microalbuminuria, exercise stress test, and fundus oculi examinations all were more frequently prescribed in hypertensive outpatients than in normotensive individuals (P < 0.001 for all comparisons). In addition, hypertensive outpatients had more recent (within 1 year) data on major CV risk factors, including BP, glucose and lipid profiles, and creatinine levels, as well as diagnostic examinations for organ‐damage detection, as compared with testing recorded in normotensive individuals (P < 0.001).
Table 3.
Proportions of Patients Having Diagnostic Tests and Proportions of Patients Having Recent (Within 1 Year) Data on Major CV Risk Factors and Diagnostic Tests in Their Own Clinical Record Form in the Overall Population and in Subgroups of Outpatients With and Without Hypertension
| Overall Population, N = 9864 | Normotensive Patients, n = 2717 | Hypertensive Patients, n = 7147 | |
|---|---|---|---|
| Availability of diagnostic tests, n (%) | |||
| ECG | 7506 (76.1) | 1803 (66.4) | 5703 (79.8) |
| Echocardiogram (Doppler) | 4586 (46.5) | 792 (29.1) | 3794 (53.1) |
| Carotid ultrasound (Doppler) | 3490 (35.4) | 689 (25.4) | 2801 (39.2) |
| Microalbuminuria | 3274 (33.2) | 795 (29.3) | 2479 (34.7) |
| Exercise stress test | 2189 (22.2) | 417 (15.3) | 1772 (24.8) |
| Fundus oculi | 3547 (36.0) | 667 (24.5) | 2880 (40.3) |
| Abdominal echography (%) | 1309 (13.3) | 261 (9.6) | 1048 (14.7) |
| Frequency (<1 year) of major CV risk factors, n (%) | |||
| BP levels (%) | 5260 (53.3) | 1397 (51.4) | 3863 (54.1) |
| FPG | 6493 (65.8) | 1726 (63.5) | 4767 (66.7) |
| HbA1c | 2874 (29.1) | 664 (24.4) | 2210 (30.9) |
| TOT‐C | 6331 (64.2) | 1669 (65.2) | 4662 (61.4) |
| HDL‐C | 5522 (56.0) | 2717 (52.8) | 4087 (57.2) |
| LDL‐C | 4110 (41.7) | 1019 (37.5) | 3091 (43.2) |
| TG | 5729 (58.1) | 1512 (55.6) | 4217 (59.0) |
| Cr | 4772 (48.4) | 1192 (43.9) | 3580 (50.1) |
| Frequency (<1 year) of diagnostic tests, n (%) | |||
| ECG | 4913 (49.8) | 1131 (41.6) | 3782 (52.9) |
| Echocardiogram (Doppler) | 2924 (29.6) | 510 (18.8) | 2414 (33.8) |
| Carotid ultrasound (Doppler) | 2192 (22.2) | 425 (15.6) | 1767 (24.7) |
| Microalbuminuria | 2278 (23.1) | 531 (19.5) | 1747 (24.4) |
| Exercise stress test | 1418 (14.4) | 258 (9.5) | 1160 (16.2) |
| Fundus oculi | 2267 (23.0) | 441 (16.2) | 1826 (25.5) |
| Abdominal echography | 794 (8.0) | 158 (5.8) | 636 (8.9) |
Abbreviations: BP, blood pressure; Cr, creatinine; CV, cardiovascular; ECG, electrocardiogram; FPG, fasting plasma glucose; HbA1c, glycated hemoglobin; HDL‐C, high density lipoprotein cholesterol; LDL‐C, low density lipoprotein cholesterol; TG, triglycerides; TOT‐C, total cholesterol.
All differences between the 2 groups were statistically significant at P < 0.001 value, with the exception of BP levels (P = 0.019), FPG (P = 0.003), and TG (P = 0.003).
Such an approach, however, was not associated with better BP‐control rates in hypertensive outpatients than in normotensive individuals. As shown in Table 4, in univariate analysis, the presence of either obesity or DM, as well as baseline systolic BP levels and number of antihypertensive drugs, were significantly related to BP control; in multivariate analysis, however, only baseline systolic BP levels remained statistically significant.
Table 4.
Univariate and Multivariate Regression Analysis
| Univariate Analysis | Multivariate Analysis | |||
|---|---|---|---|---|
| OR (95% CI) | P Value | OR (95% CI) | P Value | |
| Age, y | 1.001 (0.996‐1.006) | 0.739 | — | — |
| Sex, M/F | 1.065 (0.967‐1.174) | 0.201 | — | — |
| Smoking | 0.931 (0.841‐1.031) | 0.170 | — | — |
| Dyslipidemia | 0.988 (0.897‐1.089) | 0.809 | — | — |
| Obesity | 0.687 (0.611‐0.772) | 0.001 | 0.819 (0.623‐1.078) | 0.155 |
| DM | 0.859 (0.777‐0.950) | 0.003 | 0.983 (0.777‐1.244) | 0.887 |
| Baseline SBP levels | 1.712 (1.665‐1.760) | 0.001 | 1.714 (1.666‐1.762) | 0.001 |
| No. of antihypertensive drugs | 1.134 (1.073‐1.199) | 0.001 | 0.909 (0.794‐1.040) | 0.909 |
| No. of OD diagnostic tests | 0.979 (0.954‐1.005) | 0.106 | — | — |
Abbreviations: CI, confidence interval; DM, diabetes mellitus; F, female; M, male; OD, Organ Damage; OR, odds ratio; SBP, systolic blood pressure.
Discussion
The purpose of this study was to evaluate the impact of hypertension on global CV risk stratification and achievement of therapeutic targets for CV risk factors in adult outpatients in Italy. In the present analysis, we are able to highlight some important differences in not only the distribution and detection of major CV risk factors, but mostly in the clinical management and therapeutic approaches adopted by physicians in the presence or absence of hypertension at baseline observation.
A higher prevalence of major CV risk factors and comorbidities was observed among hypertensive than among normotensive individuals. Because it is widely recognized that physicians' ability to achieve the recommend therapeutic targets largely depends on patients' individual global CV risk profile—the higher the risk, the lower the control rate23, 24, 25—our findings seem to confirm that hypertensive patients at high CV risk achieved the recommended therapeutic targets in lower proportions than those observed for normotensive individuals. Outpatients with hypertension, in fact, achieved therapeutic targets of major CV risk factors in significantly lower proportions compared with normotensive individuals. Of note, these differences seem to be substantially unrelated to the use of diagnostic examinations or CV drugs. In our analysis, in fact, hypertensive patients underwent advanced diagnostic examinations and received pharmacological therapies in significantly higher proportions than did individuals with normal BP profiles.
The differences observed among drug prescriptions between the 2 groups, including BP‐, glucose‐ and lipid‐lowering drugs, as well as antiplatelet agents, may be related to the significantly higher prevalence of hypertension, dyslipidemia, DM, and other comorbidities among hypertensive outpatients than in normotensive individuals. Even in this case, however, the greater use of pharmacological drugs in hypertensive patients was not paralleled by a better control of major CV risk factors as compared with that obtained in normotensive individuals, thus suggesting that aspects other than high BP levels should be taken into account in the clinical management of CV disease, beyond the number of prescriptions and drug dosages.
Treated hypertensive outpatients achieved the recommended target BP levels in relatively low proportions (about 30%) of predefined high‐risk subgroups, and mostly for systolic BP. These findings, which demonstrated the relative difficulty of physicians in lowering systolic BP levels in a setting of real‐world practice, confirmed those reported in other surveys performed at national level.26, 27
Finally, the presence of hypertension seems to provide a favorable impact on increasing physicians' accuracy for clinical data collection and registration, thus confirming our previous observations.28 In a previous analysis of this database, in fact, we found that a significant increase in the proportion of patients treated according to guidelines was observed in those physicians who were more accurate in recording clinical data of their outpatients.28 In the present analysis, the presence of hypertension was associated with higher clinical data availability on major CV risk factors, markers of organ damage, and comorbidities as compared with data reported for normotensive individuals. These discrepancies observed between the 2 groups with regard to clinical data collection and registration may represent, in our opinion, a crucial aspect, which may account for different rates of normal thresholds of major CV risk factors observed in our population sample.
Study Limitations
The present study is based on a cross‐sectional, descriptive survey and, as such, it can only identify associations and cannot provide insights on causation. In some cases, dependence on physician self‐reporting through standardized questionnaires, rather than more objective measures such as BP measurements, may also create potential biases. Information on out‐of‐office BP levels, particularly 24‐hour ambulatory BP monitoring, was not available, thus we cannot provide data on proportions of patients achieving sustained BP control (home and/or 24‐hour ambulatory BP control). About one‐third of normotensive patients received antihypertensive drugs for CV‐related diseases other than hypertension, as well as for noncardiovascular conditions (eg, previous myocardial infarction or stroke, renal disease, vascular disease). Finally, we have data on how many patients had diagnostic examinations for detection of organ damage recorded in their own clinical records, but we have no information on how many patients had signs of hypertension‐related organ damage. These aspects should be considered when interpreting our findings, particularly those addressing physicians' attitudes and preferences for global CV risk stratification.
Conclusion
The presence of hypertension significantly improved clinical data availability, thus confirming a closer attention to global CV risk stratification by physicians when treating outpatients with hypertension than when treating those with a normal BP profile. In the presence of the higher global CV risk and greater use of diagnostic tools for organ‐damage detection and evaluation, hypertensive outpatients have more updated clinical data as compared with data reported on normotensive individuals, which can be translated into a more comprehensive global CV risk stratification. Such an approach, however, was not associated with improved global CV risk management, mostly BP control, in hypertensive outpatients compared with normotensive individuals enrolled in our population sample, particularly with regard to systolic BP levels. Our results may suggest a potential way to reduce the burden of CV disease in hypertension by improving educational interventions among physicians, who have a large number of hypertensive outpatients in their routine clinical practice.
Supporting information
Supporting Appendix
This work was originally supported by an unconditioned educational grant by Merck Sharp and Dohme Italy, for data collection.
The authors thank the Italian physicians involved in this educational program for their contribution to this project (see Supporting Information, Appendix, in the online version of this article for a list of the members of the EFFECTUS Steering Committee).
The authors have no other funding, financial relationships, or conflicts of interest to disclose.
References
- 1. Staessen JA, Wang J, Bianchi G, et al. Essential hypertension. Lancet. 2003;361:1629–1641. [DOI] [PubMed] [Google Scholar]
- 2. Turnbull F, Neal B, Ninomiya T, et al; Blood Pressure Lowering Treatment Trialists' Collaboration. Effects of different regimens to lower blood pressure on major cardiovascular events in older and younger adults: meta‐analysis of randomised trials. BMJ. 2008;336:1121–1123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Turnbull F, Neal B, Algert C, et al; Blood Pressure Lowering Treatment Trialists' Collaboration. Effects of different blood pressure‐lowering regimens on major cardiovascular events in individuals with and without diabetes mellitus: results of prospectively designed overviews of randomized trials. Arch Intern Med. 2005;165:1410–1419. [DOI] [PubMed] [Google Scholar]
- 4. Turnbull F; Blood Pressure Lowering Treatment Trialists' Collaboration. Effects of different blood‐pressure‐lowering regimens on major cardiovascular events: results of prospectively‐designed overviews of randomised trials. Lancet. 2003;362:1527–1535. [DOI] [PubMed] [Google Scholar]
- 5. Bramlage P, Böhm M, Volpe M, et al. A global perspective on blood pressure treatment and control in a referred cohort of hypertensive patients. J Clin Hypertens (Greenwich). 2010;12:666–677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Ignatius J. “RR 160/80” Scipione Riva‐Rocci (1863‐1937) [article in Finnish]. Duodecim. 1993;109:1493–1494. [PubMed] [Google Scholar]
- 7. Prugger C, Keil U, Wellmann J, et al; EUROASPIRE III Study Group. Blood pressure control and knowledge of target blood pressure in coronary patients across Europe: results from the EUROASPIRE III survey. J Hypertens. 2011;29:1641–1648. [DOI] [PubMed] [Google Scholar]
- 8. Chobanian AV. Shattuck Lecture. The hypertension paradox—more uncontrolled disease despite improved therapy [published correction appears in N Engl J Med. 2009;361:1516]. N Engl J Med. 2009;361:878–887. [DOI] [PubMed] [Google Scholar]
- 9. Lee MS, Flammer AJ, Li J, et al. Time‐trend analysis on the Framingham risk score and prevalence of cardiovascular risk factors in patients undergoing percutaneous coronary intervention without prior history of coronary vascular disease over the last 17 years: a study from the Mayo Clinic PCI registry. Clin Cardiol. 2014;37:408–416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Volpe M. The changing role of hypertension societies: shifting gears in Italy. High Blood Press Cardiovasc Prev. 2012;19:1–2. [DOI] [PubMed] [Google Scholar]
- 11. Wenger NK. Prevention of cardiovascular disease: highlights for the clinician of the 2013 American College of Cardiology/American Heart Association guidelines. Clin Cardiol. 2014;37:239–251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Mancia G, Fagard R, Narkiewicz K, et al. 2013 ESH/ESC guidelines for the management of arterial hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J. 2013;34:2159–2219. [DOI] [PubMed] [Google Scholar]
- 13. Volpe M, Tocci G, Avogaro A, et al. Global cardiovascular risk assessment in different clinical settings: basal results of the EFFECTUS (Evaluation of Final Feasible Effect of Control Training and Ultra‐Sensitisation) programme. High Blood Press Cardiovasc Prev. 2009;16:55–63. [Google Scholar]
- 14. Tocci G, Ferrucci A, Guida P, et al; EFFECTUS Steering Committee. Impact of diabetes mellitus on the clinical management of global cardiovascular risk: analysis of the results of the Evaluation of Final Feasible Effect of Control Training and Ultra Sensitization (EFFECTUS) educational program. Clin Cardiol. 2011;34:560–566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Tocci G, Ferrucci A, Guida P, et al; EFFECTUS Steering Committee. Use of electronic support for implementing global cardiovascular risk management: analysis of the results of the EFFECTUS (Evaluation of Final Feasible Effect of Control Training and Ultra Sensitisation) educational programme. High Blood Press Cardiovasc Prev. 2010;17:37–47. [Google Scholar]
- 16. Tocci G, Ferrucci A, Guida P, et al. Global cardiovascular risk management in different Italian regions: an analysis of the Evaluation of Final Feasible Effect of Control Training and Ultra Sensitisation (EFFECTUS) educational program. Nutr Metab Cardiovasc Dis. 2012;22:635–642. [DOI] [PubMed] [Google Scholar]
- 17. Chalmers J, MacMahon S, Mancia G, et al; Guidelines sub‐committee of the World Health Organization. 1999 World Health Organization‐International Society of Hypertension Guidelines for the management of hypertension. Clin Exp Hypertens. 1999;21:1009–1060. [DOI] [PubMed] [Google Scholar]
- 18. Whitworth JA; World Health Organization International Society of Hypertension Writing Group. 2003 World Health Organization (WHO)/International Society of Hypertension (ISH) statement on management of hypertension. J Hypertens. 2003;21:1983–1992. [DOI] [PubMed] [Google Scholar]
- 19. Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive Summary of the Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). JAMA. 2001;285:2486–2497. [DOI] [PubMed] [Google Scholar]
- 20. Grundy SM, Brewer HB Jr, Cleeman JI, et al. Definition of metabolic syndrome: report of the National Heart, Lung, and Blood Institute/American Heart Association conference on scientific issues related to definition. Circulation. 2004;109:433–438. [DOI] [PubMed] [Google Scholar]
- 21. Sesti G, Volpe M, Cosentino F, et al. Metabolic syndrome: diagnosis and clinical management—an official document of the Working Group of the Italian Society of Cardiovascular Prevention (SIPREC), Guest Editor: E. Agabiti Rosei, President of the Italian Society of Hypertension. High Blood Press Cardiovasc Prev. 2006;13:185–198. [Google Scholar]
- 22. Rydén L, Standl E, Bartnik M, et al. Guidelines on diabetes, pre‐diabetes, and cardiovascular diseases: executive summary. The Task Force on Diabetes and Cardiovascular Diseases of the European Society of Cardiology (ESC) and of the European Association for the Study of Diabetes (EASD). Eur Heart J. 2007;28:88–136. [DOI] [PubMed] [Google Scholar]
- 23. Tocci G, Trimarco B, Mancia G, et al. Cardiovascular risk profile in 14 513 patients with essential hypertension followed by Italian specialist physicians. High Blood Press Cardiovasc Prev. 2004;11:165–173. [Google Scholar]
- 24. Volpe M, Notaro LA, Tocci G, et al. The Reassessment of Antihypertensive Chronic Therapy (REACT) Study: an Italian observational study on hypertension management in patients with established therapy. High Blood Press Cardiovasc Prev. 2004;11:175–185. [Google Scholar]
- 25. Mancia G, Ambrosioni E, Rosei EA, et al. Blood pressure control and risk of stroke in untreated and treated hypertensive patients screened from clinical practice: results of the ForLife study. J Hypertens. 2005;23:1575–1581. [DOI] [PubMed] [Google Scholar]
- 26. Tocci G, Rosei EA, Ambrosioni E, et al. Blood pressure control in Italy: analysis of clinical data from 2005–2011 surveys on hypertension. J Hypertens. 2012;30:1065–1074. [DOI] [PubMed] [Google Scholar]
- 27. Volpe M, Tocci G, Trimarco B, et al. Blood pressure control in Italy: results of recent surveys on hypertension. J Hypertens. 2007;25:1491–1498. [DOI] [PubMed] [Google Scholar]
- 28. Giorda CB, Guida P, Avogaro A, et al; EFFECTUS Steering Committee. Association of physicians' accuracy in recording with quality of care in cardiovascular medicine. Eur J Cardiovasc Prev Rehabil. 2009;16:722–728. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting Appendix


