ABSTRACT
There are few data on the risk of exercise and the role of exercise stress testing in Brugada syndrome. We sought to address this deficiency using a systematic literature review. We identified 98 English‐language articles possibly addressing exercise in Brugada syndrome by searching PubMed and Google Scholar from January 1990 through November 2013 using the keywords “Brugada syndrome,” “exercise,” “exercise testing,” and “syncope” alone and in combinations. Abstracts were reviewed, and those articles pertaining to Brugada syndrome and exercise were reviewed in full. We identified 18 articles reporting on Brugada syndrome and exercise. This pool included 2 large studies of 93 and 50 Brugada subjects undergoing exercise testing, plus 16 case reports. There were no reports of exercise‐related sudden death, but there were 4 cases of syncope after exercise. We identified 166 Brugada patients who underwent exercise testing. During exercise testing, there were 2 reports of ventricular tachycardia and 1 report of multiple ventricular extrasystoles. ST‐segment elevation increased (ST augmentation) during the early recovery phase of exercise in 57% of patients. Exercise unmasked a Brugada electrocardiographic pattern in 5 patients. Exercise is associated with syncope and ST augmentation after exercise and may be helpful in unmasking Brugada syndrome. There are insufficient data on the risks of exercise in Brugada syndrome to make recommendations for exercise, but the observations that exercise can worsen the ST abnormalities in Brugada and produce ventricular arrhythmias suggest that patients with Brugada syndrome should be restricted from vigorous exercise.
Introduction
Brugada syndrome was initially described by Pedro and Joseph Brugada in 1992.1 Brugada syndrome is associated with ventricular arrhythmia1 and is estimated to cause 4% of all sudden cardiac deaths. Most patients with Brugada syndrome are diagnosed only after cardiac arrest.2 The electrocardiogram (ECG) patterns in Brugada syndrome (Figure 1) and diagnostic criteria have been described.3 The true prevalence of Brugada syndrome is difficult to assess because it is often concealed and the classic ECG pattern can be transient.4 Brugada syndrome is more prevalent in individuals of Japanese and Southeast Asian descent than of European descent.5, 6, 7, 8
Figure 1.
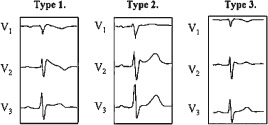
Electrocardiographic patterns in Brugada syndrome. Type 1, coved‐type ST‐segment elevation. Types 2 and 3, saddle‐type ST‐segment elevation. Reproduced from Junttila et al35 by permission of Oxford University Press (license no. 3527220781309).
In contrast to pharmacological provocative testing in Brugada syndrome, which has been extensively studied,9 there are few data on the risk of exercise training and the role of exercise stress testing in Brugada syndrome. Consequently, we performed a systematic review of the role and risk of exercise in Brugada syndrome.
Methods
We identified English‐language articles addressing exercise in Brugada syndrome by searching the PubMed database and Google Scholar from January 1990 through November 2013 using the keywords “Brugada syndrome,” “exercise,” “exercise testing,” “syncope,” “physical exertion,” and “exercise induced” alone and in combinations. Abstracts were reviewed, and those articles pertaining to Brugada syndrome and exercise were reviewed in full. We reviewed the authors of each report to avoid including duplicate reports on the same patient.
Results
Our initial search terms yielded 98 articles possibly relating to exercise and Brugada syndrome. Review of the abstracts reduced this pool to 18 articles (Table 1).
Table 1.
Studies Reporting Brugada Syndrome and Exercise
| Authors | Study Type and Patients | Symptoms Prior to Exercise Testing | Exercise and ECG Findings | Follow‐up |
|---|---|---|---|---|
| Makimoto et al (2010)10 | 93 consecutive patients vs 102 controls | Documented VF, 22; syncope, 35. Asymptomatic, 36. | Group 1: ST augmentation in recovery, 34 (37%). Group 2: no ST changes, 59 (63%). | 76 ± 38 months during follow‐up. Group 1: CE, 15/34 (44%); ICD, 25. Group 2: CE, 10/59 (17%); ICD, 38. |
| Amin et al (2009)11 | 50 subjects vs 35 controls | VF history, 2; syncope, 12. Asymptomatic, 32. | During exercise: QRS widening; QTc prolongation; ST augmentation in early recovery, 50 (100%). | None. ICD, 13. |
| Jayasuriya et al (2011)12 | Case report | Syncope | Baseline: minor ST elevation. Coved‐type ST augmentation in recovery. | VF by EPS; ICD. |
| Archontakis et al (2011)13 | Case report | NA | Baseline: minor ST elevation. Coved‐type ST augmentation in early recovery. | 9 months. Pharmacologic test and EPS. No ICD. |
| Ozeke et al (2009)14 | Case report | NA | Baseline: saddle‐type Brugada ECG. ST augmentation in recovery; hemodynamically stable VT resolved without medication. | NA |
| Papadakis et al (2009)15 | 2 case reports | NA | Baseline: minor ST elevation. Coved‐type ST augmentation in early recovery. | Ajmaline provocative test; ICD. |
| Grimster et al (2008)16 | Case report | Syncope | Baseline: type 2. Type 1 Brugada ECG changes in recovery. | ICD offered |
| Esperer et al (2007)17 | Case report | Syncope | ST augmentation in recovery. | 9 months; ICD. |
| García‐Borbolla et al (2007)18 | Case report | NA | Type 1 Brugada ECG at rest, sustained monomorphic VT in recovery. | 12 months; ICD. |
| Cho et al (2007)19 | Case report | NA | Baseline: normal ST augmentation during exercise. | No ICD |
| Guevara‐Valdivia et al (2003)20 | Case report | Syncope | ST augmentation during exercise with decrease in recovery. | ICD |
| Guevara‐Valdivia et al21 (2001) | Case report | Syncope | ST augmentation in recovery. | No follow‐up; ICD offered. |
| Furuhashi et al (2001)22 | 11 patients | Syncope, 1 | Coved‐type ST augmentation in 1 patient from baseline saddle‐type ECG. No changes in 5, ST normalization in 5. | 2 years |
| Bertaglia et al (1998)23 | Case report | NA | Normal exercise test. | EPS and ICD |
| Valdivia et al (2004)24 | Case report | Exertional syncope | NA | EPS |
| Mok et al (2004)25 | Case report | Exertional syncope | NA | ICD offered |
| Carlsson et al (2000)26 | Case report | Exertional syncope | NA | Pharmacologic test and ICD |
| Frölke et al (2008)27 | Case report | Exertional syncope | NA | Pharmacologic test and EPS, ICD |
Abbreviations: CE, cardiac events; ECG, electrocardiogram, electrocardiographic; EPS, electrophysiology study; ICD, implantable cardioverter‐defibrillator; NA, not available; QTc, corrected QT interval; VF, ventricular fibrillation; VT, ventricular tachycardia.
There were 2 large studies, containing 93 patients10 and 50 patients,11 respectively, along with an additional 12 case reports that addressed Brugada syndrome and exercise testing.12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23 Four reports described exercise‐induced syncope as the initial presentation in Brugada patients.24, 25, 26, 27 An additional study28 evaluated heart‐rate variability in Brugada patients, but it did not provide data on exercise events or ECG changes and thus was excluded.
We identified a total of 166 Brugada patients undergoing exercise testing.10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23 The average age of Brugada patients when exercise testing was performed was 46 years (range, 28–72 years). Of the Brugada patients, 98% were male. Prior to exercise testing being performed, a history of ventricular fibrillation (VF) was present in 24 patients, a history of syncope alone in 52, and a history of palpitations in 6, whereas 86 patients were asymptomatic. Exercise testing produced ECG changes in 101 of 166 (61%) patients, whereas no changes were observed in 65 (39%).
The most frequent ECG change with exercise testing was increasing or augmentation of the ST‐segment elevation (ST augmentation). The ST augmentation was observed in 95 of 166 (57%) Brugada patients. The ST augmentation occurred during early recovery after exercise in 93 Brugada patients,10, 11, 12, 13, 14, 15, 21 whereas 2 patients developed ST augmentation during the effort phase of exercise.19, 20 In 5 patients there was no significant ST elevation in leads V1 through V3 at baseline, but exercise unmasked typical coved‐type 1 ECG changes12, 13, 15, 19 and led to the diagnosis. The ECG pattern changed with exercise from a saddle‐shaped to a coved‐type Brugada pattern in 3 patients with known Brugada.14, 16, 22
Three patients developed ventricular arrhythmias with exercise: 2 developed ventricular tachycardia,14, 18 and 1 developed multiple ventricular extrasystoles.15 All 3 arrhythmias occurred during early recovery after exercise testing and resolved spontaneously.
The majority of data was derived from 2 larger studies. Makimoto et al compared 93 consecutive Brugada syndrome patients with 102 control subjects.10 Brugada syndrome patients were further analyzed according to the presence of ST augmentation during exercise stress testing. ST augmentation during exercise testing was associated with an increased risk of cardiac events in Brugada patients (hazard ratio: 3.17, 95% confidence interval: 1.37‐7.33, P = 0.007). The study was limited to hospitalized patients at a single center in Japan. Amin et al reported a single‐center retrospective analysis of 50 randomly sampled Brugada syndrome patients and 35 age‐ and sex‐matched healthy control subjects.11
Follow‐up data were available for 111 of 166 Brugada patients.10, 13, 17, 18, 22 Sudden cardiac death or aborted cardiac arrest, and VF or sustained ventricular tachyarrhythmia occurred in 15 of 111 (13%) Brugada patients during a mean follow‐up of 75 ± 38 months. An implantable cardioverter‐defibrillator was offered to 85 patients and implanted in 83 patients.10, 11, 12, 15, 17, 18, 20, 23 A history of VF and exercise‐induced ST augmentation were independent predictors10 of subsequent sudden cardiac death or aborted cardiac arrest, VF, or sustained ventricular tachycardia.
Discussion
We reviewed the literature on the role and risks of exercise in Brugada syndrome. We were able to identify only 18 relevant articles: 2 large studies and 16 case reports including a total of 170 Brugada patients. Syncope after physical exercise was the initial presentation in 4 patients. Exercise testing produced increases in ST‐segment elevation in 57% of patients, predominantly during the early recovery phase of exercise. Exercise also unmasked the Brugada ECG pattern in 5 patients and worsened ventricular arrhythmia in 3 cases.
Risk stratification in Brugada syndrome remains inexact. The relative risk of syncope, arrhythmic death, or implantable cardioverter‐defibrillator shocks was 3.2 (95% confidence interval: 2.13‐4.93) higher over 32 months in Brugada patients with a history of syncope or aborted sudden cardiac death compared with asymptomatic Brugada patients.29 However, even in the absence of a history of cardiac arrest, patients still have a risk for sudden arrhythmic death.30 More than 80% of patients with Brugada syndrome have symptoms at night during sleep or rest.28 There are only a few case reports regarding symptoms with exercise in Brugada syndrome and ST augmentation during the recovery phase of exercise with exercise testing. Two relatively larger studies10, 11 have documented that exercise augments ST elevation, especially early in recovery, and that ST augmentation is a risk factor for subsequent cardiac events, but the role of routine exercise testing both to detect Brugada patients and to predict their risk for cardiac death requires further study.
We were unable to find evidence directly linking physical exercise or exercise training to cardiac events in Brugada syndrome. Nevertheless, the limited data that exercise can cause syncope, produce ST augmentation, and provoke ventricular arrhythmias in this population suggest that exercise should be considered a risk factor for these patients until proven otherwise.
The increase in ST segment immediately after exercise is likely due to increased parasympathetic tone, because vagal reactivation occurs soon after exercise.31 This is consistent with the observation that VF in Brugada patients occurs more frequently during sleep, when vagal tone is also increased, than while awake (87% vs 13%).32 This possible role of parasympathetic tone also suggests that exercise training potentially could be detrimental in Brugada. Exercise training increases parasympathetic tone, which theoretically could increase the risk of ventricular arrhythmia in Brugada patients.
Present recommendations for physical activity and sports participation in Brugada patients33, 34 suggest that such patients avoid participating in high‐intensity sports based on expert opinion. This systematic review found very few articles on the effect of exercise and exercise training in patients with Brugada syndrome. Our results and conclusions are necessarily based on these few articles, and these reports may be affected by publication bias. Publication bias refers to the possibility that patients with abnormal responses to exercise are more likely to be reported in the literature. We cannot determine how many Brugada patients with subtle ECG patterns underwent exercise testing with unremarkable findings and were not reported. Our review is also dependent on the assumption that Brugada was diagnosed correctly by the authors of the original manuscripts.
Conclusion
The observations that exercise can worsen the ST abnormalities in Brugada syndrome and produce ventricular arrhythmias, plus the probability that enhanced parasympathetic tone is both a risk factor in Brugada and an effect of exercise training, suggest that patients with Brugada syndrome should be restricted from vigorous exercise and exercise training until further studies confirm or disprove this recommendation.
Paul D. Thompson, MD, has served as an unpaid advisor for Runner's World and owns stock in General Electric, which makes electrocardiographic and exercise stress testing equipment. Shihab Masrur, MD, and Sarfaraz Memon, MD, have no conflicts of interest to disclose.
References
- 1. Brugada P, Brugada J. Right bundle branch block, persistent ST segment elevation and sudden cardiac death: a distinct clinical and electrocardiographic syndrome. A multicenter report. J Am Coll Cardiol. 1992;20:1391–1396. [DOI] [PubMed] [Google Scholar]
- 2. Paul M, Gerss J, Schulze‐Bahr E, et al. Role of programmed ventricular stimulation in patients with Brugada syndrome: a meta‐analysis of worldwide published data. Eur Heart J. 2007;28:2126–2133. [DOI] [PubMed] [Google Scholar]
- 3. Antzelevitch C, Brugada P, Borggrefe M, et al. Brugada syndrome: report of the second consensus conference: endorsed by the Heart Rhythm Society and the European Heart Rhythm Association [published correction appears in Circulation. 2005;112:e74]. Circulation. 2005;111:659–670. [DOI] [PubMed] [Google Scholar]
- 4. Brugada J, Brugada P, Brugada R. The syndrome of right bundle branch block ST segment elevation in V1 to V3 and sudden death—the Brugada syndrome. Europace. 1999;1:156–166. [DOI] [PubMed] [Google Scholar]
- 5. Miyasaka Y, Tsuji H, Yamada K, et al. Prevalence and mortality of the Brugada‐type electrocardiogram in one city in Japan. J Am Coll Cardiol. 2001;38:771–774. [DOI] [PubMed] [Google Scholar]
- 6. Greer RW, Glancy DL. Prevalence of the Brugada electrocardiographic pattern at the Medical Center of Louisiana in New Orleans. J La State Med Soc. 2003;155:242–246. [PubMed] [Google Scholar]
- 7. Hermida JS, Lemoine JL, Aoun FB, et al. Prevalence of the Brugada syndrome in an apparently healthy population. Am J Cardiol. 2000;86:91–94. [DOI] [PubMed] [Google Scholar]
- 8. Centers for Disease Control and Prevention . Sudden, unexpected, nocturnal deaths among Southeast Asian refugees. MMWR Morb Mortal Wkly Rep. 1981;30:581–584, 589. [PubMed] [Google Scholar]
- 9. Obeyesekere MN, Klein GJ, Modi S, et al. How to perform and interpret provocative testing for the diagnosis of Brugada syndrome, long‐QT syndrome, and catecholaminergic polymorphic ventricular tachycardia. Circ Arrhythm Electrophysiol. 2011;4:958–964. [DOI] [PubMed] [Google Scholar]
- 10. Makimoto H, Nakagawa E, Takaki H, et al. Augmented ST‐segment elevation during recovery from exercise predicts cardiac events in patients with Brugada syndrome. J Am Coll Cardiol. 2010;56:1576–1584. [DOI] [PubMed] [Google Scholar]
- 11. Amin AS, de Groot EA, Ruijter JM, et al. Exercise‐induced ECG changes in Brugada syndrome. Circ Arrhythm Electrophysiol. 2009;2:531–539. [DOI] [PubMed] [Google Scholar]
- 12. Jayasuriya C, Whitman M. Exercise‐induced Brugada sign. Europace. 2011;13:446–447. [DOI] [PubMed] [Google Scholar]
- 13. Archontakis S, Gatzoulis K, Arsenos P, et al. A case of asymptomatic Brugada electrocardiographic pattern incidentally unmasked during the recovery phase of an exercise stress test. Hosp Chron. 2011;6:200–202. [Google Scholar]
- 14. Ozeke O, Cağli KE, Aras D, et al. Exercise‐induced ventricular tachycardia associated with asymptomatic Brugada syndrome in a patient with urinary bladder stone [article in Turkish]. Turk Kardiyol Dern Ars. 2009;37:128–131. [PubMed] [Google Scholar]
- 15. Papadakis M, Petzer E, Sharma S. Unmasking of the Brugada phenotype during exercise testing and its association with ventricular arrhythmia on the recovery phase. Heart. 2009;95:2022. [DOI] [PubMed] [Google Scholar]
- 16. Grimster A, Segal OR, Behr ER. Type I Brugada electrocardiogram pattern during the recovery phase of exercise testing. Europace. 2008;10:897–898. [DOI] [PubMed] [Google Scholar]
- 17. Esperer HD, Hoos O, Hottenrott K. Syncope due to Brugada syndrome in a young athlete. Br J Sports Med. 2007;41:180–181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. García‐Borbolla M, García‐Borbolla R, Valenzuela LF, et al. Ventricular tachycardia induced by exercise testing in a patient with Brugada syndrome [article in Spanish]. Rev Esp Cardiol. 2007;60:993–994. [DOI] [PubMed] [Google Scholar]
- 19. Cho JH, Cho D, Choi J, et al. An unusual case of exercise‐induced idiopathic Brugada electrocardiographic pattern. Korean Circ J. 2007;37:517–519. [Google Scholar]
- 20. Guevara‐Valdivia ME, de Micheli A, Iturralde P, et al. Infrequent electrocardiographic changes during exercise stress test in a patient with Brugada's syndrome [article in Spanish]. Arch Cardiol Mex. 2003;73:212–217. [PubMed] [Google Scholar]
- 21. Guevara‐Valdivia ME, Iturralde Torres P, de Micheli A, et al. Electrocardiographic changes during stress test in a patient with “Brugada syndrome” [article in Spanish]. Arch Cardiol Mex. 2001;71:66–72. [PubMed] [Google Scholar]
- 22. Furuhashi M, Uno K, Tsuchihashi K, et al. Prevalence of asymptomatic ST segment elevation in right precordial leads with right bundle branch block (Brugada‐type ST shift) among the general Japanese population. Heart. 2001;86:161–166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Bertaglia E, Michieletto M, Spedicato L, et al. Right bundle branch block, intermittent ST segment elevation and inducible ventricular tachycardia in an asymptomatic patient: an unusual presentation of the Brugada syndrome? G Ital Cardiol. 1998;28:893–898. [PubMed] [Google Scholar]
- 24. Valdivia CR, Tester DJ, Rok BA, et al. A trafficking defective, Brugada syndrome‐causing SCN5A mutation rescued by drugs. Cardiovasc Res. 2004;62:53–62. [DOI] [PubMed] [Google Scholar]
- 25. Mok NS, Chan NY. Brugada syndrome presenting with sustained monomorphic ventricular tachycardia. Int J Cardiol. 2004;97:307–309. [DOI] [PubMed] [Google Scholar]
- 26. Carlsson J, Erdogan A, Rolf A, et al. Recurrent syncope in a 34‐year‐old woman triathlete [article in German]. Dtsch Med Wochenschr. 2000;125:1074–1078. [DOI] [PubMed] [Google Scholar]
- 27. Frölke JP, Bruggeman AW, Klomp FP, et al. Brugada syndrome during physical therapy: a case report. Cases J. 2008;1:107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Krittayaphong R, Veerakul G, Nademanee K, et al. Heart rate variability in patients with Brugada syndrome in Thailand. Eur Heart J. 2003;24:1771–1778. [DOI] [PubMed] [Google Scholar]
- 29. Gehi AK, Duong TD, Metz LD, et al. Risk stratification of individuals with the Brugada electrocardiogram: a meta‐analysis. J Cardiovasc Electrophysiol. 2006;17:577–583. [DOI] [PubMed] [Google Scholar]
- 30. Brugada J, Brugada R, Brugada P. Determinants of sudden cardiac death in individuals with the electrocardiographic pattern of Brugada syndrome and no previous cardiac arrest. Circulation. 2003;108:3092–3096. [DOI] [PubMed] [Google Scholar]
- 31. Arai Y, Saul JP, Albrecht P, et al. Modulation of cardiac autonomic activity during and immediately after exercise. Am J Physiol. 1989;256(1 part 2):H132–H141. [DOI] [PubMed] [Google Scholar]
- 32. Matsuo K, Kurita T, Inagaki M, et al. The circadian pattern of the development of ventricular fibrillation in patients with Brugada syndrome. Eur Heart J. 1999;20:465–470. [DOI] [PubMed] [Google Scholar]
- 33. Maron BJ, Chaitman BR, Ackerman MJ, et al. Recommendations for physical activity and recreational sports participation for young patients with genetic cardiovascular diseases. Circulation. 2004;109:2807–2816. [DOI] [PubMed] [Google Scholar]
- 34. Maron BJ, Zipes DP, et al. Introduction: eligibility recommendations for competitive athletes with cardiovascular abnormalities—general considerations. J Am Coll Cardiol. 2005;45:1318–1321. [DOI] [PubMed] [Google Scholar]
- 35. Junttila MJ, Raatikainen M, Karjalainen J, et al. Prevalence and prognosis of subjects with Brugada‐type ECG pattern in a young and middle‐aged Finnish population. Eur Heart J. 2004;25:874–878. [DOI] [PubMed] [Google Scholar]


