ABSTRACT
The acetylcholine (ACh) spasm provocation test proposed by Yasue, Okumura et al more than a quarter‐century ago has become a popular method for induction of coronary spasm. This test is safe and has a low rate of complications. However, it may be limited in its ability to document attacks in daily life because previously it was the gold‐standard method for diagnosing active variant angina. There may be some clinical issues to modify for the next generation of cardiologists. A maximal ACh dose of 50/100 µg in the right coronary artery/left coronary artery is recommended in the Japanese Circulation Society guidelines. We often experienced the usefulness of a maximal ACh dose of 80/200 µg for the induction of coronary spasm in some cases with low or moderate disease activity. It may be necessary to reconsider the maximal ACh dose as a modified method for today's real‐world clinical practice. In young patients with rest angina, intracoronary injection of ACh is less sensitive for diagnosis; in these cases, we recommend performing sequential spasm provocation tests. Especially in female patients, to document coronary artery spasm we recommend performing ACh tests first, instead of ergonovine tests, due to the supersensitivity of ACh. We also recommend supplementary use of ACh and ergonovine. This review summarizes our experiences with the ACh spasm provocation test over a period of 24 years. We have found it to be a reliable and useful method for contributing a variety of clinical information and recommend it to the next generation of cardiologists.
Introduction
Coronary artery spasm may be involved in the genesis of various cardiac disorders, such as acute coronary syndrome, unstable angina, serious fatal arrhythmia, sudden cardiac death, syncope, transient heart failure, and atypical chest pain.1, 2, 3, 4, 5, 6, 7 As clinical noninvasive methods, we employ 24‐hour Holter recording, exercise testing, the hyperventilation test, cold stress test, and cardiac scintigraphy.8, 9, 10 However, we often cannot obtain ischemic electrocardiographic (ECG) changes by performing these noninvasive methods in patients with low disease activity. In these clinical situations, we decided to perform spasm provocation tests in patients suspected of coronary spastic angina (CSA). As an invasive method, we perform intracoronary (IC) injection of acetylcholine (ACh) and ergonovine (ER) in the cardiac catheterization laboratory. Yasue and Okumura reported the usefulness of the ACh spasm provocation test in patients with variant angina more than 25 years ago.11, 12, 13 The sensitivity and specificity of the ACh spasm provocation test in active variant angina were >90%. Because the half‐life of ACh is remarkably short, the provoked coronary spasm resolves spontaneously within a few minutes in most patients, without administration of nitrates, and therefore we can diagnose more spasms than with an ER test. We employ the ACh spasm provocation test to diagnose all CSA—not only variant angina showing transient ST‐segment elevation, but also nonvariant angina with all CSA except for variant angina.
The Japanese Circulation Society (JCS) guideline for CSA was established in 2008.14 In this review, we reexamine the clinical usefulness of the ACh spasm provocation test proposed by Yasue and Okumura and summarize clinically important issues concerning the procedure, complications, the incidence of provoked spasm in various cardiac disorders, and limitations of the ACh test.
Our Experience of 24 Years
We performed ACh spasm provocation tests from January 1991 through December 2013 in 1546 patients (1090 male; mean age, 64.8 ± 10.7 years), consisting of 1065 patients with ischemic heart diseases and 481 with nonischemic heart diseases. During this period, we performed a total of 7302 coronary angiography procedures, including 1872 percutaneous coronary intervention (PCI) procedures and 5430 diagnostic/follow‐up cardiac catheterizations. We performed ACh spasm provocation tests in more than a quarter of patients with diagnostic/follow‐up catheterization (1546/5430, 28.5%). During the same period, we also performed selective ER spasm provocation tests in 1114 patients. We tried to perform the selective spasm provocation tests to examine the incidence of provoked spasm in patients who had undergone coronary angiography as much as possible. We also performed both ACh and ER tests in 461 patients, adding IC injection of ACh after an ER test in 240 patients.
History of the Acetylcholine Test
Stein et al first reported the usefulness of intravenous (IV) injection of ER in diagnosing coronary insufficiency in 1949.15 In 1972, the first ER spasm provocation test in the world was employed at the Cleveland Clinic during cardiac catheterization.16 Hackett et al and Ishise et al reported the usefulness of IC administration of ER instead of IV injection of ER in 1987.17, 18 In contrast, Yasue et al reported that subcutaneous injection of methacholine, an analog of ACh and the neurotransmitter of the parasympathetic nervous system, induced an attack of variant angina or coronary artery spasm in 1974.19 And also they reported that atropine, a parasympatholytic agent, suppressed the attack in some patients with variant angina. Subsequently, Endo reported the coronary arteriogram and ventriculogram during attack induced by methacholine in Prinzmetal variant angina in 1976.20 Yasue et al reported that IC injection of ACh induced coronary spasm and attack in patients with variant angina and that the activity of the parasympathetic nervous system may play a role in the pathogenesis of coronary spasm in 1986.21 Okumura and Yasue et al reported that sensitivity of the IC injection of ACh was 90% in variant angina and specificity of the IC injection of ACh was 99%, and that multivessel coronary spasm was often observed in patients with variant angina by using IC injection of ACh in 1988.11, 12 Since then, the ACh spasm provocation test proposed by Yasue, Okumura et al has superseded IV injection of ER as the standard test for the induction of coronary artery spasm in the cardiac catheterization laboratory in Japan. The spasm test is not broadly employed outside of Asia; for example, it is not done in Europe or the United States except in a few specialized centers. Previously, IC injection of ACh was the gold standard for diagnosing variant angina, but now we employ this method to document coronary artery spasm in patients with not only variant angina, but also nonvariant angina.
The Acetylcholine Spasm Provocation Test
Procedure
The JCS guidelines recommended that cardiologists should perform the ACh spasm provocation test after patients have discontinued medications for ≥48 hours.14 However, to avoid precipitating cardiac events due to coronary spasm because patients are off medications before admission, we have employed ≥24 hours' cessation of medications before performing the test. We recommend performing the ACh spasm provocation test in the morning whenever possible. A bipolar electrode catheter is inserted into the right ventricular apex through the femoral vein or antecubital vein and is connected to a temporary pacemaker set at the rate of 45 beats/min. Provocation of coronary artery spasm is performed with an IC injection of ACh. Acetylcholine chloride (Neucholin‐A, 30 µg/2 mL; Zeria Seiyaku, Tokyo, Japan) is injected in incremental doses of 20 and 50 µg into the right coronary artery (RCA) and of 20, 50, and 100 µg into the left coronary artery (LCA) over 20 seconds, with at least a 3‐minute interval between injections, according to the original method proposed by Yasue and Okumura. In addition, we employ the maximal dose of 80 µg into the RCA and 200 µg into the LCA if the first injections do not provoke spasm. We do not recommend a single bolus injection of ACh, to avoid severe complications. Coronary arteriography is performed when either ST‐segment changes or chest pain (or both) occur, or after 1 minute following the completion of each injection. Intracoronary injection of ACh into the responsible vessel is not performed if coronary artery spasm occurs spontaneously during coronary angiography. When a coronary spasm is induced and does not resolve spontaneously within 3 minutes after the completion of ACh injection, or when hemodynamic instability due to the coronary spasm occurs, 2.5 to 5.0 mg of isosorbide dinitrate is injected into the responsible vessel. During the study, arterial blood pressure and an ECG are continuously monitored on an oscilloscope. A standard 12‐lead ECG is recorded every 30 seconds. Other centers use continuous and simultaneous 12‐lead ECG registrations; it is essential to use 12 leads to be able to detect ischemic changes. We recommend performing frequent test shots at about 30‐second intervals with a contrast medium during ACh testing, if possible. We also recommend trying to perform coronary angiography before coronary spasm with complete obstruction is induced by pharmacologic agents. Moreover, ECG changes should be checked without administration of contrast medium, ACh, or saline into the responsible vessel for at least 30 to 60 seconds. We should report the ACh test as negative but not negative for coronary spasm when IC injection of ACh dose not provoke spasm.
Positive Spasm Definition and Spasm Configuration
According the JCS guidelines,14 positive coronary artery spasm is defined as transient luminal narrowing >90% and ischemic ECG findings. A finding of usual chest pain is not always a requirement. Approximately 25 years ago, positive coronary artery spasm was defined in our institutions as transient luminal narrowing >90% with ischemic ECG findings or usual chest pain. In the majority of hospitals in Japan, the above criteria were employed in the cardiac catheterization laboratory. A few patients diagnosed in the past with positive coronary artery spasm according to the above criteria may classify as suspected but not definite coronary spasm based on the JCS guidelines today. Some cardiologists employed ≥75% transient luminal narrowing as an angiographically positive spasm with the ACh spasm provocation test. However, this positive spasm definition may lead to false‐positive in some patients. We believe that angiographically positive spasm requires ≥90% stenosis in the clinical findings. Patients with catheter‐induced spasms should be excluded. Catheter‐induced spasm is often observed in the RCA proximal (segment 1) and rarely in left main trunks (segment 5). In these situations, after spontaneous relief without administration of nitrates, you should perform the ACh spasm provocation test. As configuration of provoked spasms, we often recognize diffuse transient narrowing during ACh spasm provocation tests. Focal spasm is defined as a discrete transient vessel narrowing of >90% localized in the major and branch coronary artery. Diffuse spasm is diagnosed when a transient vessel narrowing is ≥90% compared with the baseline coronary angiography observed from the proximal to the distal segment in the 3 major coronary arteries and branches. Angiographically evident stenosis of positive spasm, the spasm site according to the American Heart Association (AHA) classification,22 the spasm configuration, and real‐time symptoms except for chest pain or pressure are necessary issues for the ACh spasm provocation test summary.
Indications and Exclusion Criteria
The provocation test is not performed if patients have left main narrowing (>50%), triple‐vessel disease, 2‐vessel disease with total occlusion, heart failure (New York Heart Association class III or IV), renal failure (creatinine >2.0 mg/dL), or severe bronchial asthma; if spontaneous spasm is found; or if isosorbide dinitrate is initially used to relieve spasms in the coronary artery tested. We also do not perform spasm provocation tests if the patient will undergo multiple coronary angioplasties or bypass surgery. However, for patients with multiple organic stenosis and rest angina, we recommend performing the ACh spasm provocation test to clarify the presence of coronary spasm. According to the JCS guidelines,14 the ACh spasm provocation test during coronary angiography performed in patients in whom CSA is suspected based on symptoms, but who have not been diagnosed with coronary spasm by noninvasive evaluations, is classified as class I. In contrast, in patients without symptoms suggestive of CSA, the ACh spasm provocation test is classified as class III. However, we have performed the ACh spasm provocation test as much as possible when we suspect coronary artery spasm (except in patients with the above exclusion criteria), because coronary artery spasm may be present irrespective of atypical or silent symptoms.
Chest Symptoms During the Acetylcholine Spasm Provocation Test
During ACh spasm provocation tests, some patients complain of unusual chest pain and pressure even though a typical positive spasm is obtained. In our data, about 80.3% of patients with positive spasm (≥90%) complained of usual chest pain. This result was similar to the data by Sato et al (67%).23 However, the remaining patients did not complain of usual chest symptoms despite documenting a typical positive spasm. Moreover, some patients reported less usual chest pain. This is one of the limitations of the ACh spasm provocation test. We do not always document usual chest symptoms by performing ACh spasm provocation tests. We should understand the test's limitations.
Maximal Acetylcholine Dose
The JCS guidelines specify a maximal ACh dose of 50 µg in the RCA and 100 µg in the LCA.14 In patients with variant angina, sensitivity and specificity under these maximal ACh doses were >90%. However, we perform the ACh spasm provocation test proposed by Yasue and Okumura in patients with not only variant angina, but also nonvariant angina. We may have a negative ACh result in patients with CSA who have low or moderate disease activity (but not high disease activity). If a positive spasm is not obtained using the standard maximal dose, we recommend IC injection of 80 µg of ACh in the RCA and 200 µg of ACh in the LCA in patients highly suspected of having coronary artery spasm.24 However, we should take care for false‐positive results, keeping in mind that we diagnose coronary spasm not through the results of the ACh spasm provocation test alone, but also using other noninvasive evaluations and the clinical background of each patient. In approximately 20% to 25% of patients with negative spasm under the standard maximal dose, a positive spasm is obtained with 80 µg of ACh in the RCA and 200 µg of ACh in the LCA (Figure 1). We should reconsider the maximal ACh dose in patients with nonvariant angina in the future.
Figure 1.
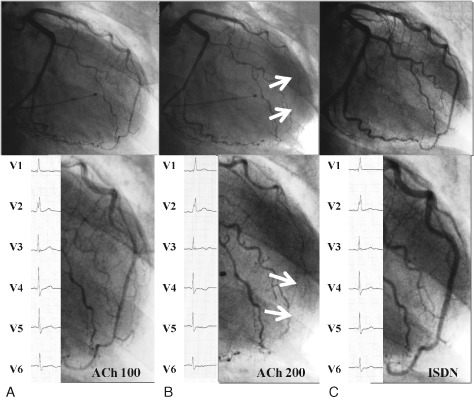
Representative case documenting spasm by IC injection of 200 µg of ACh but not 100 µg in the LCA. Patient is an 84‐year‐old male with a chief complaint of chest pressure at rest beginning 6 months ago. Neither usual chest pressure/ischemic ECG changes nor positive spasm were observed by ACh 100 µg administration into the LCA (A), whereas usual chest pressure, ischemic ECG change (ST‐segment depression in V4 through V6), and subtotal spasm on the distal LAD were recognized by ACh 200 µg injection (B). His LCA (C) had no organic stenosis. We could diagnose CSA by the administration of ACh 200 µg in this case. Abbreviations: ACh, acetylcholine; CSA, coronary spastic angina; ECG, electrocardiogram; IC, intracoronary; ISDN, isosorbide dinitrate; LAD, left anterior descending artery; LCA, left coronary artery.
Acetylcholine Test Procedures in the Real World
Intracoronary Injection of Nitrates to Relieve Provoked Spasm on the First Attempt
Intracoronary administration of nitrates was performed to relieve spasms on the first attempt of ACh testing in 1.49% of patients (13/873). In contrast, IC administration of nitrates before performing another coronary artery test was necessary to relieve spasms induced by the selective ER test in 5.04% of patients (32/654). The incidence of the need for injection of nitrates on the first attempt during ACh testing was significantly lower than it was for selective ER testing. In all 1546 patients undergoing ACh testing, 31 patients (2.0%) required administration of nitrates on the first attempt. Multiple spasms were more often observed on the first attempt in the LCA rather than the RCA (78.6% vs 11.8%; P < 0.001). Even after the administration of nitrates to relieve provoked spasms on the first attempt, positive coronary spasm was obtained in 21.1% of patients in another coronary artery using ACh. We recommend performing the ACh spasm provocation test in another coronary artery even if IC nitrate was administered to relieve provoked spasms on the first attempt, and we also recommend performing the ACh spasm provocation test first in the LCA, not in the RCA.
Temporary Pacemaker Insertion During Acetylcholine Testing
Because IC injection of ACh causes transient atrioventricular block due to parasympathetic action of ACh, the JCS guidelines recommend the insertion of a temporary pacemaker. Especially often in the RCA, and sometimes in the LCA, we experience right ventricle pacing rhythm during ACh testing. Ong et al reported that transient atrioventricular block was frequently observed and occurred mostly during provocation of the RCA; it always resolved within seconds after reducing the speed of the ACh injection, due to the short half‐life of ACh.25, 26 They first performed the ACh spasm provocation test in the LCA, and if that provoked a positive spasm, they did not perform the ACh test in the RCA. Thus, they might not always perform ACh spasm provocation tests on both coronary arteries. We administered the IC injection of ACh over 20 seconds based on the JCS guidelines; however, Ong et al injected the IC ACh into the responsible vessels for 3 minutes. Our employed methods proposed by Yasue and Okumura were different from the method used by Ong et al. We recommend the insertion of a temporary pacemaker during ACh testing when performing ACh procedures based on the JCS guidelines.
The Incidence of Abnormal Coronary Response and Provoked Spasm
Abnormal Coronary Response With Acetylcholine Testing
Abnormal coronary response on ACh testing is observed in patients with early coronary atherosclerosis.27, 28 We retrospectively analyzed the abnormal response rate during 17 years (January 1991 to December 2007) of spasm provocation tests in 2093 consecutive patients (1198 ACh and 895 ER).29 Abnormal response was defined as transient luminal narrowing >90% with or without ischemic ECG changes or chest symptoms during the spasm provocation tests. The incidence of metabolic syndromes such as hypertension, dyslipidemia, and diabetes mellitus was significantly increased in the latter period (January 2001 to December 2007) compared with that in the former period (January 1991 to December 2000). The values of total cholesterol, triglycerides, and fasting blood sugar were also significantly increased in the latter period. The frequency of abnormal coronary response to ACh in the latter period was significantly higher than that in the former period (60.0% vs 34.0%; P <0.01), whereas there was no difference concerning abnormal response to ER between the 2 periods (31.9% vs 30.7%; not significant). The prevalence of abnormal coronary responses to ER was not different in proportion as time passed, whereas the prevalence of abnormal coronary response by ACh was significantly increased as time passed. Damage to coronary vascular smooth muscle may not always be observed, whereas coronary endothelial dysfunction may be frequently recognized in Japanese patients. The frequency of coronary artery spasm may decrease due to the administration of statins by way of Rho kinase inhibition, according to the report of Yasue et al.30 We should lower the level of total cholesterol, triglycerides, and blood sugar. If the prevalence of dyslipidemia and diabetes mellitus decreases in the future in Japan, the prevalence of abnormal responses may fall and coronary endothelial dysfunction may improve. According to the JCS guidelines, smoking cessation, blood pressure control, maintenance of ideal body weight, correction of impaired glucose tolerance, correction of lipid abnormalities, avoidance of excessive fatigue and mental stress, and no or moderate drinking are classified as class I.
Incidence of Provoked Spasm
We reported the frequency of provoked coronary artery spasm in patients undergoing coronary arteriography with ACh spasm provocation testing in 685 consecutive patients in 1999.31 Coronary artery spasm was evident in 221 patients (32.3%). In patients with ischemic heart disease, the frequency of spasm was 45.7%. Spasm occurred often during effort and rest in patients with angina (25/51, 49%), effort angina (25/74, 33.8%), recent myocardial infarction (30/80, 37.5%), healed myocardial infarction (14/37, 37.8%), and especially in patients with rest angina (83/124, 66.9%), whereas spasm was relatively uncommon in patients with nonischemic heart disease (23/252, 9.1%). Spasm was superimposed on significant atherosclerotic lesions in 35.9% of patients and on nonfixed atherosclerotic lesions in 30.8%. There were no other articles concerning the incidence of provoked spasm of ACh in consecutive patients except ours, whereas there were 2 articles concerning the frequency of provoked spasm by IV injection of ER.32, 33 According to past reports of comparisons between whites and Japanese (Figure 2), the prevalence of provoked spasms was 3× higher in Japanese than in whites.31, 34, 35 However, Ong et al recently reported a similar prevalence of coronary spasm (33.4%) with ACh spasm provocation tests in white patients with unobstructed coronary arteries, among 921 patents.36 Racial differences concerning coronary spasms may be absent, and coronary artery spasms may have no borders.
Figure 2.
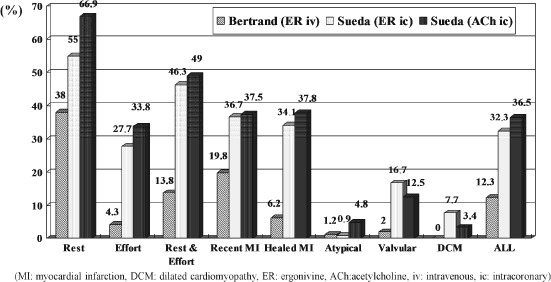
Comparison of provoked spasm frequency of Bertrand et al and the authors of the current study. Abbreviations: ACh, acetylcholine; DCM, dilated cardiomyopathy; ER, ergonovine; ic, intracoronary; iv, intravenous; MI, myocardial infarction.
Major and Minor Complications
Serious major complications during ACh spasm provocation tests were observed in 4 out of 715 patients (0.56%), including 2 cases of shock due to the proximal left anterior descending artery and proximal circumflex artery spasm, similar to spasm in the left main trunks. This was reversed by intra‐arterial administration of norepinephrine as well as nitrate; one case of sustained ventricular tachycardia was reversed by cardioversion; and one case of cardiac tamponade was reversed by surgical drainage from the subxyphoid lesion.37 The major complication rate of IC administration of ACh was not different from previous data (0.46%) with IV ER procedures by Bertrand et al (Table 1).32 However, no cases of death or irreversible complications occurred. According to the past reports by IV injection of ER, there were some complications with acute myocardial infarction, but we experienced no myocardial infarction when performing our ACh spasm provocation tests.38, 39 Although it is considered a safe and reliable method, the spasm provocation test using ACh should be performed carefully. We also experienced 14 serious major complications of ACh testing seen in 1546 examinations, and the rate of serious major complications was 0.9%. Paroxysmal atrial fibrillation occurred in 16.2% of patients who underwent the ACh spasm provocation test, with sinus rhythm in 717 patients; 71.6% of the patients recovered to sinus rhythm spontaneously in the cardiac catheterization laboratory. No thromboembolic events were encountered in our study. Intravenous injection of cibenzoline is also effective in restoring sinus rhythm, as well as disopyramide. We summarize our recommendation for ACh spasm provocation tests in Figure 3.
Table 1.
Serious Major Complications Among Past Studies
| Pharmacologic Agents | No. of Patients | VF | VT, (sustained VT) | Bradycardia | Shock | Tamponade | AMI | DC | CABG | Death | Serious Major Complications, n (%) | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Buxton (1980) | ER IV | 106 | 2 | 1 (1) | 2 | 5 | 0 | 0 | 0 | 1 | 3 | 5 (4.72) |
| Bertrand (1982) | Methyl ER IV | 1089 | 4 | 1 (1) | 2 | — | 0 | 0 | 4 | 0 | 0 | 5 (0.46) |
| Harding (1992) | ER IV | 3447 | (7) | (7) | — | — | — | 4 | — | 0 | 0 | 11 (0.03) |
| Ong (2014) | ACh IC | 847 | 0 | 1 (0) | 6 | — | 0 | 0 | 0 | 0 | 0 | 0 (0) |
| Sueda (1999) | ACh IC | 715 | 0 | 7 (1) | — | 2 | 1 | 0 | 1 | 0 | 0 | 4 (0.56) |
Abbreviations: ACh, acetylcholine; AMI, acute myocardial infarction; CABG, coronary artery bypass graft; DC, direct current; ER, ergonovine; IC, intracoronary; IV, intravenous; VF, ventricular fibrillation; VT, ventricular tachycardia.
Figure 3.
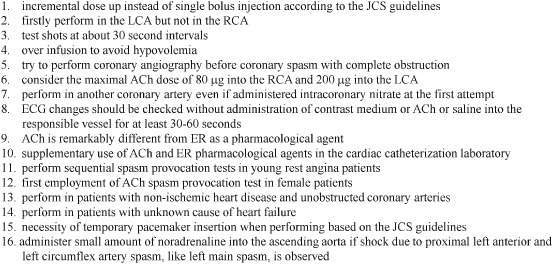
Our recommendation for ACh spasm provocation tests. Abbreviations: ACh, acetylcholine; ECG, electrocardiographic; ER, ergonovine; JCS, Japanese Circulation Society; LCA, left coronary artery; RCA, right coronary artery.
Difference Between Acetylcholine and Ergonovine Spasm Provocation Tests
Both ACh and ER are useful in demonstrating coronary artery spasm invasively in the cardiac catheterization laboratory. However, ACh acts through mediating cholinergic muscarinic receptors,40 whereas ER probably acts through serotogenic receptors. Different mediators may have potential to cause different responses. We performed selective IC administration of both ACh and ER in the same 171 patients with <50% stenosis.41 There was no difference in the incidence of provoked spasm between the 2 pharmacologic agents (ACh 33% vs ER 32%; not significant). Coronary spasms were induced by either pharmacologic agent in 134 vessels. Concordance was 94% in all vessels, whereas the remaining 6% of vessels were different from each other. The nonconcordance rate of the RCA was significantly higher than that of the LCA (10% vs 4%; P < 0.01). However, ACh provoked more diffuse and distal spasms and ER provoked more focal and proximal spasms. Seventy‐four of the 134 vessels (55%) had coronary spasms in the same coronary arteries. Concordance of both provoked spasm sites and spasm configurations in the same coronary artery was observed in only 18 vessels (13%). Cardiologists should watch for these differences between ACh and ER as pharmacological agents for the induction of coronary artery spasm. We recommend the supplementary use of these 2 pharmacological agents in the cardiac catheterization laboratory, if available.
Limitations of Acetylcholine Testing
When Acetylcholine Testing Does Not Provoke Spasm in Suspected Coronary Spastic Angina
When the standard ACh tests did not provoke spasm in variant angina, Yasue and Okumura performed IV administration of 0.2 mg of ER. However, IV administration of ER may cause refractory multiple spasms because this method is unselective. To perform the test safely, the JCS guidelines recommend IC injection of ER for spasm provocation instead of IV administration of ER. Today in our institutions IC injection of ER is administered in a total dose of 64 µg into the LCA and 40 µg into the RCA. If no spasm is provoked under the above procedure, we may often add IC injection of ACh (RCA, 50 or 80 µg; LCA, 100 or 200 µg) following the IC administration of ER. Goto et al also reported the usefulness of adding IC injection of ACh following IV infusion of ER when IV administration of ER 0.4 mg showed negative spasms.42 In these situations, we should take care for false‐positive results. However, we should reconsider the false‐negative by performing the standard single spasm provocation tests.
Acetylcholine Is Less Sensitive in Younger Patients With Rest Angina
Coronary artery spasm is not always induced by the ACh test in all rest angina patients. Sensitivity of the ACh spasm provocation test in patients with rest angina is approximately 70%. We sometimes experience negative ACh findings in young rest angina patients irrespective of a strong suspicion of CSA. We compared the positive frequency of provoked spasm by ACh test in 380 rest angina patients age <40 years (n = 12) and age ≥40 years (n = 368). There was no difference concerning the coronary risk factors and organic stenosis between the 2 groups. The rate of positive spasm with ACh was significantly lower in the younger group than in the older group (33.3% vs 71.5%; P < 0.05). The cumulative coronary risk factors in the younger group were significantly lower than those in the older group (0.8 ± 0.7 vs 1.8 ± 1.0, P < 0.01). Positive spasm was obtained in 1 patient by IC injection of ER and in 3 patients by adding IC administration of ACh after an ER test. Thus, the provoked positive spasm rate in the younger group became similar to that in the older group after performing sequential spasm provocation tests (66.7% vs 71.5%; not significant). To diagnose coronary artery spasm in younger rest angina patients, if possible we recommend performing sequential spasm provocation tests, such as first the ACh test, then the ER test, and adding IC injection of ACh after ER tests, because the grade and severity of coronary endothelial disturbance in younger rest angina patients may be lower than that in older rest angina patients.
Acetylcholine Is Supersensitive for Female Patients
Japanese female patients with CSA had the characteristics of diffuse provoked spasm, less organic stenosis, and less history of smoking, but only 1 in 10 of all patients with CSA are female. We examined the sex difference concerning the coronary response between ACh and ER in 461 patients (167 female; mean age, 64.4 ± 11.3 years) who underwent testing with both pharmacologic agents. Intracoronary injection of ACh and ER provoked spasm in 221 patients (61 female and 160 male). In female patients, ACh provoked spasm in all but 2 patients (96.7%; 59 patients), whereas ER provoked spasm in only 20 patients (32.8%). Intracoronary injection of ACh documented positive spasm in 91 out of 94 vessels (96.8%), whereas only 20 vessels (21.3%) provoked spasm by IC injection of ER in female patients. A representative case is shown in Figure 4. Positive spasm by ACh was significantly higher than that by ER. Meanwhile, provoked spasm by ACh (129 patients) was significantly higher than by ER (97 patients) in male patients (80.6% vs 60.6%; P < 0.01), and the number of vessels with provoked spasm was also significantly higher in ACh than ER (185/231, 80.1% vs 115/231, 49.8%; P < 0.001).43 As a spasm provocation test, ACh is supersensitive in female patients. Especially in female patients, we recommend first employing the ACh test instead of the ER test. In the cardiac catheterization laboratory in the future, we may select pharmacological agents according to sex for the induction of coronary artery spasm.
Figure 4.
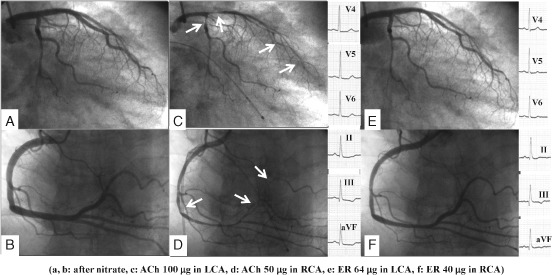
A case of CSA showing different coronary responses between ACh and ER in a female. Patient is a 70‐year‐old female complaining of rest angina at early morning and midnight. Frequent sublingual nitroglycerine suppressed her chest pain. Her coronary angiogram (A, B) was normal. IC injection of 100 µg ACh (C) provoked diffuse spasm at both proximal LAD and LCX, accompanied by more than usual chest pain and ischemic ECG change (ST‐segment depression in leads V4 through V6 at 1.0 mV). In the RCA, 50 µg ACh (D) induced diffuse spasm at distal portion accompanied by usual chest pain and ischemic ECG change (ST‐segment depression in II through III aVF leads at 1.0 mV). However, after the spontaneous spasm relief induced by ACh, IC administration of ER 64/40 µ (E, F) did not provoke spasm in both coronary arteries. Neither chest pain nor ischemic ECG change were recognized during the ER spasm provocation test. Abbreviations: ACh, acetylcholine; CSA, coronary spastic angina; ECG, electrocardiographic; ER, ergonovine; IC, intracoronary; LAD, left anterior descending artery; LCX, left circumflex artery; RCA, right coronary artery.
Acetylcholine Test for Patients With Nonischemic Heart Disease
The majority of cardiologists do not perform spasm provocation tests in patients with nonischemic heart disease and nonobstructive coronary artery disease. We examined the frequency of provoked spasm in 416 patients with nonischemic heart disease and nonobstructive coronary artery disease such as atypical chest pain, valvular heart disease, hypertrophic cardiomyopathy, congestive heart failure, and other conditions. Positive coronary spasm was obtained in 17.3% of nonischemic heart disease patients (72/416). Positive spasm was 11.4% (15/132), 19% (8/42), 16.7% (5/30), 23.9% (16/67), and 19.3% (28/145) in patients with atypical chest pain, valvular heart disease, hypertrophic cardiomyopathy, congestive heart failure, and other conditions, respectively. We recommend performing spasm provocation tests in patients with not only ischemic heart disease but also nonischemic heart disease with nonobstructive coronary artery disease, because 1 of 6 nonischemic heart disease patients had provoked coronary spasm. We also recommend performing ACh spasm provocation tests in patients with unknown cause of heart failure. Approximately a third of patients with heart failure exhibited provoked spasms with the ACh test.44 In these patients, the administration of long‐acting calcium‐channel antagonists and nitrates instead of β‐blockers improved left ventricular function. Coronary artery spasm may cause transient heart failure, possibly due to multiple spasms. We first named this disease state vasospastic heart failure.
Acetylcholine Testing in the Future
Coronary artery spasm may be involved in the pathogenesis of various cardiac disorders, such as ischemic heart disease and nonischemic heart disease. We recently experienced a case of silent coronary spasm without chest symptoms; abnormal ECG was the only symptom. Up until now have mainly performed ACh spasm provocation tests in patients with rest angina. However, whenever possible we should investigate the presence of coronary artery spasm in all patients who have undergone coronary angiography. Performing routine spasm provocation tests in all patients who have undergone coronary angiography in the world may help us to recognize new clinical knowledge.
Conclusion
In the cardiac catheterization laboratory, many cardiologists are so busy performing PCIs that there is scarcely time to perform ACh spasm provocation tests.45 However, it is also necessary for young cardiologists to learn how to perform selective spasm provocation tests safely. Before obtaining the techniques for PCI, they should learn diagnostic cardiac catheterization techniques. In diagnosing patients with ischemic or nonischemic heart disease, the majority of cardiologists investigate the presence or absence of coronary atherosclerosis alone. However, even if we performed PCIs in all patients with coronary atherosclerosis in the world, we will still experience ischemic heart disease due to coronary artery spasm in the future. We hope that young cardiologists can gain insight into the real truth of each patient who has undergone coronary angiography by performing ACh spasm provocation tests in the cardiac catheterization laboratory. It is only spasm, but spasm it is.
Acknowledgments
The authors acknowledge the helpful comments of professors Yuji Shigematsu, MD, Mareomi Hamada, MD, Jitsuo Higaki MD, and Kunio Hiwada MD, as well as Kensuke Tsunemitsu, MD, president of Saiseikai Saijo Hospital.
The authors have no funding, financial relationships, or conflicts of interest to disclose.
References
- 1. Yasue H, Takizawa A, Nagao M, et al. Long‐term prognosis for patients with variant angina and influential factors. Circulation. 1988;78:1–9. [DOI] [PubMed] [Google Scholar]
- 2. Kimura E, Kishida H. Treatment of variant angina with drugs: a survey of 11 cardiology institutes in Japan. Circulation. 1981;63:844–848. [DOI] [PubMed] [Google Scholar]
- 3. Nakamura M, Takeshita A, Nose Y. Clinical characteristics associated with myocardial infarction, arrhythmia, and sudden death in patients with vasospastic angina. Circulation. 1987;75:1110–1116. [DOI] [PubMed] [Google Scholar]
- 4. Shimokawa H, Nagasawa K, Irie T, et al. Clinical characteristics and long‐term prognosis of patients with variant angina: a comparative study between western and Japanese populations. Int J Cardiol. 1988;18:331–349. [DOI] [PubMed] [Google Scholar]
- 5. Nishi I, Iida K, Kawano S, et al. Effects of anti‐vasospastic agents in Japanese patients with dilated cardiomyopathy and coronary vasospasm. Jpn Heart J. 2002;43:333–342. [DOI] [PubMed] [Google Scholar]
- 6. Meisel SR, Mazur A, Chetboun I, et al. Usefulness of implantable cardioverter‐defibrillators in refractory variant angina pectoris complicated by ventricular fibrillation in patients with angiographically normal coronary arteries. Am J Cardiol. 2002;89:1114–1116. [DOI] [PubMed] [Google Scholar]
- 7. Chavalier P, Dacosta A, Defaye P, et al. Arrhythmic cardiac arrest due to isolated coronary artery spasm: long‐term outcome of seven resuscitated patients. J Am Coll Cardiol. 1998;31:57–61. [DOI] [PubMed] [Google Scholar]
- 8. Yasue H, Omote S, Takizawa A, et al. Circadian variation of exercise capacity in patients with Prinzmetal's variant angina: role of exercise‐induced coronary arterial spasm. Circulation. 1979;59:938–948. [DOI] [PubMed] [Google Scholar]
- 9. Nakao K, Ohgushi M, Yoshimura M, et al. Hyperventilation as a specific test for diagnosis of coronary artery spasm. Am J Cardiol. 1997;80:545–549. [DOI] [PubMed] [Google Scholar]
- 10. Nakajima K, Shimizu K, Taki J, et al. Utility of iodine‐123‐BMIPP in the diagnosis and follow up vasospastic angina. J Nucl Med. 1995;36:1934–1940. [PubMed] [Google Scholar]
- 11. Okumura K, Yasue H, Matsuyama K, et al. Sensitivity and specificity of intracoronary injection of acetylcholine for the induction of coronary artery spasm. J Am Coll Cardiol. 1988;12:883–888. [DOI] [PubMed] [Google Scholar]
- 12. Okumura K, Yasue H, Horio Y, et al. Multivessel coronary spasm in patients with variant angina: a study with intracoronary injection of acetylcholine. Circulation. 1988;77:535–542. [DOI] [PubMed] [Google Scholar]
- 13. Okumura K, Yasue H, Matsuyama K, et al. Diffuse disorder of coronary artery vasomotility in patients with coronary spastic angina: hyperreactivity to the constrictor effects of acetylcholine and the dilator effects of nitroglycerin. J Am Coll Cardiol. 1996;27:45–52. [DOI] [PubMed] [Google Scholar]
- 14. JCS Joint Working Group . Guidelines for diagnosis and treatment of patients with vasospastic angina (coronary spastic angina) (JCS 2008): digest version. Circ J. 2010;74:1745–1762. [DOI] [PubMed] [Google Scholar]
- 15. Stein I. Observations on the action of ergonovine on the coronary circulation and its use in the diagnosis of coronary artery insufficiency. Am Heart J. 1949;37:36–45. [DOI] [PubMed] [Google Scholar]
- 16. Heupler FA Jr. Provocative testing for coronary arterial spasm: risk, method and rationale. Am J Cardiol. 1980;46:335–337. [DOI] [PubMed] [Google Scholar]
- 17. Hackett D, Larkin S, Chierchia S, et al. Induction of coronary artery spasm by a direct local action of ergonovine. Circulation. 1987;75:577–582. [DOI] [PubMed] [Google Scholar]
- 18. Ishise S, Monji T, Takakuwa T, et al. Clinical application of intracoronary administration of ergonovine for detecting vasospastic angina [article in Japanese]. Kokyu To Junkan. 1987;35:191–195. [PubMed] [Google Scholar]
- 19. Yasue H, Touyama M, Shimamoto M, et al. Role of autonomic nervous system in the pathogenesis of Prinzmetal's variant form of angina. Circulation. 1974;50:534–539. [DOI] [PubMed] [Google Scholar]
- 20. Endo M, Hirosawa K, Kaneko N, et al. Prinzmetal's variant angina: coronary arteriogram and left ventriculogram during angina attack induced by methacholine. N Engl J Med. 1976;294:252–255. [DOI] [PubMed] [Google Scholar]
- 21. Yasue H, Horio Y, Nakamura N, et al. Induction of coronary artery spasm by acetylcholine in patients with variant angina: possible role of the parasympathetic nervous system in the pathogenesis of coronary artery spasm. Circulation. 1986;74:955–963. [DOI] [PubMed] [Google Scholar]
- 22. Austen WG, Edwards JE, Frye RL, et al. A reporting system on patients evaluated for coronary artery disease: report of the Ad Hoc Committee for Grading of Coronary Artery Disease, Council on Cardiovascular Surgery, American Heart Association. Circulation. 1975;51(4 suppl):5–40. [DOI] [PubMed] [Google Scholar]
- 23. Sato K, Kaikita K, Nakayama N, et al. Coronary vasomotor response to intracoronary acetylcholine injection, clinical features, and long‐term prognosis in 873 consecutive patients with coronary spasm: analysis of a single‐center study over 20 years. J Am Heart Assoc. 2013;2:e000227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Ong P, Athanasiadis A, Hill S, et al. Coronary microvascular dysfunction assessed by intracoronary acetylcholine provocation testing is a frequent cause of ischemia and angina in patients with exercise‐induced electrocardiographic changes and unobstructed coronary arteries. Clin Cardiol. 2014;37:462–467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Ong P, Athanasiadis A, Borgulya G, et al. High prevalence of a pathological response to acetylcholine testing in patients with stable angina pectoris and unobstructed coronary arteries: the ACOVA study. J Am Coll Cardiol. 2012;59:655–662. [DOI] [PubMed] [Google Scholar]
- 26. Ong P, Athanasiadis A, Sechtem U. Patterns of coronary vasomotor responses to intracoronary acetylcholine provocation. Heart. 2013;99:1288–1295. [DOI] [PubMed] [Google Scholar]
- 27. Yasue H, Matsuyama K, Matsuyama K, et al. Responses of angiographically normal human coronary arteries to intracoronary injection of acetylcholine by age and segment: possible role of early coronary atherosclerosis. Circulation. 1990;81:482–490. [DOI] [PubMed] [Google Scholar]
- 28. Vita JA, Treasure CB, Nabel EG, et al. Coronary vasomotor response to acetylcholine relates to risk factors for coronary artery disease. Circulation. 1990;81:491–497. [DOI] [PubMed] [Google Scholar]
- 29. Sueda S, Kohno H, Oshita A, et al. Coronary abnormal response has increased in Japanese patients: analysis of 17 years' spasm provocation tests in 2093 cases. J Cardiol. 2010;55:354–361. [DOI] [PubMed] [Google Scholar]
- 30. Yasue H, Mizuno Y, Harada E, et al; SCAST (Statin and Coronary Artery Spasm Trial) Investigators. Effect of a 3‐hydrooxy‐3‐methylglutaryl coenzyme A reductase inhibitor, fluvastatin, on coronary spasm after withdrawal of calcium‐channel blockers. J Am Coll Cardiol. 2008;51:1742–1748. [DOI] [PubMed] [Google Scholar]
- 31. Sueda S, Ochi N, Kawada H, et al. Frequency of provoked coronary vasospasm in patients undergoing coronary arteriography with spasm provocation test of acetylcholine. Am J Cardiol. 1999;83:1186–1190. [DOI] [PubMed] [Google Scholar]
- 32. Bertrand ME, LaBlanche JM, Tilmant PY, et al. Frequency of provoked coronary arterial spasm in 1089 consecutive patients undergoing coronary arteriography. Circulation. 1982;65:1299–1306. [DOI] [PubMed] [Google Scholar]
- 33. Nosaka H, Nobuyoshi M. Coronary arterial spasm and symptomatology in ischemic and nonischemic heart disease: study of the ergonovine maleate provocative test in 3000 consecutive patients [article in Japanese]. J Cardiogr Suppl. 1987;12:35–47. [PubMed] [Google Scholar]
- 34. Pristipino C, Beltrame JF, Finocchiaro ML, et al. Major racial differences in coronary constrictor response between Japanese and Caucasians with recent myocardial infarction. Circulation. 2000;101:1102–1108. [DOI] [PubMed] [Google Scholar]
- 35. Beltrame JF, Sasayama S, Maseri A. Racial heterogeneity in coronary artery vasomotor reactivity: differences between Japanese and Caucasian patients. J Am Coll Cardiol. 1999;33:1442–1452. [DOI] [PubMed] [Google Scholar]
- 36. Ong P, Athanasiadis A, Borgulya G, et al. Clinical usefulness, angiographic characteristics, and safety evaluation of intracoronary acetylcholine provocation testing among 921 consecutive white patients with unobstructed coronary arteries. Circulation. 2014;129:1723–1730. [DOI] [PubMed] [Google Scholar]
- 37. Sueda S, Saeki H, Otani T, et al. Major complications during spasm provocation tests with an intracoronary injection of acetylcholine. Am J Cardiol. 2000;85:391–394. [DOI] [PubMed] [Google Scholar]
- 38. Buxton A, Goldberg S, Hirshfeld JW, et al. Refractory ergonovine induced coronary vasospasm: importance of intracoronary nitroglycerin. Am J Cardiol. 1980;46:329–334. [DOI] [PubMed] [Google Scholar]
- 39. Harding MB, Leithe ME, Mark DB, et al. Ergonovine maleate testing during cardiac catheterization: a 10‐year perspective in 3447 patients without significant coronary artery disease or Prinzmetal's variant angina [published correction appears in J Am Coll Cardiol. 1993;21:848]. J Am Coll Cardiol. 1992;20:107–111. [DOI] [PubMed] [Google Scholar]
- 40. Ludmer PL, Selwyn AP, Shook TL, et al. Paradoxical vasoconstriction induced by acetylcholine in atherosclerotic coronary arteries. N Engl J Med. 1986;315:1046–1051. [DOI] [PubMed] [Google Scholar]
- 41. Goto A, Ito S, Kondo H, et al. Evaluation of adjunctive intracoronary administration of acetylcholine following intravenous infusion of ergonovine to provoke coronary artery spasm. J Cardiol. 1999;34:309–316. [PubMed] [Google Scholar]
- 42. Sueda S, Kohno H, Fukuda H, et al. Induction of coronary artery spasm by two pharmacological agents: comparison between intracoronary injection of acetylcholine and ergonovine. Coron Artery Dis. 2003;14:451–457. [DOI] [PubMed] [Google Scholar]
- 43. Sueda S, Miyoshi T, Sasaki Y, et al. Gender differences in sensitivity of acetylcholine and ergonovine to coronary spasm provocation test. Heart Vessels. 2014. doi: 10.1007/s00380-014-0614-4. [DOI] [PubMed] [Google Scholar]
- 44. Sakata K, Nawada R, Ohbayashi K, et al. Diffuse and severe left ventricular dysfunction induced by epicardial coronary artery spasm. Angiology. 2000;51:837–847. [DOI] [PubMed] [Google Scholar]
- 45. Yasue H, Nakagawa H, Itoh T, et al. Coronary artery spasm—clinical features, diagnosis, pathogenesis, and treatment. J Cardiol. 2008;51:2–17. [DOI] [PubMed] [Google Scholar]


