Abstract
Background
There is little research on overall cardiovascular (CV) health among couples. Our aim was to examine concordance levels for CV health among couples, using the American Heart Association ideal health metrics, and to investigate if the CV health of an individual is associated with that of his or her partner.
Hypothesis
There is a positive association between the overall cardiovascular health of an individual and that of his/her partner.
Methods
The Mitchelstown Study is a community‐based cohort study of middle‐aged Irish adults. Potential couples were identified as 2 study participants living at the same address. This list was cross‐referenced with self‐reported marital status and telephone number in the electronic patient record. Information on CV health metrics (smoking, body mass index, physical activity, diet, blood pressure, cholesterol, and glucose) was collected using standardized methods. Participants were categorized as ideal, intermediate, or poor for each of the metrics and for overall CV health. The 0‐ to 14‐point CV health metrics score was compared within couples using linear regression.
Results
Of 2047 participants, 191 potential couples were identified. We excluded 6 sibling pairs, 1 divorced couple, and 3 couples who self‐reported being single. The analysis includes 181 couples. There were significant associations between partners for smoking, diet, blood pressure, cholesterol, and glucose (P < 0.05). No couple had ideal CV health (ie, both partners with 7 ideal metrics). Most couples (n = 127, 69%) were concordant for poor CV health. There was a significant relationship between partners for the CV health metrics score (P < 0.05).
Conclusions
Our results suggest an individual's CV health is associated with that of his or her partner. Therefore, prevention strategies targeting couples and families may be appropriate.
Introduction
Cardiovascular disease (CVD) is a leading cause of death worldwide.1 In Europe it accounts for 46% of totale deaths.2 A substantial portion of the population‐attributable risk for CVD, such as coronary heart disease, has been linked to suboptimal risk‐factor management and lifestyle behaviors.3
Previous studies have demonstrated an association between an individual's cardiovascular (CV) risk factors and those of their partner.4, 5 The presence of any given condition or risk factor in both partners is known as spousal concordance. Spousal concordance levels vary depending on the risk factor in question, with smoking being the factor most likely to be correlated.5
Assortative mating and a shared environment, including shared resources and social networks, are considered to be the main drivers behind spousal concordance.5, 6 Spouses can also influence the health behavior of their partner. Data from the Health and Retirement Study (HRS) in the United States showed that when one spouse improved his or her behavior, the other spouse was also likely to do so.7 The effect was evident for smoking status, alcohol consumption, exercise, cholesterol screening, and receiving a flu shot and was stable following adjustment for sociodemographic factors and self‐rated health. Marriage is also considered to have a protective effect on health.8 Married individuals have been shown to have better outcomes following percutaneous coronary intervention compared with those who are unmarried.9
In 2010, the American Heart Association (AHA) devised the concept of ideal, intermediate, and poor CV health based on the levels of 7 CV risk factors and behaviors: smoking status, body mass index (BMI), physical activity levels, healthy diet score, blood pressure (BP), total cholesterol, and fasting plasma glucose.10 Ideal CV health was defined as ideal health in each health metric (ie, the absence of smoking, ideal BMI, physical activity at goal, a healthy diet pattern, untreated total cholesterol <200 mg/dL, fasting glucose <100 mg/dL, untreated BP <120/80 mm Hg, and finally, the absence of clinical CVD). Recent studies have shown that the prevalence the prevalence of ideal CV health in populations is extremely low.11, 12, 13 Achieving a greater number of ideal health metrics is associated with a lower risk of total and CVD mortality.13
Few studies have examined the overall CV health of couples, and to our knowledge there are no studies assessing spousal concordance for ideal CV health. Therefore, our aim was to describe the CV health metrics and concordance levels for CV health among couples from a community‐based sample and to examine if the CV health status of an individual is associated with that of his or her partner.
Methods
Study Population
The Mitchelstown study is a population‐based cohort study of individuals recruited from a single large primary‐care center, the Livinghealth Clinic (LHC), in Mitchelstown, County Cork, Ireland. The study was established to examine CV health and related factors in an Irish adult sample. Those registered with the clinic in the age bracket of 50 to 69 years were eligible for the study. Eligible individuals were assigned a random number and invited based on this random number in batches of 150 until the target sample size of 2000 was achieved. A final sample of 2047 was recruited (response rate, 67%). Details of the Mitchelstown Study have been published previously.14
A couple was defined as two individuals living at the same address. The initial list was cross‐referenced with self‐reported marital status from the questionnaire, telephone numbers and surnames, and the electronic patient record in the primary‐care center. We excluded sibling pairs and those with discordant marital status on the self‐reported questionnaire. All couples in the sample were male‐female relationships.
Measurements
Baseline data were collected for 1 year, from 2010 to 2011. All participants self‐completed the baseline questionnaire, and the baseline physical examination was carried out by a trained researcher according to detailed standard operating procedures. Using the AHA definitions, individual health metrics were classified as ideal, intermediate, or poor.
Participants self‐reported smoking status by questionnaire. Never, former, and current smokers were categorized into ideal, intermediate, and poor health categories, respectively.
The short form of the International Physical Activity Questionnaire (IPAQ) was used to measure physical activity. Activity levels were converted into metabolic equivalent of task (MET) according to the IPAQ criteria, and the IPAQ categories of low, moderate, and high were used to define poor, intermediate, and ideal health, respectively.
Information on dietary habits was obtained with a modified version of the European Prospective Investigation of Cancer (EPIC) Food Frequency Questionnaire, which has been validated for use in the Irish population.15 Intake goals were defined using the 5 AHA ideal dietary goals: ≥4.5 cups of fruits and vegetables per day, ≥2 3.5‐oz servings of fish per week, ≥3 1‐oz servings of fiber‐rich whole grains per day, <1500 mg sodium per day, and ≤36 oz of sugar‐sweetened beverages per week.10 Participants with 4 to 5 of these ideal diet components were categorized as having an ideal diet score, those with 2 to 3 components as having an intermediate score, and those with 0 to 1 component as having a poor diet score.
Height was measured using a portable height measure (Seca Leicester, Birmingham, UK). Weight was measured using a portable electronic scale (model WB‐100MA; Tanita Corp., Arlington Heights, IL). Body mass index was then calculated. Participants with BMI ≥30, 25 to <30, and <25 kg/m2 were categorized into poor, intermediate, and ideal health categories, respectively.
Three BP readings were taken on the right arm, 1 minute apart, using the Omron model M7 digital automatic BP monitor (Omron Healthcare, Lake Forest, IL). The average of the second and third BP reading was defined as the clinic BP. A combination of BP level and self‐reported treatment status from the questionnaire was used to define hypertension category. Ideal, intermediate, and poor health were defined as <120/80 mm Hg, 120/80 to 139/89 mm Hg or treated to goal, and ≥140/90 mm Hg, respectively.
A blood sample was taken after an 8‐hour fast. This was analyzed for total cholesterol and glucose. Serum total cholesterol was measured enzymatically by an Olympus automatic analyzer (model AU5400; Olympus Optical, Tokyo, Japan). Plasma glucose concentrations were determined using a glucose‐hexokinase assay. Ideal, intermediate, and poor health for total cholesterol were defined as <5 mmol/L, 5 to 6 mmol/L or treated to goal, and >6 mmol/L, respectively. Current use of cholesterol‐lowering medication was based on self‐report. For fasting glucose, ideal health was defined as <5.5 mmol/L, intermediate health as 5.5 to 6.9 mmol/L, and poor health as ≥7 mmol/L, or self‐report of doctor‐diagnosed diabetes.
Participants were also classified into an overall CV health category based on the combination of individual health metrics. Ideal CV health is defined as all 7 health metrics at ideal levels and the absence of clinical CVD. Those with a previous diagnosis of CVD with controlled individual metrics were excluded from ideal categories and categorized in intermediate groups.10 Intermediate health was defined as ≥1 of 7 health metrics at intermediate levels, but no poor health metric. Poor health was defined as ≥1 of 7 health metrics at the poor level.13
Statistical Analysis
All analyses were carried out using Stata version 12 (StataCorp, College Station, TX). Continuous variables were described by mean ± SD and compared by t tests or corresponding nonparametric tests based on distribution properties. Categorical variables were described by percentages and compared by χ2 tests.
The prevalence of each CV health metric was calculated. The association between individual health metrics was calculated across couples using χ2 tests. Concordance levels among couples for overall CV health were calculated by dividing the number of couples with complete agreement by the total number of couples.
As previously described, a 0‐ to 14‐point CV health metric score was calculated. A score of 0 was given for poor health, 1 for intermediate health, and 2 for ideal health for each metric.16 The distribution of the scores between male and female partners was compared using the Kolmogorov‐Smirnov test. The relationship between couples' scores was examined using the Pearson correlation coefficient and linear regression. The regression analysis was adjusted for potential confounding factors including age, educational attainment (primary, secondary, third‐level education), and medical‐card status (yes/no). Medical‐card status was used as a proxy indicator of socioeconomic status, as holders are entitled to free access to health care on the basis of income.
All participants provided written informed consent, and the study was approved by the Clinical Research Ethics Committee of the Cork Teaching Hospitals. All investigations were carried out in accordance with the Declaration of Helsinki.
Results
Of 2047 participants, 191 potential couples were identified. We excluded 6 sibling pairs, 1 divorced couple, and 3 couples who did not self‐report being married in the baseline questionnaire. Therefore, 181 couples (n = 362 individuals, 18% of the cohort) were included in the analysis. The mean age was 61 years (SD = 5) for male partners and 60 years (SD = 5) for female partners. Approximately one‐third of participants had a medical card (n = 123, 34%), and in 27.6% of couples both partners had a medical card (n = 50; Table 1).
Table 1.
Characteristics of Men and Women in the Sample (N = 362) and Level of Concordance Among Couples (N = 181)
| Total Sample (N = 362), n (%) | Men, n (%) | Women, n (%) | Level of Concordance Among Partners, n (% of Couples) | |
|---|---|---|---|---|
| Age, ya | ||||
| 50–54 | 75 (21.0) | 29 (16.2) | 46 (25.7) | 23 (12.7) |
| 55–59 | 86 (24.0) | 43 (24.0) | 43 (24.0) | 23 (12.7) |
| 60–64 | 119 (33.2) | 56 (31.3) | 63 (35.2) | 33 (18.2) |
| 65–69 | 78 (21.8) | 51 (28.5) | 27 (15.1) | 24 (13.3) |
| Educationb | ||||
| Primary | 89 (26.1) | 53 (30.8) | 36 (21.3) | 18 (9.9) |
| Secondary | 191 (56.0) | 93 (54.1) | 98 (58.0) | 53 (29.3) |
| Tertiary | 61 (17.9) | 26 (15.1) | 35 (20.7) | 11 (6.1) |
| Medical carda | 123 (34.0) | 60 (33.2) | 63 (34.8) | 50 (27.6) |
| Self‐rated healthb | ||||
| Very good/good | 309 (86.3) | 153 (85.5) | 156 (87.2) | 137 (75.7) |
| Fair/poor/very poor | 49 (13.7) | 26 (14.5) | 23 (12.8) | 7 (3.9) |
| Self‐reported previous diagnosis of CVD | 19 (5.2) | 18 (12.9) | 2 (1.4) | 0 |
Abbreviations: CVD, cardiovascular disease.
Significant association between sex and sociodemographic characteristic at P < 0.001 level.
Significant association at the P < 0.05 level.
The proportion of participants who had ideal levels of individual CV health metrics was below 20%, with the exception of smoking (n = 170, 48.9%, classified as ideal) and glucose levels (n = 267, 75.4%, classified as ideal; Table 2). With the exception of physical activity and total cholesterol, more female partners met ideal levels for each health metric. Overall, 19 participants had a self‐reported previous diagnosis of CVD, which resulted in 5 participants being reclassified from the ideal to the intermediate category of the physical‐activity metric. No other metric was altered based on previous CVD status.
Table 2.
Distribution of the Cardiovascular Health Metrics (Total N = 362)
| Health Metric | Level | Definition | Total Sample, N = 362, n (%) | Men (n = 181), n (%) | Women, n = 181, n (%) | P Value |
|---|---|---|---|---|---|---|
| Smoking | Ideal | Never | 170 (48.9) | 69 (40.1) | 101 (57.4) | 0.004 |
| Intermediate | Former | 133 (38.2) | 79 (45.9) | 54 (30.7) | ||
| Poor | Current | 45 (12.9) | 24 (14.0) | 21 (11.9) | ||
| Physical activity | Ideal | IPAQ high | 69 (20.2) | 40 (24.5) | 29 (16.3) | 0.165 |
| Intermediate | IPAQ moderate | 116 (34.0) | 53 (32.5) | 63 (35.4) | ||
| Poor | IPAQ low | 156 (45.8) | 70 (42.9) | 86 (48.3) | ||
| Healthy diet score | Ideal | 4–5 components | 8 (2.3) | 3 (1.7) | 5 (2.8) | 0.013 |
| Intermediate | 2–3 components | 247 (70.4) | 112 (64.0) | 135 (76.7) | ||
| Poor | 0–1 components | 96 (27.3) | 60 (34.3) | 36 (20.5) | ||
| BMI | Ideal | <25 kg/m2 | 72 (19.9) | 22 (12.2) | 50 (27.6) | 0.001 |
| Intermediate | 25–29.99 kg/m2 | 172 (47.5) | 96 (53.0) | 76 (42.0) | ||
| Poor | ≥30 kg/m2 | 118 (32.6) | 63 (34.8) | 55 (30.4) | ||
| BP | Ideal | <120/80 mm Hg, without medication | 72 (19.9) | 25 (13.8) | 47 (26.1) | 0.013 |
| Intermediate | 120/80–139/89 mm Hg or treated to <120/80 mm Hg | 186 (51.5) | 102 (56.4) | 84 (46.7) | ||
| Poor | ≥140/90 mm Hg | 103 (28.5) | 54 (29.8) | 49 (27.2) | ||
| Cholesterol | Ideal | <5 mmol/L, without medication | 59 (17.0) | 38 (22.2) | 21 (11.9) | 0.004 |
| Intermediate | 5–6 mmol/L or <5 mmol/L, on medication | 220 (63.2) | 109 (63.7) | 111 (62.7) | ||
| Poor | >6 mmol/L | 69 (19.8) | 24 (14.1) | 45 (25.4) | ||
| Glucose | Ideal | FSG <5.5 mmol/L | 267 (75.4) | 111 (63.4) | 156 (87.1) | 0.000 |
| Intermediate | FSG 5.5–6.9 mmol/L | 59 (16.7) | 44 (25.2) | 15 (8.4) | ||
| Poor | FSG ≥7 mmol/L or doctor‐diagnosed DM | 28 (7.9) | 20 (11.4) | 8 (4.5) | ||
| Overall CV health status | Ideal | All 7 health metrics at ideal levels, absence of clinical CVD | 0 | 0 | 0 | 0.506 |
| Intermediate | ≥1 of the 7 health metrics at intermediate levels, no poor health metrics | 30 (10.7) | 12 (9.4) | 18 (11.8) | ||
| Poor | ≥1 of the 7 health metrics at a poor level | 250 (82.3) | 116 (90.6) | 134 (88.2) |
Abbreviations: BMI, body mass index; BP, blood pressure; CV, cardiovascular; CVD, cardiovascular disease; DM, diabetes mellitus; FSG, fasting serum glucose; IPAQ, International Physical Activity Questionnaire.
Table 3 outlines the association between partners across individual health metrics on the basis of paired data. There was evidence of a significant association for smoking status (P < 0.001), BP (P < 0.05), diet score (P < 0.05), total cholesterol (P < 0.05), and glucose levels (P < 0.05).
Table 3.
Univariate Association Between Partners' Individual Health Metrics (N = 181 Couples)
| Male Partner's Health Metric | Female Partner's Health Metric, n (% of total couples) | |||
|---|---|---|---|---|
| Ideal | Intermediate | Poor | P Value | |
| Smoking | 0.000 | |||
| Ideal | 49 (27.1) | 14 (7.7) | 1 (0.6) | |
| Intermediate | 43 (23.7) | 25 (13.8) | 11 (6.1) | |
| Poor | 6 (3.3) | 11 (6.1) | 7 (3.9) | |
| Physical activity | 0.809 | |||
| Ideal | 7 (3.9) | 14 (7.7) | 18 (9.9) | |
| Intermediate | 7 (3.9) | 16 (8.8) | 30 (16.6) | |
| Poor | 11 (6.1) | 26 (14.4) | 32 (17.7) | |
| Healthy diet | 0.010 | |||
| Ideal | 1 (0.6) | 2 (1.1) | 0 (0) | |
| Intermediate | 4 (2.2) | 86 (47.5) | 19 (10.5) | |
| Poor | 0 (0) | 44 (24.3) | 15 (8.3) | |
| BMI | 0.483 | |||
| Ideal | 7 (3.9) | 7 (3.9) | 8 (4.4) | |
| Intermediate | 28 (15.5) | 44 (24.3) | 24 (13.3) | |
| Poor | 15 (8.3) | 25 (13.8) | 23 (12.7) | |
| BP | 0.024 | |||
| Ideal | 6 (3.3) | 11 (6.1) | 8 (4.4) | |
| Intermediate | 30 (16.6) | 53 (29.3) | 18 (9.9) | |
| Poor | 11 (6.1) | 20 (11.0) | 23 (12.7) | |
| Cholesterol | 0.019 | |||
| Ideal | 0 (0) | 28 (15.5) | 9 (5.0) | |
| Intermediate | 19 (10.5) | 63 (34.8) | 25 (13.8) | |
| Poor | 1 (0.6) | 13 (7.2) | 9 (5.0) | |
| Glucose | 0.044 | |||
| Ideal | 101 (55.8) | 7 (3.9) | 2 (1.1) | |
| Intermediate | 34 (18.8) | 6 (3.3) | 4 (2.2) | |
| Poor | 17 (9.4) | 0 (0) | 2 (1.1) | |
Abbreviations: BMI, body mass index; BP, blood pressure.
Total number may not add up to 181 couples due to missing data.
There was evidence of spousal concordance for overall CV health (Figure 1). No couple had ideal CV health. Only 4.4% (n = 8) of couples had intermediate CV health. Most couples (n = 124, 69%) had poor CV health.
Figure 1.
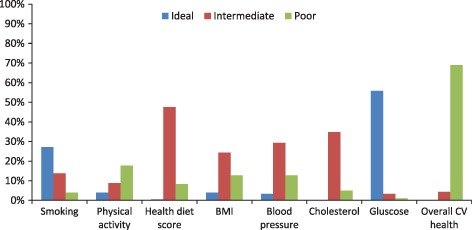
Proportion of couples who were concordant across each level of the cardiovascular health metrics. Abbreviations: CV, cardiovascular; BMI, body mass index.
The distribution of the CV health metrics score demonstrated a greater proportion of men at the lower end of the scale (P < 0.05; Figure 2). The average score for men was 7.0, and for women 7.6 (P < 0.05). The correlation between partners' scores was significant (r = 0.29, P = 0.001). The linear regression R2 was 0.08, with β = 0.35 and P = 0.001. Including age, education, and medical‐card status in the model did not significantly change the results (R2 = 0.06 with β = 0.35 and P = 0.008). Participants with missing data across the 7 health metrics were excluded from the calculation of the overall score. There were 54 couples missing a health metric score. Sensitivity analyses, in which analyses were repeated with these participants included as zero or poor health, showed that the results were unchanged (analyses not shown).
Figure 2.
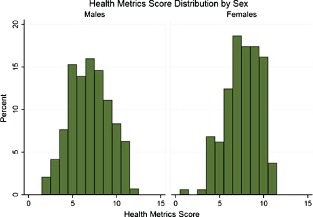
Distribution of health metrics score by sex.
Discussion
The aim of this study was to examine spousal concordance across 7 CV health metrics and to investigate whether the CV health status of an individual is associated with that of his or her partner. No couple achieved ideal CV health in all 7 components, which was to be expected, given the low prevalence of ideal CV health among individuals in this community‐based sample. This is in keeping with previous work on individuals that has shown a very low prevalence of ideal CV health in American and European populations.11, 12 Our results suggest an association between couples for the individual health metrics. The majority of couples had poor CV health, defined as poor health on any 1 of the 7 health metrics. Our findings suggest that an individual's overall CV health is related to that of his or her partner. There was a significant positive relationship between partners' CV health using the AHA CV health metrics score. This is an important finding, given the emerging evidence of a relationship between the CV health metric score and outcomes.13, 17 A high score on this scale was found to be associated with reduced risk of all‐cause mortality and mortality resulting from diseases of the circulatory system.16
Our study supports previous evidence of spousal concordance across CV risk factors.5, 6 There were significant associations between partners' levels of individual health metrics evident for smoking status, diet scores, total cholesterol, glucose, and BP. However, we did not find an association for BMI or physical activity. Also, though there was a positive association between partners' overall CV health score, the mean scores between male and female partners were different, and this may reflect the well‐established sex differences in CV risk. It is well known that men have a higher risk of CVD than women.18 The distributions were also different. The results suggest that partners may differ in some health behaviors; for example, it is recognized that men utilize health services less frequently than women.19 Interventions targeting couples may help overcome this.
Studies have shown an increased risk of hypertension and hyperlipidemia among individuals if their partners have the disease.4, 20 Previous studies have shown a benefit to targeting couples rather than individuals with prevention measures.21, 22 Spousal support may be an important factor.23, 24 Therefore, in certain circumstances, preventive strategies that target couples rather than individuals may have greater impact than those that target individuals alone.
Estimating CV risk is a key component of prevention guidelines.25 This estimation of risk needs to be communicated to patients. However, health literacy and numeracy need to be such that a patient can understand the message being conveyed, and frequently this is not the case.26 A number of tools have been suggested to deal with this; for example, the concept of biological vs chronological age.27, 28 In our study, the Framingham Risk Score was significantly correlated with the ideal health metrics score (data not shown). The Framingham Risk Score was also significantly correlated between partners (data not shown). The concept of the ideal health metrics could be used when communicating risk to patients and their partners and may facilitate understanding and acceptance of necessary intervention or lifestyle changes. However, further work is needed to standardize the assessment of physical activity and diet to increase the applicability of the CV health metrics in everyday clinical practice.
Study Limitations
This cross‐sectional study was conducted in 1 primary‐care center with a predominantly Caucasian sample of people age 50 to 69 years, which will limit the external generalizabilty of our findings to other populations. We were unable to study associations between ideal health metrics and clinical outcomes, such as CV events, in couples. However, the fact that participants have been recruited from 1 primary‐care center will allow analysis of incident CV events in the future. The strengths of the study include the use of validated standardized methods for the measurement of the health metrics. In addition, the objective measurement of BP and cholesterol during the baseline assessment allowed for the inclusion of previously undiagnosed hypertension and hyperlipidemia. To our knowledge, this is the first article that applies the ideal CV health metrics to couples.
Conclusion
Novel approaches are urgently required to address the major public health problem of CVD. Targeting couples rather than individuals may be one such approach. Furthermore, the CV health metrics concept could potentially be used as a risk‐communication tool, as patients may find it easier to understand than traditional risk‐prediction tools. Interventional studies are necessary to examine whether such approaches would have the desired effect and improve understanding of CV risk, which could ultimately lead to improvement in health status.
Acknowledgments
The authors acknowledge the participants in the study, the members of the survey team, the study nurses and administrators, and the staff at the Livinghealth Clinic.
The Mitchelstown Study is funded by a research grant from the Health Research Board Ireland (reference HRC/2007/13). Dr Anne Marie O'Flynn is funded by a Health Research Board Ireland Research Training Fellowship (reference HPF/2012/14). Dr Sheena McHugh is funded by the Health Research Board Interdisciplinary Capacity Enhancement Award (reference HRB/ICE/2012/12). Mr Jamie Madden is funded by the Health Research Board Ireland under the PhD Scholars Programme (reference PHD/2007/16). Prof Ivan Perry received funding through his institution from the Health Research Board Ireland to fund the initial data collection for the submitted work (reference HRC/2007/13). Prof Patricia Kearney was awarded the Health Research Board Research Leader Award (reference HRB/RL/2013/7).
The authors have no other funding, financial relationships, or conflicts of interest to disclose.
Drs Anne Marie O'Flynn and Sheena M. McHugh are joint first authors and contributed equally to the writing of this article.
References
- 1. Ouwens M, Wollersheim H, Hermens R, et al. Integrated care programmes for chronically ill patients: a review of systematic reviews. Int J Qual Health Care. 2005;17:141–146. [DOI] [PubMed] [Google Scholar]
- 2. Nichols M, Townsend N, Scarborough P, et al. Trends in age‐specific coronary heart disease mortality in the European Union over three decades: 1980–2009. Eur Heart J. 2013;34:3017–3027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Yusuf S, Hawken S, Ounpuu S, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case‐control study. Lancet. 2004;364:937–952. [DOI] [PubMed] [Google Scholar]
- 4. McAdams DeMarco M, Coresh J, Woodward M, et al. Hypertension status, treatment, and control among spousal pairs in a middle‐aged adult cohort. Am J Epidemiol. 2011;174:790–796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Di Castelnuovo A, Quacquaruccio G, Donati MB, et al. Spousal concordance for major coronary risk factors: a systematic review and meta‐analysis. Am J Epidemiol. 2009;169:1–8. [DOI] [PubMed] [Google Scholar]
- 6. Meyler D, Stimpson JP, Peek MK. Health concordance within couples: a systematic review. Soc Sci Med. 2007;64:2297–2310. [DOI] [PubMed] [Google Scholar]
- 7. Falba TA, Sindelar JL. Spousal concordance in health behavior change. Health Serv Res. 2008;43(1 part 1):96–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Manzoli L, Villari P, M Pirone G, et al. Marital status and mortality in the elderly: a systematic review and meta‐analysis. Soc Sci Med. 2007;64:77–94. [DOI] [PubMed] [Google Scholar]
- 9. Barbash IM, Gaglia MA Jr, Torguson R, et al. Effect of marital status on the outcome of patients undergoing elective or urgent coronary revascularization. Am Heart J. 2013;166:729–736. [DOI] [PubMed] [Google Scholar]
- 10. Lloyd‐Jones DM, Hong Y, Labarthe D, et al; American Heart Association Strategic Planning Task Force and Statistics Committee. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association's strategic Impact Goal through 2020 and beyond. Circulation. 2010;121:586–613. [DOI] [PubMed] [Google Scholar]
- 11. Bambs C, Kip KE, Dinga A, et al. Low prevalence of “ideal cardiovascular health” in a community‐based population: the Heart Strategies Concentrating on Risk Evaluation (Heart SCORE) study. Circulation. 2011;123:850–857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Vetrano DL, Martone AM, Mastropaolo S, et al. Prevalence of the seven cardiovascular health metrics in a Mediterranean country: results from a cross‐sectional study. Eur J Public Health. 2013;23:858–862. [DOI] [PubMed] [Google Scholar]
- 13. Folsom AR, Yatsuya H, Nettleton JA, et al. Community prevalence of ideal cardiovascular health, by the American Heart Association definition, and relationship with cardiovascular disease incidence. J Am Coll Cardiol. 2011;57:1690–1696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Kearney PM, Harrington JM, McCarthy VJ, et al. Cohort profile: the Cork and Kerry Diabetes and Heart Disease Study. Int J Epidemiol. 2013;42:1253–1262. [DOI] [PubMed] [Google Scholar]
- 15. Harrington J. Validation of a Food Frequency Questionnaire as a Tool for Assessing Nutrient Intake [thesis]. Galway, Ireland: National University of Ireland; 1997. [Google Scholar]
- 16. Ford ES, Greenlund KJ, Hong Y. Ideal cardiovascular health and mortality from all causes and diseases of the circulatory system among adults in the United States. Circulation. 2012;125:987–995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Yang Q, Cogswell ME, Flanders WD, et al. Trends in cardiovascular health metrics and associations with all‐cause and CVD mortality among US adults. JAMA. 2012;307:1273–1283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Waldron I. Why do women live longer than men? Soc Sci Med. 1976;10:349–362. [DOI] [PubMed] [Google Scholar]
- 19. Bertakis KD, Azari R, Helms LJ, et al. Gender differences in the utilization of health care services. J Fam Pract. 2000;49:147–152. [PubMed] [Google Scholar]
- 20. Hippisley‐Cox J, Coupland C, Pringle M, et al. Married couples' risk of same disease: cross sectional study. BMJ. 2002;325:636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Pyke SD, Wood DA, Kinmonth AL, et al. Change in coronary risk and coronary risk factor levels in couples following lifestyle intervention. The British Family Heart Study. Arch Fam Med. 1997;6:354–360. [DOI] [PubMed] [Google Scholar]
- 22. Knutsen SF, Knutsen R. The Tromsø Survey: the Family Intervention study—the effect of intervention on some coronary risk factors and dietary habits, a 6‐year follow‐up. Prev Med. 1991;20:197–212. [DOI] [PubMed] [Google Scholar]
- 23. Hong TB, Franks MM, Gonzalez R, et al. A dyadic investigation of exercise support between cardiac patients and their spouses. Health Psychol. 2005;24:430–434. [DOI] [PubMed] [Google Scholar]
- 24. Franks MM, Stephens MA, Rook KS, et al. Spouses' provision of health‐related support and control to patients participating in cardiac rehabilitation. J Fam Psychol. 2006;20:311–318. [DOI] [PubMed] [Google Scholar]
- 25. Perk J, De Backer G, Gohlke H, et al. European Guidelines on cardiovascular disease prevention in clinical practice (version 2012). The Fifth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of nine societies and by invited experts) [published correction appears in Eur Heart J. 2012;33:2126]. Eur Heart J. 2012;33:1635–1701. [DOI] [PubMed] [Google Scholar]
- 26. Eichler K, Wieser S, Brügger U. The costs of limited health literacy: a systematic review. Int J Public Health. 2009;54:313–324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Webster R, Heeley E. Perceptions of risk: understanding cardiovascular disease. Risk Manag Healthc Policy. 2010;3:49–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Ton VK, Martin SS, Blumenthal RS, et al. Comparing the new European cardiovascular disease prevention guideline with prior American Heart Association guidelines: an editorial review. Clin Cardiol. 2013;36:E1–E6. [DOI] [PMC free article] [PubMed] [Google Scholar]


