ABSTRACT
Background
Imaging cardiac stress test use has risen significantly, leading to the development of appropriate use criteria. Prior studies have suggested the rate of inappropriate testing is 13% to 14%, but inappropriate testing in hospitalized patients has not been well studied.
Hypothesis
Appropriate use of stress testing in hospitalized patients is not comparable to the ambulatory setting.
Methods
We studied 459 consecutive patients referred for imaging stress tests (nuclear imaging or stress echocardiography) at a single institution over a 6‐month period. Appropriate use was determined by research cardiologists blinded to patient outcomes.
Results
Most tests (68%) were in patients with chest pain or possible acute coronary syndrome (ACS). Another 20% were for preoperative evaluation. The rate of inappropriate testing was 13%. Imaging modality did not correlate with appropriate use. Only 2% of the chest pain or possible ACS were inappropriate, compared to 49% of the preoperative exams (P < 0.001). The most common reason a test was considered inappropriate was for a low‐risk patient for preoperative exam (77% of inappropriate tests). Using Thrombolysis in Myocardial Infarction score 0 to define inappropriate testing in the possible ACS cohort might make an additional 27% inappropriate.
Conclusions
The rate of inappropriate use of cardiac stress testing with imaging in the inpatient setting is similar to that in the ambulatory setting. However, there is wide variation in inappropriate testing based on the indication for the test. Taking risk into consideration in possible ACS patients could result in a larger number of tests being considered inappropriate.
Introduction
The number of cardiac stress tests with imaging, both myocardial perfusion imaging (MPI) and stress echocardiography (SE), have risen dramatically over the past 2 decades.1, 2, 3 Yet, the increase in testing did not result in appreciable improvements in patient outcomes,1, 4 and testing itself is not without risk.5 These findings led to the development of appropriate use criteria (AUC), to ensure optimal patient care.6, 7 Application of the AUC has shown variable rates of inappropriate testing, with the largest studies finding inappropriate use in the range of 13% to 14%.8, 9 These studies have focused primarily or exclusively on ambulatory patients.
Chest pain is among the most common complaints of patients presenting to the emergency department.10 Many of these patients are low risk and can be safely discharged with limited testing11, 12, 13; however, cardiac stress testing is still frequently performed.14 Other uses of cardiac stress testing in the hospital setting, such as for patients with cardiac complaints other than chest pain or for preoperative testing, have been less well studied. A better understanding of the utilization and degree of appropriateness of cardiac stress testing in the hospital setting could have significant impact on the quality and cost of care provided to a large number of patients.
The purpose of our study was to determine the rate of inappropriate cardiac stress testing, both MPI and SE, in hospitalized patients. We hypothesized that the rate of inappropriate testing would be low in patients presenting with angina or an ischemic equivalent, despite patients being at low risk, due to limits in the current AUC. We also hypothesized that the rate of inappropriate testing would be higher for other indications.
Methods
Patient Selection
All patients referred for MPI or SE from September 1, 2010 through February 28, 2011, at the Hospital of the University of Pennsylvania, were included in the study. All patient data were collected prospectively as part of an ongoing quality‐improvement initiative. The determination of appropriate use was performed retrospectively as described below. The protocol was approved by the institutional review board. Complete data were available on all patients.
Determination of Appropriate Use
All cardiac stress tests were reviewed by 2 research cardiologists with nuclear and echocardiographic certification at the end of the data collection period, applying the most recent AUC for MPI and SE.6, 7 The reviewers were blinded to the results of the test and the subsequent hospital course. There was a very strong agreement (agreement 94%, kappa 0.82) using the 3‐part AUC determination (appropriate, unclear, inappropriate) and an even stronger correlation when the studies were dichotomized (inappropriate or uncertain/appropriate) (agreement 97%, kappa 0.85). For those cases where there was a disagreement, a third reviewer made the final determination.
Statistical Analysis
All patients had baseline clinical information collected prior to testing. For patients presenting with acute chest pain or an ischemic equivalent, a Thrombolysis in Myocardial Infarction (TIMI) score was calculated. The primary analysis was the rate of inappropriate cardiac stress testing. Prespecified subanalyses included the clinical predictors of inappropriate testing, comparisons between MPI and SE, and comparisons based on the indication for testing. We also compared the rate of inappropriate testing based on TIMI scores where appropriate. Continuous variables were compared using a t test, and categorical variables were compared with a Fisher exact test. To determine the independent predictors of inappropriate testing, we performed binary logistic regression using the predictors that were significant on univariate analyses. All tests of significance were 2‐sided, and P < 0.05 was considered significant.
Results
A total of 459 cardiac stress tests with imaging were performed during the study period, with data available for all patients. The AUC could not be applied in 2 patients whose clinical scenarios were not covered, and the remaining 457 form the cohort for this analysis. Baseline characteristics, stratified by type of test, are shown in Table 1. Overall, the patients referred for MPI were at higher risk than those referred for SE, with more frequent history of coronary disease, hypertension, and hyperlipidemia.
Table 1.
Patient Characteristics Stratified by Imaging Modality
| All Patients, n = 457 | Myocardial Perfusion Imaging, n = 369 | Stress Echocardiography, n = 88 | P Valuea | |
|---|---|---|---|---|
| Age, y | 61.2 ± 13.9 | 62.2 ± 13.7 | 56.9 ± 14.0 | 0.001 |
| Male | 55%, n = 250 | 55%, n = 201 | 56%, n = 49 | 0.90 |
| White | 46%, n = 211 | 46%, n = 170 | 47%, n = 41 | 0.93 |
| Known coronary disease | 30%, n = 138 | 34%, n = 124 | 16%, n = 14 | 0.001 |
| Diabetes | 30%, n = 137 | 31%, n = 115 | 25%, n = 22 | 0.30 |
| Hypertension | 77%, n = 350 | 83%, n = 306 | 50%, n = 44 | <0.001 |
| Tobacco use | 27%, n = 123 | 29%, n = 106 | 19%, n = 17 | 0.08 |
| Hyperlipidemia | 56%, n = 255 | 62%, n = 230 | 28%, n = 25 | <0.001 |
| TIMI score ≤2b | 70%, n = 218/312 | 64%, n = 163/254 | 95%, n = 55/58 | <0.001 |
Abbreviations: TIMI, Thrombolysis in Myocardial Infarction.
P value compares myocardial perfusion imaging to stress echocardiography.
TIMI scores are only for patients presenting with chest pain or possible acute coronary syndrome.
The indications for testing are shown in the Figure 1. There were no significant differences in testing indication based on the type of test ordered (P = 0.6 for comparison). Sixty‐eight percent of the tests were performed for patients with chest pain or an ischemic equivalent, nearly all of which were considered acute, and therefore were categorized as possible acute coronary syndrome (ACS). These patients were mostly at low risk, with 70% having a TIMI score of ≤2, and 27% having a TIMI score of 0. An additional 20% of studies were for preoperative risk assessment. Of the remaining patients, 2% were asymptomatic. Patient characteristics based on indication for testing are shown in Table 2.
Figure 1.
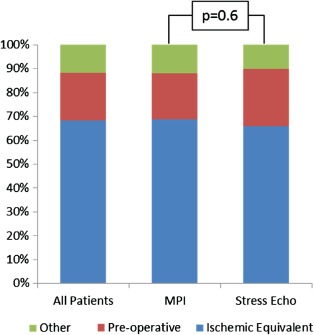
Indications for cardiac stress testing stratified by imaging modality. Chest pain/acute coronary syndrome includes all patients presenting with possible acute coronary syndrome. Abbreviations: MPI, myocardial perfusion imaging.
Table 2.
Patient Characteristics Stratified by Testing Indication
| Chest Pain/Possible ACS, n = 312 | Preoperative Evaluation, n = 92 | Other Indications, n = 53 | P Valuea | |
|---|---|---|---|---|
| Age, y | 59.9 ± 13.7 | 66.8 ± 11.4 | 60.7 ± 14.0 | <0.001 |
| Male | 51%, n = 159 | 64%, n = 59 | 60%, n = 32 | 0.03 |
| White | 36%, n = 113 | 75%, n = 69 | 55%, n = 29 | <0.001 |
| Known coronary disease | 31%, n = 97 | 25%, n = 23 | 34%, n = 18 | 0.30 |
| Diabetes | 29%, n = 90 | 36%, n = 33 | 26%, n = 14 | 0.20 |
| Hypertension | 79%, n = 246 | 80%, n = 74 | 57%, n = 30 | 0.88 |
| Tobacco use | 28%, n = 87 | 27%, n = 25 | 21%, n = 11 | 0.99 |
| Hyperlipidemia | 56%, n = 174 | 57%, n = 52 | 55%, n = 29 | 0.91 |
Abbreviations: ACS, acute coronary syndrome.
P values are for comparisons between the chest pain/possible ACS group and the preoperative evaluation group.
Overall, 13% of cardiac stress tests with imaging were considered inappropriate. Of those deemed inappropriate, over three‐fourths were preoperative evaluations (Table 3). There was no significant difference based on the imaging modality (12% of MPI vs 15% of SE, P = 0.47). Inappropriately tested patients were more likely to be white, and less likely to have known coronary artery disease or diabetes (Table 4). There were significant differences based on the indication for testing, with only 2% of patients tested for chest pain or possible ACS considered inappropriate, compared to 49% of patients tested for preoperative evaluation (P < 0.001). Asymptomatic patients accounted for 9% of the inappropriate tests (5 inappropriate out of 8 studied). The TIMI score had no impact on whether a test was considered inappropriate. Binary logistic regression analysis showed that known coronary artery disease (P = 0.002), diabetes (P = 0.004), and preoperative evaluation as the indication for testing (P < 0.001) were independently associated with inappropriate testing.
Table 3.
Inappropriate Testing Indications Stratified by Imaging Modality
| Indication | No. of Myocardial Perfusion Imaging, n = 32 | No. of Stress Echocardiography, n = 25 |
|---|---|---|
| Asymptomatic, low CAD risk | 3 | |
| Asymptomatic, intermediate CAD risk, ECG interpretable | 1 | |
| Asymptomatic, known CAD, last stress imaging <2 years | 1 | |
| Definite acute coronary syndrome | 1 | |
| Intermediate risk surgery, moderate/good functional status | 5 | |
| Intermediate risk surgery, no clinical risk factors | 7 | 6 |
| Nonacute chest pain, low pretest probability CAD, ECG interpretable, able to exercise | 3 | 1 |
| Vascular surgery, asymptomatic <1 year following normal testing or catheterization, or revascularization | 1 | |
| Syncope, low CAD risk | 1 | 1 |
| Vascular surgery, moderate/good functional status | 9 | |
| Vascular surgery, no clinical risk factors | 17 |
Abbreviations: CAD, coronary artery disease; ECG, electrocardiograph.
Table 4.
Clinical Characteristics of Inappropriate Testing
| Inappropriate, n = 57 | Appropriate or Uncertain, n = 400 | P Value | |
|---|---|---|---|
| Age, y | 62.1 ± 12.8 | 61.1 ± 14.1 | 0.61 |
| Male | 67%, n = 38 | 53%, n = 212 | 0.06 |
| White | 72%, n = 41 | 43%, n = 170 | <0.001 |
| Known coronary disease | 11%, n = 6 | 33%, n = 132 | <0.001 |
| Diabetes | 18%, n = 10 | 32%, n = 127 | 0.03 |
| Hypertension | 67%, n = 38 | 78%, n = 312 | 0.07 |
| Tobacco use | 33%, n = 19 | 26%, n = 104 | 0.27 |
| Hyperlipidemia | 47%, n = 27 | 57%, n = 228 | 0.20 |
| TIMI score ≤2a | 80%, n = 4/5 | 70%, n = 214/305 | 0.62 |
Abbreviations: TIMI, Thrombolysis in Myocardial Infarction.
TIMI scores are only for patients presenting with chest pain or possible acute coronary syndrome.
Discussion
We studied the rate of inappropriate cardiac stress testing with imaging according to AUC guidelines at a large academic medical center and found it to be 13%. Although appropriateness was similar regardless of the type of stress testing (MPI or SE), there were significant variations based on the indication for testing. Patients with chest pain or possible ACS, by far the most common reason for testing, had a very low rate of inappropriate testing at only 2%. Preoperative evaluation, the second most common indication, had a much higher rate of inappropriate testing at 49%.
Although the overall rate of inappropriate testing in our cohort is the same as Hendel et al found in a large cohort of ambulatory patients, this may not be a suitable comparison as the patient populations are very different.9 In that study, asymptomatic patients accounted for over two‐thirds of the inappropriate studies, whereas in our study only 9% of the inappropriate tests were in asymptomatic patients. Only 4% of the inappropriate ambulatory cardiac stress tests were preoperative evaluations, whereas that indication accounted for 77% of the inappropriate tests in our study.
We believe that the low rate of inappropriate testing in patients presenting with chest pain may be reflective of limitations in the AUC in the hospital setting. Any patient with possible or suspected ACS is considered appropriate for imaging testing, without consideration of patient risk. Yet the MPI AUC document mentions that the writing group felt that a TIMI score ≤2 identified low‐risk patients.6 Penumetsa et al have shown that although pretest risk of coronary artery disease has a significant impact on the likelihood of a positive cardiac stress test, it has very little impact on the decision to order the test, with over two‐thirds of low‐risk patients receiving imaging stress tests.14 In our cohort, even a more conservative threshold using a TIMI score of 0 would have rendered as much as 27% of those patients inappropriate for imaging testing and would have markedly altered our primary end point. This presumes that those patients would be appropriate candidates for treadmill electrocardiograph testing or some other type of risk stratification.
Risk level is incorporated into the AUC recommendations regarding chronic stable angina patients and preoperative evaluations. In both settings, there is a clear distinction between patients at low and moderate risk of having coronary artery disease. We believe that it should be incorporated into the recommendations for suspected ACS as well. There is evidence that low‐risk patients can be treated safely without imaging. Randomized trials have shown that low‐risk patients can be safely discharged without imaging cardiac stress tests, with no impact on clinical events.11, 13 In a study of 1000 low‐risk patients evaluated with exercise testing without imaging, there was only 1 cardiac event in the group of 640 patients with negative tests over a 30‐day follow‐up.12
Some drivers of inappropriate testing, including gaps in physician education and medicolegal concerns, are likely to be equally present in both the ambulatory and inpatient setting, whereas others, particularly financial considerations, are less likely translatable. Some have suggested that financial incentives for the ordering physician have driven the rise in cardiac stress testing in the ambulatory setting, possibly resulting in unnecessary tests. Third‐party payers, using prior authorization and radiology benefits managers, may refuse to pay for tests that appear to be clinically appropriate.3, 15 These financial influences may have less impact in the inpatient setting, where the ordering physician may be less likely to be the interpreting physician, and the payer is more likely to pay for the patient's care in a single payment, giving the payer less impetus to be involved in the choice of testing regimen. How these considerations might impact efforts to improve appropriate use in the hospital setting has not been well studied.
Limitations
A limitation of our study is that it is a single‐center, urban academic hospital experience. Whether this would be as applicable in nonteaching institutions or in a suburban or rural setting requires further study.
Conclusion
We applied the AUC to cardiac stress testing with imaging in the hospital setting, and found that 13% were inappropriate. Although the testing modality was not predictive of appropriate use, we found that a much higher percentage of preoperative tests were inappropriate than those ordered to evaluate for chest pain or suspected ACS. Because risk is not considered in patients being evaluated for possible ACS, very few of these imaging tests are considered inappropriate by the current AUC.
The authors have no funding, financial relationships, or conflicts of interest to disclose.
References
- 1. Lucas FL, DeLorenzo MA, Siewers AE, et al. Temporal trends in the utilization of diagnostic testing and treatments for cardiovascular disease in the United States, 1993‐2001. Circulation. 2006;113:374–379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Department of Health and Human Services . Office of Inspector General. Growth in advanced imaging paid under the Medicare physician fee schedule. October 2007. http://oig.hhs.gov/oei/reports/oei‐01‐06‐00260.pdf. Accessed November 19, 2013.
- 3. Hendel RC. Utilization management of cardiovascular imaging: pre‐certification and appropriateness. JACC Cardiovasc Imaging. 2008;1:241–248. [DOI] [PubMed] [Google Scholar]
- 4. Garber AM, Solomon NA. Cost‐effectiveness of alternative test strategies for the diagnosis of coronary artery disease. Ann Intern Med. 1999;130:719–728. [DOI] [PubMed] [Google Scholar]
- 5. Einstein AJ, Weiner SD, Bernheim A, et al. Multiple testing, cumulative radiation dose, and clinical indications in patients undergoing myocardial perfusion imaging. JAMA. 2010;304:2137–2144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Hendel RC, Berman DS, Di Carli MF, et al. ACCF/ASNC/ACR/AHA/ASE/SCCT/SCMR/SNM 2009 appropriate use criteria for cardiac radionuclide imaging: a report of the American College of Cardiology Appropriate Use Criteria Task Force, the American Society of Nuclear Cardiology, the American College of Radiology, the American Heart Association, the American Society of Echocardiography, the Society for Cardiac Computed Tomography, the Society for Cardiac Magnetic Resonance, and the Society of Nuclear Medicine. J Am Coll Cardiol. 2009;53:2201–2229. [DOI] [PubMed] [Google Scholar]
- 7. Douglas PS, Garcia MJ, Haines DE, et al. ACCF/ASE/AHA/ASNC/HFSA/HRS/SCAI/SCCM/SCCT/SCMR 2011 appropriate use criteria for echocardiography: a report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, American Society of Echocardiography, American Heart Association, American Society of Nuclear Cardiology, Heart Failure Society of America, Heart Rhythm Society, Society for Cardiovascular Angiography and Interventions, Society of Critical Care Medicine, Society of Cardiovascular Computed Tomography, and Society for Cardiovascular Magnetic Resonance. J Am Soc Echocardiogr. 2011;24:229–367. [DOI] [PubMed] [Google Scholar]
- 8. Mehta R, Ward RP, Chandra S, et al. Evaluation of the American College of Cardiology Foundation/American Society of Nuclear Cardiology appropriateness criteria for SPECT myocardial perfusion imaging. J Nucl Cardiol. 2008;15:337–344. [DOI] [PubMed] [Google Scholar]
- 9. Hendel RC, Cerqueira M, Douglas PS, et al. A multicenter assessment of the use of single‐photon emission computed tomography myocardial perfusion imaging with appropriateness criteria. J Am Coll Cardiol. 2010;55:156–162. [DOI] [PubMed] [Google Scholar]
- 10. Niska R, Bhuiya F, Xu J. National Hospital Ambulatory Medical Care Survey: 2007 Emergency Department Summary. Natl Health Stat Report. 2010;26:1–31. [PubMed] [Google Scholar]
- 11. Gomez MA, Anderson JL, Karagounis LA, et al. An emergency department‐based protocol for rapidly ruling out myocardial ischemia reduces hospital time and expense: results of a randomized study (ROMIO). J Am Coll Cardiol. 1996;28:25–33. [DOI] [PubMed] [Google Scholar]
- 12. Amsterdam EA, Kirk JD, Diercks DB, et al. Immediate exercise testing to evaluate low‐risk patients presenting to the emergency department with chest pain. J Am Coll Cardiol. 2002;40:251–256. [DOI] [PubMed] [Google Scholar]
- 13. Jeetley P, Burden L, Stoykova B, et al. Clinical and economic impact of stress echocardiography compared with exercise electrocardiography in patients with suspected acute coronary syndrome but negative troponin: a prospective randomized controlled study. Eur Heart J. 2007;28:204–211. [DOI] [PubMed] [Google Scholar]
- 14. Penumetsa SC, Mallidi J, Friderici JL, et al. Outcomes of patients admitted for observation of chest pain. Arch Intern Med. 2012;172:873–877. [DOI] [PubMed] [Google Scholar]
- 15. Willens HJ, Nelson K, Hendel RC. Appropriate use criteria for stress echocardiography: impact of updated criteria on appropriateness ratings, correlation with pre‐authorization guidelines, and effect of temporal trends and an educational initiative on utilization. JACC Cardiovasc Imaging. 2013;6:297–309. [DOI] [PubMed] [Google Scholar]


