ABSTRACT
Objective: To report the trends in quality of life (QoL) reporting for radical cystectomy (RC) and urinary diversion (UD) over the last four decades, as RC for bladder cancer is associated with significant morbidity and QoL issues.
Material and methods: We searched PubMed, Medical Literature Analysis and Retrieval System Online (MEDLINE), Excerpta Medica dataBASE (EMBASE), Cumulative Index to Nursing and Allied Health Literature (CINAHL), and the Cochrane library for published studies from January 1980 to January 2017 in the English language. We divided the published articles into three time periods: period-1 (1980–1997), period-2 (1998–2007) and period-3 (2008–2017).
Results: A total of 85 QoL studies (8417 patients) were identified, of which 3347 (39.8%) patients had an ileal conduit (IC), 1078 (12.8%) had a continent UD (CD), 3264 (38.8%) had a neobladder (NB), and in the remaining 728 (8.6%) the type of UD was not specified. Whilst there were 15, 24 and 41 studies in period-1, period-2 and period-3 respectively, two (13%), 20 (83%) and 37 (90%) used a validated QoL tool; and none, six (25%) and 23 (56%) used a urology specific QoL tool during these three time periods. Similarly, the number of prospective studies increased from one (7%) to four (17%) and 14 (34%) in these three time periods. The proportion of reported IC patients reduced from 65% (784 patients) to 36% (899) and 35% (1664) from period-1 to period-3, whereas the proportion of NB patients increased from 4.5% (54) to 44% (1105) and 44% (2105). Over the last few years there have been QoL studies on laparoscopic and robotic IC and NB UDs.
Conclusion: Our review suggests an increasing use of validated, bladder cancer-specific questionnaires with UD-specific constructs.
Abbreviations: BCI: Bladder Cancer Index; BDI: Beck Depression Inventory; BIS: Body Image Scale; CD: continent urinary diversion; EORTC QLQ-30C: European Organisation for the Research and Treatment of Cancer Quality of Life 30-item core questionnaire; ERAS: enhanced recovery after surgery; FACT(-BL)(-G)(-VCI): Functional Assessment of Cancer Therapy(-Bladder Cancer)(-General)(-Vanderbilt Cystectomy Index); IC: ileal conduit; NB: neobladder; (HR)QoL: (health-related) quality of life; (RA)RC: (robot-assisted) radical cystectomy; SF-36: 36-item short-form health survey; SIP: Sickness Impact Profile; UD: urinary diversion
KEYWORDS: Quality of life, cystectomy, ileal conduit, neobladder, urinary diversion, review
Introduction
Radical cystectomy (RC) with urinary diversion (UD) is associated with significant morbidity. Once patients recover from this surgery, quality of life (QoL) becomes an important priority having a significant role in their future psychological and emotional well-being [1–3]. UD impacts QoL and there are different types of UD to choose from, including ileal conduit (IC) to continent cutaneous UD (CD) and neobladder (NB) [3–8].
Measuring QoL can help assess the impact of RC and UD, identify patient preference, help in staff training, and be useful for audit and clinical governance [1]. The choice of UD depends on patient suitability and preference, with a possible surgical bias related to the surgical expertise available in the centre. Whilst enthusiasts favour NB, there is little evidence to support that one UD type is better than another [9–12]. It seems that for now, the choice of UD should be individualised and based on patient counselling and expectations, with an active but unbiased surgical input. Measuring QoL in these patients has changed from self-designed to non-validated and now validated tools, including generic and disease-specific measures. Over time the shift has been to use bladder cancer-specific health-related QoL (HRQoL) tools supplemented by patient-reported outcome measures [8,13–18].
Publication trends reflect clinical practice [19]. Trends in the type of UD offered could help patients in their choice of UD type, improve counselling and allocation of healthcare resources. The QoL aspect seems to be the most important element in UD once patients have recovered from their initial surgery. There is no bibliometric study looking at the publication trends of reporting QoL in UD patients. We therefore assessed the trend in QoL reporting after RC and UD over the last four decades.
Materials and methods
Inclusion criteria
All studies reporting on QoL after UD, irrespective of the type of UD.
Studies published in English language over the last four decades.
Exclusion criteria
Animal studies and case reports.
Studies on UD that did not assess QoL.
Search strategy and study selection
We performed a systematic review of the world literature to identify original studies reporting on QoL in UD. It was carried out using Cochrane and Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) methodology.
We searched PubMed, Medical Literature Analysis and Retrieval System Online (MEDLINE), Excerpta Medica dataBASE (EMBASE), Cumulative Index to Nursing and Allied Health Literature (CINAHL) and the Cochrane library for published studies from January 1980 to January 2017. We used the following search terms ‘urinary diversion’, ‘quality of life’, ‘neobladder’, ‘ileal conduit’, ‘cutaneous diversion’, ‘cystectomy’, ‘health-related quality of life’, and ‘QoL’. All articles from 1980 to 1997, and only articles directly comparing two or more different UD types from 1998 to 2017 were selected for screening. All full-length articles published in the English language were included in the original search and the two reviewers (K.R., B.K.S.) independently identified all studies that fitted the inclusion criteria (Figure 1).
Figure 1.
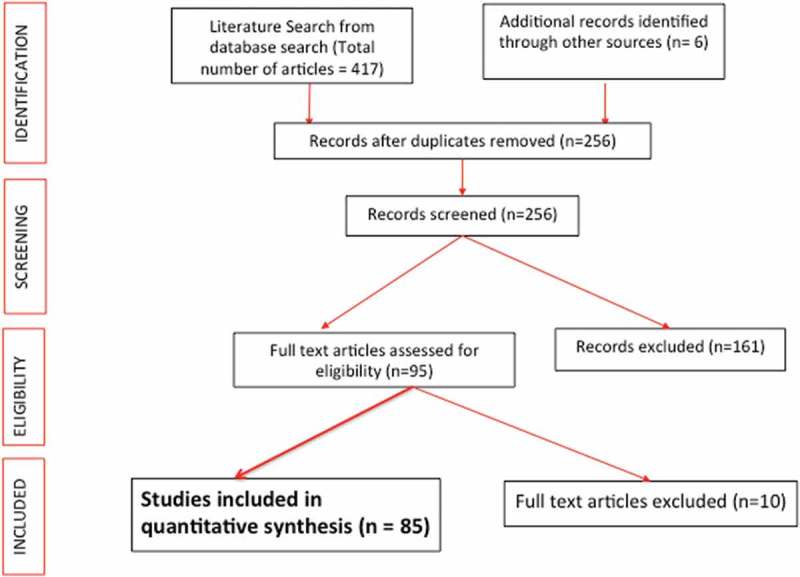
PRISMA flowchart of study inclusion.
We included all studies where patients underwent UD (1980–1997), and at least two forms of UD were used and QoL was measured using either a validated or non-validated questionnaire (1998–2017). After screening the abstracts (n = 295), 85 studies met the inclusion criteria and were included in our present review (Appendix 1). Each of the 85 studies was then assessed in a standardised fashion. The following information was collected for each study: number of patients, type of UD compared, study design, type of instrument used to assess HRQoL outcome (general vs disease-specific and validated vs non-validated), major findings of the study, and any other characteristics unique to the study.
We divided the last four decades into three time periods: period-1 (1980–1997), period-2 (1998–2007), and period-3 (2008–2017).
Primary outcome measures
Trends of QoL reporting over the last four decades.
Number of studies and type of UD done.
Secondary outcome measures
Geographical variation in the reporting of the QoL studies.
Journals which published these QoL studies.
Data extraction and analysis
Both reviewers (K.R., B.K.S.) independently identified all studies that appeared to fit the inclusion criteria and any disagreement was resolved with mutual consensus. All data were collected in an Excel spreadsheet and then transferred to a Word document. The study was carried out using the Cochrane and PRISMA methodology. Included studies showed a high level of heterogeneity and bias, and data were not suitable for a meta-analysis, and hence have been presented in a descriptive manner.
Results
Over the last 37 years, a total of 85 post-RC QoL studies (8417 patients) have been reported (Tables 1 and 2). Of these UD patients (within the 85 studies), 3347 (39.8%) had an IC, 1078 (12.8%) had a CD, 3264 (38.8%) had a NB, and in the remaining 728 (8.6%) the type of UD was not specified (Tables 1 and 2). Whilst there were 15, 24 and 41 studies in period-1, period-2, and period-3, respectively, two (13%), 20 (83%) and 37 (90%) used a validated QoL tool; and none, six (25%) and 23 (56%) used a urology specific QoL tool during these three time periods. Similarly, the number of prospective studies increased from one (7%) to four (17%) and 14 (34%) in these three time periods.
Table 1.
The number of studies and types of UD performed over the last four decades (five studies were overlapping*).
| Year | No. of countries (studies*) | No. of patients | Validated scale (urology specific) used, n | Prospective/retrospective, n | IC/CD/NB/unspecified, n | Open/lap or robotic, n |
|---|---|---|---|---|---|---|
| 1980–1997 | 6 (15) | 1206 | 2 (0) | 1/14 | 784/368/54/0 | 1206/0 |
| 1998–2007 | 11 (24) | 2464 | 20 (6) | 4/20 | 899/428/1105/32 | 2432/0 |
| 2008–2017 | 18 (41) | 4747 | 37 (23) | 14/27 | 1664/282/2105/696 | 3939/112 |
| Total | 35 (80) | 8417 | 59 (29) | 19/61 | 3347/1078/3264/728 | 7577/112 |
lap, laparoscopic.
Table 2.
QoL of the included UD studies over the last four decades (Appendix 1).
| Journal | Author | Country | Year | No. of Patients | Scale used – 1 | Scale used 2 | IC | CD | NB | CD/NB | Study type | Conclusion on QoL | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Br J Urol | Jones et al. | UK | 1980 | 34 | Self-designed questionnaire | 34 | Retro. | Stoma problems | ||||
| 2 | Scand J Urol Nephrol | Fosså et al. | Norway | 1987 | 59 | Self – psychological/social issues | 59 | Retro. | Good QoL | ||||
| 3 | J Urol | Boyd et al. | USA | 1987 | 172 | BDI, POMS, physical impact | 87 | 85 | Retro. | Preop. counselling important, patients overall satisfied but more for CD | |||
| 4 | Br J Urol | Månsson et al. | Sweden | 1988 | 60 | Self-designed questionnaire | 40 | 20 | Retro. | Less stoma problems and more freedom for activities in CD | |||
| 5 | Scand J Urol Nephrol | Mommsen et al. | Denmark | 1989 | 68 | Self-designed questionnaire | 68 | Retro. | Preop. counselling important but often neglected | ||||
| 6 | Br J Urol | Chadwick and Stower | UK | 1990 | 41 | Interview – appliance management | 41 | Retro. | 83% improved QoL, 90% continue household duty, leakage problem | ||||
| 7 | Scand J Caring Sci | Månsson et al. | Sweden | 1991 | 34 | Interview | 20 | 14 | Retro. | Sexual problems postop., lack of psychological support from health services – irrespective of UD | |||
| 8 | Br J Urol | Nordström et al. | Sweden | 1992 | 66 | Interview – sexual function | 66 | Retro. | 90% men had erectile dysfunction, 5/6 females had lower sexual activity | ||||
| 9 | Scand J Urol Nephrol | Nordström et al. | Sweden | 1992 | 66 | Interview – psychological function | 66 | Retro. | 80% overall good health, 70% unchanged social activity, leak, body image in females | ||||
| 10 | Scand J Urol Nephrol | Bjerre et al. | Denmark | 1994 | 76 | Self-designed questionnaire | 50 | 26 | Retro. | Global satisfaction high and similar in both groups | |||
| 11 | Br J Urol | Bjerre et al. | Denmark | 1995 | 67 | Interview + questionnaire | 29 | 38 | Retro. | High global satisfaction with both UDs, Urinary leak more frequent in NB, but IC patients affected more | |||
| 12 | J Urol | Gerharz et al. | Germany | 1997 | 192 | Self-designed questionnaire | 131 | 61 | Retro. | Less stoma problems in CD, overall scores similar | |||
| 13 | Int J Urol | Okada et al. | Japan | 1997 | 137 | Self-designed questionnaire | 63 | 74 | Retro. | Less stoma problems in CD, but more night catheterisations, more satisfied patients in CD, counselling/consent | |||
| 14 | Eur Urol | Filipas et al. | Germany | 1997 | 81 | Interview + questionnaire | 27 | 54 | Retro. | No difference in global satisfaction and health, UD type must consider psychological and employment status | |||
| 15 | Scand J Urol Nephrol | Bjerre et al. | Denmark | 1997 | 37 | Self-designed questionnaire | 20 | 17 | Retro. | No difference in two groups | |||
| 16 | Br J Urol | Månsson et al. | Sweden | 1997 | 50 | SIP | MCT | 17 | 17 | 16 | Pros. | Defensive strategies and philosophical outlook generally did not influence the psychosocial outcome of intervention | |
| 17 | Scand J Urol Nephrol | Bjerre et al. | Denmark | 1998 | 76 | Self-designed questionnaire | 27 | 49 | Retro. | No difference in two groups | |||
| 18 | Urology | Weijerman et al. | The Netherlands | 1998 | 56 | SIP | 23 | 33 | Retro. | Overall QoL favourable in both groups | |||
| 19 | Br J Urol | Sullivan et al. | Canada | 1998 | 86 | Urinary symptoms, activity level, overall wellbeing | 42 | 44 | Retro. | Good overall QoL, significant effect on sex life, 70% patients had no limit on activities | |||
| 20 | Br J Urol | Månsson et al. | Sweden | 1998 | 57 | Interview + questionnaire | MCT + VAS | 17 | 22 | 18 | Pros. | Patients with wet stoma did not do less well than continent procedures, and the adjustment improved with time | |
| 21 | J Urol | Hart et al. | USA | 1999 | 224 | 4 self-reporting questionnaire | 24 | 93 | 103 | Retro. | Good overall QoL in all groups | ||
| 22 | Int J Urol | Kitamura et al. | Japan | 1999 | 79 | EORTC QLQ-C30 | Self-designed questionnaire | 36 | 22 | 21 | Retro. | Little difference in all groups, patients accepted and adapted to present general quality status | |
| 23 | Qual Life Res | Hardt et al. | Germany | 2000 | 44 | SF-36 | FLZM | 24 | 20 | Pros. | High global satisfaction with both UDs, 75% would choose same UD again | ||
| 24 | Ann Surg Oncol | McGuire et al. | USA | 2000 | 92 | SF-36 | 38 | 16 | 38 | Retro. | IC patients have decreased mental QoL but continent UDs do not, compared to population norms | ||
| 25 | Urology | Fujisawa et al. | Japan | 2000 | 56 | SF-36 | 20 | 36 | Retro. | No difference in two groups | |||
| 26 | World J Urol | Hobisch et al. | Austria | 2000 | 102 | EORTC QLQ-C30 | Self-designed questionnaire | 33 | 69 | Retro. | QoL better with NB in all domains | ||
| 27 | Eur Urol | Kulaksizoglu et al. | Turkey | 2002 | 68 | EORTC QLQ-C30 | BDI | 49 | 2 | 15 | Pros. | Psychological and HRQoL measures come to baseline values and stabilise after the 12th-month period | |
| 28 | BJU Int | Månsson et al. | Sweden | 2002 | 64 | FACT-BL | HADS | 35 | 29 | Retro. | No difference overall between groups (NB – more incontinence, but better appreciation of appearance and erectile function) | ||
| 29 | BJU Int | Hara et al. | Japan | 2002 | 85 | SF-36 | 37 | 48 | Retro. | Patients satisfied with overall QoL and health status in both groups | |||
| 30 | J Urol | Dutta et al. | USA | 2002 | 72 | SF-36 | FACT-G | 23 | 49 | Retro. | NB marginally better when adjusted for age, stage and sex | ||
| 31 | Eur Urol | Henningsohn et al. | Sweden | 2003 | 395 | Self-designed questionnaire | 218 | 88 | 89 | Retro. | Compromised sexual function main source of distress in RC patients, addressing self-assessed distress may improve patient care | ||
| 32 | BJU Int | Protogerou et al. | Greece | 2004 | 108 | EORTC QLQ-C30 | Self-designed questionnaire | 58 | 50 | Retro. | QoL same in both groups. Higher emotional function compared to NB population but more urinary + sexual problems | ||
| 33 | Eur Urol | Joniau et al. | Belgium | 2005 | 58 | Self-designed questionnaire | 58 | Retro. | ONB substitution has acceptable impact on patient’s everyday life. | ||||
| 34 | J Urol | Yoneda et al. | Japan | 2005 | 48 | SF-36 | FACT-Bl | 48 | Retro. | No difference in HRQoL between patients and controls | |||
| 35 | Cancer | Allareddy et al. | USA | 2006 | 82 | FACT-BL | 56 | 26 | Retro. | No difference in IC vs continent UD; no major difference between non-RC and RC patients | |||
| 36 | Jpn J Clin Oncol | Kikuchi et al. | Japan | 2006 | 49 | FACT-BL | 20 | 14 | 15 | Retro. | QoL – no difference; body image and urinary function affected. 10/13 IC, 7/9 CD, 6/7 NB would choose same operation again | ||
| 37 | Int J Urol | Harano et al. | Japan | 2007 | 41 | SF-36 | Urinary continence questionnaire | 20 | 21 | Retro. | HRQoL in the NB group and those in the CD group were similar | ||
| 38 | Cancer | Gilbert et al. | USA | 2007 | 188 | BCI | 66 | 122 | Retro. | More urinary leak in NB | |||
| 39 | Acta Med Okayama | Saika et al. | Japan | 2007 | 109 | EORTC QLQ-C30 | Patient satisfaction | 56 | 31 | 22 | Retro. | No difference in HRQoL, more patients disappointed with NB – preop. counselling | |
| 40 | Urology | Månsson et al. | Sweden | 2007 | 61 | FACT-BL | HADS | 61 | Pros. | Swedish men had better FACT-BL and HADS scores, patient assessed outcome differ with different populations | |||
| 41 | Eur J Surg Oncol | Autorino et al. | Italy | 2008 | 79 | SF-36 | 44 | 35 | Retro. | No significant difference in scores between IC and NB. Compared to control population – physical, social and emotional functioning worse in both IC and NB groups | |||
| 42 | Urology | Sogni et al. | Italy | 2008 | 85 | EORTC QLQ-C30 | EORTC QLQ-BLM30 | 53 | 32 | Retro. | No difference in QoL or complications and survival | ||
| 43 | BJU Int | Yuh et al. | USA | 2009 | 34 | FACT-BL | 34 | Pros. | Pre- and post-RC QoL, postop. QoL scores similar at 3 months and exceeded baseline at 6 months | ||||
| 44 | Scand J Urol Nephrol | Frich et al. | Norway | 2009 | 72 | Self-designed questionnaire | 37 | 35 | Retro. | Patients with all UDs rated their QoL as high with no significant difference between them. More patients in NB group experienced practical problems compared to IC. Influence on everyday life was significantly better in favour of IC compared to NB. | |||
| 45 | Ann R Coll Surg Engl | Philip et al. | UK | 2009 | 52 | SF-36 | 24 | 28 | Retro. | NB patients were younger and more fit. HRQoL was favourable in both UDs, with physical functioning significantly better in NB group. Conclude – body image issues persist although no formal body image measures used. | |||
| 46 | Urology | Somani et al. | UK | 2009 | 32 | SWLS | EORTC QLQ-C30 | 29 | 3 | Pros. | No difference in scores between IC and NB | ||
| 47 | BJU Int | Miyake et al. | Japan | 2010 | 80 | SF-36 | 80 | Retro. | HRQoL similar except physical health, emotional problems and bodily pain, which were worse in NB patients. No difference between men and women. | ||||
| 48 | J Urol | Large et al. | USA | 2010 | 40 | FACT-VCI | 19 | 21 | Retro. | Women undergoing RC with ONB vs IP have similar HRQoL outcomes | |||
| 49 | Urology | Hedgepeth et al. | USA | 2010 | 336 | BCI | BIS | 85 | 139 | Pros. | Longest F/U – 8 years. Initial worsening of body image in both UDs. Earlier return of body image to baseline for IC, with NB never returning to baseline. Age but not sex associated with body image with older patients having better body image | ||
| 50 | Int Urol Nephrol | Vakalopoulos et al. | Greece | 2011 | 39 | FACT-G | FACT-VCI; BDI; SF-36 | 14 | 25 | Retro. | Patients with UUC surprisingly presented at least equal QoL than the presumably less debilitating ONB | ||
| 51 | ISRN Urol | Erber et al. | Germany | 2012 | 301 | EORTC QLQ-C30 | BLM30 | 146 | 115 | Retro. | Many arguments in favour of NB rather than IC as the UD of choice. | ||
| 52 | Urology | Anderson et al. | USA | 2012 | 190 | FACT-VCI | 70 | 101 | Retro. | Patients with IC had VCI scores that averaged 5 points > than those who had an ONB UD at 1-year postop. | |||
| 53 | Eur J Surg Oncol | Miyake et al. | Japan | 2012 | 212 | SF-36 | 212 | Retro. | HRQoL with NB is generally favourable irrespective of the type of NB | ||||
| 54 | Urology | Stegemann et al. | USA | 2012 | 91 | CARE questionnaire | 84 | 6 | Pros. | Initial decline in QoL after surgery but approached preoperative baseline levels at ≤90 days | |||
| 55 | Cir Esp | Mucciardi et al. | Italy | 2013 | 58 | EORTC QLQ-C30 | 58 | Retro. | Cutaneous ureterostomy represents a valuable alternative for elderly patients with high surgical risk | ||||
| 56 | Acta Inform Med | Prcic et al. | Bosnia & Hersegovina | 2013 | 106 | SIP | 66 | 20 | 20 | Pros. | NB provides significantly better QoL than IC | ||
| 57 | Korean J Urol | Shim et al. | South Korea | 2013 | 42 | K-BIS | Author-constructed questionnaire | 13 | 29 | Retro. | NB was associated with significantly better body image than IC | ||
| 58 | Mol Clin Oncol | Yang et al. | China | 2013 | 82 | SF-36 | Continence questionnaire (NB group only) | 28 | 54 | Pros. | SF-36 scores were significantly greater following NB than non-NB – total health scores were higher | ||
| 59 | Can J Urol | Metcalfe et al. | Canada | 2013 | 84 | FACT-VCI | 53 | 31 | Retro. | No statistically significant association between the type of UD and QoL | |||
| 60 | Urol Ann | Asgari et al. | Iran | 2013 | 149 | Author-constructed questionnaire | 70 | 16 | 63 | Pros. | Global satisfaction was higher with CD and NB compared with IC. Continent UD provides better results in terms of QoL compared to IC | ||
| 61 | Cent Eur J Urol | Aboumarzouk et al. | Poland | 2013 | 63 | Assessment based on psychological, social, sexual and physical states (no particular scale used) | 39 | 24 | Pros. | No difference between the groups regarding QoL; no difference between either UD in all comparative aspects e.g. length of hospital stay, complications etc., except that the NB had a longer operative time | |||
| 62 | Health Qual Life Outcomes | Gacci et al. | Italy | 2013 | 37 | EORTC QLQ-C30 | FACT-BL and QLQ-BLM30 | 16 | 12 | 9 | Retro. | Patients with cutaneous ureterostomy had worse HRQoL compared to those who underwent IC or NB, primarily due to physical/emotional perception of body image. | |
| 63 | J Urol | Parekh et al. | USA | 2013 | 40 | Pros. | |||||||
| 64 | Arch Esp Urol | Fuentes et al. | Spain | 2014 | 25 | FACT-Bl | 2 | 19 | 3 | Retro. | Ureterosigmoidostomy may be a good choice for UD in selected patients, with similar QoL to other types of UD | ||
| 65 | Urol Oncol | Miyake et al. | Japan | 2014 | 234 | SF-36 | 234 | Retro. | Both types resulted in satisfactory outcomes; sigmoid NB group appeared to be more favourable than ileal NB group in terms of long-term voiding function | ||||
| 66 | Ann Surg Oncol | Rouanne et al. | France | 2014 | 31 | SF-12 | Urinary symptom profile/Contilife questionnaire | 31 | Retro. | Ileal NB reconstruction provides long-term satisfaction with maintained HRQoL | |||
| 67 | BJU Int | Singh et al. | India | 2014 | 164 | EORTC QLQ-C30 | 80 | 84 | Pros. | NB better QoL outcomes than IC | |||
| 68 | Urology | Large et al. | USA | 2014 | 73 | FACT-VCI | 27 | 16 | Pros. | Scores did not statistically differ from baseline to 6-month follow-up between UD types | |||
| 69 | Urology | Aboumohamed et al. | USA | 2014 | 182 | BCI | BIS | 182 | Retro. | RARC has comparable HRQoL outcomes to open RC; UD technique does not appear to affect QoL | |||
| 70 | BJU Int | Poch et al. | USA | 2014 | 43 | BCI | EORTC-BIS | 38 | 5 | ? | HRQoL outcomes after RARC show recovery of urinary and bowel domains at ≤6 months | ||
| 71 | Int J Urol | Zahran et al. | Egypt | 2014 | 74 | EORTC QLQ-C30 | FACT-Bl | 74 | Retro. | After ONB in women, HRQoL is lower than that of the normal population – night time incontinence being a particular issue | |||
| 72 | World J Urol | Mischinger et al. | Germany | 2014 | 56 | SF-36 | QLQ-C30 + QLQ-BLM30 + TNQ | 56 | Pros. | Contradictory results – suggest that the questionnaires are not useful to evaluate HRQoL in patients with different NBs | |||
| 73 | BJU Int | Messer et al. | USA | 2014 | 40 | FACT-VCI | 37 | 3 | Pros. | HRQoL returns to baseline 3 months post-RC, with no significant difference in HRQoL between open RC and RARC | |||
| 74 | BMC Urol | Huang et al. | China | 2015 | 294 | EORTC-QOL | BIS, BCI | 78 | 39 | Retro. | The mean BIS score in ileal ONB group patients was significantly better than that in IC group patients at the 1-year follow-up, but there was no significant difference at the long-term follow-up. | ||
| 75 | Urol Oncol | Goldberg et al. | Israel | 2015 | 95 | BCI | 49 | 46 | Retro. | Increased risk of urinary incontinence and sexual dysfunction for NB reconstruction vs IC | |||
| 76 | Eur Urol | Bochner et al. | USA | 2015 | 124 | Self-designed questionnaire | Global health, side effects, emotional | 27 (r), 23 (o) | 0 (r), 3(o) | 33 (r) 32 (o) | Pros. | There were no clinical or statistical differences between the two arms in QoL change from baseline to 3 month or from 3 to 6 months in any of the evaluated domains | |
| 77 | Eur Urol | Satkunasivam et al. | USA | 2016 | 107 | Modified BCI, SF-36 | mucus- and pad-related questions included | 28 (r), 79 (o) | Retro. | Ileal ONB had comparable bladder cancer-specific HRQOL scores to open ONB. However, pad size and daytime wetness were worse for ileal ONB, albeit over a significantly shorter follow-up | |||
| 78 | BJU Int | Longo et al. | Italy | 2016 | 70 | BCI – translated to Italian | Likert scale, BCI assessed stoma and appliance function | 35 | 35 | Retro. | Chronic ureteric stenting does not affect the QoL of patients with bladder cancer undergoing CD compared with those undergoing IC UD. | ||
| 79 | Oncol Lett | Liu et al. | China | 2016 | 85 | Karnofsky performance scale (functional), FACT-G, BSS | 27 | 28 (traditional), 30 (tubeless) | Retro. | The HRQoL scores of the patients in the improved group were significantly higher than those of the patients in the other two groups, and the difference was statistically significant | |||
| 80 | Eur Urol | Khan et al. | UK | 2016 | 164 | FACT-Bl | BCa; Bladder Cancer Subscale | 17 (o), 3 (r), 18 (l) | 3 (o), 2 (r), 1 (l) | Pros. | There were no statistically significant relationships in QoL according to surgical arm (o, open; r, robotic; l, laparoscopic) | ||
| 81 | J Urol | Winters et al. | USA | 2018 | 166 | Retro. | |||||||
| 82 | Minerva Urol Nefrol | Zahran et al. | Egypt | 2017 | 145 | EORTC-QLQ-C30 (translated to Arabic) | FACT-Bl | 64 | 84 | Retro. | In women, HRQoL is better after ONB than IC as long as continence status is preserved. If incontinence is expected, IC may be a better option for UD. | ||
| 83 | Urology | Gellhaus et al. | USA | 2017 | 128 | BCI | 44 | 48 | 36 (IP) | Retro. | Urinary function but not urinary bother was significantly better in IC and IP compared to NB UDs. Older men with IC had better urinary function than older men with NB. In younger men, IP patients had significantly better urinary function than NB patients. | ||
| 84 | Eur J Surg Oncol | Mischinger et al. | Germany | 2017 | 56 | GIQLI | 23 (Studer) 33(I-pouch) | Retro. | No significant differences in postoperative bowel disorders were found between both NB types | ||||
| 85 | World J Urol | Kretschmer et al. | Germany | 2017 | 121 | EORTC–QLQ-C30 – German translation | ICIQ-SF questionnaire | 50 | 50 | Retro. | ONB is an independent predictor for better overall HRQoL at 3 months, but not 12 months after RC (global health score, physical functioning, role functioning) | ||
CARE, Convalescence and Recovery Evaluation; GIQLI, Gastrointestinal Quality of Life Index: FLZM, Fragen zur Lebenszufriedenheit; HADS, Hospital Anxiety and Depression Scale; ICIQ-SF, International Consultation on Incontinence Questionnaire short form; IP, Indiana pouch; l, laparoscopic; MCT, meta-contrast technique; o, open; ONB, orthotopic NB; Pros., prospective; POMS, profile of mood status; r, robotic; Retro., retrospective; SWLS, Satisfaction With Life Scale; TNQ, neobladder-specific questionnaire; UUC, uretero-ureterocutaneostomy; VAS, visual analogue scale.
The overall proportion of reported IC patients reduced from 65% (784 patients) to 36% (899) and 35% (1664) from period-1 to period-3, whereas the proportion of reported NB patients increased from 4.5% (54) to 44% (1105) and 44% (2105). The reporting of both the UD types was broadly similar over the last two decades. Over the last few years there have also been QoL studies on laparoscopic and robot-assisted IC and NB UDs.
Overall, 43 (51%) studies came from Europe, 22 (26%) from the USA, and 16 (19%) from Asia (Table 3), with 16 studies published in BJU International (British Journal of Urology before 1999) and 10 studies in Urology.
Table 3.
Geographical density and impact of studies over the last four decades.
| Year | Number and country | Number and continent | Number and Journal |
|---|---|---|---|
| 1980–1997 | 5 – Sweden 4 – Denmark 2 – UK, Germany 1 – USA, Japan, Norway |
14 – Europe 1 – USA, Asia |
5 – Br J Urol (BJU Int) 3 – J Urol 1 – Eur Urol, Int J Urol |
| 1998–2007 | 7 – Japan 5 – USA 4 – Sweden 1 – Germany, Denmark, Netherlands, Canada, Austria, Turkey, Greece, Belgium |
11 – Europe 7 – Asia 6 – USA |
5 – BJU Int 3 – Urology, J Urol 2 – Int J Urol, Eur Urol, Cancer |
| 2008-–2017 | 14 – USA 5 – Italy 4 – Germany 3 – UK, Japan, China 2 – Egypt 1 – Norway, Greece, Bosnia, South Korea, Canada, Iran, Poland, Spain, France, India, Israel |
18 – Europe 15 – USA 8 – Asia 2 – Africa 1 – Middle East |
7 – Urology 6 – BJU Int 3 – Eur Urol, Eur J Surg Oncol 2 – World J Urol, Urol Oncol |
Discussion
Over the last decade, there have been more QoL studies and more validated and prospective studies. Similarly, the proportionate numbers of NBs has also increased over the last two decades, with newer studies now reporting on laparoscopic and robot-assisted UDs (Tables 1 and 2). There has also been a rise in the number of studies reporting on QoL outcomes in these patients, demonstrating the importance placed on QoL in the last decade.
Change in QoL trends over the last four decades
Whilst publication trends show that better reporting of QoL with more validated questionnaires are now being used, it seems that as long as the patient is well counselled and supported in their decision they learn to cope and adjust with their UD type [1].
Compared to previous decades, the past decade has seen an upsurge in focus on QoL outcomes in bladder cancer. This has occurred in tandem with the development of new and specific HRQoL instruments used in bladder cancer [1,8]. There has also been considerable variability in the use of QoL assessment tools, with a progressive uptake of validated assessment methods in the last decade. Our literature review revealed 13 of the 15 studies between 1987 and 1997 used a non-validated ad hoc (self-designed) instrument to assess QoL outcomes compared to only four in the 2009–2017 period. This suggests that the process of HRQoL measurement is becoming increasingly popular and perhaps clinically responsive.
The ad hoc instruments previously used were potentially poor measures of reliability and qualitative outcomes, and subject to bias due to their inherent non-validated nature [1,8]. In addition, there has been a gradual rise in the globalisation of quality assessment in patients after RC, given that 18 different countries are represented across the studies in 2009–2017 compared to only six in 1987–1997. Only one study across the last three decades accounted for sociocultural influences in health perception and QoL evaluation [11]. Perhaps there is a role for cross-cultural testing of these QoL instruments to ensure the validity and reliability of these tools across patients from other countries and cultures [12].
Generic vs cancer-specific QoL assessment
In the past more generic QoL assessment tools were used. Previously, the Beck Depression Inventory (BDI) and Sickness Impact Profile (SIP) [13] were used to assess HRQoL across a wide range of medical conditions, and therefore these were not responsive to finer, qualitative, postoperative changes pertinent to bladder cancer and UD. Similarly, the 36-item short-form health survey (SF-36) [14], which was commonly used in this time period did not incorporate postoperative concerns specific to bladder surgery, including issues such as erectile dysfunction or urinary incontinence. Indeed, even cancer-specific scales [European Organisation for the Research and Treatment of Cancer Quality of Life 30-item core questionnaire (EORTC QLQ-30C) [15] and Functional Assessment of Cancer Therapy-General (FACT-G) [16]] failed to address specific domains of importance to patients with bladder cancer.
The importance of developing instruments that measure specific outcomes for patients with bladder cancer is slowly being addressed as demonstrated by the fact that 23 studies from 2009 onwards used a bladder-specific QoL tool. Tools such as the FACT-Bladder Cancer (FACT-BL), Bladder Cancer Index (BCI) [17], Body Image Scale (BIS), FACT-Vanderbilt Cystectomy Index (FACT-VCI) [18], suggest a greater appreciation for having a responsive tool that can identify specific concerns in post-RC patients and hopefully act as a framework to compare outcomes and validate more specific tools.
Despite several retrospective studies reporting no clear superiority for NB surgery [17,20–23], recent data suggest that NB is increasingly being offered to patients. Although the type of UD should be individualised, the surgeon or centre should be able to offer both types of UDs for surgical equipoise, based on patient preference.
Table 1 suggests a progressive increase in the number of prospective studies being performed in the last decade, along with a rise in the reported numbers of NB UDs. We can perhaps postulate that the shift towards NBs has predominantly been driven by improved surgical training in a more complex procedure and better patient counselling, offering a choice of UD rather than the QoL outcomes [24].
Role of laparoscopic and robot-assisted surgery in post-RC QoL
The advent of minimally invasive surgery, such as robot-assisted RC (RARC) and laparoscopic surgery, has led to decreased length of stay and morbidity, and faster recovery. Multicentre data from the USA has suggested a significant rise in its use from 0.6% in 2004 to 12.8% in 2010 [2,3,25]. Poch et al. [26] assessed QoL before and after RARC and reported no significant QoL advantage for RARC. However, the authors found quicker return of urinary function and better body image postoperatively with intracorporeal vs extracorporeal UDs. Studies have failed to show a QoL benefit of RARC compared to open RC [2,27]. A recent meta-analysis also suggests postoperative HRQoL to be similar in patients undergoing RARC and open RC [28]. With the advent of enhanced recovery after surgery (ERAS) protocols, there is now a reduction in postoperative morbidity and hospital stay, with a recent study reporting higher emotional well-being in patients who underwent ERAS [29].
Strengths and limitations of the review
Despite the current trend of QoL studies moving in the right direction with the increased use of validated and specific HRQoL measures; the fact remains that there are still significant challenges in measuring QoL in UD patients. Sexual dysfunction although common is perhaps poorly captured. Conversely, although disease-specific questionnaires are more responsive than generic questionnaires to subtle changes within disease-specific domains, the high disease-specific sensitivity of these questionnaires may limit the ability to account for unexpected events. For example, an unanticipated neurological adverse event may not be addressed in the disease-specific instrument’s questions and as a result this may not be reflected in an accurate QoL change. Of the newer QoL tools, the Bladder Utility Symptom Scale (BUSS) seems to be a novel patient-reported outcome instrument and measures HRQoL for all patients with bladder cancer regardless of treatment received or stage of the disease [30].
Various studies have been published investigating QoL after RC and UD. However, there is an extensive deal of heterogeneity amongst these studies with regards to methodology, the use of non-validated QoL instruments, and the underpowered and retrospective nature of the majority of data make interpretation difficult. Based on the present studies, QoL has not shown to be significantly variable across the different types of UD. As the majority of them are retrospective in nature, there also remains the risk of inherent selection bias. Furthermore, QoL is only measured postoperatively in most of these studies, and in the absence of preoperative QoL data, it is not truly possible to determine the effect of UD. With different approaches to UD and in the absence of any randomised trials, results from the ongoing prospective, multicentre, randomised trial of open vs robotic radical cystectomy (RAZOR) trial may provide an answer in the near future [31].
Conclusion
The last four decades has seen gradual but significant improvements in the way QoL assessment is conducted in RC patients, with the implementation of several validated, bladder cancer-specific questionnaires and UD-specific constructs. The emergence of more prospective studies with validated QoL instruments has improved our ability to identify their QoL and to understand the differences between various UD types.
Appendix 1. Reference list for the 85 included studies
[1] Jones MA, Breckman B, Hendry WF. Life with an ileal conduit: results of questionnaire surveys of patients and urological surgeons. Br J Urol 1980; 52: 21–5.
[2] Fosså SD, Reitan JB, Ous S, Kaalhus O. Life with an ileal conduit in cystectomized bladder cancer patients: expectations and experience. Scand J Urol Nephrol 1987; 21: 97–101.
[3] Boyd SD, Feinberg SM, Skinner DG, Lieskovsky G, Baron D, Richardson J. Quality of life survey of urinary diversion patients: comparison of ileal conduits versus continent Kock ileal reservoirs. J Urol 1987; 138: 1386–9. h
[4] Månsson A, Johnson G, Månsson W. Quality of life after cystectomy. Comparison between patients with conduit and those with continent caecal reservoir urinary diversion. Br J Urol 1988; 62: 240–5.
[5] Mommsen S, Jakobsen A, Sell A. Quality of life in patients with advanced bladder cancer. A randomized study comparing cystectomy and irradiation – the Danish Bladder Cancer Study Group (DAVECA protocol 8201). Scand J Urol Nephrol 1989; 125 (Suppl.): 115–20.
[6] Chadwick DJ, Stower MJ. Life with urostomy. Br J Urol 1990; 65: 189–91.
[7] Månsson A, Johnson G, Månsson W. Psychosocial adjustment to cystectomy for bladder carcinoma and effects on interpersonal relationships. Scand J Caring Sci 1991; 5: 129–34.
[8] Nordström GM, Nyman CR. Male and female sexual function and activity following ileal conduit urinary diversion. Br J Urol 1992; 70: 33–9.
[9] Nordström G, Nyman CR, Theorell T. Psychosocial adjustment and general state of health in patients with ileal conduit urinary diversion. Scand J Urol Nephrol 1992; 26: 139–47.
[10] Bjerre BD, Johansen C, Steven K. Health-related quality of life after urinary diversion: continent diversion with the Kock pouch compared with ileal conduit. A questionnaire study. Scand J Urol Nephrol 1994; 157 (Suppl.): 113–8.
[11] Bjerre BD, Johansen C, Steven K. Health-related quality of life after cystectomy: bladder substitution compared with ileal conduit diversion. A questionnaire survey. Br J Urol 1995; 75: 200–5.
[12] Gerharz EW, Weingartner K, Dopatka T, Kohl UN, Basler HD, Riedmiller HN. Quality of life after cystectomy and urinary diversion: results of a retrospective interdisciplinary study. J Urol 1997; 158: 778–85.
[13] Okada Y, Oishi K, Shichiri Y, Kakehi Y, Hamaguchi A, Tomoyoshi T et al. Quality of life survey of urinary diversion patients: comparison of continent urinary diversion versus ileal conduit. Int J Urol 1997; 4: 26–31.
[14] Filipas D, Egle UT, Büdenbender C, Fisch M, Fichtner J, Hoffmann SO et al. Quality of life and health in patients with urinary diversion: a comparison of incontinent versus continent urinary diversion. Eur Urol 1997; 32: 23–9.
[15] Bjerre BD, Johansen C, Steven K. A questionnaire study of sexological problems following urinary diversion in the female patient. Scand J Urol Nephrol 1997; 31: 155–60.
[16] Månsson A, Colleen S, Hermerén G, Johnson G. Which patients will benefit from psychosocial intervention after cystectomy for bladder cancer? Br J Urol 1997; 80: 50–7.
[17] Bjerre BD, Johansen C, Steven K. Sexological problems after cystectomy: bladder substitution compared with ileal conduit diversion. A questionnaire study of male patients. Scand J Urol Nephrol 1998; 32: 187–93.
[18] Weijerman PC, Schurmans JR, Hop WC, Schröder FH, Bosch JL. Morbidity and quality of life in patients with orthotopic and heterotopic continent urinary diversion. Urology 1998; 51: 51–56.
[19] Sullivan LD, Chow VD, Ko DS, Wright JE, McLoughlin MG. An evaluation of quality of life in patients with continent urinary diversions after cystectomy. Br J Urol 1998; 81: 699–704.
[20] Månsson A, Christensson P, Johnson G, Colleen S. Can preoperative psychological defensive strategies, mood and type of lower urinary tract reconstruction predict psychosocial adjustment after cystectomy in patients with bladder cancer? Br J Urol 1998; 82: 348–56.
[21] Hart S, Skinner EC, Meyerowitz BE, Boyd S, Lieskovsky G, Skinner DG. Quality of life after radical cystectomy for bladder cancer in patients with an ileal conduit, cutaneous or urethral kock pouch. J Urol 1999; 162: 77–81.
[22] Kitamura H, Miyao N, Yanase M, Masumori N, Matsukawa M, Takahashi A et al. Quality of life in patients having an ileal conduit, continent reservoir or orthotopic neobladder after cystectomy for bladder carcinoma. Int J Urol 1999; 6: 393–9.
[23] Hardt J, Filipas D, Hohenfellner R, Egle UT. Quality of life in patients with bladder carcinoma after cystectomy: first results of a prospective study. Qual Life Res 2000; 9: 1–12.
[24] McGuire MS, Grimaldi G, Grotas J, Russo P. The type of urinary diversion after radical cystectomy significantly impacts on the patient’s quality of life. Ann Surg Oncol 2000; 7: 4–8.
[25] Fujisawa M, Isotani S, Gotoh A, Okada H, Arakawa S, Kamidono S. Health-related quality of life with orthotopic neobladder versus ileal conduit according to the SF-36 survey. Urology 2000; 55: 862–5.
[26] Hobisch A, Tosun K, Kinzl J, Kemmler G, Bartsch G, Höltl L et al. Quality of life after cystectomy and orthotopic neobladder versus ileal conduit urinary diversion. World J Urol 2000; 18: 338–44.
[27] Kulaksizoglu H, Toktas G, Kulaksizoglu IB, Aglamis E, Unlüer E. When should quality of life be measured after radical cystectomy? Eur Urol 2002; 42: 350–5.
[28] Månsson Å, Davidsson T, Hunt S, Månsson W, The quality of life in men after radical cystectomy with a continent cutaneous diversion or orthotopic bladder substitution: is there a difference? BJU Int 2002; 90: 386–90.
[29] Hara I, Miyake H, Hara S, Gotoh A, Nakamura I, Okada H et al. Health-related quality of life after radical cystectomy for bladder cancer: a comparison of ileal conduit and orthotopic bladder replacement. BJU Int 2002; 89: 10–3.
[30] Dutta SC, Chang SC, Coffey CS, Smith JA, Jack G, Cookson MS. Health related quality of life assessment after radical cystectomy: comparison of ileal conduit with continent orthotopic neobladder. J Urol 2002; 168: 164–7.
[31] Henningsohn L, Wijkström H, Steven K, Pedersen J, Ahlstrand C, Aus G et al. Relative importance of sources of symptom-induced distress in urinary bladder cancer survivors. Eur Urol 2003; 43: 651–62.
[32] Protogerou V, Moschou M, Antoniou N, Varkarakis J, Bamias A, Deliveliotis C. Modified S-pouch neobladder vs ileal conduit and a matched control population: a quality-of-life survey. BJU Int 2004; 94: 350–4.
[33] Joniau S, Benijts J, Van Kampen M, De Waele M, Ooms J, Van Cleynenbreugel B et al. Clinical experience with the n-shaped ileal neobladder: assessment of complications, voiding patterns, and quality of life in our series of 58 patients. Eur Urol 2005; 47: 666–73.
[34] Yoneda T, Adachi H, Urakami S, Kishi H, Shigeno K, Shiina H et al. Health related quality of life after orthotopic neobladder construction and its comparison with normative values in the Japanese population. J Urol 2005; 174: 1944–7.
[35] Allareddy V, Kennedy J, West MM, Konety BR. Quality of life in long-term survivors of bladder cancer. Cancer 2006; 106: 2355–62.
[36] Kikuchi E, Horiguchi Y, Nakashima J, Ohigashi T, Oya M, Nakagawa K et al. Assessment of long-term quality of life using the fact-bl questionnaire in patients with an ileal conduit, continent reservoir, or orthotopic neobladder. Jpn J Clin Oncol 2006; 36: 712–6.
[37] Harano M, Eto M, Nakamura M, Hasegawa Y, Kano M, Yamaguchi A et al. A pilot study of the assessment of the quality of life, functional results, and complications in patients with an ileal neobladder for invasive bladder cancer. Int J Urol 2007; 14: 112–7.
[38] Gilbert SM, Wood DP, Dunn RL, Weizer AZ, Lee CT, Montie JE et al. Measuring health-related quality of life outcomes in bladder cancer patients using the Bladder Cancer Index (BCI). Cancer 2007; 109: 1756–62.
[39] Saika T, Arata R, Tsushima T, Nasu Y, Suyama B, Takeda K et al. Health-related quality of life after radical cystectomy for bladder cancer in elderly patients with an ileal conduit, ureterocutaneostomy, or orthotopic urinary reservoir: a comparative questionnaire survey. Acta Med Okayama 2007; 61: 199–203.
[40] Månsson Å, Al Amin M, Malmström PU, Wijkström H, Abol Enein H, Månsson W. Patient-assessed outcomes in Swedish and Egyptian men undergoing radical cystectomy and orthotopic bladder substitution – a prospective comparative study. Urology 2007; 70: 1086–90.
[41] Autorino R, Quarto G, Di Lorenzo G, De Sio M, Perdonà S, Giannarini G et al. Health related quality of life after radical cystectomy: comparison of ileal conduit to continent orthotopic neobladder. Eur J Surg Oncol 2009; 35: 858–64.
[42] Sogni F, Brausi M, Frea B, Martinengo C, Faggiano F, Tizzani A et al. Morbidity and quality of life in elderly patients receiving ileal conduit or orthotopic neobladder after radical cystectomy for invasive bladder cancer. Urology 2008; 71: 919–23.
[43] Yuh B, Butt Z, Fazili A, Piacente P, Tan W, Wilding G et al. Short-term quality-of-life assessed after robot-assisted radical cystectomy: a prospective analysis. BJU Int 2009: 103: 800–4.
[44] Frich PS, Kvestad CA, Angelsen A. Outcome and quality of life in patients operated on with radical cystectomy and three different urinary diversion techniques. Scand J Urol Nephrol 2009; 43: 37–41.
[45] Philip J, Manikandan R, Venugopal S, Desouza J, Javlé PM. Orthotopic neobladder versus ileal conduit urinary diversion after cystectomy – a quality-of-life based comparison. Ann R Coll Surg Engl 2009; 91: 565–9.
[46] Somani BK, Gimlin D, Fayers P, N’Dow J. Quality of life and body image for bladder cancer patients undergoing radical cystectomy and urinary diversion – a prospective cohort study with a systematic review of literature. Urology 2009; 74: 1138–43.
[47] Miyake H, Furukawa J, Muramaki M, Takenaka A, Fujisawa M. Orthotopic sigmoid neobladder after radical cystectomy: assessment of complications, functional outcomes and quality of life in 82 Japanese patients. BJU Int 2010; 106: 412–6.
[48] Large MC, Katz MH, Shikanov S, Eggener SE, Steinberg GD. Orthotopic neobladder versus Indiana pouch in women: a comparison of health related quality of life outcomes. J Urol 2010; 183: 201–6.
[49] Hedgepeth RC, Gilbert SM, He C, Lee CT, Wood DP. Body image and bladder cancer specific quality of life in patients with ileal conduit and neobladder urinary diversions. Urology 2010; 76: 671–5.
[50] Vakalopoulos I, Dimitriadis G, Anastasiadis A, Gkotsos G, Radopoulos D. Does intubated uretero-ureterocutaneostomy provide better health-related quality of life than orthotopic neobladder in patients after radical cystectomy for invasive bladder cancer? Int Urol Nephrol 2011; 43: 743–8.
[51] Erber B, Schrader M, Miller K, Schostak M, Baumunk D, Lingnau A et al. Morbidity and quality of life in bladder cancer patients following cystectomy and urinary diversion: a single-institution comparison of ileal conduit versus orthotopic neobladder. ISRN Urol 2012: 2012: 342,796. DOI:10.5402/2012/342,796.
[52] Anderson CB, Feurer ID, Large MC, Steinberg GD, Barocas DA, Cookson MS et al. Psychometric characteristics of a condition-specific, health-related quality-of-life survey: the FACT-Vanderbilt Cystectomy Index. Urology 2012; 80: 77–83.
[53] Miyake H, Furukawa J, Muramaki M, Inoue T, Fujisawa M. Health related quality of life after radical cystectomy: Comparative study between orthotopic sigmoid versus ileal neobladders. Eur J Surg Oncol 2012; 38: 1089–94.
[54] Stegemann A, Rehman S, Brewer K, Kesavadas T, Hussain A, Chandrasekhar R et al. Short-term patient-reported quality of life after robot-assisted radical cystectomy using the convalescence and recovery evaluation. Urology 2012; 79: 1274–80.
[55] Mucciardi G, Macchione L, Galì A, di Benedetto A, Subba E, Pappalardo R et al. [Quality of life and overall survival in high risk patients after radical cystectomy with a simple urinary derivation]. Cir Esp 2015; 93: 368–74.
[56] Prcic A, Aganovic D, Hadziosmanovic O. Sickness Impact Profile (SIP) score, a good alternative instrument for measuring quality of life in patients with ileal urinary diversions. Acta Inform Med 2013; 21: 160–5.
[57] Shim B, Kim KH, Yoon H, Park YY, Lee DH. Body image following radical cystectomy and ileal neobladder or conduit in korean patients. Korean J Urol 2014; 55: 161–6.
[58] Yang M, Wang H, Wang J, Ruan M. Impact of invasive bladder cancer and orthotopic urinary diversion on general health-related quality of life: An SF-36 survey. Mol Clin Oncol 2013; 1: 758–62.
[59] Metcalfe M, Estey E, Jacobsen NE, Voaklander D, Fairey AS. Association between urinary diversion and quality of life after radical cystectomy. Can J Urol 2013; 20: 6626–31.
[60] Asgari MA, Safarinejad MR, Shakhssalim N, Soleimani M, Shahabi A, Amini E. Quality of life after radical cystectomy for bladder cancer in men with an ileal conduit or continent urinary diversion: A comparative study. Urol Ann 2013; 5: 190–6.
[61] Aboumarzouk OM, Drewa T, Olejniczak P, Chlosta PL. Laparoscopic radical cystectomy: neobladder or ileal conduit, debate still goes on. Cent Eur J Urol 2014; 67: 9–15.
[62] Gacci M, Saleh O, Cai T, Gore JL, D’Elia C, Minervini A et al. Quality of life in women undergoing urinary diversion for bladder cancer: results of a multicenter study among long-term disease-free survivors. Health Qual Life Outcomes 2013; 11: 43. DOI:10.1186/1477–7525-11–43.
[63] Parekh DJ, Messer J, Fitzgerald J, Ercole B, Svatek R. Perioperative outcomes and oncologic efficacy from a pilot prospective randomized clinical trial of open versus robotic assisted radical cystectomy. J Urol 2013; 189: 474–9.
[64] Fuentes J, Ramos E, Truan D, Portillo JA, Campos-Juanatey F, Gala L et al. Review of a series of cystectomies in women for bladder cancer: complications and quality of life. Arch Esp Urol 2014; 67: 303–12.
[65] Miyake H, Furukawa J, Sakai I, Muramaki M, Yamashita M, Inoue TA et al. Orthotopic sigmoid vs. ileal neobladders in Japanese patients: a comparative assessment of complications, functional outcomes, and quality of life. Urol Oncol 2013; 31: 1155–60.
[66] Rouanne M, Legrand G, Neuzillet Y, Ghoneim T, Cour F, Letang N et al. Long-term women-reported quality of life after radical cystectomy and orthotopic ileal neobladder reconstruction. Ann Surg Oncol 2014; 21: 1398–404.
[67] Singh V, Yadav R, Sinha RJ, Gupta DK. Prospective comparison of quality-of-life outcomes between ileal conduit urinary diversion and orthotopic neobladder reconstruction after radical cystectomy: a statistical model. BJU Int 2014; 113: 726–32.
[68] Large MC, Malik R, Cohn JA, Richards KA, Ganshert C, Kunnavakkum R et al. Prospective health-related quality of life analysis for patients undergoing radical cystectomy and urinary diversion. Urology 2014; 84: 808–14.
[69] Aboumohamed AA, Raza SJ, Al-Daghmin A, Tallman C, Creighton T, Crossley H et al. Health-related quality of life outcomes after robot-assisted and open radical cystectomy using a validated bladder-specific instrument: a multi-institutional study. Urology 2014; 83: 1300–8.
[70] Poch MA, Stegemann AP, Rehman S, Sharif MA, Hussain A, Consiglio JD et al. Short-term patient reported health-related quality of life (HRQL) outcomes after robot-assisted radical cystectomy (RARC). BJU Int 2014; 113: 260–5.
[71] Zahran MH, El-Hefnawy AS, Zidan EM, El-Bilsha MA, Taha DE, Ali-El-Dein B. Health-related quality of life after radical cystectomy and neobladder reconstruction in women: Impact of voiding and continence status. Int J Urol 2014; 21: 887–92.
[72] Mischinger J, Abdelhafez MF, Todenhöfer T, Schwentner C, Aufderklamm S, Stenzl A et al. Quality of life outcomes after radical cystectomy: long-term standardized assessment of Studer Pouch versus I-Pouch. World J Urol 2015; 33: 1381–7.
[73] Messer JC, Punnen S, Fitzgerald J, Svatek R, Parekh DJ. Health-related quality of life from a prospective randomised clinical trial of robot-assisted laparoscopic vs open radical cystectomy. BJU Int 2014; 114: 896–902.
[74] Huang Y, Pan X, Zhou Q, Huang H, Li L, Cui X et al. Quality-of-life outcomes and unmet needs between ileal conduit and orthotopic ileal neobladder after radical cystectomy in a Chinese population: a 2-to-1 matched-pair analysis. BMC Urol 2015; 15: 117. DOI:10.1186/s12894-015–0113-7.
[75] Goldberg H, Baniel J, Mano R, Rotlevy G, Kedar D, Yossepowitch O. Orthotopic neobladder vs. ileal conduit urinary diversion: A long-term quality-of-life comparison. Urol Oncol 2016; 34: 121.e1-121.e7. DOI:10.1016/j.urolonc.2015.10.006.
[76] Bochner BH, Dalbagni G, Sjoberg DD, Silberstein J, Keren Paz GE, Donat SM et al. Comparing open radical cystectomy and robot-assisted laparoscopic radical cystectomy: A randomized clinical trial. Eur Urol 2015; 67: 1042–50.
[77] Satkunasivam R, Santomauro M, Chopra S, Plotner E, Cai J, Miranda G et al. Robotic intracorporeal orthotopic neobladder: urodynamic outcomes, urinary function, and health-related quality of life. Eur Urol 2016; 69: 247–53.
[78] Longo N, Imbimbo C, Fusco F, Ficarra V, Mangiapia F, Di Lorenzo G et al. Complications and quality of life in elderly patients with several comorbidities undergoing cutaneous ureterostomy with single stoma or ileal conduit after radical cystectomy. BJU Int 2016; 118: 521–6.
[79] Liu Z, Tian Q, Xia S, Yin H, Yao D, Xiu Y. Evaluation of the improved tubeless cutaneous ureterostomy technique following radical cystectomy in cases of invasive bladder cancer complicated by peritoneal metastasis. Oncol Lett 2016; 11: 1401–5.
[80] Khan MS, Gan C, Ahmed K, Ismail AF, Watkins J, Summers JA et al. A single-centre early phase randomised controlled three-arm trial of open, robotic, and laparoscopic radical cystectomy (CORAL). Eur Urol 2016; 69: 613–21.
[81] Winters BR, Wright JL, Holt SK, Dare A, Gore JL, Schade GR. Health related quality of life following radical cystectomy: compariative analysis from medicare health outcomes survey. J Urol 2018; 199: 669–75.
[82] Zahran MH, Taha DE, Harraz AM, Zidan EM, El-Bilsha MA, Tharwat M et al. Health related quality of life after radical cystectomy in women: Orthotopic neobladder versus ileal loop conduit and impact of incontinence. Minerva Urol Nefrol 2017; 69: 262–70.
[83] Gellhaus PT, Cary C, Kaimakliotis HZ, Johnson CS, Weiner M, Koch MO et al. Long-term health-related quality of life outcomes following radical cystectomy. Urology 2017; 106: 82–6.
[84] Mischinger J, Abdelhafez MF, Rausch S, Todenhöfer T, Neumann E, Aufderklamm S et al. Perioperative morbidity, bowel function and oncologic outcome after radical cystectomy and ileal orthotopic neobladder reconstruction: Studer-pouch versus I-pouch. Eur J Surg Oncol 2018; 44: 178–84.
[85] Kretschmer A, Grimm T, Buchner A, Grabbert M, Jokisch F, Schneevoigt BS et al. Prospective evaluation of health-related quality of life after radical cystectomy: focus on peri- and postoperative complications. World J Urol 2017; 35: 1223–31.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- [1].Somani BK, MacLennan SJ, N’Dow J.. Quality of life with urinary diversion. Eur Urol Suppl. 2010;9:763–771. [Google Scholar]
- [2].Messer JC, Punnen S, Fitzgerald J, et al. Health-related quality of life from a prospective randomised clinical trial of robot-assisted laparoscopic vs open radical cystectomy. BJU Int. 2014;114:896–902. [DOI] [PubMed] [Google Scholar]
- [3].Novara G, Catto JW, Wison T, et al. Systematic review and cumulative analysis of perioperative outcomes and complications after robot-assisted radical cystectomy. Eur Urol. 2015;67:376–401. [DOI] [PubMed] [Google Scholar]
- [4].Stein JP, Esrig D, Freeman JA, et al. Prospective pathologic analysis of female cystectomy specimens: risk factors for orthotopic diversion in women. Urology. 1998;51:951–955. [DOI] [PubMed] [Google Scholar]
- [5].Stein JP. Commentary. urinary diversion and bladder substitution in patients with bladder cancer. Urol Oncol. 2000;5:232–233. [DOI] [PubMed] [Google Scholar]
- [6].Clark PE, Stein JP, Groshen SG, et al. Radical cystectomy in the elderly. Cancer. 2005;104:36–43. [DOI] [PubMed] [Google Scholar]
- [7].Allareddy V, Kennedy J, West MM, et al. Quality of life in long-term survivors of bladder cancer. Cancer. 2006;106:2355–2362. [DOI] [PubMed] [Google Scholar]
- [8].Somani BK, Nabi G, Wong S, et al. How close are we to knowing whether orthotopic bladder replacement surgery is the new gold standard? Evidence from a systematic review update. Urology. 2009;74:1331–1339. [DOI] [PubMed] [Google Scholar]
- [9].Dutta SC, Chang SC, Coffey CS, et al. Health related quality of life assessment after radical cystectomy: comparison of ileal conduit with continent orthotopic neobladder. J Urol. 2002;168:164–167. [PubMed] [Google Scholar]
- [10].Hautmann RE, Abol-Enein H, Hafez K, et al. Urinary diversion. Urology. 2007;69(Suppl):17–49. [DOI] [PubMed] [Google Scholar]
- [11].Månsson Å, Al-Amin M, Malmstrom M, et al. Patient-assessed outcomes in Swedish and Egyptian men undergoing radical cystectomy and orthotopic bladder substitution – a prospective comparative study. Urology. 2007;70:1086–1090. [DOI] [PubMed] [Google Scholar]
- [12].Aaronson N, Alonso J, Burnam A, et al. Assessing health status and quality-of-life instruments: attributes and review criteria. Qual Life Res. 2002;11:193–205. [DOI] [PubMed] [Google Scholar]
- [13].Bergner M, Bobbitt RA, Carter WB, et al. The sickness impact profile: development and final revision of a health status measure. Med Care. 1981;19:787–805. [DOI] [PubMed] [Google Scholar]
- [14].Ware JE, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–483. [PubMed] [Google Scholar]
- [15].Aaronson NK, Ahmedzai S, Bergman B, et al. The European organization for research and treatment of cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst. 1993;85:365–376. [DOI] [PubMed] [Google Scholar]
- [16].Cella DF, Tulsky DS, Gray G, et al. The functional assessment of cancer therapy scale: development and validation of the general measure. J Clin Oncol. 1993;11:570–579. [DOI] [PubMed] [Google Scholar]
- [17].Gilbert SM, Wood DP, Dunn RL, et al. Measuring health-related quality of life outcomes in bladder cancer patients using the Bladder Cancer Index (BCI). Cancer. 2007;109:1756–1762. [DOI] [PubMed] [Google Scholar]
- [18].Cookson MS, Dutta SC, Chang SS, et al. Health related quality of life in patients treated with radical cystectomy and urinary diversion for urothelial carcinoma of the bladder: development and validation of a new disease specific questionnaire. J Urol. 2003;170:1926–1930. [DOI] [PubMed] [Google Scholar]
- [19].Pietropaolo A, Proietti S, Geraghty R, et al. Trends of ‘urolithiasis: interventions, simulation and laser technology‘ over the last 16 years (2000-2015) as published in the literature (PubMed): a systematic review from European section of Uro-technology (ESUT). World J Urol. 2017;35:1651–1658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Wright JL, Porter MP. Quality-of-life assessment in patients with bladder cancer. Nat Clin Pract Urol. 2007;4:147–154. [DOI] [PubMed] [Google Scholar]
- [21].Månsson Å, Davidsson T, Hunt S, et al. The quality of life in men after radical cystectomy with a continent cutaneous diversion or orthotopic bladder substitution: is there a difference? BJU Int. 2002;90:386–390. [DOI] [PubMed] [Google Scholar]
- [22].Yoneda T, Adachi H, Urakami S, et al. Health related quality of life after orthotopic neobladder construction and its comparison with normative values in the Japanese population. J Urol. 2005;174:1944–1947. [DOI] [PubMed] [Google Scholar]
- [23].Singh V, Yadav R, Sinha RJ, et al. Prospective comparison of quality-of-life outcomes between ileal conduit urinary diversion and orthotopic neobladder reconstruction after radical cystectomy: a statistical model. BJUI Int. 2014;113:726–732. [DOI] [PubMed] [Google Scholar]
- [24].Frich PS, Kvestad C, Angelsen A. Outcome and quality of life in patients operated on with radical cystectomy and three different urinary diversion techniques. Scand J Urol Nephrol. 2009;43:37–41. [DOI] [PubMed] [Google Scholar]
- [25].Yuh B, Wilson T, Bochner B, et al. Systematic review and cumulative analysis of oncologic and functional outcomes after robot-assisted radical cystectomy. Eur Urol. 2015;67:402–422. [DOI] [PubMed] [Google Scholar]
- [26].Poch MA, Stegemann AP, Rehman S, et al. Short-term patient reported health-related quality of life (HRQL) outcomes after robot-assisted radical cystectomy (RARC). BJU Int. 2014;113:260–265. [DOI] [PubMed] [Google Scholar]
- [27].Bochner BH, Dslbagni G, Sjoberg DD, et al. Comparing open radical cystectomy and robot-assisted laparoscopic radical cystectomy: A randomized clinical trial. Eur Urol. 2015;67:1042–1050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Lauridsen SV, Tønnesen H, Jensen BT, et al. Complications and health-related quality of life after robot-assisted versus open radical cystectomy: a systematic review and meta-analysis of four RCTs. Syst Rev. 2017;6:150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Karl A, Buchner A, Becker A, et al. A new concept for early recovery after surgery for patients undergoing radical cystectomy for bladder cancer: results of a prospective randomized study. J Urol. 2014;191:335–340. [DOI] [PubMed] [Google Scholar]
- [30].Perlis N, Krahn MD, Boehme KE, et al. The bladder utility symptom scale: a novel patient reported outcome instrument for bladder cancer. J Urol. 2018;200:283–291. [DOI] [PubMed] [Google Scholar]
- [31].Smith ND, Castle EP, Gonzalgo ML, et al. The RAZOR (randomized open vs robotic cystectomy) trial: study design and trial update. BJU Int. 2015;115:198–205. [DOI] [PMC free article] [PubMed] [Google Scholar]


