Abstract
Introduction:
The Medicare Part D medication therapy management (MTM) program positions pharmacists to optimize beneficiaries’ medications and improve care. Little is known regarding Part D MTM delivery by community pharmacists and other pharmacist provider types.
Objectives:
To (1) characterize Medicare Part D MTM delivery by community pharmacists, (2) compare MTM delivery by community pharmacists to other pharmacists, and (3) generate hypotheses for future research.
Methods:
A descriptive cross-sectional study using merged data from a 20% random sample of Medicare beneficiary enrollment data with a 100% sample of recently available 2014 Part D MTM files was conducted. Andersen’s Behavioral Model was applied to describe MTM delivery across beneficiary characteristics. Descriptive and bivariate statistics were used to compare delivery of MTM between community and other pharmacist providers.
Results:
Among beneficiaries sampled, community pharmacists provided comprehensive medication reviews (CMRs) to 22% (n=26,337) of beneficiaries receiving at least one CMR. Almost half (49.4%) were provided face-to-face. Across pharmacist cohorts, median days to CMR offer of post-MTM program enrollment were within the 60-day policy requirement. The community pharmacist cohort had fewer days from CMR offer to receipt (median 47 days). Community pharmacists provided more medication therapy problem (MTP) recommendations (mean [SD] of 1.8 [3.5]; p<0.001), but resolved less MTPs (0.2 [0.7]; p<0.001), and most commonly served beneficiaries that were in the south but less in the west/northeast. Additionally, community pharmacists served a smaller proportion of black beneficiaries, yet a larger proportion of Hispanic beneficiaries (p<0.001).
Conclusion:
Community pharmacists provided approximately one in five CMRs for MTM eligible beneficiaries in 2014, with CMRs occurring more quickly, resulting in more MTP recommendations, but resolving less MTPs than those provided by non-community pharmacists. Future research should explore geographic/racial-ethnic disparities in beneficiaries served and strategies to increase negligible MTP resolution by community pharmacists.
Keywords: Community Pharmacists, Medication Therapy Management, Medicare Part D
Preventable medication therapy problems (MTPs) are a major public health concern in the United States, affecting over seven million patients and costing nearly $21 billion annually across inpatient and outpatient health care settings.1 Community pharmacists can serve as a resource to improve medication use. Pharmacists may provide medication management services, including “services that focus on medication appropriateness, effectiveness, safety, and adherence with the goal of improving health outcomes” as defined by the Joint Commission of Pharmacy Practitioners.2 Medication therapy management (MTM) is an example of a medication management service.2,3
The complex medication needs of Medicare beneficiaries may be met by MTM, and is required as one component of Medicare Part D. In Part D MTM, eligible beneficiaries must be offered an annual comprehensive medication review (CMR) and quarterly targeted medication reviews (TMRs), with follow-up provided on any medication therapy problem (MTP) recommendations.4 Several models for MTM delivery have been reported, including contracts with MTM vendors who provide services either “in-house” or through contracts with “external” providers, such as community pharmacists.5 Although “any qualified provider” may provide MTM, plans have reported most commonly using pharmacists.5 Heterogeneity among pharmacists providing MTM in the outpatient6 call-center and community pharmacy settings7 have been reported, including variations in MTM service characteristics, populations served, and MTM practice maturity level, making it difficult to measure outcomes.6,7 Therefore, it is unknown how MTM delivery models could be tailored to different population segments in order to optimize outcomes. Moreover, challenges unique to MTM delivery in the community pharmacy setting exist. For example, the need to redefine workflow to incorporate MTM has been noted as a barrier.8–10 Defining and developing new roles for support staff have been emphasized.9,11–13 Moreover, community pharmacists have struggled with patient and prescriber understanding and acceptance of MTM services.8,14–16 Additional barriers reported include high demand for dispensing-related activities, cumbersome MTM documentation, insufficient staff training, and inadequate staffing hours.8,9,17–19
Despite the barriers to providing MTM services in the community pharmacy setting, community pharmacists also have unique advantages to delivering MTM, such as established relationships with patients through prescription fulfillment services. However, little information is available regarding the extent of community pharmacist involvement in Part D MTM, the characteristics of beneficiaries served by community pharmacists as opposed to other pharmacist providers, and the variation in MTM delivery by community pharmacists compared with other pharmacist providers. This information could provide a foundation for future research comparing MTM delivery models. Therefore, the objectives of this study were to (1) characterize Medicare Part D MTM delivery by community pharmacists, (2) compare MTM delivery by community pharmacists to that of other pharmacists, and (3) generate hypotheses for future research.
Methods
Study Design
This hypothesis-generating descriptive study used a cross-sectional design to compare MTM delivery between beneficiaries receiving CMRs from one of three different pharmacist provider type cohorts: community pharmacists, MTM vendor in-house pharmacists, and Medicare Part D plan pharmacists.
Data Sources
We used a number of administrative claims data files obtained from the Centers for Medicare & Medicaid Services (CMS) through a third party contractor called ResDAC; more detailed information is available online.20 These files were used to describe beneficiary characteristics and the delivery of MTM services. We obtained a 20% random sample of the 2014 Medicare master beneficiary summary file and Parts A, B, and D health claims data, as well as a 100% sample of the 2014 Part D MTM files. These files represent a recent expansion of data resources provided by CMS and were first made available for research in 2017. Beneficiary characteristics (e.g., age, gender, race, plan enrollment, and area of residence) are contained in the master beneficiary summary file. In addition, we also used Parts A, B, and D claims data to capture inpatient, outpatient, and prescription medication utilization under the Medicare program. The Part D MTM files contain detailed information regarding enrollment in the MTM program, dates of CMR offer, dates of CMR receipt, method of CMR delivery, and the type of CMR provider. In addition, a number of summary variables describing the delivery of MTM services are also provided for each beneficiary in the MTM file including annual counts of MTP recommendations, MTPs resolved, and TMRs received.
Cohort Definitions
For this paper, we limit our description of the delivery of MTM services to Medicare beneficiaries eligible for benefits due to age qualification (Figure). Beneficiaries were eligible for inclusion in this study if they were 65 and older and they were continuously enrolled in Medicare Parts A, B, and D for all 12 months of the 2014 calendar year. To describe MTM service delivery and the types of providers, we limited the population to beneficiaries in the 20% random sample that linked to the Part D MTM files receiving at least one CMR in 2014 by a (1) community, (2) plan, or (3) vendor in-house pharmacist. The community pharmacist cohort included beneficiaries with CMRs coded as delivered by “local pharmacists” and “MTM vendor local pharmacists” as these represent community pharmacists providing MTM through contracts directly between the plan and the community pharmacy or through an MTM vendor as an intermediary. The plan pharmacist cohort included beneficiaries with CMRs coded as provided by pharmacists employed directly by plans as well as pharmacists employed by a pharmacy benefit manager (PBM). These providers were combined as both the plan and PBM’s revenue focuses on medical/prescription claims rather than MTM. The MTM vendor in-house pharmacist cohort included beneficiaries with CMRs coded as delivered by “MTM vendor in-house pharmacists” which represents pharmacists employed directly (not “external” contracts) by MTM vendors.
Figure 1. Flow Diagram of MTM eligible Medicare Beneficiaries receiving CMRs in 2014.
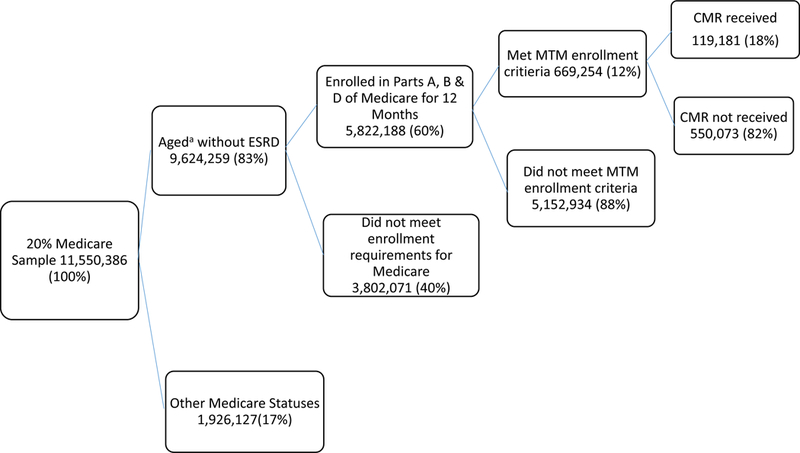
Abbreviations: MTM, Medication Therapy Management; CMR, comprehensive medication review; ESRD, end stage renal disease
aAn individual aged 65 or over, who is enrolled in the Medicare program.
Individuals aged 64 and younger and individuals eligible for Medicare through end-stage renal disease (ESRD) or other disabilities were excluded.
Variables
To describe beneficiary characteristics, we used the Andersen Behavioral Model of Health Services Use as a conceptual framework to group individual determinants of health care utilization variables into predisposing, enabling, and need characteristics.21,22 According to the model, an individual’s use of a health service (e.g., MTM) is dependent on their predisposing characteristics, ability to use the health service (enabling), and need for the service.21,22
For the purposes of this study, predisposing characteristics included age as a continuous variable, gender, and race/ethnicity. Enabling variables included geographic region of the country (Northeast, South, Midwest, West, and Other Region) and urban residence.23 Additionally, an income assistance status variable for Medicare enrollment24 (Medicare/Medicaid dual enrollment, qualified Medicare beneficiary enrollment, specified low-income Medicare beneficiary enrollment, or no income assistance) was included. Lastly, given the unique benefit design of Part D in which patient out-of-pocket copayment rates vary at different levels of prescription spend, we described MTM delivery across copayment status. Copayment status was hierarchically defined as the maximum stage of the Part D benefit achieved throughout the calendar year from (1) catastrophic coverage to (2) prescription use in the coverage gap (e.g., donut hole) to (3) no coverage gap exposure.
Finally, need variables included any inpatient hospitalization or emergency department visits within the calendar year. To evaluate the burden of health conditions and medication use, we used the Elixhauser Index and a count of therapeutic drug classes prescribed to beneficiaries during the year.25 Beneficiaries were categorized as having a condition if there was at least one inpatient and/or two outpatient codes within the calendar year for each condition. We used a simple count of the 30 Elixhauser conditions to describe disease burden as well as weighted Elixhauser indices shown to be predictive of readmission to the hospital and overall mortality.26
The MTM delivery variables evaluated included (1) beneficiary entry into MTM program, (2) beneficiary MTM services received, and (3) pharmacist provider interventions. First, entry into MTM program variables included days from plan enrollment to MTM enrollment, days from MTM enrollment to CMR offer, days from CMR offer to first CMR received, and Part D contract type (managed care, prescription drug plan [PDP], or employer sponsored). For Part D contract type, we collapsed managed care preferred provider organizations (PPOs) and regional PPOs into “managed care” as managed care programs generally have higher standards to meet for the CMS Star Ratings and thus are more incentivized to design robust MTM programs.27 Second, variables for MTM services received included CMR delivery method (face-to-face, telephone, telehealth), number of CMRs and TMRs received, and CMR recipient (beneficiary, beneficiary’s prescriber, caregiver/other authorized individual). Per 2014 CMS guidance,28 we grouped “other authorized individual” with “caregiver” for analytical purposes.
Lastly, pharmacist-prescriber intervention variables included number of MTP recommendations made and number of MTP resolutions.
Statistical Analysis
Descriptive statistics were computed using SAS v 9.4 software29 to describe MTM delivery in 2014 across the three pharmacist provider types. Bivariate statistics were used to assess differences in MTM delivery across pharmacist cohorts. We compared beneficiaries receiving a CMR from a community pharmacist to those receiving a CMR from a plan pharmacist and from a vendor in-house pharmacist in separate analyses. Chi-square tests were used to compare categorical variables and two-tailed t-tests or Wilcoxon rank-sum tests were used for continuous variables when appropriate. An alpha of 0.05 or lower was deemed significant for all statistical analyses.
This study was approved by the University of Minnesota Institutional Review Board.
Results
Among the 20% random sample of continuously enrolled Medicare beneficiaries qualified for benefits through aged enrollment criteria, 119,181 beneficiaries received a CMR in 2014 (Figure). Community pharmacists provided 22% of these CMRs, 30% were provided by plan pharmacists, and 35% were provided by vendor in-house pharmacists (Table 1). Approximately 12% of CMRs were provided by other pharmacist and health care provider types. These data are reported to provide full context but were not included in subsequent analyses.
Table 1.
CMR Provider Types Among 2014 Sample (N=119,181)
| Provider Type | n (%) |
|---|---|
| Community Pharmacists | 26,337 (22.1%) |
| Local Pharmacist | 7,734 (29.4%) |
| MTM Vendor Local Pharmacist | 18,603 (70.6%) |
| Plan Pharmacists | 35,741 (30.0%) |
| Plan Sponsor Pharmacist | 25,531 (71.4%) |
| Plan Benefit Manager Pharmacist | 10,210 (28.6%) |
| MTM Vendor In-house Pharmacist | 42,225 (35.4%) |
| MTM Vendor In-House Pharmacist | 42,225 (100.0%) |
| Other Pharmacists | 7,624 (6.4%) |
| LTC Consultant Pharmacist | 585 (7.7%) |
| Hospital Pharmacist | 0 (0.0%) |
| Pharmacist, Other | 7,039 (92.3%) |
| Other Providers | 7,254 (6.1%) |
| Physician | 412 (5.7%) |
| Registered Nurse | 1,163 (16.0%) |
| Licensed Practical Nurse | 332 (4.6%) |
| Nurse Practitioner | 4,971 (68.5%) |
| Physician’s Assistant | 0 (0.0%) |
| Other | 376 (5.2%) |
CMR = comprehensive medication review; LTC = long-term care; MTM = Medication Therapy Management.
Beneficiary predisposing, enabling, and need characteristics are compared across the three pharmacist cohorts: (1) community, (2) plan, and (3) vendor in-house pharmacist in Table 2.
Table 2.
Comparison of Predisposing, Enabling, and Need Characteristics of Medicare Beneficiaries Receiving a CMR by Community Pharmacists and Other Pharmacist Providers in 2014
| N=104,303 (100%) | |||||
|---|---|---|---|---|---|
| CMR Provided By: | |||||
| Community RPh n (%) |
Plan RPh n (%) |
p-value† | MTM Vendor In- House RPh n (%) |
p-value‡ | |
| Total Beneficiaries by Provider Status | 26,337 (25.3%) | 35,741 (34.3%) | 42,225 (40.5%) | ||
| Predisposing Variables | |||||
| Mean Age (SD) | 75 (6.8) | 75 (6.8) | 0.04 | 75 (6.9) | <0.001 |
| Male Gender | 9795 (37.2%) | 13,551 (37.9%) | 0.07 | 15,887 (37.6%) | 0.254 |
| Race | <0.001 | <0.001 | |||
| White | 18,767 (71.3%) | 24,922 (69.7%) | 32,322 (76.5%) | ||
| Black | 3012 (11.4%) | 4727 (13.2%) | 5296 (12.5%) | ||
| Asian | 512 (1.9%) | 1041 (2.9%) | 774 (1.8%) | ||
| Hispanic | 3743 (14.2%) | 4532 (12.7%) | 3227 (7.6%) | ||
| North American Native | 42 (0.2%) | 90 (0.3%) | 138 (0.3%) | ||
| Other/Unknown | 261 (1.0%) | 429 (1.2%) | 468 (1.1%) | ||
| Enabling Variables | |||||
| Urban Residence | 21,441 (81.4%) | 31,665 (88.6%) | <0.001 | 34,335 (81.3%) | 0.754 |
| Geographic Region | <0.001 | <0.001 | |||
| Northeast | 2217 (8.4%) | 4895 (13.7%) | 10,759 (25.5%) | ||
| South | 15,183 (57.6%) | 11,611 (32.5%) | 14,559 (34.5%) | ||
| Midwest | 5423 (20.6%) | 5943 (16.6%) | 9997 (23.7%) | ||
| West | 2520 (9.6%) | 12,338 (34.5%) | 6792 (16.1%) | ||
| Other | 994 (3.8%) | 954 (2.7%) | 118 (0.3%) | ||
| Income Enrollment Status | <0.001 | <0.001 | |||
| Dual Medicaid Enrollment | 4684 (17.8%) | 4711 (13.2%) | 7953 (18.8%) | ||
| Qualified Medicare Beneficiary | 1307 (5.0%) | 993 (2.8%) | 1482 (3.5%) | ||
| Specified Low-Income Medicare Beneficiary | 1282 (4.9%) | 963 (2.7%) | 1183 (2.8%) | ||
| No Low Income Subsidy Coverage | 19,064 (72.4%) | 29,074 (81.3%) | 31,607 (74.9%) | ||
| Copayment Status Indicator | <0.001 | <0.001 | |||
| Catastrophic Coverage During Year | 5779 (21.9%) | 5899 (16.5%) | 10,417 (24.7%) | ||
| Coverage Gap Exposure During Year | 10,589 (40.2%) | 14,639 (41.0%) | 15,605 (37.0%) | ||
| No Coverage Gap Exposure During Year | 9969 (37.9%) | 15,203 (42.5%) | 16,203 (38.4%) | ||
| Need Variables | |||||
| Cognitively Impaired | 1079 (4.1%) | 913 (2.6%) | <0.001 | 503 (1.2%) | <0.001 |
| Any Hospitalization | 2323 (8.8%) | 2175 (6.1%) | <0.001 | 5875 (13.9%) | <0.001 |
| Any ED Visit | 2658 (10.1%) | 2613 (7.3%) | <0.001 | 6761 (16.0%) | <0.001 |
| Mean Count of Hospitalization (SD) | 0.15 (0.6) | 0.09 (0.4) | <0.001 | 0.22 (0.7) | <0.001 |
| Mean Count of ED Visits (SD) | 0.19 (0.8) | 0.12 (0.5) | <0.001 | 0.27 (0.8) | <0.001 |
| Mean Number of Elixhauser Conditions (SD) | 0.63 (1.5) | 0.43 (1.2) | <0.001 | 1.01 (1.8) | <0.001 |
| Mean Elixhauser Mortality Weight (SD) | 1.02 (4.2) | 0.68 (3.5) | <0.001 | 1.67 (5.3) | <0.001 |
| Mean Therapeutic Drug Classes (SD) | 15.20 (5.2) | 14.42 (5.2) | <0.001 | 14.87 (5.0) | <0.001 |
| Specific Elixhauser Conditions | |||||
| Diabetes | 3097 (11.8%) | 2900 (8.1%) | <0.001 | 7733 (18.3%) | <0.001 |
| Hypertension | 3746 (14.2%) | 3875 (10.8%) | <0.001 | 10,101 (23.9%) | <0.001 |
| Congestive Heart Failure | 1253 (4.8%) | 947 (2.6%) | <0.001 | 2890 (6.8%) | <0.001 |
| Chronic Pulmonary Disease | 1492 (5.7%) | 1218 (3.4%) | <0.001 | 3297 (7.8%) | <0.001 |
| Depression | 587 (2.2%) | 404 (1.1%) | <0.001 | 1180 (2.8%) | <0.001 |
CMR = comprehensive medication review; ED = emergency department; MTM = medication therapy management; RPh = pharmacist; SD = standard deviation.
p-values represent comparisons using t-tests (continuous variables) or chi-square tests (categorical variables) between community pharmacist and plan pharmacist cohorts.
p-values represent comparisons using t-tests (continuous variables) or chi-square tests (categorical variables) between community pharmacist and MTM Vendor In-house pharmacist cohorts.
Predisposing Characteristics
Across all three pharmacist cohorts, beneficiaries were approximately 75 years of age and 37–38% were male. Community pharmacists served a smaller proportion of black beneficiaries (11.4%; p<0.001) compared with plan and vendor in-house pharmacist providers (13.2% and 12.5%, respectively). However, community pharmacists served a larger proportion of Hispanic beneficiaries (14.2%; p<0.001); almost double the proportion of beneficiaries served by vendor in-house pharmacists (7.6%).
Enabling Characteristics
The majority of beneficiaries receiving CMRs were urban residents across the three pharmacist provider cohorts; however, community pharmacists served more rural-residing beneficiaries (18.6%; p<0.001) compared with plan pharmacists (11.4%). A larger proportion of beneficiaries served by community pharmacists resided in the south (57.6%; p<0.001) compared with plan (32.5%) and vendor in-house pharmacist providers (34.5%). However, community pharmacists served smaller proportions of beneficiaries residing in the northeast and west (8.4% and 9.6%, respectively) compared with vendor in-house pharmacists (25.5% and 16.1%) and plan pharmacists (13.7% and 34.5%) respectively. Across all three pharmacist cohorts, the majority of beneficiaries lacked a low income assistance enrollment subsidy, however, those without a subsidy were less served by community pharmacists than by plan pharmacists (72.4% and 81.3%, respectively; p<0.001).
Need Characteristics
Community pharmacists provided CMRs to more cognitively impaired beneficiaries (4%) compared with both plan (3%) and vendor in-house (1%) pharmacists (p<0.001). When comparing other need variables (e.g., emergency department visit, Elixhauser conditions, hospitalization), the community pharmacist cohort comprised a slightly “sicker” (i.e., “needier”) population than the plan pharmacist cohort, but a healthier population than the MTM vendor in-house pharmacist cohort.
Table 3 compares MTM delivery by pharmacist provider type including (1) beneficiary entry into MTM program, (2) MTM services received, and (3) MTM interventions made.
Table 3.
Comparison of MTM Delivery to Beneficiaries Receiving CMRs by Community Pharmacists and Other Pharmacist Provider Types in 2014
| 104,303 (100%) | |||||
|---|---|---|---|---|---|
| CMR Provided By: | |||||
| Community RPh n (%) |
Plan RPh n (%) |
p-value† | MTM Vendor In-House RPh n (%) |
p-value‡ | |
| Total Beneficiaries by Provider Status | 26,337 (25.3%) | 35,741 (34.3%) | 42,225 (40.5%) | ||
| Entry into MTM Program | |||||
| Days from Plan Enrollment to MTM Enrollment | |||||
| Mean | 68.4 (78) | 72.9 (83) | 79.5 (78) | ||
| Median | 31 | 48 | <0.001c | 33 | <0.001d |
| 25th Percentile | 0 | 0 | 26 | ||
| 75th Percentile | 100 | 111 | 119 | ||
| Days from MTM Enrollment to CMR Offer, n (%) | |||||
| Mean (SD) | 30.5 (33) | 17.8 (29) | 20.4 (20) | ||
| Median | 28 | 9 | <0.001§ | 16 | <0.001¶ |
| 25th Percentile | 9 | 0 | 4 | ||
| 75th Percentile | 38 | 26 | 28 | ||
| 0 | 174 (0.7%) | 11,071 (31.0%) | 1,004 (2.4%) | ||
| 1–30 | 16,757 (63.6%) | 18,394 (51.5%) | 32,157 (76.2%) | ||
| 31–60 | 7915 (30.1%) | 5004 (14.0%) | 7757 (18.4%) | ||
| 61+ | 1491 (5.7%) | 1263 (3.5%) | 1178 (2.8%) | ||
| Unknown | 0 (0.0%) | 9 (0.0%) | 129 (0.3%) | ||
| Days from CMR Offer to First CMR Received | |||||
| Mean | 85.5 (86) | 101.4 (85) | 116.6 (93) | ||
| Median | 47 | 76 | <0.001§ | 94 | <0.001¶ |
| 25th Percentile | 20 | 32 | 31 | ||
| 75th Percentile | 140 | 155 | 194 | ||
| Part D Contract Type, n (%) | 0.394 | <0.001 | |||
| Managed Care | 19,643 (74.6%) | 26,543 (74.3%) | 19,734 (46.7%) | ||
| Prescription Drug Plan | 6690 (25.4%) | 9188 (25.7%) | 22,323 (52.9%) | ||
| Employer Sponsored | 4 (0.0%) | 10 (0.0%) | 168 (0.4%) | ||
| MTM Services Received | |||||
| CMR Delivery Method, n (%) | <0.001 | <0.001 | |||
| Face-to-Face | 13,010 (49.4%) | 380 (1.1%) | 9 (0.0%) | ||
| Telephone | 13,327 (50.6%) | 35,361 (98.9%) | 42,216 (100.0%) | ||
| Telehealth Consultation (Video Conferencing) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | ||
| CMR Recipient | <0.001 | <0.001 | |||
| Beneficiary | 23,281 (88.4%) | 32,261 (90.3%) | 36,246 (85.8%) | ||
| Beneficiary’s Prescriber | 53 (0.2%) | 7 (0.0%) | 14 (0.0%) | ||
| Caregiver/Other Authorized Individual | 3003 (11.4%) | 3473 (9.7%) | 5965 (14.1%) | ||
| Mean Number of CMRs Received (SD) | 1.01 (0.1) | 1.02 (0.1) | <0.001 | 1.03 (0.2) | <0.001 |
| Mean Number of Targeted Medication Reviews (SD) | 10.29 (8.9) | 5.71 (6.7) | <0.001 | 18.36 (18) | <0.001 |
| MTM Interventions Made | |||||
| Mean Number of MTP Recommendations Made to Prescribers (SD) | 1.80 (3.5) | 1.17 (2.5) | <0.001 | 1.64 (2.8) | <0.001 |
| Mean Number of MTP Resolutions With Prescribers (SD) | 0.22 (0.7) | 0.33 (0.9) | <0.001 | 0.35 (0.8) | <0.001 |
CMR = comprehensive medication review; MTM = Medication Therapy Management; MTP = medication therapy problem; RPh = pharmacist; SD = standard deviation.
P-values represent comparisons using t-tests (continuous variables) or chi-square tests (categorical variables) between community pharmacist and plan pharmacist cohorts.
P-values represent comparisons using t-tests (continuous variables) or chi-square tests (categorical variables) between community pharmacist and MTM Vendor In-house pharmacist cohorts.
P-values represent comparisons using Wilcoxon rank sum tests between community pharmacist and plan pharmacist cohorts.
P-values represent comparisons using Wilcoxon rank sum tests between community pharmacist and MTM Vendor In-house pharmacist cohorts.
Beneficiary Entry into MTM Program
Beneficiaries receiving MTM services from community pharmacists were enrolled into the MTM program within a median (25th percentile, 75th percentile) of 31 days (0, 100) from plan enrollment, which was significantly fewer days than beneficiaries receiving MTM services from plan or vendor in-house pharmacists (48 [0, 111] and 33 days [26, 119], respectively; p<0.001). The number of days between MTM enrollment and the CMR offer differed by pharmacist type, with the CMR offer occurring at a median (25th percentile, 75th percentile) of 28 (9, 38) days for community pharmacists, 9 (0, 26) days for plan pharmacists, and 16 (4, 28) for vendor in-house pharmacists (p<0.001). More beneficiaries in the community pharmacist cohort received the CMR offer greater than 60 days post-MTM program enrollment compared with plan and vendor in-house pharmacists. However, beneficiaries within the community pharmacist cohort had fewer median (25th percentile, 75th percentile) days between CMR offer to CMR receipt (47 [20, 140]; p<0.001), compared with plan (76 [32, 155]) and vendor in-house (94 [31, 194]) pharmacist cohorts. Among beneficiaries receiving CMRs from community pharmacists compared with plan pharmacists, there were no differences in beneficiary contract type (i.e., managed care vs. PDP). However, the payer mix for beneficiaries receiving CMRs from community pharmacists was significantly different from those receiving CMRs from MTM vendor in-house pharmacists (p<0.001).
MTM Services Received
Community pharmacists provided more CMRs face-to-face (49%; p<0.001) compared with plan and vendor in-house pharmacists (1% and 0%, respectively). For all three pharmacist provider types, at least 85% of CMRs provided were to the beneficiary. The community pharmacist cohort provided more TMRs than the plan pharmacist cohort (mean [SD] of 10.29 [8.9] vs. 5.71 [6.7], respectively; p<0.001), but less than the MTM vendor in-house pharmacist cohort (mean [SD] of 10.29 [8.9] vs. 18.36 [18], p<0.001).
MTM Interventions Made
Community pharmacists made slightly more MTP recommendations to prescribers (mean [SD] of 1.8 [3.5]; p<0.001) compared with plan and vendor in-house pharmacists (1.17 [2.5] and 1.64 [2.8], respectively). However, community pharmacists resolved slightly fewer MTPs (0.22 [0.7]; p<0.001) compared with plan and vendor in-house pharmacists (0.33 [0.9] and 0.35 [0.8], respectively).
Discussion
This is the first study, to our knowledge, to use a nationally representative sample of MTM beneficiaries to examine MTM delivery by community pharmacists. We found that of Medicare beneficiaries receiving at least one CMR in 2014, approximately 20% had the CMR provided by a community pharmacist. This finding appears to align with previous estimates from CMS that the use of MTM vendor-contracted community pharmacists occurred with only 26% of plans in 2014.30 However, utilization of community pharmacists for Part D MTM has grown, with about 65% of plans reporting use of MTM vendor-contracted community pharmacists in 2018.5 Therefore, better understanding of MTM delivery by community pharmacists has important practice implications.
We observed some differences between beneficiaries served by community pharmacists versus plan or MTM vendor in-house pharmacists. It is important to note that given the large sample sizes in this study, comparisons between cohorts were all statistically significant. However, statistical significance does not always imply clinical or policy significance. For this reason, we focus the discussion of results on findings with more meaningful clinical and/or policy implications. For example, we noted regional and racial/ethnic variation in beneficiaries served by community pharmacists compared with the other pharmacist provider cohorts. In addition, smaller proportions of patients lacking a low-income subsidy status24 were served by community pharmacists, indicating a less wealthy beneficiary cohort. Generally, beneficiaries served by community pharmacists appeared to be less medically complex than those served by MTM vendor in-house pharmacists, but more complex than those served by plan pharmacists. However, community pharmacists served a greater proportion of patients with cognitive impairment. Reasons for these differences are unknown and pose clinical/policy implications and thus, future research is warranted.
CMS guidance requires that plans offer beneficiaries newly eligible for MTM a CMR within 60 days of enrollment into the MTM program.4,28 Across all pharmacist provider cohorts examined, most CMRs were compliant with this requirement (medians of 28, 9, and 16 days for community, plan, and vendor in-house pharmacists, respectively). However, community pharmacists provided the greatest proportion of CMR offers greater than 60 days post-enrollment (6%). Reasons for this are unclear; it is conceivable that these beneficiaries were uniquely transient and unable to be reached at earlier time points. It is also unclear whether a plan representative was responsible for making offers prior to contact by the community pharmacist and the method (e.g., letter, phone outreach) by which offers were made.
Interestingly, the time from offer to CMR completion was the shortest for patients served by community pharmacists (medians of 47, 76, and 94 days for community, plan, and vendor in-house pharmacists respectively; p<0.001). Currently, CMS does not provide guidance on when a CMR must occur following an offer. Rather, with the inclusion of CMR completion rates as a Star Measure, plans are incentivized to ensure CMR completion occurs at some point during the calendar year.31 It is possible that, given declines in drug product reimbursements (e.g., direct and indirect remuneration fees32) since 2010,33 community pharmacists could feel increased pressure as compared with plan and MTM vendor in-house pharmacists to prioritize the completion of CMRs. Additionally, it is possible that personal relationships between community pharmacists and their patients resulted in more rapid patient acceptance of CMR offers. Recent literature has evaluated strategies, such as the use of scripted language, as well as phone calls and bag stuffers, for encouraging patients to accept CMR offers.15,34–36 As these practices become more common, research should examine whether changes in time from offer to CMR completion occur across provider types or are unique to specific provider types.
Not surprisingly, community pharmacists were the only pharmacist provider cohort examined that provided a meaningful number of CMRs face-to-face with patients and/or caregivers. However, it is notable that about half of community pharmacist-provided CMRs were conducted by telephone. Since 2014, telephonic MTM delivery by community pharmacists has become even more common, and MTM provision over video-conferencing has emerged.37 Future research should explore the effects of MTM delivery mode on patient outcomes, and whether variation is found by provider type.
We found that community pharmacists, as compared with plan and MTM vendor in-house pharmacists, made slightly more MTP recommendations to prescribers. However, on average, slightly fewer MTP resolutions occurred. Additionally, the majority of beneficiaries served by community pharmacists were urban residents; however, community pharmacists served more rural residents compared with plan pharmacists. These findings align with existing literature that has identified prescriber relationships and temporal/spatial location as a barrier for MTM delivery and MTP resolution.16,38 The inclusion of pharmacists in health information exchange is an important first step and the need for such has been noted previously. One study showed that having access to and sending medication recommendations using the electronic health record that physicians use resulted in efficient communications and timely medication changes.39 Therefore, without prescriber buy-in, information exchange will likely be insufficient for MTP resolution. Prior research found that while community pharmacists identified more MTPs during a CMR when having access to patient health records, they reported no difference in their confidence to resolve MTPs.40 Another study showed that trust is often the basis for pharmacist-physician collaborative relationships and recommendation acceptance.41 Medicare Part D MTM models in which community pharmacists practice under collaborative drug therapy management should be explored to determine whether MTP resolution is improved.
This study has limitations. Analyses were conducted for a 20% random sample of Medicare beneficiaries nationwide, linked to MTM claims data; therefore, we were limited by information in the administrative data set. Moreover, the data presented are from 2014 and CMS Part D MTM guidance and related policies (e.g., Star Measures) have changed since that time. However, these data represent the most recent Part D MTM claims data available to researchers and provide the first, to our knowledge, nationally representative estimates of MTM delivery by community pharmacists. Additionally, 2014 CMS MTM guidance increased emphasis on CMR receipt by patients residing in long-term care facilities who otherwise receive required monthly drug regimen reviews.28 Unfortunately, the long term care status of beneficiaries was unavailable in the 2014 data. Therefore, future evaluations should examine the extent to which these patients are served and what, if any, variation exists across provider types. It is also important to note that our analysis only includes MTM enrolled patients who received at least one CMR in 2014; patients who received only TMRs are not reported because most MTM claims data are linked to CMR claims. Additionally, given that CMS does not have specific coding for “community pharmacist”, it is possible that some CMRs were misattributed to their designated MTM provider cohort. Future CMR reporting should include more commonly used nomenclature to distinguish community pharmacists and other pharmacist provider types (e.g., ambulatory care) to facilitate program evaluation and research. Finally, our analyses only provide estimates pertaining to patient characteristics and Part D MTM delivery by pharmacist providers and did not evaluate impacts on patient outcomes. Future research should examine the effects of Medicare Part D MTM on patient outcomes, discerning beneficiaries that benefit to varying degrees, including how outcomes may be impacted by provider types.
Conclusion
Community pharmacists provided approximately one in five CMRs for Part D MTM eligible beneficiaries in 2014. Community pharmacists compared with non-community pharmacist providers completed CMRs more quickly, produced more MTP recommendations, but resolved fewer MTPs. There is a need for continued focus on the unique opportunities and challenges associated with community pharmacist MTM delivery. Future research should explore geographic/racial-ethnic disparities in beneficiaries served and strategies to increase negligible MTP resolution by community pharmacists.
Acknowledgements:
The authors would like to acknowledge the contributions of Eric Berger, M.S. for programming the tables and data to support this project.
Conflict of interest statement: Dr. Adeoye is supported by the Indiana Clinical and Translational Sciences Institute funded, in part by Award Number TL1TR001107 (A. Shekhar, PI) from the National Institutes of Health, National Center for Advancing Translational Sciences, Clinical and Translational Sciences Award; outside the work submitted. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Drs. Farley, Pestka, and Zillich have nothing to disclose. Dr. Coe reports grants from National Center for Advancing Translational Sciences of the National Institutes of Health under award number KL2TR002241, outside the submitted work. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Dr. Farris reports consulting with QuiO, outside the submitted work. Dr. Snyder reports grants (R21HS025005 and 1R18HS025943–01A1) and personal fees from Agency for Healthcare Research and Quality, and personal fees from Westat, Inc., outside the submitted work.
Contributor Information
Omolola A. Adeoye, Purdue University College of Pharmacy, Indianapolis, IN..
Joel F. Farley, University of Minnesota College of Pharmacy, Minneapolis, MN..
Antoinette B. Coe, University of Michigan College of Pharmacy, Ann Arbor, Michigan..
Deborah L. Pestka, University of Minnesota College of Pharmacy, Minneapolis, MN..
Karen B. Farris, University of Michigan College of Pharmacy, Ann Arbor, Michigan..
Alan J. Zillich, Purdue University College of Pharmacy, Indianapolis, IN..
Margie E. Snyder, Purdue University College of Pharmacy, Indianapolis, IN..
References
- 1.Lahue BJ, Pyenson B, Iwasaki K, Blumen HE, Forray S, Rothschild JM. National burden of preventable adverse drug events associated with inpatient injectable medications: healthcare and medical professional liability costs. Am Health Drug Benefits 2012;5(7):1–10. [PMC free article] [PubMed] [Google Scholar]
- 2.Joint Commission of Pharmacy Practitioners. Medication Management Services (MMS) Definition and Key Points [March 14, 2018]. Available from https://jcpp.net/wp-content/uploads/2018/05/Medication-Management-Services-Definition-and-Key-Points-Version-1.pdf. Accessed March 6, 2019.
- 3.Bluml BM. Definition of medication therapy management: development of professionwide consensus. J Am Pharm Assoc (2003) 2005;45(5):566–72. [DOI] [PubMed] [Google Scholar]
- 4.Centers for Medicare and Medicaid Services (CMS). CY 2019 medication therapy management program guidance and submission instructions [April 6, 2018]. Available from www.cms.gov/Medicare/Prescription-Drug-Coverage/PrescriptionDrugCovContra/Downloads/Memo-Contract-Year-2019-Medication-Therapy-Management-MTM-Program-Submission-v-040618.pdf. Accessed March 7, 2019.
- 5.Centers for Medicare and Medicaid Services (CMS). 2018. Medicare Part D Medication Therapy Management (MTM) programs fact sheet [2018]. Available from www.cms.gov/Medicare/Prescription-Drug-Coverage/PrescriptionDrugCovContra/Downloads/CY2018-MTM-Fact-Sheet.pdf. Accessed May 1, 2019.
- 6.Viswanathan M, Kahwati LC, Golin CE, et al. Medication therapy management interventions in outpatient settings: a systematic review and meta-analysis. JAMA Intern Med 2015;175(1):76–87. [DOI] [PubMed] [Google Scholar]
- 7.Snyder ME, Jaynes HA, Gernant SA, Lantaff WM, Hudmon KS, Doucette WR. Variation in medication therapy management delivery: Implications for health care policy. J Manag Care Spec Pharm 2018;24(9):896–902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Blake KB, Madhavan SS. Perceived barriers to provision of medication therapy management services (MTMS) and the likelihood of a pharmacist to work in a pharmacy that provides MTMS. Ann Pharmacother 2010;44(3):424–31. [DOI] [PubMed] [Google Scholar]
- 9.Bright DR, Lengel AJ, Powers MF. Pharmacists’ perceptions of barriers to implementing medication therapy management and the role of pharmacy technicians in overcoming the barriers. J Pharm Technol 2009;25(6):361–7. [Google Scholar]
- 10.Schommer JC, Planas LG, Johnson KA, Doucette WR. Pharmacist-provided medication therapy management (part 1): Provider perspectives in 2007. J Am Pharm Assoc (2003) 2008;48(3):354–63. [DOI] [PubMed] [Google Scholar]
- 11.Lengel M, Kuhn CH, Worley M, Wehr AM, McAuley JW. Pharmacy technician involvement in community pharmacy medication therapy management. J Am Pharm Assoc (2003) 2018;58(2):179–85. [DOI] [PubMed] [Google Scholar]
- 12.Gernant SA, Nguyen M-O, Siddiqui S, Schneller M. Use of pharmacy technicians in elements of medication therapy management delivery: A systematic review. Res Social Adm Pharm 2018;14(10):883–90. [DOI] [PubMed] [Google Scholar]
- 13.Pattin AJ, Powers MF, Lengel AJ. Training community pharmacy technicians about their roles in the provision of medication therapy management services. J Pharm Technol 2011;27(1):9–14. [Google Scholar]
- 14.Garcia GM, Snyder ME, McGrath SH, Smith RB, McGivney MS. Generating demand for pharmacist-provided medication therapy management: identifying patient-preferred marketing strategies. J Am Pharm Assoc (2003) 2009;49(5):611–6. [DOI] [PubMed] [Google Scholar]
- 15.Huet AL, Frail CK, Lake LM, Snyder ME. Impact of passive and active promotional strategies on patient acceptance of medication therapy management services. J Am Pharm Assoc (2003) 2015;55(2):178–81. [DOI] [PubMed] [Google Scholar]
- 16.McGrath SH, Snyder ME, Duenas GG, Pringle JL, Smith RB, McGivney MS. Physician perceptions of pharmacist-provided medication therapy management: qualitative analysis. J Am Pharm Assoc (2003) 2010;50(1):67–71. [DOI] [PubMed] [Google Scholar]
- 17.Adeoye OA, Lake LM, Lourens SG, Morris RE, Snyder ME. What predicts medication therapy management completion rates? The role of community pharmacy staff characteristics and beliefs about medication therapy management. J Am Pharm Assoc (2003) 2018;58(4s):S7–S15. [DOI] [PubMed] [Google Scholar]
- 18.Bacci JL, McGrath SH, Pringle JL, Maguire MA, McGivney MS. Implementation of targeted medication adherence interventions within a community chain pharmacy practice: The Pennsylvania Project. J Am Pharm Assoc (2003) 2014;54(6):584–93. [DOI] [PubMed] [Google Scholar]
- 19.Lounsbery JL, Green CG, Bennett MS, Pedersen CA. Evaluation of pharmacists’ barriers to the implementation of medication therapy management services. J Am Pharm Assoc (2003) 2009;49(1):51–8. [DOI] [PubMed] [Google Scholar]
- 20.Research Data Assistance Center (ResDAC).Part D medication therapy management data file [2019]. Available from www.resdac.org/cms-data/files/part-d-mtm-data-file/data-documentation. Accessed May 14, 2019.
- 21.Aday LA, Andersen R. A framework for the study of access to medical care. Health Serv Res 1974;9(3):208–20. [PMC free article] [PubMed] [Google Scholar]
- 22.Andersen R, Newman JF. Societal and individual determinants of medical care utilization in the United States. The Milbank Quarterly 2005;83(4): 10.1111/j.1468-0009.2005.00428.x. [DOI] [PubMed] [Google Scholar]
- 23.National Bureau of Economic Research. CMS’s SSA to FIPS CBSA and MSA county crosswalk. Available from www.nber.org/data/cbsa-msa-fips-ssa-county-crosswalk.html. Accessed March 6, 2019.
- 24.Medicare.gov. Medicare savings programs. Available from www.medicare.gov/your-medicare-costs/get-help-paying-costs/medicare-savings-programs. Accessed March 6, 2019.
- 25.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care 1998;36(1):8–27. [DOI] [PubMed] [Google Scholar]
- 26.Agency for Healthcare Research and Quality; HCUP Elixhauser Comorbidity Software. Healthcare Cost and Utilization Project (HCUP) [June 2017]. Available from www.hcup-us.ahrq.gov/toolssoftware/comorbidity/comindex2012-2015.txt. Accessed February 28, 2019.
- 27.Centers for Medicare and Medicaid Services (CMS). Trends in Part C & D star rating measure cut points [December 19, 2018]. Available from www.cms.gov/Medicare/Prescription-Drug-Coverage/PrescriptionDrugCovGenIn/Downloads/2019_Cut_Point_Trend.pdf. Accessed March 6, 2019.
- 28.Centers for Medicare and Medicaid Services (CMS). CY 2014 medication therapy management program guidance and submission instructions [April 5, 2013]. Available from www.cms.gov/medicare/prescription-drug-coverage/prescriptiondrugcovcontra/downloads/memo-contract-year-2014-medication-therapy-management-mtm-program-submission-v040513.pdf. Accessed March 7, 2019.
- 29.SAS [computer program]. Version 9.4. Cary, NC: SAS Institute Inc.; 2013. [Google Scholar]
- 30.Centers for Medicare and Medicaid Services (CMS). 2014. Medicare Part D Medication Therapy Management (MTM) programs fact sheet [August 21, 2014]. Available from www.cms.gov/medicare/prescription-drug-coverage/prescriptiondrugcovcontra/downloads/cy2014-mtm-fact-sheet.pdf. Accessed March 6, 2019.
- 31.Academy of Managed Care Pharmacy, American Pharmacists Association. Medicare star ratings: stakeholder proceedings on community pharmacy and managed care partnerships in quality. J Am Pharm Assoc (2003) 2014;54(3):228–40. [DOI] [PubMed] [Google Scholar]
- 32.Specialty Pharmacy Times. White paper: DIR fees simply explained [October 25, 2017]. Available from www.specialtypharmacytimes.com/news/white-paper-dir-fees-simply-explained. Accessed March 6, 2019.
- 33.Centers for Medicare and Medicaid Services (CMS). Medicare Part D – Direct and Indirect Remuneration (DIR) [January 19, 2017]. Available from www.cms.gov/newsroom/fact-sheets/medicare-part-d-direct-and-indirect-remuneration-dir. Accessed May 14, 2019.
- 34.Miguel A, Hall A, Liu W, et al. Improving comprehensive medication review acceptance by using a standardized recruitment ccript: A randomized control trial. J Manag Care Spec Pharm 2017;23(1):13–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Miller DE, Roane TE, Salo JA, Hardin HC. Evaluation of comprehensive medication review completion rates using 3 patient outreach models. J Manag Care Spec Pharm 2016;22(7):796–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Stafford R, Thomas J, Payakachat N, et al. Using an array of implementation strategies to improve success rates of pharmacist-initiated medication therapy management services in community pharmacies. Res Social Adm Pharm 2017;13(5):938–46. [DOI] [PubMed] [Google Scholar]
- 37.Lam A Practice innovations: delivering medication therapy management services via Videoconference interviews. Consult Pharm 2011;26(10):764–74. [DOI] [PubMed] [Google Scholar]
- 38.Snyder ME, Zillich AJ, Primack BA, et al. Exploring successful community pharmacist-physician collaborative working relationships using mixed methods. Res Social Adm Pharm 2010;6(4):307–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Farris KB, Mitrzyk BM, Batra P, et al. Linking the patient-centered medical home to community pharmacy via an innovative pharmacist care model. J Am Pharm Assoc (2003) 2019;59(1):70–8. [DOI] [PubMed] [Google Scholar]
- 40.Gernant SA, Zillich AJ, Snyder ME. Access to medical records’ impact on community pharmacist-delivered medication therapy management: A pilot from the Medication Safety Research Network of Indiana (Rx-SafeNet). J Pharm Pract 2018;31(6):642–50. [DOI] [PubMed] [Google Scholar]
- 41.Zillich AJ, McDonough RP, Carter BL, Doucette WR. Influential characteristics of physician/pharmacist collaborative relationships. Ann Pharmacother 2004;38(5):764–70. [DOI] [PubMed] [Google Scholar]


